Association of Nights and Weekends with Survival of Traumatic Out-of-Hospital Cardiac Arrest following Traffic Collisions: Japanese Registry-Based Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Data Source
2.2. Study Setting and Population
2.3. Variables
2.4. Outcomes
2.5. Statistical Analysis
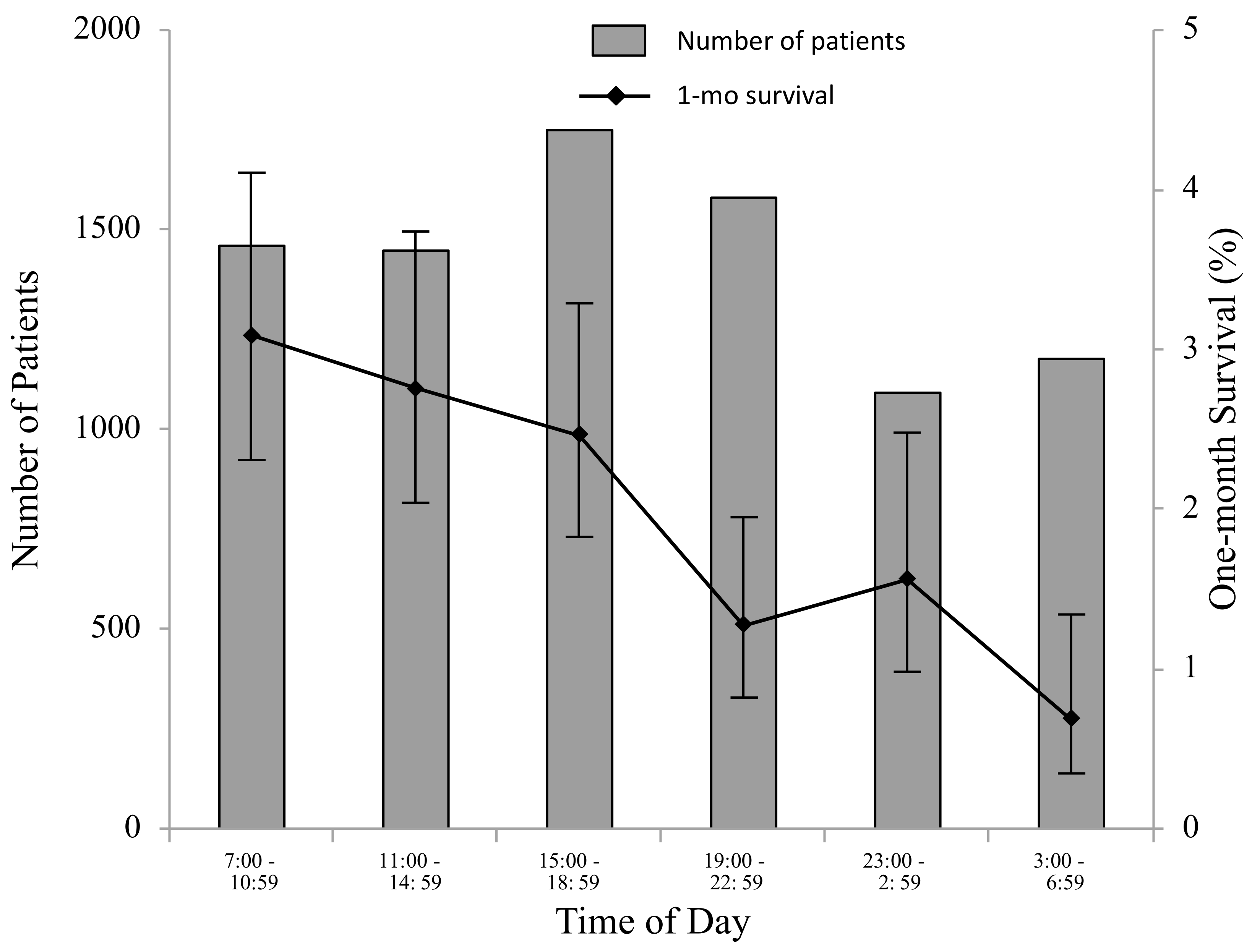
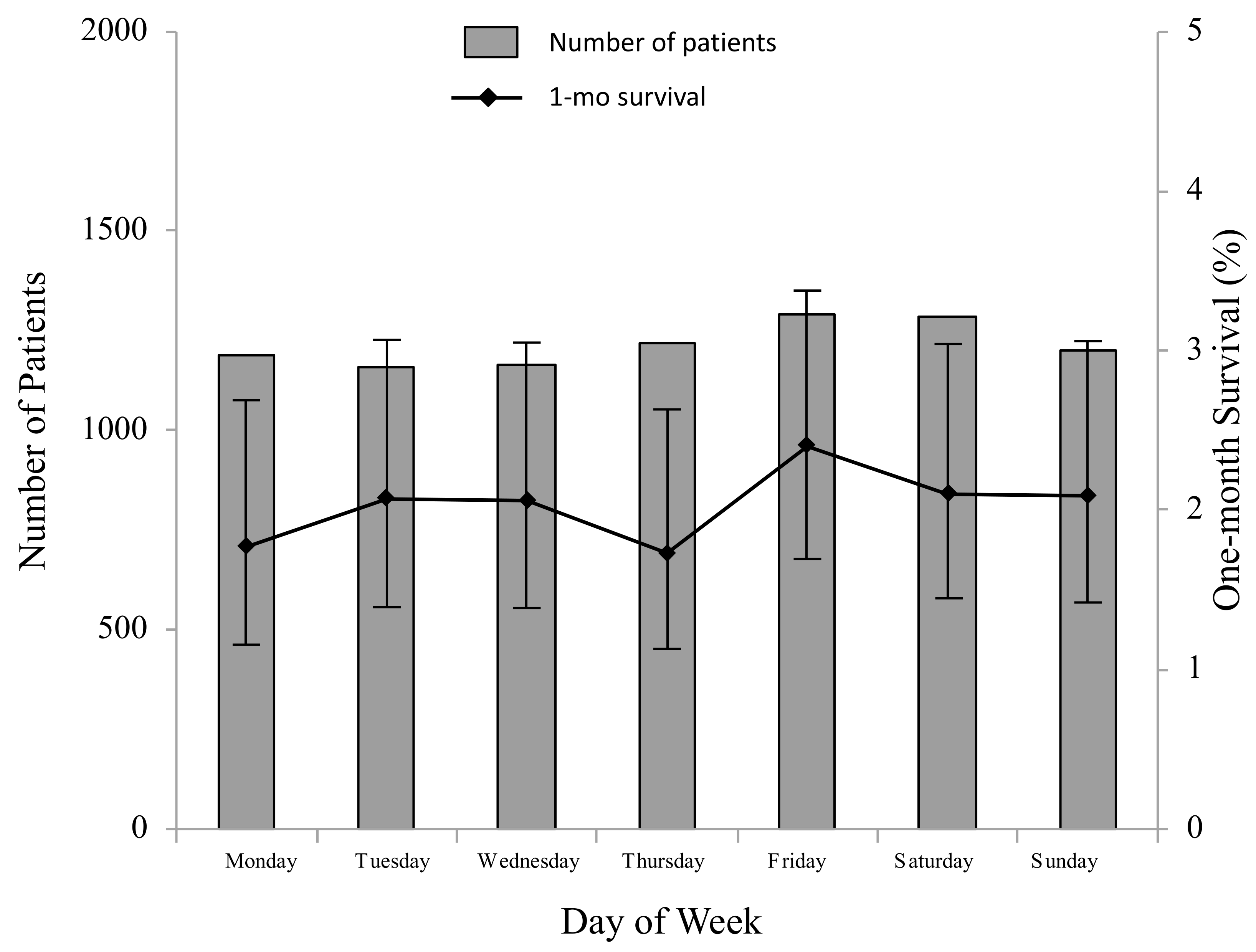
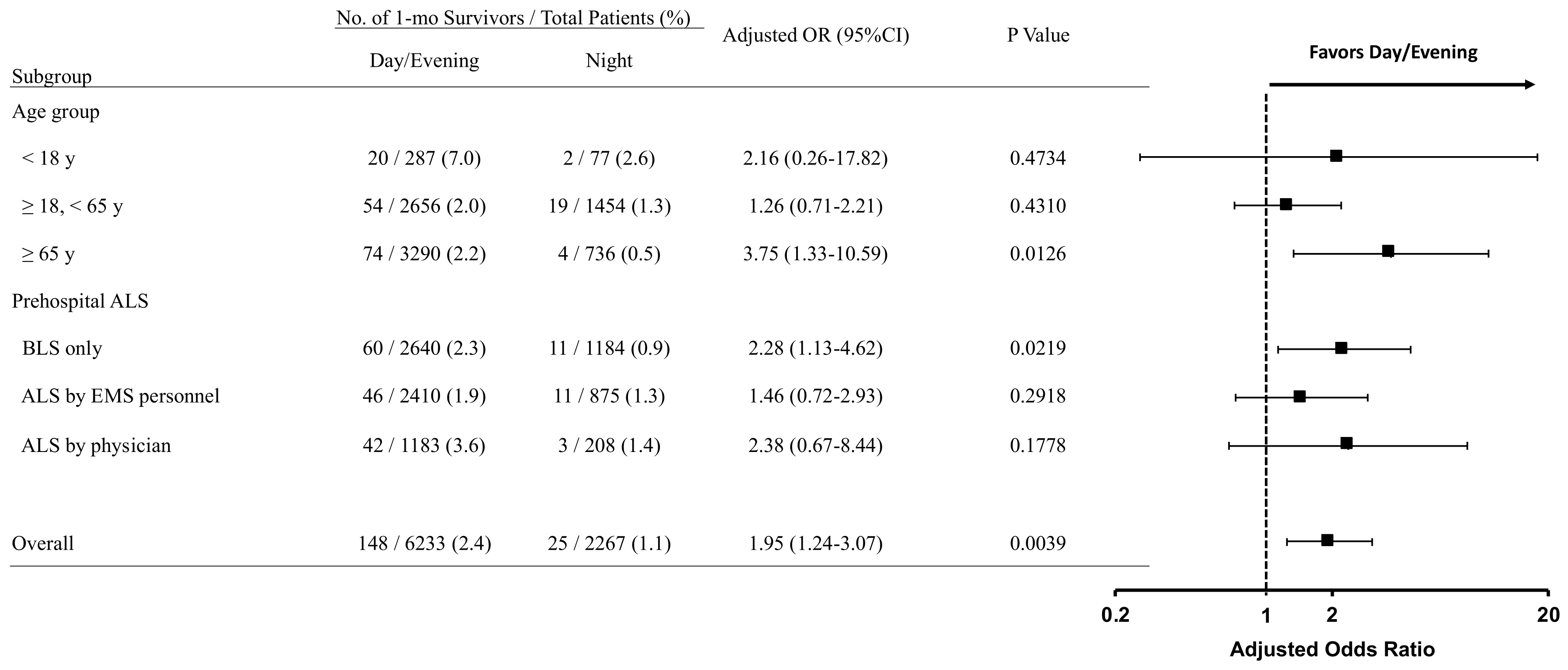
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Myat, A.; Song, K.J.; Rea, T. Out-of-hospital cardiac arrest: Current concepts. Lancet 2018, 391, 970–979. [Google Scholar] [CrossRef]
- Rea, T.D.; Eisenberg, M.S.; Sinibaldi, G.; White, R.D. Incidence of EMS-treated out-of-hospital cardiac arrest in the United States. Resuscitation 2004, 63, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Atwood, C.; Eisenberg, M.S.; Herlitz, J.; Rea, T.D. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation 2005, 67, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.; Koster, R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010, 81, 1479–1487. [Google Scholar] [CrossRef] [PubMed]
- Ong, M.E.; Shin, S.D.; De Souza, N.N.; Tanaka, H.; Nishiuchi, T.; Song, K.J.; Ko, P.C.; Leong, B.S.; Khunkhlai, N.; Naroo, G.Y.; et al. PAROS Clinical Research Network. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation 2015, 96, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Fire and Disaster Management Agency. Kyukyukyujo-no Genkyo 2019 [Current Situations of Emergency Medical Services and Rescue Services 2019]; Fire and Disaster Management Agency: Tokyo, Japan, 2019. [Google Scholar]
- Okubo, M.; Kiyohara, K.; Iwami, T.; Callaway, C.W.; Kitamura, T. Nationwide and regional trends in survival from out-of-hospital cardiac arrest in Japan: A 10-year cohort study from 2005 to 2014. Resuscitation 2017, 115, 120–128. [Google Scholar] [CrossRef]
- Fukuda, T.; Ohashi-Fukuda, N.; Matsubara, T.; Doi, K.; Kitsuta, Y.; Nakajima, S.; Yahagi, N. Trends in Outcomes for Out-of-Hospital Cardiac Arrest by Age in Japan: An Observational Study. Medicine 2015, 94, e2049. [Google Scholar] [CrossRef]
- Fukuda, T.; Ohashi-Fukuda, N.; Kondo, Y.; Hayashida, K.; Kukita, I. Association of Prehospital Advanced Life Support by Physician with Survival After Out-of-Hospital Cardiac Arrest With Blunt Trauma Following Traffic Collisions: Japanese Registry-Based Study. JAMA Surg. 2018, 153, e180674. [Google Scholar] [CrossRef]
- Zwingmann, J.; Mehlhorn, A.T.; Hammer, T.; Bayer, J.; Südkamp, N.P.; Strohm, P.C. Survival and neurologic outcome after traumatic out-of-hospital cardiopulmonary arrest in a pediatric and adult population: A systematic review. Crit. Care 2012, 16, R117. [Google Scholar] [CrossRef] [Green Version]
- Hopson, L.R.; Hirsh, E.; Delgado, J.; Domeier, R.M.; McSwain, N.E.; Krohmer, J. National Association of EMS Physicians; American College of Surgeons Committee on Trauma. Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest: Joint position statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma. J. Am. Coll. Surg. 2003, 196, 106–112. [Google Scholar]
- Beck, B.; Tohira, H.; Bray, J.E.; Straney, L.; Brown, E.; Inoue, M.; Williams, T.A.; McKenzie, N.; Celenza, A.; Bailey, P.; et al. Trends in traumatic out-of-hospital cardiac arrest in Perth, Western Australia from 1997 to 2014. Resuscitation 2016, 98, 79–84. [Google Scholar] [CrossRef]
- Barnard, E.; Yates, D.; Edwards, A.; Fragoso-Iñiguez, M.; Jenks, T.; Smith, J.E. Epidemiology and aetiology of traumatic cardiac arrest in England and Wales—A retrospective database analysis. Resuscitation 2017, 110, 90–94. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Kouseiroudou Hakusyo 2019 [Annual Report on Health, Labour and Welfare 2019–2020]; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2020. [Google Scholar]
- Zhou, Y.; Li, W.; Herath, C.; Xia, J.; Hu, B.; Song, F.; Cao, S.; Lu, Z. Off-Hour Admission and Mortality Risk for 28 Specific Diseases: A Systematic Review and Meta-Analysis of 251 Cohorts. J. Am. Heart Assoc. 2016, 5, e003102. [Google Scholar] [CrossRef] [Green Version]
- Wallace, S.K.; Abella, B.S.; Shofer, F.S.; Leary, M.; Agarwal, A.K.; Mechem, C.C.; Gaieski, D.F.; Becker, L.B.; Neumar, R.W.; Band, R.A. Effect of time of day on prehospital care and outcomes after out-of-hospital cardiac arrest. Circulation 2013, 127, 1591–1596. [Google Scholar] [CrossRef] [Green Version]
- Koike, S.; Tanabe, S.; Ogawa, T.; Akahane, M.; Yasunaga, H.; Horiguchi, H.; Matsumoto, S.; Imamura, T. Effect of time and day of admission on 1-month survival and neurologically favourable 1-month survival in out-of-hospital cardiopulmonary arrest patients. Resuscitation 2011, 82, 863–868. [Google Scholar] [CrossRef]
- Carr, B.G.; Reilly, P.M.; Schwab, C.W.; Branas, C.C.; Geiger, J.; Wiebe, D.J. Weekend and night outcomes in a statewide trauma system. Arch. Surg. 2011, 146, 810–817. [Google Scholar] [CrossRef]
- Cummins, R.O.; Chamberlain, D.; Hazinski, M.F.; Nadkarni, V.; Kloeck, W.; Kramer, E.; Becker, L.; Robertson, C.; Koster, R.; Zaritsky, A.; et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: The in-hospital ‘Utstein style’. American Heart Association. Circulation 1997, 95, 2213–2239. [Google Scholar] [CrossRef]
- Jacobs, I.; Nadkarni, V.; Bahr, J.; Berg, R.A.; Billi, J.E.; Bossaert, L.; Cassan, P.; Coovadia, A.; D’Este, K.; Finn, J.; et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004, 110, 3385–3397. [Google Scholar]
- Tanigawa, K.; Tanaka, K. Emergency medical service systems in Japan: Past, present, and future. Resuscitation 2006, 69, 365–370. [Google Scholar] [CrossRef] [Green Version]
- Hori, S. Emergency medicine in Japan. Keio J. Med. 2010, 59, 131–139. [Google Scholar] [CrossRef] [Green Version]
- Pronovost, P.J.; Angus, D.C.; Dorman, T.; Robinson, K.A.; Dremsizov, T.T.; Young, T.L. Physician staffing patterns and clinical outcomes in critically ill patients: A systematic review. JAMA 2002, 288, 2151–2162. [Google Scholar] [CrossRef] [PubMed]
- Needleman, J.; Buerhaus, P.; Mattke, S.; Stewart, M.; Zelevinsky, K. Nurse-staffing levels and the quality of care in hospitals. N. Engl. J. Med. 2002, 346, 1715–1722. [Google Scholar] [CrossRef] [PubMed]
- Needleman, J.; Buerhaus, P.; Pankratz, V.S.; Leibson, C.L.; Stevens, S.R.; Harris, M. Nurse staffing and inpatient hospital mortality. N. Engl. J. Med. 2011, 364, 1037–1045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuhn, G. Circadian rhythm, shift work, and emergency medicine. Ann. Emerg. Med. 2001, 37, 88–98. [Google Scholar] [CrossRef]
- Trockel, M.T.; Menon, N.K.; Rowe, S.G.; Stewart, M.T.; Smith, R.; Lu, M.; Kim, P.K.; Quinn, M.A.; Lawrence, E.; Marchalik, D.; et al. Assessment of Physician Sleep and Wellness, Burnout, and Clinically Significant Medical Errors. JAMA Netw. Open 2020, 3, e2028111. [Google Scholar] [CrossRef]
- Tsutsumi, A. Workstyle reform for Japanese doctors. Environ. Occup. Health Pract. 2020, 2, eohp.2020-0008-OP. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Outline of the “Act on the Arrangement of Related Acts to Promote Work Style Reform” (Act No. 71 of 2018); Ministry of Health, Labour and Welfare: Tokyo, Japan, 2018. [Google Scholar]
- Lee, S.; McCann, D.M.; Messenger, J.C. International Labour Organization. Working Time Around the World: Trends in Working Hours, Laws and Policies in a Global Comparative Perspective; Routledge: London, UK, 2007. [Google Scholar]
- Pega, F.; Náfrádi, B.; Momen, N.C.; Ujita, Y.; Streicher, K.N.; Prüss-Üstün, A.M.; Technical Advisory Group; Descatha, A.; Driscoll, T.; Fischer, F.M.; et al. Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000–2016: A systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 154, 106595. [Google Scholar] [CrossRef]
- World Medical Association. WMA Resolution on Task Shifting from the Medical Profession. Available online: https://www.wma.net/policies-post/wma-resolution-on-task-shifting-from-the-medical-profession/ (accessed on 1 June 2021).
- Orkin, A.M.; Rao, S.; Venugopal, J.; Kithulegoda, N.; Wegier, P.; Ritchie, S.D.; VanderBurgh, D.; Martiniuk, A.; Salamanca-Buentello, F.; Upshur, R. Conceptual framework for task shifting and task sharing: An international Delphi study. Hum. Resour. Health 2021, 19, 61. [Google Scholar] [CrossRef]

| Characteristic | All Patients n = 8500 | Time of Day | Day of Week | ||||
|---|---|---|---|---|---|---|---|
| Day/Evening n = 6233 | Night n = 2267 | p Value | Weekday n = 6018 | Weekend n = 2482 | p Value | ||
| Baseline Characteristics | |||||||
| Age, years | |||||||
| – Mean (SD) | 57.7 (22.3) | 60.0 (22.3) | 51.3 (21.0) | <0.0001 | 59.0 (22.1) | 54.6 (22.5) | <0.0001 |
| – Median (IQR) | 63 (41–76) | 66 (45–78) | 52 (33–69) | <0.0001 | 65 (43–77) | 58 (37–74) | <0.0001 |
| (1) < 18 years—No. (%) | 364 (4.3) | 287 (4.6) | 77 (3.4) | <0.0001 | 239 (4.0) | 125 (5.0) | <0.0001 |
| (2) ≥ 18, < 65 y—No. (%) | 4110 (48.4) | 2656 (42.6) | 1454 (64.1) | 2759 (45.8) | 1351 (54.4) | ||
| (3) ≥65 years—No. (%) | 4026 (47.4) | 3290 (52.8) | 736 (32.5) | 3020 (50.2) | 1006 (40.5) | ||
| Sex | |||||||
| (1) Male—No. (%) | 5828 (68.6) | 4016 (64.4) | 1812 (79.9) | <0.0001 | 4029 (66.9) | 1799 (72.5) | <0.0001 |
| (2) Female—No. (%) | 2672 (31.4) | 2217 (35.6) | 455 (20.1) | 1989 (33.1) | 683 (27.5) | ||
| Witness | |||||||
| (1) No witness—No. (%) | 2795 (32.9) | 1943 (31.2) | 852 (37.6) | <0.0001 | 1982 (32.9) | 813 (32.7) | 0.6047 |
| (2) By family member—No. (%) | 335 (3.9) | 304 (4.9) | 31 (1.4) | 229 (3.8) | 106 (4.3) | ||
| (3) By non–family member—No. (%) | 5370 (63.2) | 3986 (63.9) | 1384 (61.0) | 3807 (63.3) | 1563 (63.0) | ||
| Bystander CPR | |||||||
| (1) Yes–No. (%) | 2096 (24.7) | 1709 (27.4) | 387 (17.1) | <0.0001 | 1431 (23.8) | 665 (26.8) | 0.0034 |
| (2) No–No. (%) | 6404 (75.3) | 4524 (72.6) | 1880 (82.9) | 4587 (76.2) | 1817 (73.2) | ||
| Public–access defibrillation | |||||||
| (1) Yes–No. (%) | 25 (0.3) | 20 (0.3) | 5 (0.2) | 0.4501 | 18 (0.3) | 7 (0.3) | 0.8949 |
| (2) No–No. (%) | 8475 (99.7) | 6213 (99.7) | 2262 (99.8) | 6000 (99.7) | 2475 (99.7) | ||
| Dispatcher’s instruction for CPR | |||||||
| (1) Yes–No. (%) | 1703 (20.0) | 1304 (20.9) | 399 (17.6) | 0.0007 | 1193 (19.8) | 510 (20.5) | 0.4483 |
| (2) No–No. (%) | 6797 (80.0) | 4929 (79.1) | 1868 (82.4) | 4825 (80.2) | 1972 (79.5) | ||
| Initial rhythm | |||||||
| (1) VF—No. (%) | 151 (1.8) | 113 (1.8) | 38 (1.7) | <0.0001 | 107 (1.8) | 44 (1.8) | 0.8400 |
| (2) VT—No. (%) | 11 (0.1) | 10 (0.1) | 1 (0.0) | 8 (0.1) | 3 (0.1) | ||
| (3) PEA—No. (%) | 2954 (34.7) | 2268 (36.4) | 686 (30.3) | 2113 (35.1) | 841 (33.9) | ||
| (4) Asystole—No. (%) | 5191 (61.1) | 3682 (59.1) | 1509 (66.6) | 3657 (60.8) | 1534 (61.8) | ||
| (5) Others (e.g., Bradycardia)—No. (%) | 193 (2.3) | 160 (2.6) | 33 (1.4) | 133 (2.2) | 60 (2.4) | ||
| Prehospital ALS | |||||||
| (1) BLS only—No. (%) | 3824 (45.0) | 2640 (42.3) | 1184 (52.2) | <0.0001 | 2675 (44.5) | 1149 (46.3) | 0.0760 |
| (2) ALS by EMS personnel—No. (%) | 3285 (38.6) | 2410 (38.7) | 875 (38.6) | 2325 (38.6) | 960 (38.7) | ||
| (3) ALS by physician—No. (%) | 1391 (16.4) | 1183 (19.0) | 208 (9.2) | 1018 (16.9) | 373 (15.0) | ||
| Response time, min | |||||||
| —Mean (SD) | 10.5 (6.1) | 10.6 (5.9) | 10.5 (6.3) | 0.4011 | 10.4 (5.9) | 10.8 (6.4) | 0.0034 |
| —Median (IQR) | 9 (7–12) | 9 (7–12) | 9 (7–12) | 0.0754 | 9 (7–12) | 9 (7–13) | 0.0153 |
| Transport time, min | |||||||
| —Mean (SD) | 26.1 (11.4) | 26.4 (11.6) | 25.3 (11.1) | <0.0001 | 26.1 (11.5) | 26.0 (11.4) | 0.5774 |
| —Median (IQR) | 24 (18–33) | 24 (18–33) | 23 (17–31) | <0.0001 | 24 (17–33) | 24 (18–33) | 0.6613 |
| Year of arrest | |||||||
| (1) 2013—No. (%) | 1751 (20.6) | 1266 (20.3) | 485 (21.4) | 0.1679 | 1257 (20.9) | 494 (19.9) | 0.5670 |
| (2) 2014—No. (%) | 1696 (19.9) | 1216 (19.5) | 480 (21.2) | 1178 (19.6) | 518 (20.9) | ||
| (3) 2015—No. (%) | 1700 (20.0) | 1254 (20.1) | 446 (19.7) | 1208 (20.1) | 492 (19.8) | ||
| (4) 2016—No. (%) | 1690 (19.9) | 1270 (20.4) | 420 (18.5) | 1187 (19.7) | 503 (20.3) | ||
| (5) 2017—No. (%) | 1663 (19.6) | 1227 (19.7) | 436 (19.2) | 1188 (19.7) | 475 (19.1) | ||
| Season of arrest | |||||||
| (1) Spring (March, April, May)—No. (%) | 1997 (23.5) | 1466 (23.5) | 531 (23.4) | 0.9200 | 1426 (23.7) | 571 (23.0) | 0.5902 |
| (2) Summer (June, July, August)—No. (%) | 1906 (22.4) | 1404 (22.5) | 502 (22.2) | 1333 (22.2) | 573 (23.1) | ||
| (3) Autumn (September, October, November)—No. (%) | 2229 (26.2) | 1639 (26.3) | 590 (26.0) | 1566 (26.0) | 663 (26.7) | ||
| (4) Winter (December, January, February)—No. (%) | 2368 (27.9) | 1724 (27.7) | 644 (28.4) | 1693 (28.1) | 675 (27.2) | ||
| Region of arrest | |||||||
| (1) North—No. (%) | 906 (10.7) | 729 (11.7) | 177 (7.8) | <0.0001 | 646 (9.9) | 260 (10.5) | 0.5502 |
| (2) East—No. (%) | 4588 (54.0) | 3281 (52.6) | 1307 (57.7) | 3269 (54.2) | 1319 (53.1) | ||
| (3) West—No. (%) | 2910 (34.2) | 2175 (34.9) | 735 (32.4) | 2039 (34.1) | 871 (35.1) | ||
| (4) South—No. (%) | 96 (1.1) | 48 (0.8) | 48 (2.1) | 64 (1.8) | 32 (1.3) | ||
| Outcome | Day/Evening n = 6233 | Night n = 2267 | Adjusted OR (95%CI) | p Value |
|---|---|---|---|---|
| One–month survival—No. (%) | 148 (2.4) | 25 (1.1) | 1.95 (1.24–3.07) | 0.0039 |
| Prehospital ROSC—No. (%) | 407 (6.5) | 72 (3.2) | 1.56 (1.18–2.06) | 0.0017 |
| Outcome | Weekday n = 6018 | Weekend n = 2482 | Adjusted OR (95% CI) | p Value |
|---|---|---|---|---|
| One-month survival—No. (%) | 121 (2.0) | 52 (2.1) | 0.97 (0.69–1.38) | 0.8712 |
| Prehospital ROSC—No. (%) | 354 (5.9) | 125 (5.0) | 1.19 (0.95–1.49) | 0.1351 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukuda, T.; Ohashi-Fukuda, N.; Sekiguchi, H.; Inokuchi, R.; Kukita, I. Association of Nights and Weekends with Survival of Traumatic Out-of-Hospital Cardiac Arrest following Traffic Collisions: Japanese Registry-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 12769. https://doi.org/10.3390/ijerph182312769
Fukuda T, Ohashi-Fukuda N, Sekiguchi H, Inokuchi R, Kukita I. Association of Nights and Weekends with Survival of Traumatic Out-of-Hospital Cardiac Arrest following Traffic Collisions: Japanese Registry-Based Study. International Journal of Environmental Research and Public Health. 2021; 18(23):12769. https://doi.org/10.3390/ijerph182312769
Chicago/Turabian StyleFukuda, Tatsuma, Naoko Ohashi-Fukuda, Hiroshi Sekiguchi, Ryota Inokuchi, and Ichiro Kukita. 2021. "Association of Nights and Weekends with Survival of Traumatic Out-of-Hospital Cardiac Arrest following Traffic Collisions: Japanese Registry-Based Study" International Journal of Environmental Research and Public Health 18, no. 23: 12769. https://doi.org/10.3390/ijerph182312769
APA StyleFukuda, T., Ohashi-Fukuda, N., Sekiguchi, H., Inokuchi, R., & Kukita, I. (2021). Association of Nights and Weekends with Survival of Traumatic Out-of-Hospital Cardiac Arrest following Traffic Collisions: Japanese Registry-Based Study. International Journal of Environmental Research and Public Health, 18(23), 12769. https://doi.org/10.3390/ijerph182312769






