Self-Management Nursing Intervention for Controlling Glucose among Diabetes: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
Background
2. Materials and Methods
2.1. Design
2.2. Eligibility Criteria and Outcome Variables
2.3. Search Strategy
2.4. Quality Assessment
2.5. Data Collection
2.6. Data Analysis
3. Results
3.1. Data Extraction
3.2. Characteristics of Studies
3.3. Methodological Quality
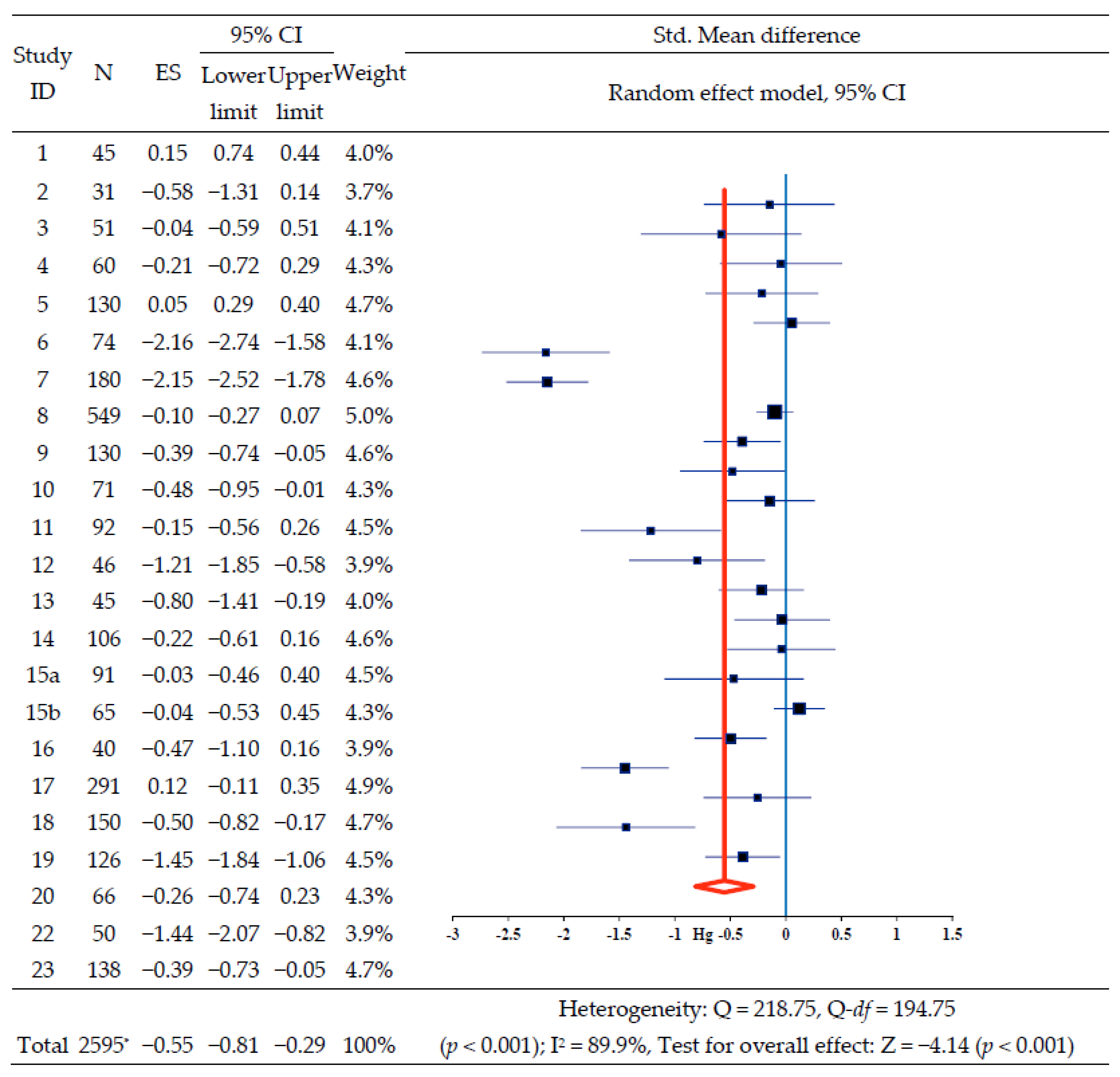
3.4. Effect of Nursing Intervention on HbA1c
3.5. Effect of Nursing Intervention on Secondary Outcomes
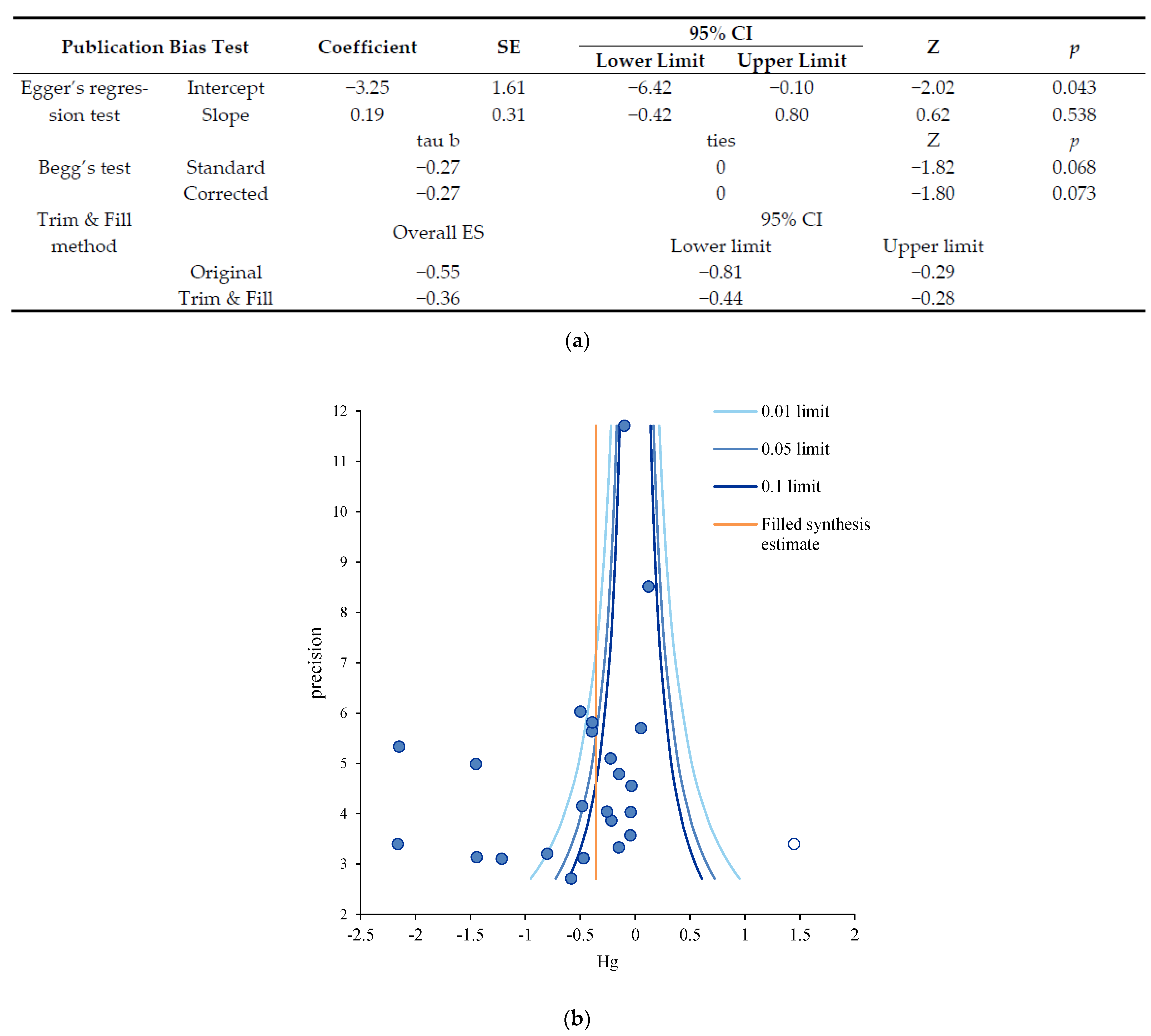
3.6. Publication Bias Analysis
4. Discussion
Limitations
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Newsroom Fact Sheet Diabetes. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 1 January 2001).
- Sarwar, N.; Gao, P.; Seshasai, S.K.; Gobin, R.; Kaptoge, S.; Di Angelantonio, E.; Ingelsson, E.; Lawlor, D.A.; Selvin, E.; Stampfer, M.; et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 735, 2215–2222. [Google Scholar] [CrossRef]
- Bourne, R.R.; Stevens, G.A.; White, R.A.; Smith, J.L.; Flaxman, S.R.; Price, H.; Jonas, J.B.; Keeffe, J.; Leasher, J.; Naidoo, K.; et al. Causes of vision loss worldwide, 1990–2010: A systematic analysis. Lancet Glob. Health 2013, 1, 339–349. [Google Scholar] [CrossRef]
- Kumar, K.M.; Saboo, B.; Rao, P.V.; Sarda, A.; Viswanathan, V.; Kalra, S.; Sethi, B.; Shah, N.; Srikanta, S.S.; Jain, S.M.; et al. Type 1 diabetes: Awareness, management and challenges: Current scenario in India. Indian J. Endocrinol. Metab. 2015, 19, 6–8. [Google Scholar] [CrossRef]
- Schulman-Green, D.; Jaser, S.; Martin, F.; Alonzo, A.; Grey, M.; McCorkle, R.; Redeker, N.S.; Reynolds, N.; Whittemore, R. Processes of self-management in chronic illness. J. Nurs. Sch. 2012, 44, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Rains, J.C.; Penzien, D.B.; Lipchik, G.L. Behavioral facilitation of medical treatment for headache--part II: Theoretical models and behavioral strategies for improving adherence. Headache 2006, 46, 1395–1403. [Google Scholar] [CrossRef]
- O’Donoghue, G.; O’Sullivan, C.; Corridan, I.; Daly, J.; Finn, R.; Melvin, K.; Peiris, C. Lifestyle interventions to improve glycemic control in adults with type 2 diabetes living in low-and-middle income countries: A systematic review and meta-analysis of randomized controlled trials (RCTs). Int. J. Environ. Res. Public Health 2021, 18, 6273. [Google Scholar] [CrossRef]
- Chin, Y.-R.; So, E.-S.; Lee, H.-Y. A meta-analysis of Korean diabetes patient studies from 1977 to 2008. J. Korean Public Health Nurs. 2011, 25, 5–16. [Google Scholar] [CrossRef]
- Kim, H.E.; Kim, E.J.; Kim, G. The effects of diabetes management programs using mobile app: A systematic review and a meta-analysis. J. Korean Contents Assoc. 2015, 15, 300–307. [Google Scholar] [CrossRef][Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- The Joanna Briggs Institute. Critical Appraisal Tools. South Australia, Australia. 2017. Available online: http://joannabriggs.org/research/critical-appraisal-tools.html (accessed on 10 October 2018).
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: West Sussex, UK, 2009. [Google Scholar]
- Bax, L. MIX 2.0. Professional Software for Meta-Analysis in Excel. Version 2.015. BiostatXL. 2016. Available online: https://www.meta-analysis-made-easy.com (accessed on 18 November 2018).
- Littell, J.H.; Corcoran, J.; Pillai, V. Systematic Reviews and Meta-Analysis; Oxford University Press: New York, NY, USA, 2008. [Google Scholar]
- Mavridis, D.; Salanti, G. How to assess publication bias: Funnel plot, trim-and-fill method and selection models. Evid.-Based Ment. Health 2014, 17, 30. [Google Scholar] [CrossRef]
- Jutterström, Å.; Hörnsten, H.; Sandström, H.; Stenlund, H.; Isaksson, U. Nurse-led patient-centered self-management support improves HbA1c in patients with type 2 diabetes—A randomized study. Patient Educ. Couns. 2016, 99, 1821–1829. [Google Scholar] [CrossRef]
- Park, K.M.; Kim, C.; Park, M.H.; Kim, H.R.; Shin, A.M. Effects of home visiting care program for patients with diabetes mellitus provided by public health Center. J. Korean Acad. Public Health Nurs. 2010, 24, 71–81. [Google Scholar]
- Ko, C.H.; Gu, M.O. The effects of a diabetic eduational program for coping with problem situation on self-efficacy, self care behaviors, coping and glycemic control in type 2 diabetic patients. Korean Soc. Nurs. Sci. 2004, 34, 1205–1214. [Google Scholar] [CrossRef]
- Park, J.A. Effect of the aquatic exercise program on diabetes self efficacy and self care behaviors in diabetic patients in community. J. Korean Converg. Soc. 2021, 12, 389–399. [Google Scholar] [CrossRef]
- Hyun, K.S.; Kim, K.M.; Jang, S.H. The effects of tailored diabetes education on blood glucose control and self-care. J. Korean Acad. Nurs. 2009, 39, 720–730. [Google Scholar] [CrossRef]
- Sim, K.H.; Hwang, M.S. Effect of self-monitoring of blood glucose based on diabetes self-management education on glycemic control in type 2 diabetes. J. Korean Acad. Soc. Nurs. Educ. 2013, 19, 127–136. [Google Scholar] [CrossRef][Green Version]
- Amsberg, S.; Anderbro, T.; Wredling, R.; Lisspers, J.; Lins, P.E.; Adamson, U.; Johansson, U.B. A cognitive behavior therapy-based intervention among poorly controlled adult type 1 diabetes patients—A randomized controlled trial. Patient Educ. Couns. 2009, 77, 72–80. [Google Scholar] [CrossRef]
- Prezio, E.A.; Cheng, D.; Balasubramanian, B.A.; Shuval, K.; Kendzor, D.E.; Culica, D. Community diabetes education (CoDE) for uninsured Mexican Americans: A randomized controlled trial of a culturally tailored diabetes education and management program led by a community health worker. Diabetes Res. Clin. Pract. 2013, 100, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Stuckey, H.L.; Dellasega, C.; Graber, N.J.; Mauger, D.T.; Lendel, I.; Gabbay, R.A. Diabetes nurse case management and motivational interviewing for change (DYNAMIC): Study design and baseline characteristics in the Chronic Care Model for type 2 diabetes. Contemp. Clin. Trials 2009, 30, 366–374. [Google Scholar] [CrossRef][Green Version]
- Li, D.; Elliott, T.; Klein, G.; Ur, E.; Tang, T.S. Diabetes nurse case management in a Canadian tertiary care setting: Results of a randomized controlled trial. Can. J. Diabetes 2017, 41, 297–304. [Google Scholar] [CrossRef]
- Gürkan, K.P.; Bahar, Z.; Böber, E. Effects of a home-based nursing intervention programme among adolescents with type 1 diabetes. J. Clin. Nurs. 2019, 28, 4513–4524. [Google Scholar] [CrossRef] [PubMed]
- Lemelin, A.; Godbout, A.; Paré, G.; Bernard, S. Improved glycemic control through the use of a telehomecare program in patients with diabetes treated with insulin. Diabetes Technol. Ther. 2020, 22, 243–248. [Google Scholar] [CrossRef]
- Thompson, D.M.; Kozak, S.E.; Sheps, S. Insulin adjustment by a diabetes nurse educator improves glucose control in insulin-requiring diabetic patients: A randomized trial. CMAJ 1999, 161, 959–962. [Google Scholar]
- Gallegos, E.C.; Ovalle-Berúmen, F.; Gomez-Meza, M.V. Metabolic control of adults with type 2 diabetes mellitus through education and counseling. J. Nurs. Sch. 2006, 38, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Martín-Payo, R.; Papín-Cano, C.; Fernández-Raigada, R.I.; Santos-Granda, M.I.; Cuesta, M.; González-Méndez, X. Motiva.DM2 project. A pilot behavioral intervention on diet and exercise for individuals with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2021, 171, 108579. [Google Scholar] [CrossRef]
- Wang, W.; Cheng, M.T.M.; Leong, F.L.; Goh, A.W.L.; Lim, S.T.; Jiang, Y. The development and testing of a nurse-led smartphone-based self-management programme for diabetes patients with poor glycaemic control. J. Adv. Nurs. 2020, 76, 3179–3189. [Google Scholar] [CrossRef] [PubMed]
- Alibrahim, A.; AlRamadhan, D.; Johny, S.; Alhashemi, M.; Alduwaisan, H.; Al-Hilal, M. The effect of structured diabetes self-management education on type 2 diabetes patients attending a Primary Health Center in Kuwait. Diabetes Res. Clin. Pract. 2021, 171, 108567. [Google Scholar] [CrossRef]
- Chan, M.F.; Yee, A.S.; Leung, E.L.; Day, M.C. The effectiveness of a diabetes nurse clinic in treating older patients with type 2 diabetes for their glycaemic control. J. Clin. Nurs. 2006, 15, 770–781. [Google Scholar] [CrossRef]
- Wang, X.; Yan, J.; Sun, Z.; Zhang, Y. The intervening efficacy of health management based on family and organization on elderly diabetic patients. Am. J. Transl. Res. 2021, 13, 3549–3554. [Google Scholar]
- Lyu, W.B.; Gao, Y.; Cheng, K.Y.; Wu, R.; Zhou, W.Q. Effect of self-acupoint massage on blood glucose level and quality of life in older adults with type 2 diabetes mellitus: A randomized controlled trial. J. Gerontol. Nurs. 2019, 45, 43–48. [Google Scholar] [CrossRef]
- Chi, S.; Liu, J.L.; Kang, H.C.; Lv, D.M. Continuous nursing intervention on recovery of diabetic patients. J. Biol. Regul. Homeost. Agents 2018, 32, 1507–1513. [Google Scholar]
- Mollaoğlu, M.; Beyazit, E. Influence of diabetic education on patient metabolic control. Appl. Nurs. Res. 2009, 22, 183–190. [Google Scholar] [CrossRef]
- Aubert, R.E.; Herman, W.H.; Waters, J.; Moore, W.; Sutton, D.; Peterson, B.L.; Bailey, C.M.; Koplan, J.P. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization. A randomized, controlled trial. Ann. Intern. Med. 1998, 129, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Duval, S.; Tweedie, R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J. Am. Stat. Assoc. 2000, 95, 89–98. [Google Scholar] [CrossRef]
- Lin, M.Y.; Liu, M.F.; Hsu, L.F.; Tsai, P.S. Effects of self-management on chronic kidney disease: A meta-analysis. Int. J. Nurs. Stud. 2017, 74, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Nieuwesteeg, A.; Pouwer, F.; van der Kamp, R.; van Bakel, H.; Aanstoot, H.; Hartman, E. Quality of life of children with type 1 diabetes: A systematic review. Curr. Diabetes Rev. 2012, 8, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Bosworth, H. Improving Patient Treatment Adherence: A Clinician’s Guide; Springer: New York, NY, USA, 2010. [Google Scholar]
- Ryan, P.; Sawin, K.J. The Individual and Family Self-Management Theory: Background and perspectives on context, process, and outcomes. Nurs. Outlook 2009, 57, 217–225. [Google Scholar] [CrossRef]
- Sikalidis, A.K.; Öztağ, M. Optimized snacking is positively associated with socioeconomic status and better Type 2 Diabetes Mellitus management in Turkish patients. Gazz. Med. Ital.-Arch. Sci. Med. 2020, 179, 459–467. [Google Scholar] [CrossRef]
- Nielsen, P.J.; Hafdahl, A.R.; Conn, V.S.; LeMaster, J.W.; Brown, S.A. Meta-analysis of the effect of exercise interventions on fitness outcomes among adults with type 1 and type 2 diabetes. Diabetes Res. Clin. Pract. 2006, 74, 111–120. [Google Scholar] [CrossRef]
- Van Meijel, L.A.; Tack, C.J.; De Galan, B.E. Effect of short-term use of dapagliflozin on impaired awareness of hypoglycaemia in people with type 1 diabetes. Diabetes Obes. Metab. 2021, 23, 2582–2589. [Google Scholar] [CrossRef] [PubMed]
- Klimontov, V.V.; Saik, O.V.; Korbut, A.I. Glucose variability: How does it work? Int. J. Mol. Sci. 2021, 22, 7783. [Google Scholar] [CrossRef]
- Fenerty, S.D.; Weest, C.; Davis, S.A.; Kaplan, S.G.; Feldman, S.R. The effect of reminder systems on patients’ adherence to treatment. Patient Prefer Adherence 2012, 6, 127–135. [Google Scholar] [CrossRef]
- Sikalidis, A.K.; Karaboğa, E.P. Healthy diet and self-care activities’ adherence improved life-quality and Type 2 Diabetes Mellitus management in Turkish adults. Gazz. Med. Ital.-Arch. Sci. Med. 2020, 179, 528–537. [Google Scholar] [CrossRef]
- Larsen, P.D.S. Lubkin’s Chronic Illness: Impact and Intervention, 10th ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2017. [Google Scholar]
- Riegel, B.; Jaarsma, T.; Stromberg, A. A middle-range theory of self-care of chronic illness. Adv. Nurs. Sci. 2012, 35, 194–204. [Google Scholar] [CrossRef]
- Boyd, C.M.; Fortin, M. Future of multimorbidity research: How should understanding of multimorbidity inform health system design? Public Health Rev. 2010, 32, 451–474. [Google Scholar] [CrossRef]
- Norris, S.L.; Engelgau, M.M.; Narayan, K.M. Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care 2021, 24, 561–587. [Google Scholar] [CrossRef]
- Grey, M.; Knafl, K.; McCorkle, R. A framework for the study of self- and family management of chronic conditions. Nurs. Outlook 2006, 54, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Funnell, M.M.; Brown, T.L.; Childs, B.P.; Haas, L.B.; Hosey, G.M.; Jensen, B.; Maryniuk, M.; Peyrot, M.; Piette, J.D.; Reader, D.; et al. National standards for diabetes self-management education. Diabetes Care 2007, 30, 1630–1637. [Google Scholar] [CrossRef] [PubMed][Green Version]

| Study ID | Author | Year | Country | Center | Fund | Participants | Characteristics of Participants | Quality Score |
|---|---|---|---|---|---|---|---|---|
| 1 | Park et al. [17] | 2010 | Korea | 1 | No | T2DM, N = 45 (E: 25, C: 20) | Public health center registration, Adults > 18 | 5 |
| 2 | Ko and Gu [18] | 2004 | Korea | 1 | No | T2DM, N = 31 (E: 17, C: 14) | Age 20–70 years, completed diabetes education | 8 |
| 3 | Park [19] | 2021 | Korea | 1 | No | T2DM, N = 51 (E: 26, C: 25) | Public health center registration, Adults > 18 | 8 |
| 4 | Hyun et al. [20] | 2009 | Korea | 1 | Yes | T2DM, N = 60 (E: 30, C: 30) | Uncontrolled diabetic patients, Adults > 20, HbA1C > 6.5%, PP2 > 180 mg/dL | 7 |
| 5 | Sim and Hwang [21] | 2013 | Korea | 1 | No | T2DM, N = 130 (E: 65, C: 65) | OHA treatment, HbA1C > 7.0% | 8 |
| 6 | Amsberg et al. [22] | 2009 | Sweden | 2 | Yes | T1DM, N = 74 (E: 36, C: 38) | Age: 18–65 years, BMI < 30 kg/m2, HbA1c > 7.5% | 8 |
| 7 | Prezio et al. [23] | 2013 | USA | 1 | No | T2DM, N = 180 (E: 90, C:90) | Age 18–75 years, OHA treatment | 8 |
| 8 | Stuckey et al. [24] | 2009 | USA | 2 | No | T2DM, N = 549 (E: 276, C: 273) | Uncontrolled DM (HbA1c > 8.5), hypertension (BP > 140/90), hyperlipidemia (LDL > 130), Age 18–75 year | 10 |
| 9 | Li et al. [25] | 2017 | Canada | 2 | Yes | T2DM, N = 130 (E: 69, C: 61) | Age ≥ 18, HbA1c ≥ 8% Mean age > 55 | 9 |
| 10 | Gurkan et al. [26] | 2019 | Turkey | 2 | No | T1DM, N = 71 (E: 35, C: 36) | Pediatric endocrinology outpatient (Adolescents: 13–17 years) | 9 |
| 11 | Lemelin et al. [27] | 2020 | Canada | 1 | Yes | T1DM + T2DM, N = 92 (E: 45, C: 47) | Diabetes center outpatient, Adults > 18 | 7 |
| 12 | Thompson et al. [28] | 1999 | Canada | 1 | No | T1DM + T2DM, N = 46 (E: 23, C: 23) | Adults > 18, treated with at least one injection of insulin per day HbA1c > 8.5 | 13 |
| 13 | Gallegos et al. [29] | 2006 | Mexico | 2 | No | T2DM, N = 45 (E: 25, C:20) | Cr < 1.5 ml/dl, Mean age > 40 | 6 |
| 14 | Martin-payo et al. [30] | 2021 | Spain | 4 | No | T2DM, N = 106 (E: 59, C: 47) | Health care centers, Adults > 18 | 7 |
| 15 | Jutterstrom et al. [16] | 2016 | Sweden | 10 | Yes | T2DM, N = 124 (E1: 59, E2: 33, C: 32) | Health care centers, Adults > 18 | 9 |
| 16 | Wang et al. [31] | 2020 | Singapore | 1 | Yes | T2DM, N = 40 (E: 20, C: 20) | Tertiary acute public hospital outpatient, Adults> 21, HbA1c > 8% | 5 |
| 17 | Alibrahim et al. [32] | 2021 | Kuwait | 1 | No | T2DM, N = 291 (E: 150, C: 141) | Primary Health Center, Adults > 21 | 6 |
| 18 | Chan et al. [33] | 2006 | Hong Kong (China) | 2 | No | T2DM, N = 150 (E: 75, C: 75) | Elderly > 65 | 7 |
| 19 | Wang et al. [34] | 2021 | China | 1 | Yes | T2DM, N = 126 (E: 63, C: 63) | FBG > 7.0 mmol/L, 2-h PBG > 11.1 mmol/L, HbA1C > 6.5%, Elderly > 60 | 6 |
| 20 | Lyu et al. [35] | 2019 | China | 1 | No | T2DM, N = 66 (E: 32, C: 34) | Elderly > 60 | 8 |
| 21 | Chi et al. [36] | 2018 | China | 1 | No | T2DM, N = 80 (E: 40, C: 40) | Age 30–80 years | 5 |
| 22 | Mollaoglu and Beyazit [37] | 2009 | Turkey | 1 | No | T2DM, N = 50 (E: 25, C: 25) | Mean age > 50 | 7 |
| 23 | Aubert et al. [38] | 1998 | USA | 2 | No | T1DM + T2DM, N = 138 (E: 71, C: 67) | Mean age > 50 | 9 |
| Study ID | Author | Research Design | Intervention | Intervention Contents | Facilitator | Period of Intervention | Program Session | Session Time | Post-Test Measurement | Outcome Variables |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Park et al. [17] | RCT | Home visiting | Diet, exercise, medication, and maintaining normal blood sugar range | Visiting nurse, student nurse | 10 wk | 10 session | not mentioned | Immediately | HbA1C, self-efficacy, self-care performance, cholesterol, HDL, and LDL |
| 2 | Ko and Gu [18] | Quasi-E | Education | Coping with Problem Situation | Nurse | 4 wk | 4 session | 120 min | Immediately | HbA1C, self-efficacy, self- care behaviors, and coping with problematic situations |
| 3 | Park [19] | Quasi-E | Exercise, Education, and Counselling | Aquatic exercise, self-management | Researcher, aquatic exercise instructor | 12 wk | 24 session | 80 min | Immediately | HbA1c, self- care behaviors, self-efficacy, SBP, DBP, FBS, BMI, Waist–hip ratio, and percent of body fat |
| 4 | Hyun et al. [20] | Quasi-E | Customized nursing | 1:1 customized diabetes education | doctor, diabetes education nurse, nutritionist, and pharmacist | not mentioned | 3 session | 30 min | With delay | HbA1C, PP2, self- blood glucose, insulin injection, and lifestyle |
| 5 | Sim and Hwang [21] | Quasi-E | Customized nursing | Self-Management Education (Self-monitoring of blood glucose) | Diabetes education nurse | 12 month | 2 session | 100 min | Immediately | Hb A1c, goal achievement on Hb A1c |
| 6 | Amsberg et al. [22] | RCT | Cognitive behavior therapy | Cognitive Behavior Therapy | Nurse | 8 wk | 8 session | 120 min | Immediately | HbA1c, BMI, self-care behaviors, emotional distress (PAID), fear for hypoglycemia, and psychosocial factors (anxiety, depression) |
| 7 | Prezio et al. [23] | RCT | Customized nursing | Community diabetes education (CoDE) program | Community health worker (3 full-time physicians, bilingual medical assistants and clerical staff | 12 months | 7 session | 60 min | Immediately | HbA1c, blood pressure (SBP, DBP), BMI, and lipid status (LDL, HDL, and TG) |
| 8 | Stuckey et al. [24] | RCT | Case Management | Motivational interviewing (MI) to deliver the self-management intervention | Nurse | 2-year study | not mentioned | not mentioned | Immediately | HbA1c, BMI, Lipid profile, SBP, DBP, emotional distress (PAID), treatment satisfaction (DTSQ), and depression (CES-D) |
| 9 | Li et al. [25] | RCT | Nurse Case Management | Diabetes self-management education and support, monitoring and algorithm-driven treatment adjustment | Nurse | 6 months | 12 session | 60 min | Immediately | HbA1c, diabetes distress (DDS), clinical (SBP, DBP, BMI), and behavioral and psychosocial outcome |
| 10 | Gurkan et al. [26] | Quasi-E | Home visiting | Home-based nursing intervention program | Nurse | 5 wk | 5 session | not mentioned | Immediately | HbA1c, self-efficacy, and diabetes behavior |
| 11 | Lemelin et al. [27] | Quasi-E | Customized nursing | Tele-home care (THC) Program | Nurse, doctor | 6 months | frequently feed back | not mentioned | Immediately | HbA1c, self-efficacy, and diabetes behavior rating |
| 12 | Thompson et al. [28] | RCT | Customized nursing (insulin adjustment) | Phone contact with the nurse: advice about adjustment of insulin therapy | Diabetes nurse educator | 6 months | 78 session | 15 min | Immediately | HbA1c, medical visits, and nursing interventions during 3-month period on THC |
| 13 | Gallegos et al. [29] | Quasi-E | Education and counselling | Educational session, counseling session | Nurse | 12 months (50 weeks) | 6 session | 90 min | Immediately | HbA1c, diabetes self-care activities, self-care capabilities, psychological adaptation to the chronic illness, and barriers to self-care |
| 14 | Martin-payo et al. [30] | Quasi-E | Education | Educational intervention (dietary and exercise habits) | Nurse | 6 months | 4 session | 10–20 min | Immediately | HbA1c, BMI, recommendation related to diet and exercise, motivation, competence autonomy, and social support for healthy eating and exercise |
| 15 | Jutterstrom et al. [16] | RCT | Customized nursing | E1: group intervention, E2: individual intervention | Nurse | 12 months | 6 session | 45–90 min | Immediately | HbA1c, BMI, waist circumference, blood pressure (SBP, DBP), lipid profile (Chol, HDL, LDL, and TG) |
| 16 | Wang et al. [31] | Quasi-E | Nurse-led smartphone-based self-management | Telephone follow-up and face-to-face patient education, Care4Diabetse app sessions | Nurse | 6 months | not mentioned | not mentioned | Immediately | HbA1c, Diabetes-Dependent Quality of Life (DDQoL), Revised Summary of Diabetes Self-care Activities (RSDSCA), General Self-efficacy Scale (GSS) |
| 17 | Alibrahim et al. [32] | Quasi-E | Education and self-control | DSME (diabetes self-management education) | Certified Diabetes Educator (CDE) nurses | 12 months | DSME educational sessions | 60 min | Immediately | HbA1c, BMI, waist circumference, and blood pressure |
| 18 | Chan et al. [33] | Quasi-E | Education and home visiting | Education (medication, diet, and exercises), telephone follow up | Nurse | 3 months | 6 session | 30 min | Immediately | HbA1c, SBP, DBP, body weight, and PEQD (informed choice role, co-producer role, and evaluator role) |
| 19 | Wang et al. [34] | RCT | Customized nursing | Customized health education | Nurse | 12 months | not mentioned | not mentioned | Immediately | Blood glucose level (HBA1c, FBS, and PP2), health management efficacy, self-rating anxiety scale (SAS), self-rating depression scale (SDS), and quality of life |
| 20 | Lyu et al. [35] | RCT | Self-acupoint massage | Routine nursing (exercise, diet, weight and caloric control, glucose monitoring, medication, and mental health assessment), self-acupoint massage, | Nurse (SEAM) | 12 wk | not mentioned | 120 min | Immediately | HbA1c, FBS, PP2, The Diabetes-Specific Quality of Life (QOL) |
| 21 | Chi et al. [36] | RCT | Education and home visiting | health education (knowledge of diabetes, diet and exercise, glucose management, proper insulin injection, and complications), home visits | Nurse | 12 wk | 5 session | 60 min | Immediately | Blood glucose control of patients (FBS, PP2), self-nursing ability |
| 22 | Mollaoglu and Beyazit [37] | RCT | Education and home visiting | Nurse-initiated education program (diet, exercise, use of medication, measuring blood glucose, and urine control), home visit | Nurse | 8 wk | 3 session | 70 min | Immediately | HbA1c, PP2, FBS, blood–urine glucose, lipid profile |
| 23 | Aubert et al. [38] | RCT | Case management | Followed written management algorithms (diet, exercise, oral agents, bedtime, and insulin) | Nurse (family physician and an endocrinologist) | 12 months | Not mentioned | Not mentioned | Immediately | HbA1c, FBS, medication type and dose, body weight, blood pressure, lipid levels, patient-perceived health status, episodes of severe hypoglycemia, and emergency department and hospital admissions |
| Joanna Briggs Institute of Critical Appraisal Tools Checklist for Quasi-Experimental Studies | Total Score | |||||||||||||
| Study ID | Clarity of Cause and Effect | Similarity of Treatment Groups | Similar Treatment | Comparison of the Treated Group | Multiple Measurement | Follow up Complete and If Not, Adequately Described and Analyzed | Same Way of Outcomes Measure | Reliable Way of Outcomes Measure | Appropriate Statistical Analysis | |||||
| 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | ||||
| 3 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 8 | ||||
| 4 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 7 | ||||
| 5 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 | ||||
| 10 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 | ||||
| 11 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | ||||
| 13 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 6 | ||||
| 14 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | ||||
| 17 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 6 | ||||
| 18 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 | ||||
| 19 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 6 | ||||
| Subtotal | 11 | 5 | 11 | 11 | 11 | 8 | 11 | 7 | 4 | 7.86 | ||||
| Joanna Briggs Institute of Critical Appraisal Tools Checklist for Checklist for Randomized Controlled Trials | Total Score | |||||||||||||
| Study ID | Random assignment | Allocation Concealment | Treatment Groups Similarity | Blinding of Participants | Blinding of Delivering Treatment | Blinding of Outcome Assessor | Similar Treatment | Follow up Complete and If Not, Adequately Described and Analyzed | Participants Analysis in the Groups | Same Way of Outcomes Measure | Reliable Way of Outcomes Measure | Appropriate Statistical Analysis | Appropriate of the Trial design | |
| 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 5 |
| 6 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 8 |
| 7 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 8 |
| 8 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| 9 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| 12 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13 |
| 15 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 9 |
| 16 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 5 |
| 20 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 8 |
| 21 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 5 |
| 22 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 7 |
| 23 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 |
| Subtotal | 7 | 5 | 10 | 2 | 1 | 2 | 12 | 12 | 12 | 12 | 8 | 6 | 7 | 7.61 |
| Characteristics | Subgroup | K | Study ID | N | Overall ES | 95% CI | Z (p) | I2 (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||||||
| Country | Asia | 12 | 1, 2, 3,4, 5, 10, 16, 17, 18, 19, 20, 22 | 1111 | −0.44 | −0.75 | −0.12 | −2.73 (0.006) | 83.5 |
| The others * | 10 | 6, 7, 8, 9, 11, 12, 13, 14, 15, 23 | 1484 | −0.68 | −1.12 | −0.24 | −3.03 (0.002) | 93.3 | |
| Center | One | 13 | 1, 2, 3, 4, 5, 7, 11, 12, 16, 17, 19, 20, 22 | 1208 | −0.61 | −1.06 | −0.16 | −2.63 (0.008) | 92.5 |
| Multi center * | 9 | 6, 8, 9, 10, 13, 14, 15, 18, 23 | 1387 | −0.47 | −0.75 | −0.19 | −3.25 (0.001) | 83.2 | |
| Fund | No | 15 | 1, 2, 3, 5, 7, 8, 10, 12, 13, 14, 17, 18, 20, 22, 23 | 1949 | −0.58 | −0.66 | −0.50 | −14.70 (<0.001) | 79.4 |
| Yes * | 7 | 4, 6, 9, 11, 15, 16, 19 | 646 | −0.60 | −1.10 | −0.11 | −2.39 (0.017) | 89.4 | |
| Participants | T1DM | 2 | 6, 10 | 145 | −1.31 | −2.96 | 0.34 | −1.56 (0.119) | 94.9 |
| T2DM * | 17 | 1, 2, 3, 4, 5, 7, 8, 9, 13, 14, 15, 16, 17, 18, 19, 20, 22 | 2174 | −0.47 | −0.76 | −0.18 | −3.19 (0.001) | 90.2 | |
| Both | 3 | 11, 12, 23 | 276 | −0.52 | −1.03 | −0.02 | −2.03 (0.043) | 74.5 | |
| Number of participants | <50 | 5 | 1, 2, 12, 13, 17 | 458 | −0.49 | −1.03 | 0.06 | −1.76 (0.079) | 81.8 |
| ≥50 * | 17 | 3, 4, 5, 6, 7, 8, 9, 10, 11, 14, 15, 16, 18, 19, 20, 22, 23 | 2137 | −0.57 | −0.87 | −0.26 | −3.66 (<.001) | 91.0 | |
| Research design | RCT * | 11 | 1, 6, 7, 8, 9, 12, 15, 19, 20, 22, 23 | 1528 | −0.80 | −1.26 | −0.35 | −3.47 (0.001) | 93.8 |
| Quasi-E | 11 | 2, 3, 4, 5, 10, 11, 13, 14, 16, 17, 18 | 1067 | −0.24 | −0.42 | −0.06 | −2.58 (0.010) | 49.7 | |
| Type of intervention | Nurse case management | 3 | 8, 9, 23 | 817 | −0.25 | −0.47 | −0.03 | −2.22 (0.026) | 47.3 |
| Home visiting | 4 | 1, 10, 18, 22 | 316 | −0.61 | −1.05 | −0.18 | −2.75 (0.006) | 69.3 | |
| Customized nursing * | 7 | 4, 5, 7, 11, 12, 15, 19 | 758 | −0.65 | −1.28 | −0.02 | −2.01 (0.044) | 94.2 | |
| Education | 5 | 2, 3, 13, 14, 17 | 524 | −0.23 | −0.56 | 0.10 | −1.34 (0.180) | 62.5 | |
| The others | 3 | 6, 16, 20 | 180 | −0.96 | −2.15 | 0.23 | −1.58 (0.114) | 92.6 | |
| Period of intervention | <12 weeks | 6 | 1, 2, 4, 6, 10, 22 | 331 | −0.83 | −1.47 | −0.19 | −2.56 (0.011) | 86.6 |
| ≥12 weeks | 16 | 3, 5, 7, 8, 9, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 23 | 2.264 | −0.46 | −0.75 | −0.18 | −3.16 (0.002) | 90.5 | |
| Intervention session | Not mentioned | 5 | 8, 16, 19, 20, 23 | 919 | −0.53 | −1.02 | −0.03 | −2.09 (0.037) | 89.7 |
| <6 | 7 | 2, 4, 5, 10, 14, 18, 22 | 598 | −0.43 | −0.74 | −0.13 | −2.78 (0.005) | 68.7 | |
| ≥6 * | 10 | 1, 3, 6, 7, 9, 11, 12, 13, 15, 17 | 1078 | −0.63 | −1.14 | −0.11 | −2.39 (0.017) | 93.7 | |
| Operating time per session | Not mentioned | 7 | 1, 8, 10, 11, 16, 19, 23 | 1061 | −0.45 | −0.82 | −0.08 | −2.41 (0.016) | 85.1 |
| <60 | 5 | 4, 12, 14, 18, 22 | 412 | −0.67 | −1.09 | −0.24 | −3.04 (0.002) | 76.0 | |
| ≥60 * | 10 | 2, 3, 5, 6, 7, 9, 13, 15, 17, 20 | 1122 | −0.56 | −1.06 | −0.06 | −2.20 (0.028) | 93.7 | |
| Measurement of post test | Immediately * | 21 | 1, 2, 3, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 22, 23 | 2535 | −0.57 | −0.84 | −0.30 | −4.11 (<.001) | 90.4 |
| With delay | 1 | 4 | 60 | −0.21 | −0.72 | 0.29 | −0.83 (0.406) | - | |
| Quality score | <7 | 5 | 1, 13, 16, 17, 19 | 547 | −0.55 | −1.24 | 0.15 | −1.54 (0.123) | 91.8 |
| ≥7 * | 17 | 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 14, 15, 18, 20, 22, 23 | 2048 | −0.56 | −0.85 | −0.26 | −3.68 (<0.001) | 90.0 | |
| Moderators | Subgroup | Coefficients | SE | Z | p |
|---|---|---|---|---|---|
| Country | −0.13 | 0.08 | −1.58 | 0.115 | |
| Center | 0.18 | 0.08 | 2.23 | 0.026 | |
| Fund | −0.23 | 0.09 | −2.45 | 0.014 | |
| Participants | −0.80 | 0.19 | −4.20 | <0.001 | |
| Number of participants | −0.29 | 0.10 | −2.76 | 0.006 | |
| Research design | −0.38 | 0.08 | −4.64 | <0.001 | |
| Type of intervention | Nurse case management | 0.30 | 0.09 | 3.44 | <0.001 |
| Home visiting | −0.20 | 0.12 | −1.62 | 0.106 | |
| Customized nursing * | −0.39 | 0.09 | −4.36 | <0.001 | |
| Education | 0.40 | 0.10 | 4.01 | <0.001 | |
| Period of intervention | 0.45 | 0.13 | 3.57 | <0.001 | |
| Intervention session | −0.13 | 0.08 | −1.61 | 0.108 | |
| Session operating time | −0.03 | 0.08 | −0.38 | 0.704 | |
| Measurement of post test | −0.18 | 0.26 | −0.69 | 0.492 | |
| Quality score | −0.09 | 0.10 | −0.86 | 0.391 |
| Variables | K | N | Overall ES | 95% CI | Z (p) | I2 (%) | ||
|---|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | |||||||
| Self-care related variables | Self-care | 10 | 783 | 1.13 | 0.48 | 1.78 | 3.42 (0.001) | 94.2 |
| Self-efficacy | 4 | 193 | 0.90 | 0.08 | 1.73 | 2.15 (0.031) | 85.7 | |
| Physiologic variables | FBS | 6 | 511 | −0.86 | −1.47 | −0.26 | −2.82 (0.005) | 90.0 |
| Cholesterol | 4 | 357 | 4.09 | 1.82 | 6.37 | 3.53 (<0.001) | 98.6 | |
| HDL | 5 | 537 | −0.09 | −0.25 | 0.08 | −1.01 (0.311) | 0.0 | |
| LDL | 6 | 1086 | 0.16 | −0.02 | 0.34 | 1.70 (0.090) | 42.7 | |
| SBP | 6 | 761 | −0.21 | −0.51 | 0.08 | −1.41 (0.157) | 75.5 | |
| DBP | 6 | 761 | −0.04 | −0.29 | 0.20 | −0.34 (0.734) | 65.6 | |
| BMI | 4 | 472 | −0.64 | −1.22 | −0.07 | −2.19 (0.029) | 81.1 | |
| Waist circumference | 2 | 175 | 0.33 | 0.05 | 0.61 | 2.31 (0.021) | 0.0 | |
| Psychological variables | DRED | 2 | 194 | −0.60 | −0.89 | −0.31 | −4.07 (<0.001) | 0.0 |
| QOL | 4 | 306 | 0.56 | −1.42 | 2.55 | 0.56 (0.577) | 98.1 | |
| Anxiety | 2 | 200 | −1.45 | −3.32 | 0.41 | −1.52 (0.127) | 96.9 | |
| Depression | 2 | 200 | −2.11 | −5.27 | 1.05 | −1.31 (0.191) | 98.6 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, M.-K.; Kim, M.Y. Self-Management Nursing Intervention for Controlling Glucose among Diabetes: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 12750. https://doi.org/10.3390/ijerph182312750
Cho M-K, Kim MY. Self-Management Nursing Intervention for Controlling Glucose among Diabetes: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(23):12750. https://doi.org/10.3390/ijerph182312750
Chicago/Turabian StyleCho, Mi-Kyoung, and Mi Young Kim. 2021. "Self-Management Nursing Intervention for Controlling Glucose among Diabetes: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 23: 12750. https://doi.org/10.3390/ijerph182312750
APA StyleCho, M.-K., & Kim, M. Y. (2021). Self-Management Nursing Intervention for Controlling Glucose among Diabetes: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(23), 12750. https://doi.org/10.3390/ijerph182312750






