Psychosocial and Biological Outcomes of Immersive, Mindfulness-Based Treks in Nature for Groups of Young Adults and Caregivers Affected by Cancer: Results from a Single Arm Program Evaluation from 2016–2021
Abstract
:1. Introduction
2. Materials and Methods
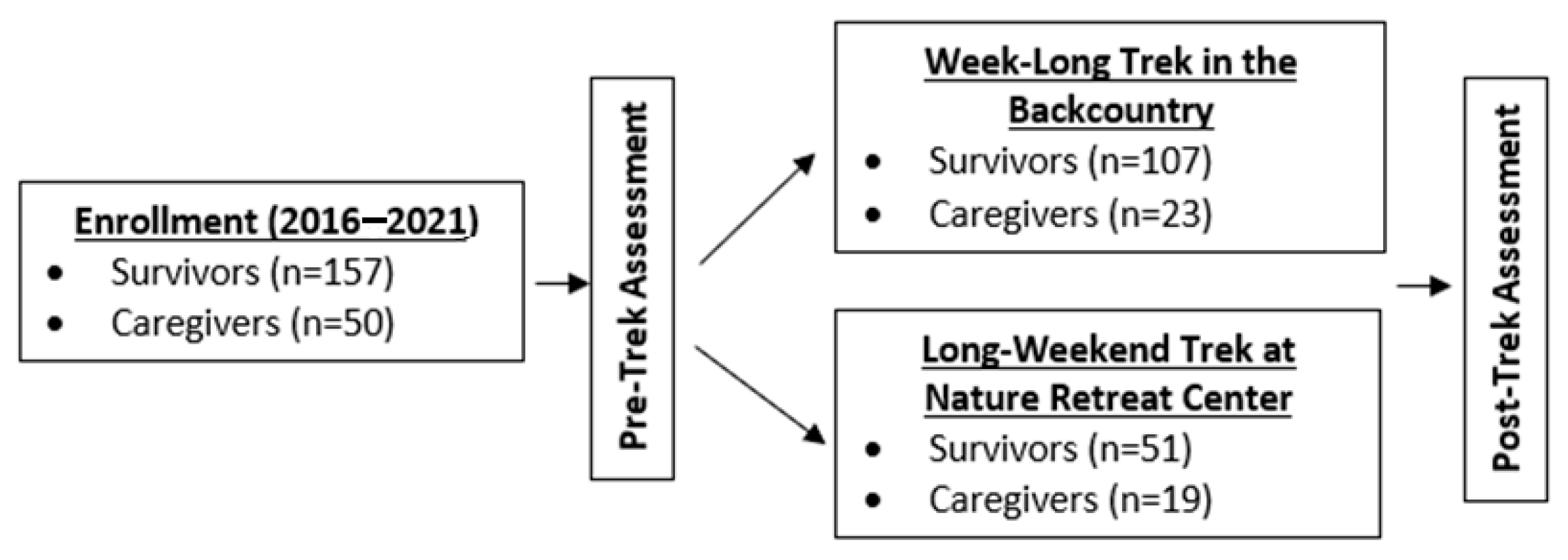
2.1. Design and Setting
2.2. Participants and Enrollment
2.3. Trek Activities, Objectives, and Curriculum
2.4. Data Collection Procedure
2.5. Measurement of Outcomes
2.5.1. Connection
2.5.2. Knowledge and Efficacy
2.5.3. Post-Trek Enjoyment, Appreciation, Insights, and Learning
2.5.4. Symptoms of Anxiety, Depression, and Sleep Disturbance
2.5.5. Inflammation
2.6. Statistical Analysis
3. Results
3.1. Socio-Demographic and Cancer-Related Characteristics
3.2. Changes in Connection
3.3. Changes in Knowledge and Efficacy
3.4. Trek Enjoyment, Appreciation, Insights, and Learning
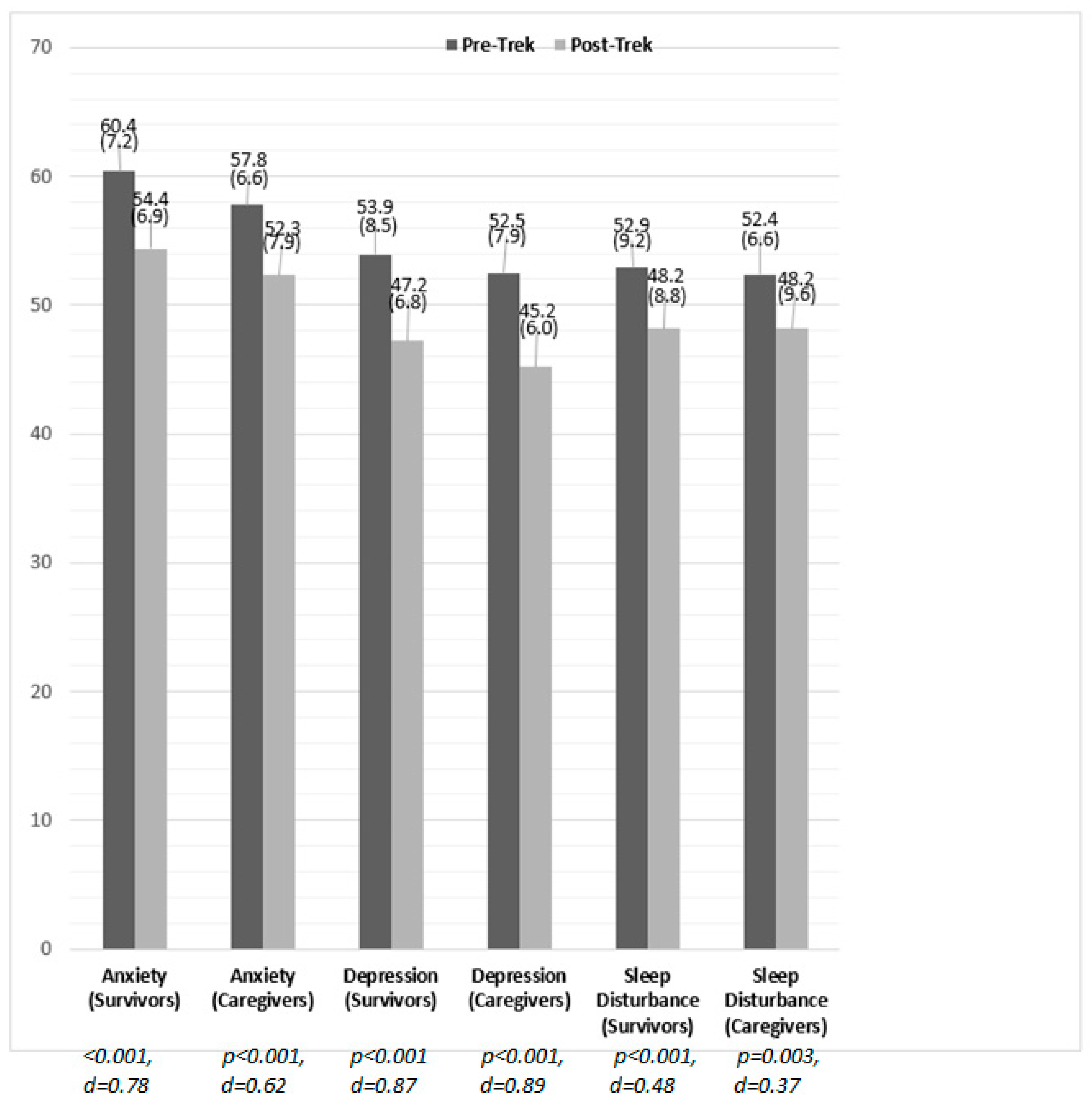
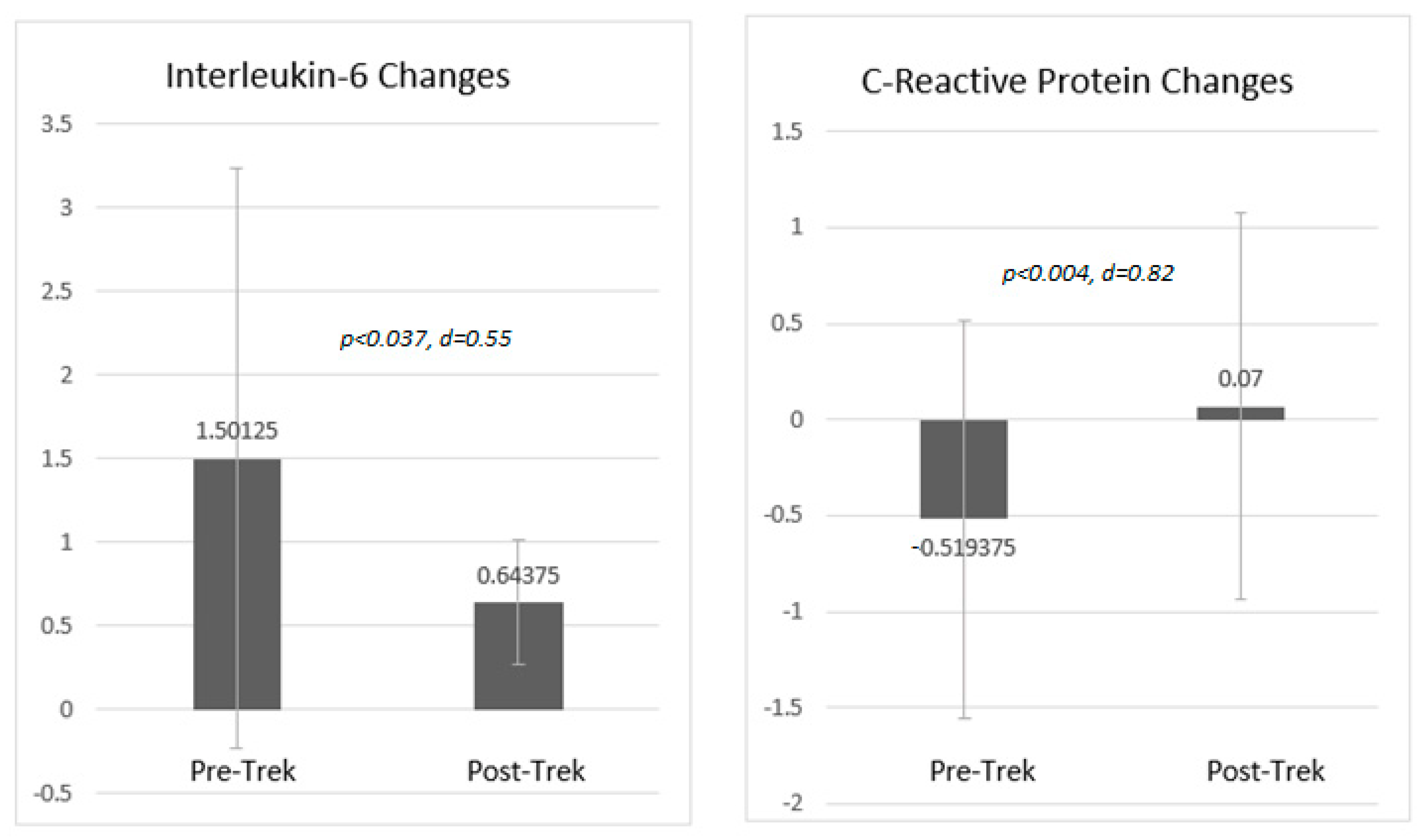
3.5. Changes in Anxiety, Depression, Sleep Disturbance and Inflammation
3.6. Primary Mode of In-Field Locomotion and Trek Type/Duration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pietrabissa, G.; Simpson, S.G. Psychological Consequences of Social Isolation During COVID-19 Outbreak. Front. Psychol. 2020, 11, 2201. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, R.; Burns, A.; Leavey, G.; Leroi, I.; Burholt, V.; Lubben, J.; Holt-Lunstad, J.; Victor, C.; Lawlor, B.; Vilar-Compte, M.; et al. Impact of the COVID-19 Pandemic on Loneliness and Social Isolation: A Multi-Country Study. Int. J. Environ. Res. Public Health 2021, 18, 9982. [Google Scholar] [CrossRef]
- Victorson, D.; Garcia, S.F.; Sanford, S.; Snyder, M.A.; Lampert, S.; Salsman, J.M. A Qualitative Focus Group Study to Illu-minate the Lived Emotional and Social Impacts of Cancer and Its Treatment on Young Adults. J. Adolesc. Young Adult Oncol. 2019, 8, 649–659. [Google Scholar] [CrossRef] [PubMed]
- Munoz, A.R.; Kaiser, K.; Yanez, B.; Victorson, D.; Garcia, S.F.; Snyder, M.A.; Salsman, J.M. Cancer experiences and health-related quality of life among racial and ethnic minority survivors of young adult cancer: A mixed methods study. Support. Care Cancer 2016, 24, 4861–4870. [Google Scholar] [CrossRef] [Green Version]
- Salsman, J.M.; Garcia, S.F.; Yanez, B.; Sanford, S.D.; Snyder, M.A.; Victorson, D. Physical, emotional, and social health differences between posttreatment young adults with cancer and matched healthy controls. Cancer 2014, 120, 2247–2254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yanez, B.; Garcia, S.F.; Victorson, D.; Salsman, J.M. Distress among young adult cancer survivors: A cohort study. Support. Care Cancer 2013, 21, 2403–2408. [Google Scholar] [CrossRef] [Green Version]
- Ryder-Burbidge, C.; Diaz, R.L.; Barr, R.D.; Gupta, S.; Nathan, P.C.; McKillop, S.J.; Fidler-Benaoudia, M.M. The Burden of Late Effects and Related Risk Factors in Adolescent and Young Adult Cancer Survivors: A Scoping Review. Cancers 2021, 13, 4870. [Google Scholar] [CrossRef] [PubMed]
- Lang, M.J.; David, V.; Giese-Davis, J. The Age Conundrum: A Scoping Review of Younger Age or Adolescent and Young Adult as a Risk Factor for Clinical Distress, Depression, or Anxiety in Cancer. J. Adolesc. Young Adult Oncol. 2015, 4, 157–173. [Google Scholar] [CrossRef] [Green Version]
- Victorson, D.; Luberto, C.; Koffler, K. Nature as Medicine: Mind, Body, and Soil. J. Altern. Complement. Med. 2020, 26, 658–662. [Google Scholar] [CrossRef]
- Gianfredi, V.; Buffoli, M.; Rebecchi, A.; Croci, R.; Oradini-Alacreu, A.; Stirparo, G.; Marino, A.; Odone, A.; Capolongo, S.; Signorelli, C. Association between Urban Greenspace and Health: A Systematic Review of Literature. Int. J. Environ. Res. Public Health 2021, 18, 5137. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Zhang, C.-Q.; Rhodes, R.E. The pathways linking objectively-measured greenspace exposure and mental health: A systematic review of observational studies. Environ. Res. 2021, 198, 111233. [Google Scholar] [CrossRef] [PubMed]
- Masterton, W.; Carver, H.; Parkes, T.; Park, K. Greenspace interventions for mental health in clinical and non-clinical populations: What works, for whom, and in what circumstances? Health Place 2020, 64, 102338. [Google Scholar] [CrossRef]
- White, M.P.; Alcock, I.; Grellier, J.; Wheeler, B.; Hartig, T.; Warber, S.L.; Bone, A.; Depledge, M.H.; Fleming, L.E. Spending at least 120 minutes a week in nature is associated with good health and wellbeing. Sci. Rep. 2019, 9, 7730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. 2018, 166, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Houlden, V.; Weich, S.; De Albuquerque, J.P.; Jarvis, S.; Rees, K. The relationship between greenspace and the mental wellbeing of adults: A systematic review. PLoS ONE 2018, 13, e0203000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dzhambov, A.M.; Markevych, I.; Hartig, T.; Tilov, B.; Arabadzhiev, Z.; Stoyanov, D.; Gatseva, P.; Dimitrova, D.D. Multiple pathways link urban green- and bluespace to mental health in young adults. Environ. Res. 2018, 166, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Kuo, M. How might contact with nature promote human health? Promising mechanisms and a possible central pathway. Front. Psychol. 2015, 6, 1093. [Google Scholar] [CrossRef]
- Frumkin, H.; Bratman, G.N.; Breslow, S.J.; Cochran, B.; Kahn, P.H., Jr.; Lawler, J.J.; Levin, P.S.; Tandon, P.S.; Varanasi, U.; Wolf, K.L.; et al. Nature Contact and Human Health: A Research Agenda. Environ. Health Perspect. 2017, 125, 075001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cui, R.; Gujral, S.; Galfalvy, H.; Szanto, K. The Role of Perceived and Objective Social Connectedness on Risk for Suicidal Thoughts and Behavior in Late-Life and Their Moderating Effect on Cognitive Deficits. Am. J. Geriatr. Psychiatry 2021. [Google Scholar] [CrossRef]
- Akers, S.W.; Joseph, R.A. Reducing the Negative Impact of Social Distancing Through Intentional Connectedness. J. Christ. Nurs. 2021, 38, 216–223. [Google Scholar] [CrossRef]
- Preston, A.J.; Rew, L. Connectedness, Self-Esteem, and Prosocial Behaviors Protect Adolescent Mental Health Following Social Isolation: A Systematic Review. Issues Ment. Health Nurs. 2021, 4, 1–10. [Google Scholar] [CrossRef]
- Bailey, M.; Cao, R.; Kuchler, T.; Stroebel, J.; Wong, A. Social Connectedness: Measurement, Determinants, and Effects. J. Econ. Perspect. 2018, 32, 259–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nitschke, J.P.; Forbes, P.A.G.; Ali, N.; Cutler, J.; Apps, M.A.J.; Lockwood, P.L.; Lamm, C. Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. Br. J. Health Psychol. 2021, 26, 553–569. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Nguyen, N.H.; Wang, D.; Lynch, B.M.; Hodge, A.M.; Bassett, J.K.; White, V.M.; Borland, R.; English, D.R.; Milne, R.L.; et al. Social connectedness and mortality after prostate cancer diagnosis: A prospective cohort study. Int. J. Cancer 2020, 147, 766–776. [Google Scholar] [CrossRef]
- Victorson, D.E.; Sauer, C.M.; Wolters, L.; Maletich, C.; Lukoff, K.; Sufrin, N. Meta-analysis of Technology-Enabled Mind-fulness-Based Programs for Negative Affect and Mindful Awareness. Mindfulness 2020, 11, 1884–1899. [Google Scholar] [CrossRef]
- Victorson, D.K.; Kentor, M.; Maletich, C.; Lawton, R.C.; Hankin Kaufman, V.; Borrero, M.; Languido, L.; Lewett, K.; Pancoe, H.; Berkowitz, C. A Systematic Review and Meta-Analysis of Mindfulness-Based Randomized Controlled Trials Relevant to Lifestyle Medicine. Am. J. Lifestyle Med. 2015, 9, 185–211. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Mind to Face Stress, Pain and Illness; Dell Publishing: New York, NY, USA, 1990. [Google Scholar]
- Basso, J.C.; McHale, A.; Ende, V.; Oberlin, D.J.; Suzuki, W.A. Brief, daily meditation enhances attention, memory, mood, and emotional regulation in non-experienced meditators. Behav. Brain Res. 2019, 356, 208–220. [Google Scholar] [CrossRef]
- Rodrigues, M.F.; Nardi, A.E.; Levitan, M. Mindfulness in mood and anxiety disorders: A review of the literature. Trends Psychiatry Psychother. 2017, 39, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Oliva, F.; Malandrone, F.; di Girolamo, G.; Mirabella, S.; Colombi, N.; Carletto, S.; Ostacoli, L. The efficacy of mindfulness-based interventions in attention-deficit/hyperactivity disorder beyond core symptoms: A systematic review, meta-analysis, and meta-regression. J. Affect. Disord. 2021, 292, 475–486. [Google Scholar] [CrossRef]
- Pedro, J.; Monteiro-Reis, S.; Carvalho-Maia, C.; Henrique, R.; Jerónimo, C.; Silva, E.R. Evidence of psychological and biological effects of structured Mindfulness-Based Interventions for cancer patients and survivors: A meta-review. Psycho-Oncol. 2021, 30, 1836–1848. [Google Scholar] [CrossRef]
- Reich, R.R.; Lengacher, C.A.; Klein, T.W.; Newton, C.; Shivers, S.; Ramesar, S.; Alinat, C.B.; Paterson, C.; Le, A.; Park, J.Y.; et al. A Randomized Controlled Trial of the Effects of Mindfulness-Based Stress Reduction (MBSR[BC]) on Levels of Inflammatory Biomarkers Among Recovering Breast Cancer Survivors. Biol. Res. Nurs. 2017, 19, 456–464. [Google Scholar] [CrossRef]
- Pilkonis, P.A.; Choi, S.W.; Reise, S.P.; Stover, A.M.; Riley, W.T.; Cella, D.; Group, P.C. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): Depression, anxiety, and anger. Assessment 2011, 18, 263–283. [Google Scholar] [CrossRef]
- Yu, L.; Buysse, D.J.; Germain, A.; Moul, D.E.; Stover, A.; Dodds, N.E.; Johnston, K.L.; Pilkonis, P.A. Development of Short Forms From the PROMIS™ Sleep Disturbance and Sleep-Related Impairment Item Banks. Behav. Sleep Med. 2012, 10, 6–24. [Google Scholar] [CrossRef]
- Crane, R.S.; Stanley, S.; Rooney, M.; Bartley, T.; Cooper, L.; Mardula, J. Disciplined Improvisation: Characteristics of Inquiry in Mindfulness-Based Teaching. Mindfulness 2015, 6, 1104–1114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDade, T.W. Development and validation of assay protocols for use with dried blood spot samples. Am. J. Hum. Biol. 2013, 26, 1–9. [Google Scholar] [CrossRef]
- McDade, T.W.; Burhop, J.; Dohnal, J. High-Sensitivity Enzyme Immunoassay for C-Reactive Protein in Dried Blood Spots. Clin. Chem. 2004, 50, 652–654. [Google Scholar] [CrossRef] [Green Version]
- McDade, T.W.; Miller, A.; Tran, T.T.; Borders, A.E.B.; Miller, G. A highly sensitive multiplex immunoassay for inflammatory cytokines in dried blood spots. Am. J. Hum. Biol. 2021, 33, e23558. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.B. Estimating Effect Sizes From Pretest-Posttest-Control Group Designs. Organ. Res. Methods 2008, 11, 364–386. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Yost, K.J.; Eton, D.T.; Garcia, S.F.; Cella, D. Minimally important differences were estimated for six Patient-Reported Out-comes Measurement Information System-Cancer scales in advanced-stage cancer patients. J. Clin. Epidemiol. 2011, 64, 507–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guirao, J.J.; Cabrera, C.M.; Jiménez, N.; Rincón, L.; Urra, J.M. High serum IL-6 values increase the risk of mortality and the severity of pneumonia in patients diagnosed with COVID-19. Mol. Immunol. 2020, 128, 64–68. [Google Scholar] [CrossRef]
- Nehring, S.M.; Goyal, A.; Bansal, P.; Patel, B.C. C Reactive Protein; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Cerqueira, É.; Marinho, D.A.; Neiva, H.P.; Lourenço, O. Inflammatory Effects of High and Moderate Intensity Exercise—A Systematic Review. Front. Physiol. 2020, 10, 1550. [Google Scholar] [CrossRef]
- Cho, S.H.; Lim, J.-E.; Lee, J.; Lee, J.S.; Jeong, H.-G.; Lee, M.-S.; Ko, Y.-H.; Han, C.; Ham, B.-J.; Han, K.-M. Association between high-sensitivity C-reactive protein levels and depression: Moderation by age, sex, obesity, and aerobic physical activity. J. Affect. Disord. 2021, 291, 375–383. [Google Scholar] [CrossRef]
- Khan, A.; Leonard, D.; Defina, L.; Barlow, C.E.; Willis, B.; Brown, E.S. Association between C reactive protein and depression in a population of healthy adults: The Cooper Center Longitudinal Study. J. Investig. Med. 2020, 68, 1019–1023. [Google Scholar] [CrossRef] [PubMed]
- Roohi, E.; Jaafari, N.; Hashemian, F. On inflammatory hypothesis of depression: What is the role of IL-6 in the middle of the chaos? J. Neuroinflamm. 2021, 18, 1–15. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, A.; Hughes, B.M.; Slavich, G.M.; Lynch, L.; Cronin, M.-T.; O’Farrelly, C.; Malone, K.M. Clinical anxiety, cortisol and interleukin-6: Evidence for specificity in emotion–biology relationships. Brain Behav. Immun. 2010, 24, 1074–1077. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Capaldi, C.; Dopko, R.L.; Zelenski, J.M. The relationship between nature connectedness and happiness: A meta-analysis. Front. Psychol. 2014, 5, 976. [Google Scholar] [CrossRef] [Green Version]
- Whitburn, J.; Linklater, W.; Abrahamse, W. Meta-analysis of human connection to nature and proenvironmental behavior. Conserv. Biol. 2020, 34, 180–193. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.M.; Jones, R.; Tocchini, K. Shinrin-Yoku (Forest Bathing) and Nature Therapy: A State-of-the-Art Review. Int. J. Environ. Res. Public Health 2017, 14, 851. [Google Scholar] [CrossRef] [Green Version]
- Zebrack, B.; Hamilton, R.; Smith, A.W. Psychosocial Outcomes and Service Use Among Young Adults With Cancer. Semin. Oncol. 2009, 36, 468–477. [Google Scholar] [CrossRef]
- Zebrack, B.J.; Block, R.; Hayes-Lattin, B.; Embry, L.; Aguilar, C.; Meeske, K.A.; Li, Y.; Butler, M.; Cole, S. Psychosocial service use and unmet need among recently diagnosed adolescent and young adult cancer patients. Cancer 2013, 119, 201–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| All (n = 207) | Cancer Survivor (n = 157) | Caregiver (n = 50) | ||||
|---|---|---|---|---|---|---|
| Mean (SD) | ||||||
| Age | 34.9 (7.4) | 33.6 (5.3) | 39.1 (10.7) | |||
| Age at first cancer diagnosis | -- | 26.6 (8.2) | -- | |||
| Years since first cancer diagnosis | -- | 6.7 (7.1) | -- | |||
| Value (Percentage) | ||||||
| Sex | ||||||
| Female | 157 | (76.0%) | 117 | (75.0%) | 18 | (36.0%) |
| Male | 50 | (24.0%) | 40 | (25.0%) | 32 | (64.0%) |
| Race | ||||||
| White | 163 | (82%) | -- | -- | -- | -- |
| Non-White | 35 | (18%) | -- | -- | -- | -- |
| US Region | ||||||
| Northeast | 42 | (20.8%) | -- | -- | -- | -- |
| Southeast | 29 | (14.4%) | -- | -- | -- | -- |
| Midwest | 86 | (42.6%) | -- | -- | -- | -- |
| Southwest | 9 | (4.5%) | -- | -- | -- | -- |
| West | 36 | (17.8%) | -- | -- | -- | -- |
| Primary Cancer Type | ||||||
| Brain | -- | -- | 19 | (12.1%) | -- | -- |
| Breast | -- | -- | 48 | (30.6%) | -- | -- |
| Colorectal | -- | -- | 6 | (3.8%) | -- | -- |
| Gynecologic | -- | -- | 3 | (5.7%) | -- | -- |
| Head and Neck | -- | -- | 4 | (2.5%) | -- | -- |
| Hematological | -- | -- | 45 | (28.7%) | -- | -- |
| Kidney & Renal | -- | -- | 1 | (0.6%) | -- | -- |
| Melanoma | -- | -- | 2 | (1.3%) | -- | -- |
| Mesothelioma | -- | -- | 1 | (0.6%) | -- | -- |
| Sarcoma | -- | -- | 12 | (7.6%) | -- | -- |
| Stomach | -- | -- | 2 | (1.3%) | -- | -- |
| Testicular | -- | -- | 3 | (1.9%) | -- | -- |
| Thyroid | -- | -- | 5 | (3.2%) | -- | -- |
| Trek Locations from 2016–2021 | ||||||
| Bahamas | 10 | (4.8%) | 5 | (3.2%) | 5 | (10.0%) |
| Boundary Waters (Minnesota) | 21 | (10.1%) | 21 | (13.4%) | 0 | (0.0%) |
| Green River (Utah) | 60 | (29.0%) | 40 | (25.5%) | 20 | (40.0%) |
| Selkirk Mountains (Idaho) | 19 | (9.2%) | 14 | (8.9%) | 5 | (10.0%) |
| Upper Peninsula (Michigan) | 63 | (30.4%) | 47 | (29.9%) | 16 | (32.0%) |
| Wind Rivers (Wyoming) | 23 | (11.1%) | 19 | (12.1%) | 4 | (8.0%) |
| Yellowstone (Wyoming) | 11 | (5.3%) | 11 | (7.0%) | 0 | (0.00%) |
| Cancer Survivors (n = 140) | Caregivers (n = 38) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Trek | Post-Trek | Sig | ES | Pre-Trek | Post-Trek | Sig | ES | |||||
| M | SD | M | SD | M | SD | M | SD | |||||
| Connection Item Indicators | ||||||||||||
| Feel connected to nature and the outdoors | 3.6 | 0.99 | 4.6 | 0.66 | 0.001 | 0.95 | 3.6 | 0.97 | 4.5 | 0.74 | 0.001 | 0.93 |
| Feel connected to other young adult cancer survivors | 2.9 | 1.1 | 4.4 | 0.83 | 0.001 | 1.1 | ||||||
| Feel connected to other caregivers affected by cancer | -- | -- | -- | -- | -- | -- | 2.5 | 1.1 | 4.3 | 0.89 | 0.001 | 1.3 |
| Able to reflect on my path & direction as a survivor | 3.6 | 0.96 | 4.3 | 0.80 | 0.001 | 0.57 | -- | -- | -- | -- | -- | -- |
| Able to reflect on my path & direction as a caregiver | -- | -- | -- | -- | -- | -- | 3.2 | 0.89 | 4.5 | 0.64 | 0.001 | 1.5 |
| Knowledge and Efficacy Item Indicators | ||||||||||||
| Aware of benefits of mindfulness for health | 3.4 | 1.1 | 4.5 | 0.75 | 0.001 | 0.89 | 2.9 | 1.2 | 4.3 | 0.68 | 0.001 | 1.4 |
| Comfortable doing outdoor activities | 3.9 | 0.96 | 4.3 | 0.80 | 0.001 | 0.37 | 4.1 | 0.97 | 4.2 | 0.85 | 0.399 | 0.18 |
| Confident incorporating mindfulness into daily life | 2.8 | 1.0 | 4.4 | 0.84 | 0.001 | 1.3 | 2.7 | 0.91 | 4.2 | 0.71 | 0.001 | 1.5 |
| Cancer Survivors (n = 146) | Caregivers (n = 40) | ||||||
|---|---|---|---|---|---|---|---|
| Single Item Indicators | Quite a Bit | Great Deal | Total | Quite a Bit | Great Deal | Total | p |
| Had fun. | 22.8 | 66.5 | 89.3 | 7.5 | 85.0 | 92.5 | 0.02 |
| Appreciation for nature and the outdoors increased. | 26.0 | 60.8 | 86.8 | 22.5 | 67.5 | 90.0 | 0.69 |
| Gained insights into things that can cause stress, frustration or discomfort. | 32.3 | 39.9 | 72.2 | 42.5 | 42.5 | 85.0 | 0.59 |
| Learned some things to help manage stress and uncertainties in life. | 32.3 | 41.8 | 74.1 | 52.5 | 35.0 | 87.5 | 0.09 |
| Learned ways to slow down and just notice mind and body. | 25.3 | 53.2 | 78.5 | 27.5 | 57.5 | 85.0 | 0.99 |
| Learned different ways to “respond” to stress instead of “reacting” to it. | 27.2 | 39.2 | 66.4 | 37.5 | 30.0 | 67.5 | 0.18 |
| Learned about being a more accepting “observer” to myself and my experiences. | 36.1 | 43.0 | 79.1 | 42.5 | 42.5 | 85.0 | 0.65 |
| I learned about being kind and compassionate to myself, even for the “little things.” | 29.1 | 48.1 | 77.2 | 35.0 | 55.0 | 90.0 | 0.94 |
| Gained deeper appreciation for some of life’s simpler things (e.g., walking, eating) | 30.4 | 52.5 | 82.9 | 15.0 | 62.5 | 77.5 | 0.07 |
| Learned about “sitting” with unpleasant experiences without becoming overwhelmed. | 31.6 | 36.1 | 67.7 | 37.5 | 40.0 | 77.5 | 0.87 |
| Have a better understanding of what mindfulness is and isn’t. | 38.6 | 43.7 | 82.3 | 55.0 | 35.0 | 90.0 | 0.13 |
| Feel more confident in ability to do things to stay healthy and well as a cancer survivor. | 37.3 | 37.3 | 74.6 | 38.5 | 41.0 | 79.5 | 0.87 |
| Plan to keep learning and practicing mindfulness meditation when return home. | 28.5 | 50.0 | 78.5 | 40.0 | 40.0 | 80.0 | 0.16 |
| Plan to spend more time in the outdoors, even if it’s just at a park, after return home. | 19.6 | 67.1 | 86.7 | 35.0 | 55.0 | 90.0 | 0.04 |
| Feel like this experience will continue to affect me in positive ways after return home. | 16.5 | 72.2 | 88.7 | 7.5 | 85.0 | 92.5 | 0.13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Victorson, D.; Doninger, G.; Victorson, S.; Victorson, G.; Hall, L.; Maletich, C.; Corr, B.R.; Scortino, K.; Burns, Z.; Allen, L.; et al. Psychosocial and Biological Outcomes of Immersive, Mindfulness-Based Treks in Nature for Groups of Young Adults and Caregivers Affected by Cancer: Results from a Single Arm Program Evaluation from 2016–2021. Int. J. Environ. Res. Public Health 2021, 18, 12622. https://doi.org/10.3390/ijerph182312622
Victorson D, Doninger G, Victorson S, Victorson G, Hall L, Maletich C, Corr BR, Scortino K, Burns Z, Allen L, et al. Psychosocial and Biological Outcomes of Immersive, Mindfulness-Based Treks in Nature for Groups of Young Adults and Caregivers Affected by Cancer: Results from a Single Arm Program Evaluation from 2016–2021. International Journal of Environmental Research and Public Health. 2021; 18(23):12622. https://doi.org/10.3390/ijerph182312622
Chicago/Turabian StyleVictorson, David, Gretchen Doninger, Scott Victorson, Gwen Victorson, Lars Hall, Carly Maletich, Bradley R. Corr, Kathy Scortino, Zachary Burns, Lori Allen, and et al. 2021. "Psychosocial and Biological Outcomes of Immersive, Mindfulness-Based Treks in Nature for Groups of Young Adults and Caregivers Affected by Cancer: Results from a Single Arm Program Evaluation from 2016–2021" International Journal of Environmental Research and Public Health 18, no. 23: 12622. https://doi.org/10.3390/ijerph182312622
APA StyleVictorson, D., Doninger, G., Victorson, S., Victorson, G., Hall, L., Maletich, C., Corr, B. R., Scortino, K., Burns, Z., Allen, L., Rosa, I., Quirk, K., Adegbemi, A., Strokoff, J., Zuidema, K., Sajdak, K., Mckibben, T., Roberts, A., McDade, T. W., ... Salsman, J. M. (2021). Psychosocial and Biological Outcomes of Immersive, Mindfulness-Based Treks in Nature for Groups of Young Adults and Caregivers Affected by Cancer: Results from a Single Arm Program Evaluation from 2016–2021. International Journal of Environmental Research and Public Health, 18(23), 12622. https://doi.org/10.3390/ijerph182312622






