Population-Based Study on Cancer Incidence in Pharmacist: A Cohort Study in Taiwan
Abstract
:1. Introduction
The Present Study
2. Methods
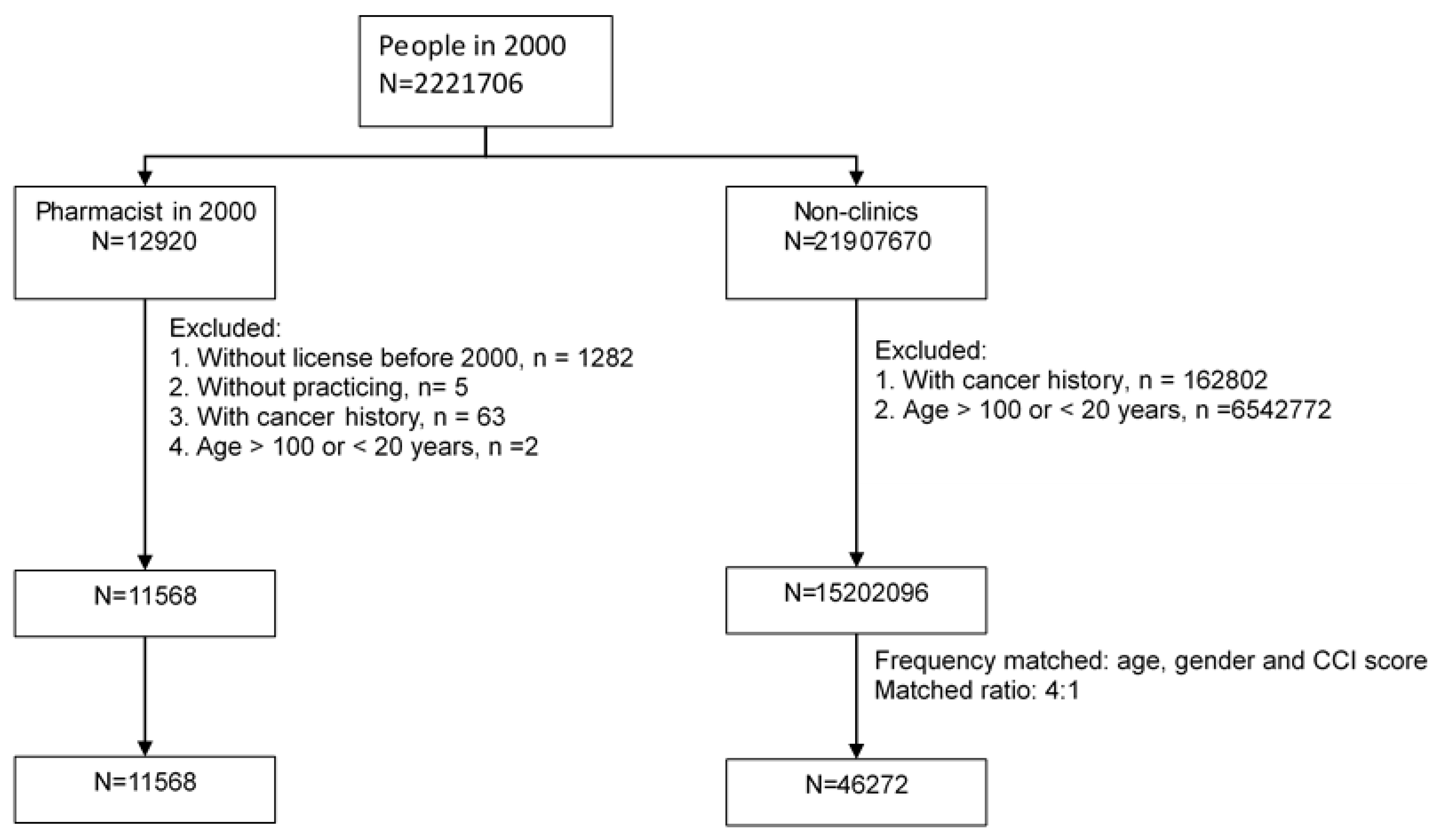
2.1. Study Design
2.2. Data Collection
2.2.1. Data Sources
2.2.2. Outcome Measures and Risk Factor
2.2.3. Study Population
2.2.4. Statistical Analyses
3. Results
3.1. Demographics Characteristics of Study Groups
3.2. Comparison of Cancer Risk between Pharmacists and General Population
3.3. The Association between Cancer Incidence and Pharmacist Characteristics
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Joseph, B.; Joseph, M. The health of the healthcare workers. Indian J. Occup. Environ. Med. 2016, 20, 71–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulutasdemir, N.; Cirpan, M.; Ozturk, E.; Tanir, F. Occupational Risks of Health Professionals in Turkey as an Emerging Economy. Ann. Glob. Health 2015, 81, 522. [Google Scholar] [CrossRef]
- Huei, L.C.; Ya-Wen, L.; Ming, Y.C.; Chen, H.L.; Yi, W.J.; Hung, L.M. Occupational health and safety hazards faced by healthcare professionals in Taiwan: A systematic review of risk factors and control strategies. SAGE Open Med. 2020, 8. [Google Scholar] [CrossRef]
- Lombardo, J.; Roussel, C. Highlighting the Risk of Occupational Exposure to Hazardous Drugs in the Health Care Setting. Pharmacy Times. 15 November 2018. Available online: https://www.pharmacytimes.com/view/highlighting-the-risk-of-occupational-exposure-to-hazardous-drugs-in-the-health-care-setting- (accessed on 17 October 2021).
- Occupational Safety and Health Administration, Ministry of Labor. Work-Related Cancer (Taiwan Occupational Safety and Health Administration of the Ministry of Labor). Available online: https://www.osha.gov.tw/enhome/ (accessed on 17 December 2015).
- Anttila, S.; Boffetta, P. Occupational Cancers, 2nd ed.; Springer Nature: Aargau, Switzerland, 2020. [Google Scholar]
- Carles, C.; Verdun-Esquer, C.; Leclerc, I.; Baldi, I. Occupational cancers: Risks and prevention. Bull. Du Cancer 2019, 106, 665–677. [Google Scholar] [CrossRef]
- Graeve, C.U.; McGovern, P.M.; Alexander, B.; Church, T.; Ryan, A.; Polovich, M. Occupational Exposure to Antineoplastic Agents: An Analysis of Health Care Workers and Their Environments. Workplace Health Saf. 2017, 65, 9–20. [Google Scholar] [CrossRef]
- Barnes, J.L.; Zubair, M.; John, K.; Poirier, M.C.; Martin, F.L. Carcinogens and DNA damage. Biochem. Soc. Trans. 2018, 46, 1213–1224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United States Department of Labor, Hazardous Drugs-Controlling Occupational Exposure to Hazardous Drugs|Occupational Safety and Health Administration (osha.gov). Available online: http://www.osha.gov/hazardous-drug/controlling-occexz#pharmacy (accessed on 27 November 2021).
- Boffetta, P.; Hainaut, P. Encyclopedia of Cancer, 3rd ed.; Elsevier Science: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Khan, Y.S.; Farhana, A. Histology, Cell; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- World Health Organization. Cancer. Available online: https://www.who.int/health-topics/cancer#tab=tab_1 (accessed on 12 September 2019).
- World Health Organization. Cancer: Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 12 September 2018).
- International Agency for Research on Cancer. Global Cancer Observatory. 2020. Available online: https://gco.iarc.fr/ (accessed on 17 October 2021).
- Union for International Cancer Control. GLOBOCAN 2020: New Global Cancer Data. 2021. Available online: https://www.uicc.org/news/globocan-2020-new-global-cancer-data (accessed on 17 October 2021).
- World Health Organization. WHO Reveals Leading Causes of Death and Disability Worldwide: 2000–2019. Available online: https://www.who.int/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000–2019 (accessed on 9 December 2020).
- Kuo, C.-N.; Liao, Y.-M.; Kuo, L.-N.; Tsai, H.-J.; Chang, W.-C.; Yen, Y. Cancers in Taiwan: Practical insight from epidemiology, treatments, biomarkers, and cost. J. Formos. Med Assoc. 2020, 119, 1731–1741. [Google Scholar] [CrossRef]
- Wei-ting, C.; Mazzetta, M. Cancer Incidence Continues to Rise in Taiwan. Focus Taiwan. Available online: https://focustaiwan.tw/society/202012290006 (accessed on 29 December 2020).
- Ministry of Health and Welfare. Taiwan Health and Welfare Report. Available online: https://www.mohw.gov.tw/lp-137-2.html (accessed on 22 April 2020).
- Health Promotion Administration, Ministry of Health and Welfare. Available online: https://www.mohw.gov.tw/mp-2.html (accessed on 7 July 2020).
- National Development Council. Taiwan Statistical Data Book 2016. Available online: https://www.roc-taiwan.org/uploads/sites/49/2016/11/Taiwan-Statistical-Data-Book-2016.pdf (accessed on 15 November 2016).
- Hsu, Y.-H.; Kung, P.-T.; Wang, Y.-H.; Chang, Y.-M.; Tsai, W.-C. A comparison of the stages at which cancer is diagnosed in physicians and in the general population in Taiwan. Can. Med. Assoc. J. 2015, 187, E412–E418. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.-S.; Hsu, C.-C.; Weng, S.-F.; Lin, H.-J.; Wang, J.-J.; Su, S.-B.; Huang, C.-C.; Guo, H.-R. Cancer Incidence in Physicians: A Taiwan National Population-based Cohort Study. Medicine 2015, 94, e2079. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.-Y.; Lin, C.-L.; Hsu, W.-H.; Wang, I.-K.; Chang, C.-C.; Huang, C.-C.; Kao, C.-H.; Liu, S.-H.; Sung, F.-C. A Comparison of Cancer Incidence among Physician Specialists and the General Population: A Taiwanese Cohort Study. J. Occup. Health 2013, 55, 158–166. [Google Scholar] [CrossRef] [Green Version]
- Yen, C.-K.; Tan, T.-H.; Feng, I.-J.; Ho, C.-H.; Hsu, C.-C.; Lin, H.-J.; Wang, J.-J.; Huang, C.-C. Comparison of Risk for End-Stage Renal Disease Between Physicians and the General Population: A Nationwide Population-Based Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 2211. [Google Scholar] [CrossRef] [Green Version]
- Chen, X. Statistical Methods for Global Health and Epidemiology: Principles, Methods and Applications; Springer Nature: Florida, FL, USA, 2020. [Google Scholar]
- Lieb, R. Population-Based Study. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; 2013; pp. 1507–1508. [Google Scholar] [CrossRef]
- Allie. Longitudinal Health Insurance Database 2000. Available online: http://allie.dbcls.jp/ (accessed on 23 January 2021).
- National Health Insurance Research Database. National Health Insurance Research Database. Available online: https://nhird.nhri.org.tw/en/index.htm (accessed on 25 January 2021).
- National Health Insurance. National Health Insurance Administration Ministry of Health and Welfare-Foreign Nationals from Hong Kong, Macau, China, or Other Countries who Reside in Taiwan with an Alien Resident Certificate (ARC). Available online: https://www.nhi.gov.tw/english/Conent_List.aspx?n=C88B41A4EAB5E692&topn=778856C209BCE527&Create=1 (accessed on 25 January 2021).
- Hsieh, C.-Y.; Su, C.-C.; Shao, S.-C.; Sung, S.-F.; Lin, S.-J.; Kao Yang, Y.-H.; Lai, E.C.-C. Taiwan’s National Health Insurance Research Database: Past and future. Clin. Epidemiol. 2019, 11, 349–358. [Google Scholar] [CrossRef] [Green Version]
- Mohanty, A.; Kabi, A.; Mohanty, A.P. Health problems in healthcare workers: A review. J. Fam. Med. Prim. Care 2019, 8, 2568–2572. [Google Scholar] [CrossRef]
- Lacombe, J.; Armstrong, M.E.G.; Wright, F.L.; Foster, C. The impact of physical activity and an additional behavioural risk factor on cardiovascular disease, cancer and all-cause mortality: A systematic review. BMC Public Health 2019, 19, 900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engel, C.L.; Rasanayagam, M.S.; Gray, J.M.; Rizzo, J. Work and Female Breast Cancer: The State of the Evidence, 2002–2017. New Solut. J. Environ. Occup. Health Policy 2018, 28, 55–78. [Google Scholar] [CrossRef] [PubMed]
- Fenga, C. Occupational exposure and risk of breast cancer. Biomed. Rep. 2016, 4, 282–292. [Google Scholar] [CrossRef] [Green Version]
- Giles, J.T.; Kennedy, D.T.; Dunn, E.C.; Wallace, W.L.; Meadows, S.L.; Cafiero, A.C. Results of a community pharmacy-based breast cancer risk-assessment and education program. Pharmacotherapy 2001, 21, 243–253. [Google Scholar] [CrossRef]
- Lin, H.-W.; Yang, L.-C.; Mafruhah, O.R.; Nguyen, H.T.; Cao, T.T.; Yam, F.K. Evolution of clinical pharmacy practice and pharmacy education in Taiwan, Vietnam, and Indonesia: A narrative review. J. Am. Coll. Clin. Pharmacy 2020, 3, 947–958. [Google Scholar] [CrossRef]
- Safitrih, L.; Perwitasari, D.A.; Ndoen, N.; Dandan, K.L. Health Workers’ Perceptions and Expectations of the Role of the Pharmacist in Emergency Units: A Qualitative Study in Kupang, Indonesia. Pharmacy 2019, 7, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, S.; Zhu, W.; Thompson, P.; Hannun, Y.A. Evaluating intrinsic and non-intrinsic cancer risk factors. Nat. Commun. 2018, 9, 3490. [Google Scholar] [CrossRef]
- Danaei, G.; Hoorn, S.V.; Lopez, A.D.; Murray, C.J.; Ezzati, M. Comparative Risk Assessment collaborating group (Cancers). Causes of cancer in the world: Comparative risk assessment of nine behavioural and environmental risk factors. Lancet 2005, 366, 1784–1793. [Google Scholar] [CrossRef] [Green Version]
- Allemani, C.; Matsuda, T.; Di Carlo, V.; Harewood, R.; Matz, M.; Nikšić, M.; Bonaventure, A.; Valkov, M.; Johnson, C.J.; Estève, J.; et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018, 391, 1023–1075. [Google Scholar] [CrossRef] [Green Version]
| Pharmacist N = 11568 | Comparison N = 46272 | |||
|---|---|---|---|---|
| n | % | n | % | |
| Men | 4731 | 40.9 | 18924 | 40.9 |
| Age, year | ||||
| 20–34 | 5407 | 46.7 | 21,628 | 46.7 |
| 35–44 | 3576 | 30.9 | 14,304 | 30.9 |
| 45–54 | 2053 | 17.8 | 8212 | 17.8 |
| 55+ | 532 | 4.60 | 2128 | 4.60 |
| Mean (SD) | 37.4 | (9.50) | 37.4 | (9.51) |
| CCI score | ||||
| 0 | 11,420 | 98.7 | 45,680 | 98.7 |
| 1 | 112 | 0.97 | 448 | 0.97 |
| 2+ | 36 | 0.31 | 144 | 0.31 |
| Work years | ||||
| 1–2 | 3498 | 30.2 | ||
| 3–5 | 4111 | 35.5 | ||
| 5+ | 3959 | 34.2 | ||
| Workplace | ||||
| Medical center | 1512 | 13.1 | ||
| Regional hospital | 1887 | 16.3 | ||
| District Hospital | 3220 | 20.1 | ||
| Clinics | 3860 | 33.4 | ||
| Pharmacy | 1989 | 17.2 | ||
| Pharmacist | Comparison | |||||||
|---|---|---|---|---|---|---|---|---|
| Event | Rate | Event | Rate | cHR (95% CI) | p-Value | aHR (95% CI) | p-Value | |
| Overall | 383 | 2.83 | 1547 | 2.96 | 0.95 (0.85–1.07) | 0.40 | 0.96 (0.85–1.07) | 0.43 |
| Gender | ||||||||
| Women | 224 | 2.80 | 714 | 2.29 | 1.22 (1.05–1.42) | 0.01 | 1.23 (1.06–1.43) | 0.007 |
| Men | 159 | 2.89 | 833 | 3.96 | 0.73 (0.61–0.86) | 0.0002 | 0.73 (0.61–0.86) | 0.0002 |
| Age, year | ||||||||
| 20–34 | 80 | 1.25 | 312 | 1.29 | 0.97 (0.76–1.24) | 0.79 | 0.97 (0.76–1.24) | 0.79 |
| 35–44 | 130 | 3.12 | 469 | 2.86 | 1.09 (0.89–1.32) | 0.40 | 1.09 (0.90–1.32) | 0.40 |
| 45–54 | 119 | 5.02 | 516 | 5.55 | 0.90 (0.74–1.10) | 0.31 | 0.90 (0.74–1.10) | 0.30 |
| 55+ | 54 | 9.37 | 250 | 11.20 | 0.83 (0.62–1.12) | 0.23 | 0.83 (0.62–1.11) | 0.21 |
| CCI score | ||||||||
| 0 | 370 | 277 | 1514 | 2.94 | 0.94 (0.84–1.05) | 0.28 | 0.94 (0.84–1.06) | 0.32 |
| 1 | 9 | 7.44 | 27 | 5.62 | 1.33 (0.62–2.82) | 0.46 | 1.33 (0.62–2.82) | 0.46 |
| 2+ | 4 | 11.32 | 6 | 4.56 | 2.55 (0.72–9.04) | 0.15 | 2.16 (0.59–7.99) | 0.25 |
| Pharmacist | Comparison | |||||
|---|---|---|---|---|---|---|
| LOCATION | Event | Rate | Event | Rate | aHR (95% CI) | p-Value |
| All | ||||||
| Liver | 27 | 0.20 | 206 | 0.39 | 0.50 (0.33–0.74) | 0.0007 |
| Breast (women only) | 116 | 1.45 | 271 | 0.87 | 1.68 (1.35–2.08) | <0.0001 |
| Lung | 20 | 0.15 | 125 | 0.24 | 0.61 (0.68–0.98) | 0.04 |
| Thyroid | 23 | 0.17 | 63 | 0.12 | 1.41 (0.88–2.28) | 0.16 |
| Colon rectum | 40 | 0.30 | 168 | 0.32 | 0.91 (0.65–1.29) | 0.60 |
| Prostate (men only) | 14 | 0.25 | 24 | 0.11 | 2.18 (1.12–4.21) | 0.02 |
| Kidney | 13 | 0.10 | 30 | 0.06 | 1.67 (0.87–3.20) | 0.12 |
| Nasopharynx | 12 | 0.09 | 41 | 0.08 | 1.13 (0.59–2.15) | 0.71 |
| Stomach | 12 | 0.09 | 57 | 0.11 | 0.80 (0.43–1.50) | 0.49 |
| Bladder | 12 | 0.09 | 34 | 0.07 | 1.33 (0.69–2.57) | 0.40 |
| Other | 94 | 0.70 | 528 | 1.01 | 0.69 (0.55–0.86) | 0.0008 |
| Women | ||||||
| Liver | 5 | 0.06 | 25 | 0.08 | 0.77 (0.30–2.02) | 0.60 |
| Breast | 116 | 1.45 | 271 | 0.87 | 1.68 (1.35–2.08) | <0.0001 |
| Lung | 9 | 0.11 | 48 | 0.15 | 0.73 (0.36–1.49) | 0.39 |
| Thyroid | 20 | 0.25 | 47 | 0.15 | 1.65 (0.98–2.79) | 0.06 |
| Colon rectum | 15 | 0.19 | 60 | 0.19 | 0.98 (0.56–1.72) | 0.94 |
| Prostate | NA | |||||
| Kidney | 4 | 0.05 | 6 | 0.02 | 2.62 (0.74–9.27) | 0.14 |
| Nasopharynx | 1 | 0.01 | 14 | 0.04 | 0.28 (0.04–2.13) | 0.22 |
| Stomach | 5 | 0.06 | 18 | 0.06 | 1.09 (0.40–2.93) | 0.87 |
| Bladder | 2 | 0.02 | 5 | 0.02 | 1.56 (0.30–8.03) | 0.60 |
| Other | 47 | 0.59 | 220 | 0.71 | 0.84 (0.61–1.15) | 0.27 |
| Men | ||||||
| Liver | 22 | 0.40 | 181 | 0.86 | 0.46 (0.30–0.72) | 0.0006 |
| Breast | NA | |||||
| Lung | 11 | 0.20 | 77 | 0.37 | 0.54 (0.29–1.02) | 0.06 |
| Thyroid | 3 | 0.05 | 16 | 0.08 | 0.71 (0.21–2.44) | 0.59 |
| Colon rectum | 25 | 0.45 | 108 | 0.51 | 0.88 (0.57–1.36) | 0.55 |
| Prostate | 14 | 0.25 | 24 | 0.11 | 2.18 (1.12–4.21) | 0.02 |
| Kidney | 9 | 0.16 | 24 | 0.11 | 1.43 (0.66–3.07) | 0.36 |
| Nasopharynx | 11 | 0.20 | 27 | 0.13 | 1.56 (0.77–3.15) | 0.21 |
| Stomach | 7 | 0.13 | 39 | 0.13 | 0.68 (0.30–1.51) | 0.34 |
| Bladder | 10 | 0.18 | 29 | 0.14 | 1.30 (0.63–2.67) | 0.47 |
| Other | 47 | 0.85 | 308 | 1.46 | 0.58 (0.43–0.79) | 0.0005 |
| All | Women | Men | ||||
|---|---|---|---|---|---|---|
| aHR (95% CI) | p-Value | aHR (95% CI) | p-Value | aHR (95% CI) | p-Value | |
| Age, year | 1.07 (1.06–1.08) | <0.0001 | 1.06 (1.05–1.08) | <0.0001 | 1.08 (1.06–1.09) | <0.0001 |
| Women vs. men | 1.59 (1.27–2.00) | <0.0001 | ||||
| CCI score | 1.42 (1.02–1.98) | 0.038 | 1.28 (0.67–2.47) | 0.456 | 1.42 (0.96–2.09) | 0.079 |
| Work years | ||||||
| 1–2 | 1.04 (0.78–1.39) | 0.772 | 1.15 (0.81–1.62) | 0.436 | ref. | |
| 3–5 | 1.03 (0.81–1.32) | 0.808 | Ref. | 1.29 (0.83–2.02) | 0.257 | |
| 5+ | Ref. | 1.03 (0.75–1.43) | 0.842 | 1.14 (0.72–1.83) | 0.576 | |
| Workplace | ||||||
| Medical center | 1.39 (0.89–2.16) | 0.149 | 1.37 (0.84–2.23) | 0.204 | 1.25 (0.42–3.71) | 0.694 |
| Regional hospital | Ref. | Ref. | Ref. | |||
| District Hospital | 1.31 (0.88–1.95) | 0.191 | 1.12 (0.70–1.80) | 0.636 | 1.99 (0.87–4.56) | 0.104 |
| Clinics | 1.28 (0.88–1.88) | 0.198 | 1.18 (0.76–1.83) | 0.471 | 1.88 (0.83–4.23) | 0.128 |
| Pharmacy | 1.59 (1.07–2.37) | 0.023 | 1.40 (0.82–2.38) | 0.215 | 2.14 (0.97–4.68) | 0.058 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, Y.-W.; Lin, C.-H.; Pai, L.-W.; Mou, C.-H.; Wang, J.-Y.; Lin, M.-H. Population-Based Study on Cancer Incidence in Pharmacist: A Cohort Study in Taiwan. Int. J. Environ. Res. Public Health 2021, 18, 12625. https://doi.org/10.3390/ijerph182312625
Lin Y-W, Lin C-H, Pai L-W, Mou C-H, Wang J-Y, Lin M-H. Population-Based Study on Cancer Incidence in Pharmacist: A Cohort Study in Taiwan. International Journal of Environmental Research and Public Health. 2021; 18(23):12625. https://doi.org/10.3390/ijerph182312625
Chicago/Turabian StyleLin, Ya-Wen, Che-Huei Lin, Lee-Wen Pai, Chih-Hsin Mou, Jong-Yi Wang, and Ming-Hung Lin. 2021. "Population-Based Study on Cancer Incidence in Pharmacist: A Cohort Study in Taiwan" International Journal of Environmental Research and Public Health 18, no. 23: 12625. https://doi.org/10.3390/ijerph182312625
APA StyleLin, Y.-W., Lin, C.-H., Pai, L.-W., Mou, C.-H., Wang, J.-Y., & Lin, M.-H. (2021). Population-Based Study on Cancer Incidence in Pharmacist: A Cohort Study in Taiwan. International Journal of Environmental Research and Public Health, 18(23), 12625. https://doi.org/10.3390/ijerph182312625






