Pet Ownership and Multiple Sclerosis during COVID-19
Abstract
1. Introduction
1.1. Objectives
- To explore the rates of pet ownership and associations with quality of life, satisfaction with social roles, and self-efficacy scores in PwMS.
- To compare the levels of attachment to pets in PwMS and people without MS.
- To compare the levels of satisfaction with social roles in pet-owning and non-pet-owning PwMS and people without MS.
- To explore the effects of the COVID-19 outbreak on people’s perceived relationships with their pets (how the participants thought their pets helped them emotionally and physically and whether they had any concerns about being a pet owner during the COVID-19 pandemic).
1.2. Hypotheses:
- Pet ownership is associated with higher rates of quality of life, self-efficacy, and satisfaction with social roles in PwMS.
- Pet attachment may be higher in PwMS than in controls.
- Satisfaction with social roles may be higher in pet-owning than non-pet-owning PwMS and controls.
- Objective 4 is exploratory; no specific hypothesis generated.
2. Materials and Methods
2.1. Study Design
2.2. Population
- Aged 18 years or over.
- Diagnosis of MS AND on the Nottingham MS Register.
- Inability or unwillingness to complete the questionnaire.
- Aged 18 years or over.
- Friend or non-blood relative of person with MS diagnosis.
- Not diagnosed with MS.
- Inability or unwillingness to complete questionnaire.
2.3. Questionnaire
2.4. Demographic Data
2.5. Pet Ownership
2.6. Data Processing
2.7. Statistical Analysis
3. Results
3.1. Demographics
3.2. Pet Ownership
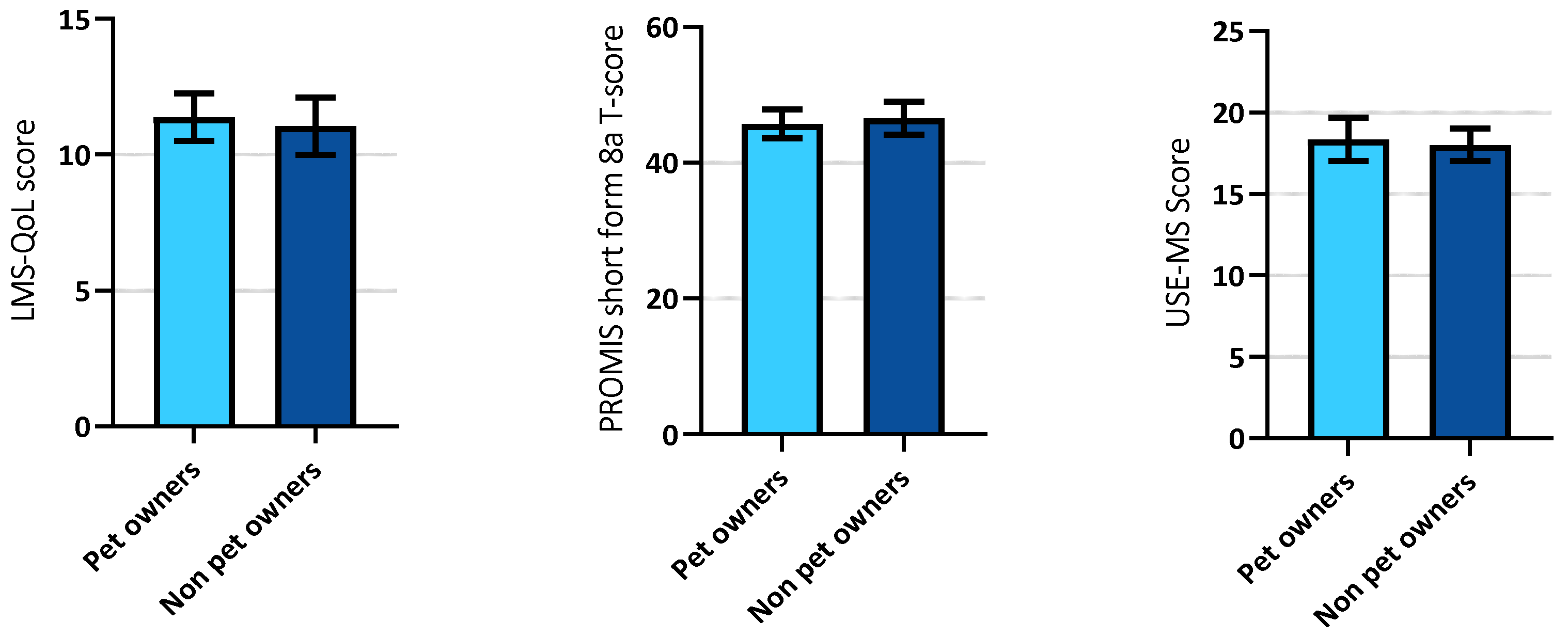
3.2.1. Pet Ownership and Multiple Sclerosis–Associations with Quality of Life, Satisfaction with Social Roles, and Self-Efficacy
3.2.2. Pet Attachment
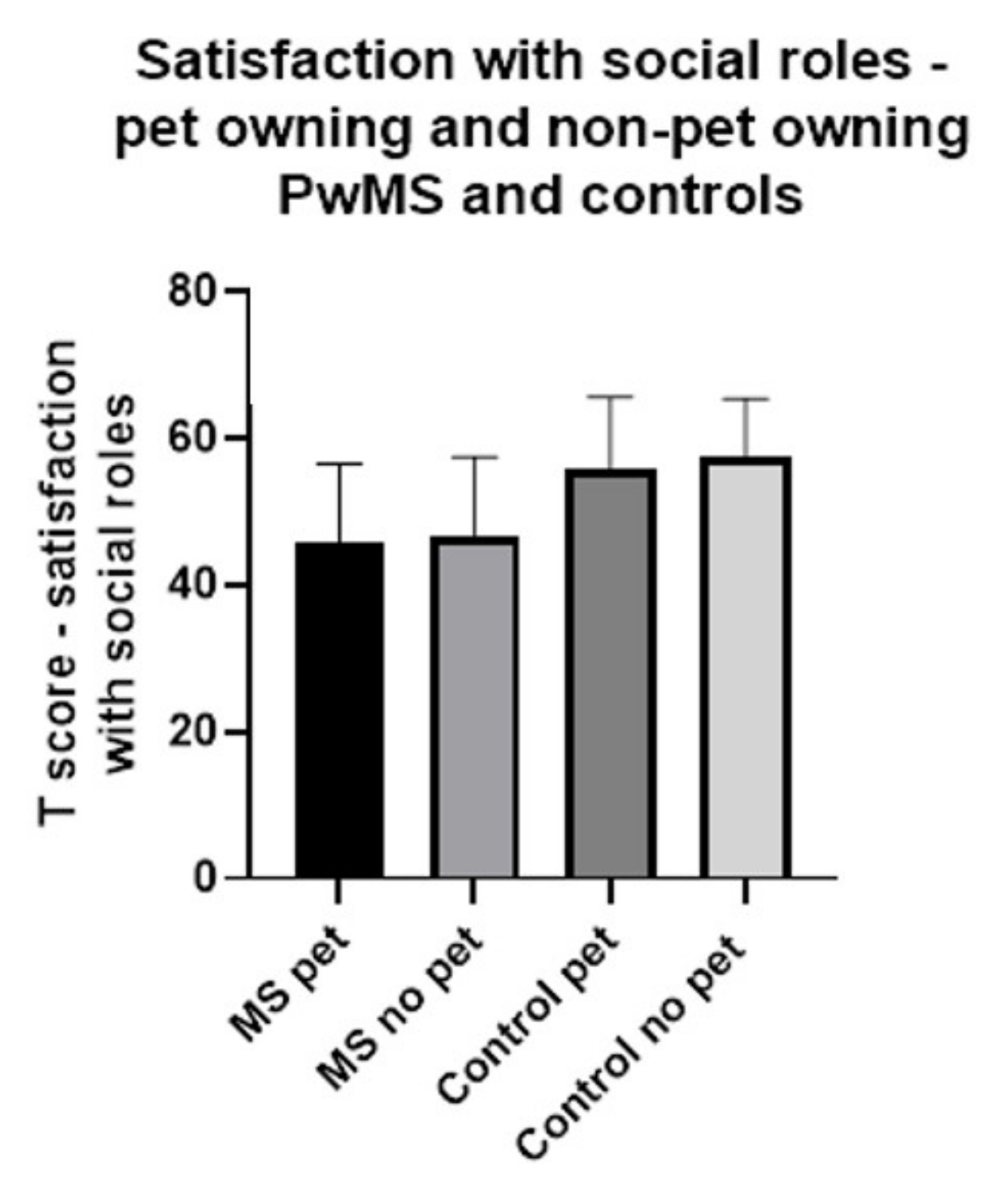
3.2.3. Satisfaction with Social Roles in Pet-Owning and Non-Pet-Owning PwMS and Controls
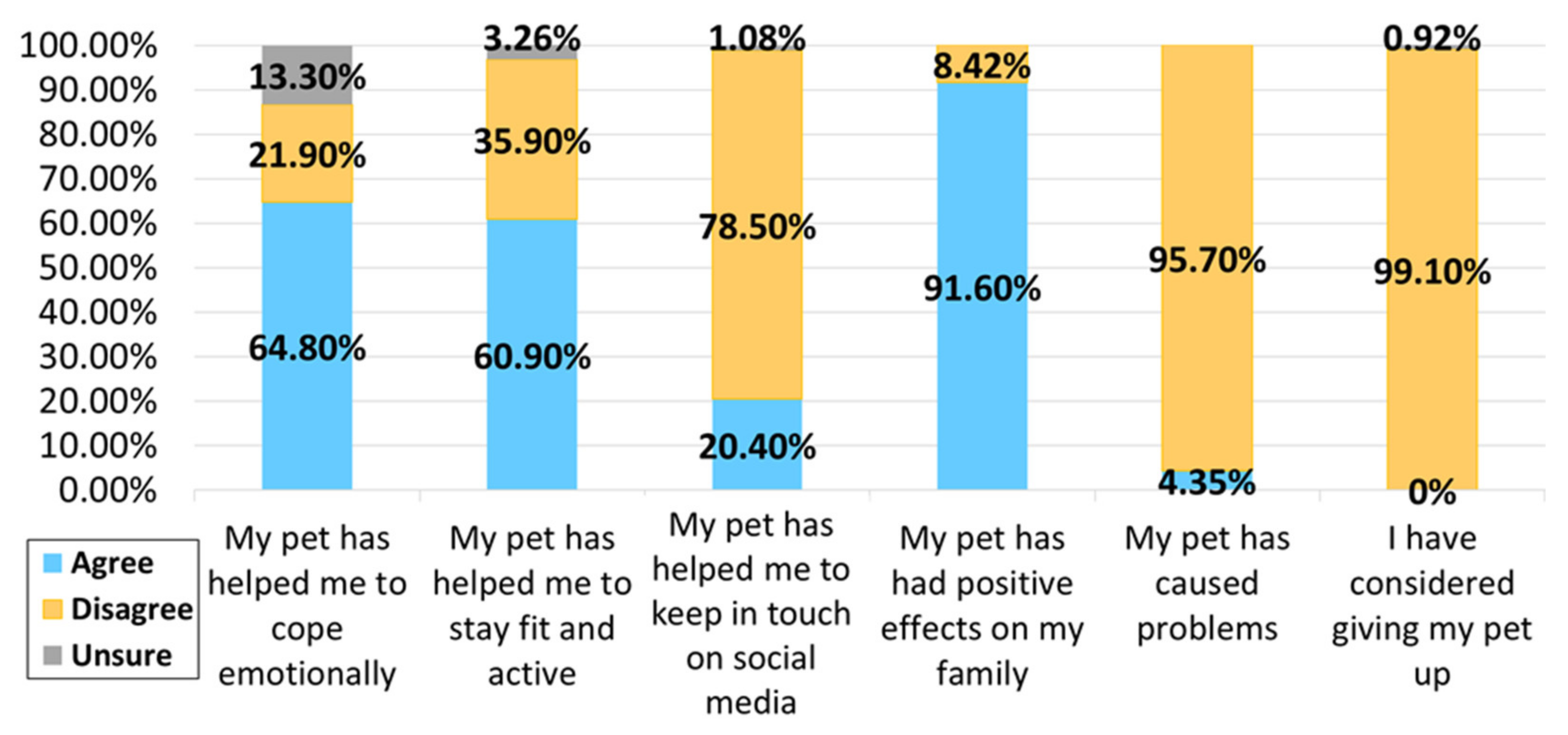
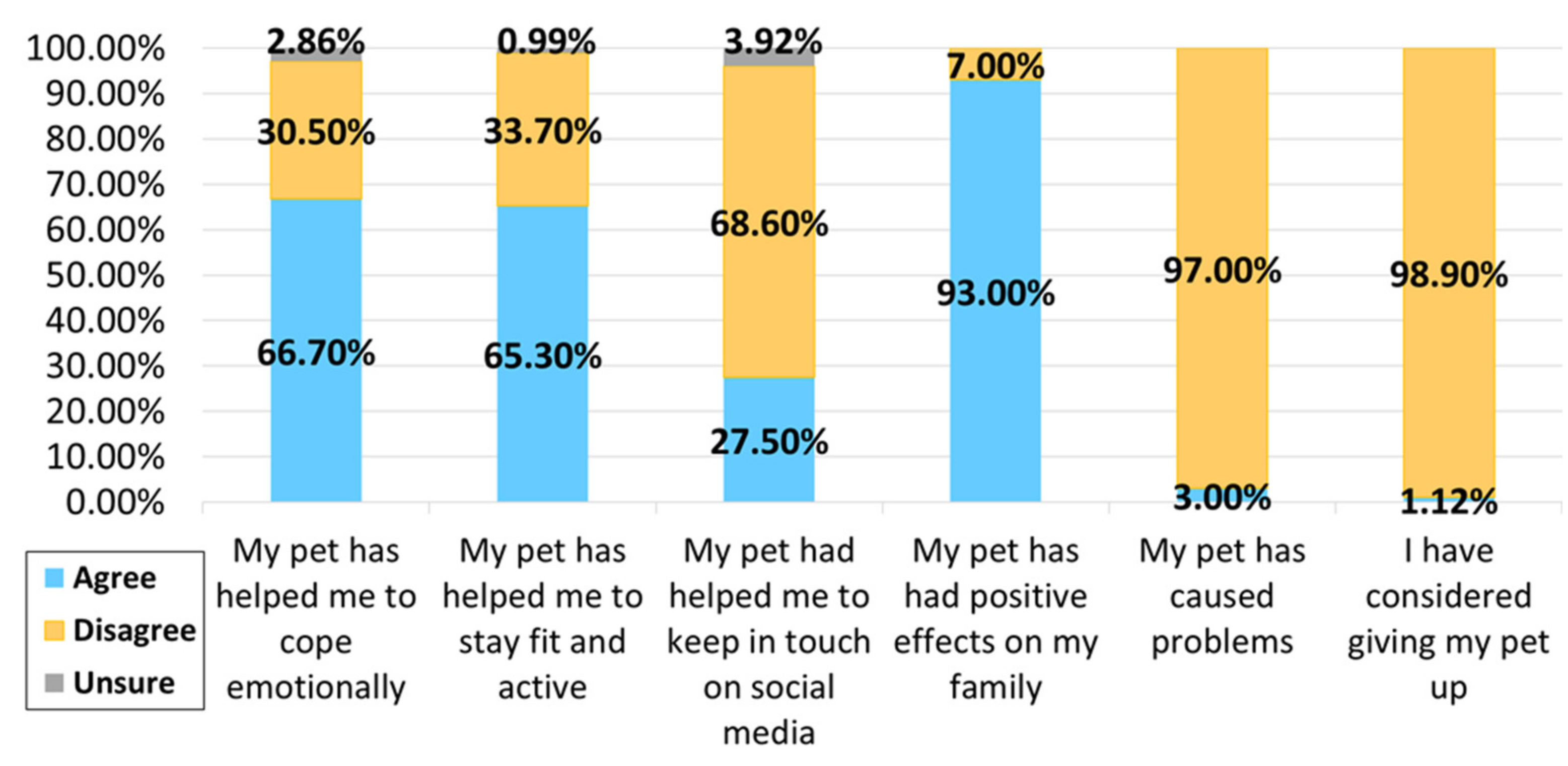
3.3. Pet Ownership during the COVID-19 Pandemic
Pet Ownership-Related Concerns during the COVID-19 Pandemic
4. Discussion
4.1. Findings
Objectives and Hypotheses
- 1.
- To explore the rates of pet ownership and associations with quality of life, satisfaction with social roles, and self-efficacy scores in PwMS/pet ownership is associated with higher rates of quality of life, self-efficacy, and satisfaction with social roles in PwMS
- MS was associated with a reduction in satisfaction with social roles.
- Employment was associated with increased satisfaction with social roles.
- Employment was associated with improved quality of life.
- Employment was associated with increased self-efficacy.
- Pet ownership was associated with a reduction in satisfaction with social roles.
- 2.
- To compare the levels of attachment to pets in PwMS and people without MS/pet attachment may be higher in PwMS than in controls.
- 3.
- To compare levels of satisfaction with social roles in pet-owning and non-pet-owning PwMS and people without MS/satisfaction with social roles may be higher in pet-owning than non-pet-owning PwMS and controls
- 4.
- To explore the effects of the COVID-19 outbreak on people’s perceived relationships with their pets (how the participants thought their pets helped them emotionally and physically and whether they had any concerns about being a pet owner during the COVID-19 pandemic)/no matched hypothesis.
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Rommer, P.S.; Eichstädt, K.; Ellenberger, D.; Flachenecker, P.; Friede, T.; Haas, J.; Kleinschnitz, C.; Pöhlau, D.; Rienhoff, O.; Stahmann, A.; et al. Symptomatology and symptomatic treatment in multiple sclerosis: Results from a nationwide MS registry. Mult. Scler. J. 2019, 25, 1641–1652. [Google Scholar] [CrossRef] [PubMed]
- Motl, R.W.; Snook, E.M.; McAuley, E.; Gliottoni, R.C. Symptoms, self-efficacy, and physical activity among individuals with multiple sclerosis. Res. Nurs. Health 2006, 29, 597–606. [Google Scholar] [CrossRef]
- Compston, A.; Coles, A. Multiple sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef]
- Barin, L.; Salmen, A.; Disanto, G.; Babačić, H.; Calabrese, P.; Chan, A.; Kamm, C.P.; Kesselring, J.; Kuhle, J.; Gobbi, C.; et al. The disease burden of Multiple Sclerosis from the individual and population perspective: Which symptoms matter most? Mult. Scler. Relat. Disord. 2018, 25, 112–121. [Google Scholar] [CrossRef]
- Janardhan, V.; Bakshi, R. Quality of life and its relationship to brain lesions and atrophy on magnetic resonance images in 60 patients with multiple sclerosis. Arch. Neurol. 2000, 57, 1485–1491. [Google Scholar] [CrossRef]
- Hermann, B.P.; Vickrey, B.; Hays, R.D.; Cramer, J.; Devinsky, O.; Meador, K.; Perrine, K.; Myers, L.W.; Ellison, G.W. A comparison of health-related quality of life in patients with epilepsy, diabetes and multiple sclerosis. Epilepsy Res. 1996, 25, 113–118. [Google Scholar] [CrossRef]
- Murphy, R.; O’Donoghue, S.; Counihan, T.; McDonald, C.; Calabresi, P.; Ahmed, M.A.; Kaplin, A.; Hallahan, B. Neuropsychiatric syndromes of multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2017, 88, 697–708. [Google Scholar] [CrossRef] [PubMed]
- Kwiatkowski, A.; Marissal, J.-P.; Pouyfaucon, M.; Vermersch, P.; Hautecoeur, P.; Dervaux, B. Social participation in patients with multiple sclerosis: Correlations between disability and economic burden. BMC Neurol. 2014, 14, 115. [Google Scholar] [CrossRef]
- Allen, K.; Blascovich, J.; Mendes, W.B. Cardiovascular Reactivity and the Presence of Pets, Friends, and Spouses: The Truth About Cats and Dogs. Psychosom. Med. 2002, 64, 727–739. [Google Scholar] [CrossRef] [PubMed]
- Irani, S.; Mahler, C.; Goetzmann, L.; Russi, E.; Boehler, A. Lung Transplant Recipients Holding Companion Animals: Impact on Physical Health and Quality of Life. Arab. Archaeol. Epigr. 2006, 6, 404–411. [Google Scholar] [CrossRef]
- Brooks, H.; Rushton, K.; Walker, S.; Lovell, K.; Rogers, A. Ontological security and connectivity provided by pets: A study in the self-management of the everyday lives of people diagnosed with a long-term mental health condition. BMC Psychiatry 2016, 16, 409. [Google Scholar] [CrossRef]
- Brooks, H.L.; Rogers, A.; Kapadia, D.; Pilgrim, J.; Reeves, D.; Vassilev, I. Creature comforts: Personal communities, pets and the work of managing a long-term condition. Chronic Illn. 2012, 9, 87–102. [Google Scholar] [CrossRef][Green Version]
- Wisdom, J.P.; Saedi, G.A.; Green, C.A. Another breed of “service” animals: STARS study findings about pet ownership and recovery from serious mental illness. Am. J. Orthopsychiatry 2009, 79, 430–436. [Google Scholar] [CrossRef]
- Wells, D.L. Associations Between Pet Ownership and Self-Reported Health Status in People Suffering from Chronic Fatigue Syndrome. J. Altern. Complement. Med. 2009, 15, 407–413. [Google Scholar] [CrossRef]
- Ryan, S.; Ziebland, S. On interviewing people with pets: Reflections from qualitative research on people with long-term conditions. Sociol. Health Illn. 2015, 37, 67–80. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Bonsaken, T.; Lerdal, A.; Fagermoan, M.S. Factors associated with self-efficacy in persons with chronic illness. Scand. J. Psychol. 2012, 53, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Jongen, P.J.; Heerings, M.; Ruimschotel, R.; Hussaarts, A.; Duyverman, L.; Van Der Zande, A.; Valkenburg-Vissers, J.; Van Droffelaar, M.; Lemmens, W.; Donders, R.; et al. Intensive social cognitive treatment (can do treatment) with participation of support partners in persons with relapsing remitting multiple sclerosis: Observation of improved self-efficacy, quality of life, anxiety and depression 1 year later. BMC Res. Notes 2016, 9, 375. [Google Scholar] [CrossRef]
- Jongen, P.J.; Ruimschotel, R.; Heerings, M.; Hussaarts, A.; Duyverman, L.; Van Der Zande, A.; Valkenburg-Vissers, J.; Wolper, H.; Van Droffelaar, M.; Lemmens, W.; et al. Improved self-efficacy in persons with relapsing remitting multiple sclerosis after an intensive social cognitive wellness program with participation of support partners: A 6-months observational study. Health Qual. Life Outcomes 2014, 12, 40. [Google Scholar] [CrossRef]
- De Guzman, A.B.; Cucueco, D.S.; Cuenco, I.B.V.; Cunanan, N.G.C.; Dabandan, R.T.; Dacanay, E.J.E. Petmanship: Understanding Elderly Filipinos’ Self-Perceived Health and Self-Esteem Captured from their Lived Experiences with Pet Companions. Educ. Gerontol. 2009, 35, 963–989. [Google Scholar] [CrossRef]
- Battalio, S.L.; Jensen, M.P.; Molton, I.R. Secondary health conditions and social role satisfaction in adults with long-term physical disability. Health Psychol. 2019, 38, 445–454. [Google Scholar] [CrossRef]
- Amtmann, D.; Bamer, A.M.; Kim, J.; Chung, H.; Salem, R. People with multiple sclerosis report significantly worse symptoms and health related quality of life than the US general population as measured by PROMIS and NeuroQoL outcome measures. Disabil. Health J. 2018, 11, 99–107. [Google Scholar] [CrossRef]
- Sturgeon, J.A.; Dixon, E.A.; Darnall, B.D.; Mackey, S.C. Contributions of physical function and satisfaction with social roles to emotional distress in chronic pain: A Collaborative Health Outcomes Information Registry (CHOIR) study. Pain 2015, 156, 2627–2633. [Google Scholar] [CrossRef]
- Krause-Parello, C.A. Pet Ownership and Older Women: The Relationships Among Loneliness, Pet Attachment Support, Human Social Support, and Depressed Mood. Geriatr. Nurs. 2012, 33, 194–203. [Google Scholar] [CrossRef]
- Jia, R.; Ayling, K.; Chalder, T.; Massey, A.; Broadbent, E.; Coupland, C.; Vedhara, K. Mental health in the UK during the COVID-19 pandemic: Cross-sectional analyses from a community cohort study. BMJ Open 2020, 10, e040620. [Google Scholar] [CrossRef] [PubMed]
- Costabile, T.; Carotenuto, A.; Lavorgna, L.; Borriello, G.; Moiola, L.; Inglese, M.; Petruzzo, M.; Trojsi, F.; Ianniello, A.; Nozzolillo, A.; et al. COVID-19 pandemic and mental distress in multiple sclerosis: Implications for clinical management. Eur. J. Neurol. 2021, 28, 3375–3383. [Google Scholar] [CrossRef] [PubMed]
- Motolese, F.; Rossi, M.; Albergo, G.; Stelitano, D.; Villanova, M.; Di Lazzaro, V.; Capone, F. The Psychological Impact of COVID-19 Pandemic on People with Multiple Sclerosis. Front. Neurol. 2020, 11, 580507. [Google Scholar] [CrossRef]
- Shaygannejad, V.; Afshari-Safavi, A.; Hatef, B. Assessment of mental health, knowledge, and attitude of patients with multiple sclerosis and neuromyelitis optica spectrum disorder in response to 2019 novel coronavirus. Neurol. Sci. 2020, 42, 2891–2901. [Google Scholar] [CrossRef]
- Ratschen, E.; Shoesmith, E.; Shahab, L.; Silva, K.; Kale, D.; Toner, P.; Reeve, C.; Mills, D.S. Human-animal relationships and interactions during the Covid-19 lockdown phase in the UK: Investigating links with mental health and loneliness. PLoS ONE 2020, 15, e0239397. [Google Scholar] [CrossRef]
- Applebaum, J.W.; Tomlinson, C.A.; Matijczak, A.; McDonald, S.E.; Zsembik, B.A. The Concerns, Difficulties, and Stressors of Caring for Pets during COVID-19: Results from a Large Survey of U.S. Pet Owners. Animals 2020, 10, 1882. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.P.; Garrity, T.F.; Stallones, L. Psychometric Evaluation of the Lexington Attachment to Pets Scale (Laps). Anthrozoös 1992, 5, 160–175. [Google Scholar] [CrossRef]
- Cella, D.; Choi, S.W.; Condon, D.M.; Schalet, B.; Hays, R.D.; Rothrock, N.E.; Yount, S.; Cook, K.F.; Gershon, R.C.; Amtmann, D.; et al. PROMIS® Adult Health Profiles: Efficient Short-Form Measures of Seven Health Domains. Value Health 2019, 22, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Segawa, E.; Schalet, B.; Cella, D. A comparison of computer adaptive tests (CATs) and short forms in terms of accuracy and number of items administrated using PROMIS profile. Qual. Life Res. 2020, 29, 213–221. [Google Scholar] [CrossRef]
- Ford, H.L.; Gerry, E.; Tennant, A.; Whalley, D.; Haigh, R.; Johnson, M.H. Developing a disease-specific quality of life measure for people with multiple sclerosis. Clin. Rehabil. 2001, 15, 247–258. [Google Scholar] [CrossRef]
- Nagaraj, K.; Taly, A.B.; Gupta, A.; Prasad, C.; Christopher, R. Prevalence of fatigue in patients with multiple sclerosis and its effect on the quality of life. J. Neurosci. Rural. Pract. 2013, 04, 278–282. [Google Scholar] [CrossRef]
- Ensari, I.; Motl, R.W.; McAuley, E. Structural and construct validity of the Leeds Multiple Sclerosis Quality of Life scale. Qual. Life Res. 2015, 25, 1605–1611. [Google Scholar] [CrossRef]
- Young, C.; Mills, R.; Woolmore, J.; Hawkins, C.; Tennant, A.; Young, C. The unidimensional self-efficacy scale for MS (USE-MS): Developing a patient based and patient reported outcome. Mult. Scler. J. 2012, 18, 1326–1333. [Google Scholar] [CrossRef] [PubMed]
- Modini, M.; Joyce, S.; Mykletun, A.; Christensen, H.; Bryant, R.A.; Mitchell, P.B.; Harvey, S.B. The mental health benefits of employment: Results of a systematic meta-review. Australas. Psychiatry 2016, 24, 331–336. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhou, Z.; Fan, X.; Nawaz, R.; Zhao, D.; Xu, T.; Su, M.; Cao, D.; Shen, C.; Lai, S. Comparison of inequity in health-related quality of life among unemployed and employed individuals in China. BMC Public Health 2021, 21, 52. [Google Scholar] [CrossRef]
- Le Roux, M.C.; Wright, S. The Relationship Between Pet Attachment, Life Satisfaction, and Perceived Stress: Results from a South African Online Survey. Anthrozoös 2020, 33, 371–385. [Google Scholar] [CrossRef]
- Dinis, F.A.; Martins, T.L.F. Does cat attachment have an effect on human health? A comparison between owners and volunteers. Pet Behav. Sci. 2016, 1, 1–12. [Google Scholar] [CrossRef][Green Version]
- Joseph, N.; Chandramohan, A.K.; D’Souza, A.L.; Basavanna, S.C.; Hariram, S.; Nayak, A.H. Assessment of pet attachment and its relationship with stress and social support among residents in Mangalore city of south India. J. Vet. Behav. 2019, 34, 1–6. [Google Scholar] [CrossRef]
- Smolkovic, I.; Fajfar, M.; Mlinaric, V. Attachment to pets and interpersonal relationships: Can a four-legged friend replace a two-legged one? J. Eur. Psychol. Stud. 2012, 3, 15. [Google Scholar] [CrossRef]
- Mein, G.; Grant, R. A cross-sectional exploratory analysis between pet ownership, sleep, exercise, health and neighbourhood perceptions: The Whitehall II cohort study. BMC Geriatr. 2018, 18, 176. [Google Scholar] [CrossRef]
- Oliva, J.L.; Johnston, K.L. Puppy love in the time of Corona: Dog ownership protects against loneliness for those living alone during the COVID-19 lockdown. Int. J. Soc. Psychiatry 2020, 67, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Boeschoten, R.E.; Braamse, A.M.; Beekman, A.T.; Cuijpers, P.; van Oppen, P.; Dekker, J.; Uitdehaag, B.M. Prevalence of depression and anxiety in Multiple Sclerosis: A systematic review and meta-analysis. J. Neurol. Sci. 2017, 372, 331–341. [Google Scholar] [CrossRef]
- Prime, H.; Wade, M.; Browne, D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020, 75, 631–643. [Google Scholar] [CrossRef] [PubMed]
- Owczarczak-Garstecka, S.; Graham, T.; Archer, D.; Westgarth, C. Dog Walking before and during the COVID-19 Pandemic Lockdown: Experiences of UK Dog Owners. Int. J. Environ. Res. Public Health 2021, 18, 6315. [Google Scholar] [CrossRef]
- Gasteiger, N.; Vedhara, K.; Massey, A.; Jia, R.; Ayling, K.; Chalder, T.; Coupland, C.; Broadbent, E. Depression, anxiety and stress during the COVID-19 pandemic: Results from a New Zealand cohort study on mental well-being. BMJ Open 2021, 11, e045325. [Google Scholar] [CrossRef]
- Burholt, V.; Windle, G.; Morgan, D.J. Cfas Wales on behalf of the CFAS Wales team A Social Model of Loneliness: The Roles of Disability, Social Resources, and Cognitive Impairment. Gerontologist 2016, 57, 1020–1030. [Google Scholar] [CrossRef]
- Freeman, J.; Gorst, T.; Gunn, H.; Robens, S. “A non-person to the rest of the world”: Experiences of social isolation amongst severely impaired people with multiple sclerosis. Disabil. Rehabil. 2020, 42, 2295–2303. [Google Scholar] [CrossRef] [PubMed]
- Beal, C.C.; Stuifbergen, A. Loneliness in Women with Multiple Sclerosis. Rehabil. Nurs. 2007, 32, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.; Hussain, S.; Sparagano, O. Did the COVID-19 Pandemic Spark a Public Interest in Pet Adoption? Front. Vet. Sci. 2021, 8, 647308. [Google Scholar] [CrossRef] [PubMed]
- Phillipou, A.; Tan, E.; Toh, W.; Van Rheenen, T.; Meyer, D.; Neill, E.; Sumner, P.; Rossell, S. Pet ownership and mental health during COVID -19 lockdown. Aust. Vet. J. 2021, 99, 423–426. [Google Scholar] [CrossRef] [PubMed]
- Radulovic, L.; Erakovic, J.; Roganovic, M. Attitudes of patients with relapsing-remitting form of multiple sclerosis using disease-modifying drugs in Montenegro regarding COVID-19 pandemic. Mult. Scler. Relat. Disord. 2020, 45, 102380. [Google Scholar] [CrossRef] [PubMed]
- Kalron, A.; Dolev, M.; Greenberg-Abrahami, M.; Menascu, S.; Frid, L.; Avrech-Shezifi, S.; Harari, G.; Magalashvili, D.; Achiron, A. Physical activity behavior in people with multiple sclerosis during the COVID-19 pandemic in Israel: Results of an online survey. Mult. Scler. Relat. Disord. 2021, 47, 102603. [Google Scholar] [CrossRef]
- Applebaum, J.W.; Adams, B.L.; Eliasson, M.N.; Zsembik, B.A.; McDonald, S.E. How pets factor into healthcare deci-sions for COVID-19: A One Health perspective. One Health 2020, 11, 100176. [Google Scholar] [CrossRef]
- Brooks, H.L.; Rushton, K.; Lovell, K.; Bee, P.; Walker, L.; Grant, L.; Rogers, A. The power of support from companion animals for people living with mental health problems: A systematic review and narrative synthesis of the evidence. BMC Psychiatry 2018, 18, 31. [Google Scholar] [CrossRef]
- Uccelli, M.M. The impact of multiple sclerosis on family members: A review of the literature. Neurodegener. Dis. Manag. 2014, 4, 177–185. [Google Scholar] [CrossRef]
- Nakash, R.A.; Hutton, J.L.; Jørstad-Stein, E.C.; Gates, S.; Lamb, S. Maximising response to postal questionnaires—A systematic review of randomised trials in health research. BMC Med Res. Methodol. 2006, 6, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.; Roberts, I.; Clarke, M.; DiGuiseppi, C.; Pratap, S.; Wentz, R.; Kwan, I. Increasing response rates to postal questionnaires: Systematic review. BMJ 2002, 324, 1183. [Google Scholar] [CrossRef] [PubMed]
- Powell, L.; Edwards, K.M.; McGreevy, P.; Bauman, A.; Podberscek, A.; Neilly, B.; Sherrington, C.; Stamatakis, E. Companion dog acquisition and mental well-being: A community-based three-arm controlled study. BMC Public Health 2019, 19, 1428. [Google Scholar] [CrossRef] [PubMed]
| Pet-Owning PwMS | Non-Pet-Owning Pwms | Pet-Owning Controls | Non-Pet-Owning Controls | |
|---|---|---|---|---|
| Age, gender, employment status | ✓ | ✓ | ✓ | ✓ |
| MS subtype | ✓ | ✓ | ||
| Pet ownership (yes/no) | ✓ | ✓ | ✓ | ✓ |
| Details of current pets (type and number) | ✓ | ✓ | ||
| Attachment to pets (LAPS) | ✓ | ✓ | ||
| Satisfaction with social roles (SPSR) | ✓ | ✓ | ✓ | ✓ |
| Quality of life (QoL/LMS-QoL) | ✓ | ✓ | ||
| Self-efficacy (USE-MS) | ✓ | ✓ | ||
| Pets during COVID-19 | ✓ | ✓ |
| PwMS (n = 189) | Control Group (n = 163) | Comparison | |
|---|---|---|---|
| Age (mean, standard deviation), years | 54, 12 | 53, 16 | Difference in means with 95% CI −1 (−4 to +2) |
| Gender male: female: not answered N (%) | 44: 143: 2 (23: 76: 1) | 77: 82: 4 (47: 50: 2) | OR 0.33; 95% CI 0.21–0.52 |
| Multiple sclerosis subtype N (%) PPMS | n/a | n/a | |
| 15 (8) | |||
| PRMS | 5 (3) | ||
| RRMS | 109 (58) | ||
| SPMS | 44 (23) | ||
| Unsure | 11 (6) | ||
| Not answered | 5 (3) | ||
| Employment status N (%) Retired | 41 (22) | 48 (29) | OR and 95% CI: 0.66 (0.40–1.08) |
| Medically retired | 42 (22) | 5 (3) | 9.03 (3.5–21.5) |
| Full time out of the house | 37 (20) | 57 (35) | 0.45 (0.28–0.73) |
| Full time working from home | 11 (6) | 11 (7) | 0.85 (0.34–1.93) |
| Part time out of the house | 25 (13) | 26 (16) | 0.80 (0.44–1.48) |
| Part time working from home | 17 (9) | 5 (3) | 3.1 (1.15–7.86) |
| Unemployed | 14 (7) | 7 (4) | 1.78 (0.70–4.61) |
| Other | 1 (1) | 4 (2) | 0.21 (0.02–1.30) |
| Not answered | 1 (1) | 0 (0) | |
| Pet owner N (%) Yes | 110 (58) | 105 (64) | OR 0.77; 95% CI 0.49–1.12 |
| No | 79 (42) | 58 (36) | |
| Effects of pandemic N (%) Carried on as normal | 29 (15) | 62 (38) | OR and 95% CI: 0.30 (0.18–0.49) |
| Socially distanced but left house regularly | 82 (43) | 77 (47) | 0.86 (0.56–1.30) |
| Isolated at home for less than 7 days | 8 (4) | 4 (2) | 1.76 (0.53–5.32) |
| Isolated at home for 8–14 days | 5 (3) | 4 (2) | 1.08 (0.32–3.57) |
| Isolated at home for more than 14 days | 62 (32) | 16 (10) | 4.49 (2.50–8.10) |
| Not answered | 3 (2) | 0 (0) |
| PwMS–Pet Owners (n = 110) | PwMS–Non-Pet Owners (n = 79) | Comparison (PwMS) | Control Group–Pet Owners (n = 105) | Control Group–Non-Pet Owners (n = 58) | Comparison (Control Group) | |
|---|---|---|---|---|---|---|
| Age mean, SD | 52.0, 11.2 | 56.0, 12.2 | Difference in means with 95% CI 4.0 (0.54–7.36) | 49.6, 13.4 | 57.9, 17.8 | Difference in means with 95% CI 8.3 (3.4–13.2) |
| Gender M: F: not answered N (%) | 23: 85: 2 (21: 77: 2) | 21: 58: 0 (27: 73: 0) | OR 0.75; 95% CI 0.38–1.47 | 46: 56: 3 (44: 53: 3) | 31: 26: 1 (53: 45: 1) | OR 0.69; 95% CI 0.36–1.33 |
| MS subtype N (%) PPMS | 5 (5) | 10 (13) | OR with 95% CI 0.34 (0.12–0.96) | n/a | n/a | n/a |
| PRMS | 4 (4) | 1 (1) | 3.02 (0.48–37.38) | |||
| RRMS | 64 (58) | 45 (57) | 1.17 (0.61–2.03) | |||
| SPMS | 26 (24) | 18 (23) | 1.08 (0.56–2.22) | |||
| Unsure | 7 (6) | 4 (5) | 1.31 (0.40–4.11 |
| Pet-Owning PwMS | Non-Pet-Owning PwMS | Pet-Owning Controls | Non-Pet-Owning Controls | |
|---|---|---|---|---|
| Attachment to pets (LAPS score) mean and 95% CI | 49.0 (46.5–51.6) | n/a | 46.3 (43.4–49.1) | n/a |
| Satisfaction with social roles (SPSR) T score mean and 95% CI | 45.7 (43.6–47.8) | 46.6 (44.1–49.0) | 55.8 (53.9–57.8) | 57.5 (55.5–59.6) |
| Quality of life LMS-QOL mean score with 95% CI | 11.4 (10.5–12.3) | 11.1 (10.0–12.1) | n/a | n/a |
| Self-efficacy USE-MS mean score with 95% CI | 18.4 (17.0–19.7) | 18.2 (16.7–19.6) | n/a | n/a |
| Nature of Concern | % (Number) Respondents in MS Group Reporting Concern (n = 110) | % (Number) Respondents in Control Group Reporting Concern (n = 105) |
|---|---|---|
| Access to veterinary care | 28 (31) | 18 (19) |
| Exercise restrictions | 14 (15) | 8 (8) |
| Access to food and supplies | 11 (12) | 6 (6) |
| Impact of illness | 10 (11) | 12 (13) |
| Financial concerns | 8 (9) | 6 (6) |
| Return to work | 5 (6) | 8 (8) |
| Changes to routine | 4 (4) | 2 (2) |
| COVID infection from pets | 1 (1) | 2 (2) |
| Other | 1 (1) | 1 (1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliver-Hall, H.; Ratschen, E.; Tench, C.R.; Brooks, H.; Constantinescu, C.S.; Edwards, L. Pet Ownership and Multiple Sclerosis during COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 12683. https://doi.org/10.3390/ijerph182312683
Oliver-Hall H, Ratschen E, Tench CR, Brooks H, Constantinescu CS, Edwards L. Pet Ownership and Multiple Sclerosis during COVID-19. International Journal of Environmental Research and Public Health. 2021; 18(23):12683. https://doi.org/10.3390/ijerph182312683
Chicago/Turabian StyleOliver-Hall, Holly, Elena Ratschen, Christopher R. Tench, Helen Brooks, Cris S. Constantinescu, and Laura Edwards. 2021. "Pet Ownership and Multiple Sclerosis during COVID-19" International Journal of Environmental Research and Public Health 18, no. 23: 12683. https://doi.org/10.3390/ijerph182312683
APA StyleOliver-Hall, H., Ratschen, E., Tench, C. R., Brooks, H., Constantinescu, C. S., & Edwards, L. (2021). Pet Ownership and Multiple Sclerosis during COVID-19. International Journal of Environmental Research and Public Health, 18(23), 12683. https://doi.org/10.3390/ijerph182312683







