Development of Nonlaboratory-Based Risk Prediction Models for Cardiovascular Diseases Using Conventional and Machine Learning Approaches
Abstract
1. Introduction
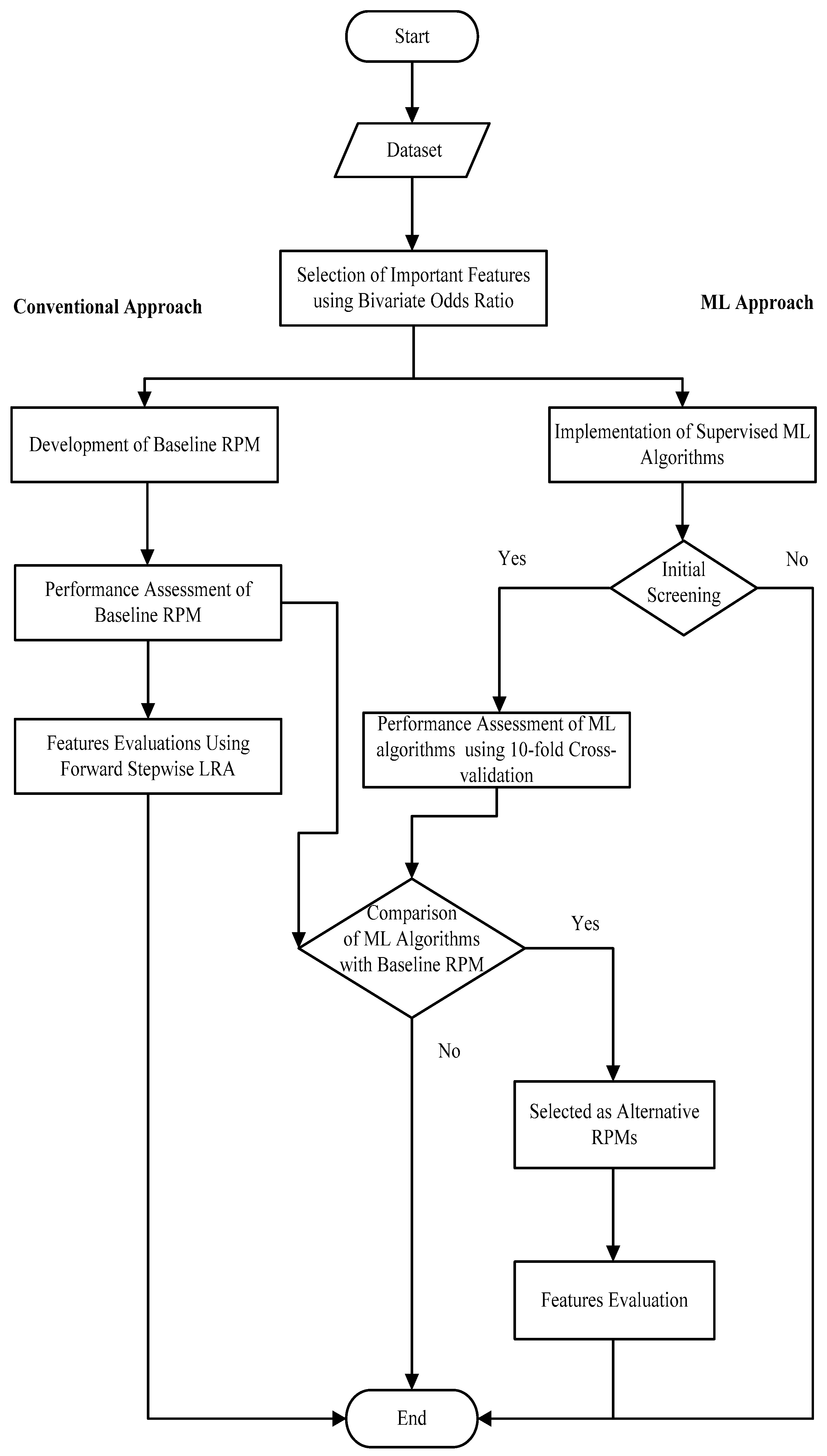
2. Materials and Methods
2.1. Study Population and Design
2.2. Description and Identification of Important Features
2.3. Development of Baseline Conventional RPM and Relative Feature Importance
2.4. Development of ML-Based RPMs
- ANN with single hidden layer model: The model consisted of a sigmoid activation function with one hidden layer having 8 hidden nodes. The multilayer-perceptron (MLP) with the backpropagation method at 0.3 momentum and learning rate was finalized. Further, weight decay as a regularization technique was also used to avoid over-fitting.
- The linear kernel SVM model: The SVM was given the entirety of the dataset and mainly trained with two different kernels, which were linear and radial basis function (RBF) kernels. These kernels identified relationships between features within the dataset and tried to find optimal hyperplanes to model the binary outcome. However, linear kernel SVM performed well in the training and testing phases. This SVM model was optimized using the SMO method. Various cost function values (ct) were implemented to optimize the linear SVM model and ct = 0.5 provided a good RPM.
- Radial basis function SVM (RBF-SVM) model: We also tried SVM with an RBF kernel to gauge the possible non-linear patterns within the dataset. The RBF-SVM had two main parameters that needed adjustment: ct and gamma. Therefore, various cost function values (ct) were implemented to optimize the model, and ct and gamma were 1.0 and 0.01, respectively, providing a good RPM.
- Random forest (RF) model: We have used various types of DT such as C4.5, J48 and RF. However, from this pool of decision trees, the RF performed well and tested further for the development of risk prediction models. RF as an ensemble method was used to create several DT from a set of features selected using the without replacement method. These DT divided the cases and controls into similar subgroups using the most important features. The voting process was used to predict the outcome of the features. A total of 300 DT with a depth of 6 and 3 randomly selected features provided us with a relatively better RPM.
2.5. Cross-Validation of ML-Based RPMs and Relative Feature Importance
3. Results
3.1. Baseline Conventional RPM and Relative Feature Importance
3.2. ML-Based RPMs and Their Performance
3.3. Performance Comparison between Baseline RPM and ML-Based RPMs
3.4. Partial Dependency Plots for Identification of Marginal Effects of Features
3.5. Relative Feature Importance through Best-Performed ML RPMs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Timmis, A.; Townsend, N.; Gale, C.; Grobbee, R.; Maniadakis, N.; Flather, M.; Wilkins, E.; Wright, L.; Vos, R.; Bax, J. European Society of Cardiology: Cardiovascular disease statistics 2017. Eur. Heart J. 2018, 39, 508–579. [Google Scholar] [CrossRef]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Zhao, D.; Liu, J.; Xie, W.; Qi, Y. Cardiovascular risk assessment: A global perspective. Nat. Rev. Cardiol. 2015, 12, 301. [Google Scholar] [CrossRef]
- Damen, J.A.; Hooft, L.; Schuit, E.; Debray, T.P.; Collins, G.S.; Tzoulaki, I.; Lassale, C.M.; Siontis, G.C.; Chiocchia, V.; Roberts, C. Prediction models for cardiovascular disease risk in the general population: Systematic review. BMJ 2016, 353, i2416. [Google Scholar] [CrossRef] [PubMed]
- Goff, D.C.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’donnell, C.J. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2935–2959. [Google Scholar] [CrossRef]
- Liu, J.; Hong, Y.; D’Agostino, R.B., Sr.; Wu, Z.; Wang, W.; Sun, J.; Wilson, P.W.; Kannel, W.B.; Zhao, D. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA 2004, 291, 2591–2599. [Google Scholar] [CrossRef]
- Kanjilal, S.; Rao, V.; Mukherjee, M.; Natesha, B.; Renuka, K.; Sibi, K.; Iyengar, S.; Kakkar, V.V. Application of cardiovascular disease risk prediction models and the relevance of novel biomarkers to risk stratification in Asian Indians. Vasc. Health Risk Manag. 2008, 4, 199. [Google Scholar] [CrossRef]
- Dalton, A.R.; Bottle, A.; Soljak, M.; Majeed, A.; Millett, C. Ethnic group differences in cardiovascular risk assessment scores: National cross-sectional study. Ethn. Health 2014, 19, 367–384. [Google Scholar] [CrossRef]
- Farzadfar, F. Cardiovascular disease risk prediction models: Challenges and perspectives. Lancet Glob. Health 2019, 7, e1288–e1289. [Google Scholar] [CrossRef]
- Hajifathalian, K.; Ueda, P.; Lu, Y.; Woodward, M.; Ahmadvand, A.; Aguilar-Salinas, C.A.; Azizi, F.; Cifkova, R.; Di Cesare, M.; Eriksen, L. A novel risk score to predict cardiovascular disease risk in national populations (Globorisk): A pooled analysis of prospective cohorts and health examination surveys. Lancet Diabetes Endocrinol. 2015, 3, 339–355. [Google Scholar] [CrossRef]
- Joseph, P.; Yusuf, S.; Lee, S.F.; Ibrahim, Q.; Teo, K.; Rangarajan, S.; Gupta, R.; Rosengren, A.; Lear, S.A.; Avezum, A. Prognostic validation of a non-laboratory and a laboratory based cardiovascular disease risk score in multiple regions of the world. Heart 2018, 104, 581–587. [Google Scholar] [CrossRef]
- Weng, S.F.; Reps, J.; Kai, J.; Garibaldi, J.M.; Qureshi, N. Can machine-learning improve cardiovascular risk prediction using routine clinical data? PLoS ONE 2017, 12, e0174944. [Google Scholar] [CrossRef] [PubMed]
- Sajeev, S.; Maeder, A. Cardiovascular risk prediction models: A scoping review. In Proceedings of the Australasian Computer Science Week Multiconference, Sydney, Australia, 29–31 January 2019; p. 21. [Google Scholar]
- Sajid, M.R.; Muhammad, N.; Zakaria, R.; Shahbaz, A.; Bukhari, S.A.C.; Kadry, S.; Suresh, A. Nonclinical Features in Predictive Modeling of Cardiovascular Diseases: A Machine Learning Approach. Interdiscip. Sci. Comput. Life Sci. 2021, 13, 201–211. [Google Scholar] [CrossRef]
- Sajid, M.R.; Muhammad, N.; Zakaria, R.; Shahbaz, A.; Nauman, A. Associated Factors of Cardiovascular Diseases in Pakistan: Assessment of Path Analyses Using Warp Partial Least Squares Estimation. Pak. J. Stat. Oper. Res. 2020, 16, 265–277. [Google Scholar] [CrossRef]
- McGorrian, C.; Yusuf, S.; Islam, S.; Jung, H.; Rangarajan, S.; Avezum, A.; Prabhakaran, D.; Almahmeed, W.; Rumboldt, Z.; Budaj, A. Estimating modifiable coronary heart disease risk in multiple regions of the world: The INTERHEART Modifiable Risk Score. Eur. Heart J. 2011, 32, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Papathanasiou, G.; Georgoudis, G.; Papandreou, M.; Spyropoulos, P.; Georgakopoulos, D.; Kalfakakou, V.; Evangelou, A. Reliability measures of the short International Physical Activity Questionnaire (IPAQ) in Greek young adults. Hellenic J. Cardiol. 2009, 50, 283–294. [Google Scholar] [PubMed]
- Ahmad, N.; Adam, S.I.M.; Nawi, A.M.; Hassan, M.R.; Ghazi, H.F. Abdominal obesity indicators: Waist circumference or waist-to-hip ratio in Malaysian adults population. Int. J. Prev. Med. 2016, 7, 82. [Google Scholar]
- Tan, M.C.; Ng, O.C.; Wong, T.W.; Joseph, A.; Chan, Y.M.; Hejar, A.R. Prevalence of metabolic syndrome in type 2 diabetic patients: A comparative study using WHO, NCEP ATP III, IDF and Harmonized definitions. Health 2013, 5, 1689. [Google Scholar] [CrossRef]
- Arruda, S.P.M.; da Silva, A.A.M.; Kac, G.; Goldani, M.Z.; Bettiol, H.; Barbieri, M.A. Socioeconomic and demographic factors are associated with dietary patterns in a cohort of young Brazilian adults. BMC Public Health 2014, 14, 654. [Google Scholar] [CrossRef]
- Kleinbaum, D.G.; Dietz, K.; Gail, M.; Klein, M.; Klein, M. Logistic Regression; Springer: Berlin/Heidelberg, Germany, 2002. [Google Scholar]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Elkan, C. Evaluating Classifiers; University of California: San Diego, CA, USA, 2012. [Google Scholar]
- Sajeev, S.; Champion, S.; Beleigoli, A.; Chew, D.; Reed, R.L.; Magliano, D.J.; Shaw, J.E.; Milne, R.L.; Appleton, S.; Gill, T.K. Predicting Australian adults at high risk of cardiovascular disease mortality using standard risk factors and machine learning. Int. J. Environ. Res. Public Health 2021, 18, 3187. [Google Scholar] [CrossRef]
- Boughorbel, S.; Jarray, F.; El-Anbari, M. Optimal classifier for imbalanced data using Matthews Correlation Coefficient metric. PLoS ONE 2017, 12, e0177678. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Vickers, A.J.; Cook, N.R.; Gerds, T.; Gonen, M.; Obuchowski, N.; Pencina, M.J.; Kattan, M.W. Assessing the performance of prediction models: A framework for some traditional and novel measures. Epidemiology 2010, 21, 128. [Google Scholar] [CrossRef] [PubMed]
- Leathart, T.; Frank, E.; Holmes, G.; Pfahringer, B. Probability calibration trees. In Proceedings of the Asian Conference on Machine Learning, Seoul, Korea, 15–17 November 2017; pp. 145–160. [Google Scholar]
- Hastie, T.; Tibshirani, R.; Friedman, J. The Elements of Statistical Learning: Data Mining, Inference, and Prediction; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2009. [Google Scholar] [CrossRef]
- De Oña, J.; Garrido, C. Extracting the contribution of independent variables in neural network models: A new approach to handle instability. Neural Comput. Appl. 2014, 25, 859–869. [Google Scholar] [CrossRef]
- Zhang, Z.; Beck, M.W.; Winkler, D.A.; Huang, B.; Sibanda, W.; Goyal, H. Opening the black box of neural networks: Methods for interpreting neural network models in clinical applications. Ann. Transl. Med. 2018, 6, 216. [Google Scholar] [CrossRef] [PubMed]
- Günther, F.; Wawro, N.; Bammann, K. Neural networks for modeling gene-gene interactions in association studies. BMC Genet. 2009, 10, 87. [Google Scholar] [CrossRef]
- Angraal, S.; Mortazavi, B.J.; Gupta, A.; Khera, R.; Ahmad, T.; Desai, N.R.; Jacoby, D.L.; Masoudi, F.A.; Spertus, J.A.; Krumholz, H.M. Machine learning prediction of mortality and hospitalization in heart failure with preserved ejection fraction. JACC Heart Fail. 2020, 8, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, S.; Yamashita, T.; Sakama, T.; Arita, T.; Yagi, N.; Otsuka, T.; Semba, H.; Kano, H.; Matsuno, S.; Kato, Y. Comparison of risk models for mortality and cardiovascular events between machine learning and conventional logistic regression analysis. PLoS ONE 2019, 14, e0221911. [Google Scholar] [CrossRef]
- Raghavendra, B.K.; Srivatsa, S.K. Evaluation of logistic regression and neural network model with sensitivity analysis on medical datasets. Int. J. Comput. Sci. Secur. 2011, 5, 503. [Google Scholar]
- Dreiseitl, S.; Ohno-Machado, L. Logistic regression and artificial neural network classification models: A methodology review. J. Biomed. Inform. 2002, 35, 352–359. [Google Scholar] [CrossRef]
- Kubat, M. An Introduction to Machine Learning; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Shalev-Shwartz, S.; Ben-David, S. Understanding Machine Learning: From Theory to Algorithms; Cambridge University Press: Cambridge, UK, 2014. [Google Scholar]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Safdar, N.F.; Bertone-Johnson, E.; Cordeiro, L.; Jafar, T.H.; Cohen, N.L. Do dietary patterns explain high prevalence of cardiovascular risk factors among Pakistani urban adults? A cross-sectional study. BMC Nutr. 2016, 2, 58. [Google Scholar] [CrossRef]
- Waseem, A.; Nafees, M.; Murtaza, G.; Sajjad, A.; Mehmood, Z.; Siddiqi, A.R. Salt toxicity (sodium intake): A serious threat to infants and children of Pakistan. Iran. J. Public Health 2014, 43, 1204. [Google Scholar]
- Iqbal, M.P. Trans fatty acids–A risk factor for cardiovascular disease. Pak. J. Med. Sci. 2014, 30, 194. [Google Scholar] [CrossRef] [PubMed]
- Jafar, T.H. Women in Pakistan have a greater burden of clinical cardiovascular risk factors than men. Int. J. Cardiol. 2006, 106, 348–354. [Google Scholar] [CrossRef]
- Jafar, T.H.; Jafary, F.H.; Jessani, S.; Chaturvedi, N. Heart disease epidemic in Pakistan: Women and men at equal risk. Am. Heart J. 2005, 150, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Liaquat, A.; Javed, Q. Current trends of cardiovascular risk determinants in Pakistan. Cureus 2018, 10, e3409. [Google Scholar] [CrossRef] [PubMed]
- Zubair, F.; Nawaz, S.K.; Nawaz, A.; Nangyal, H.; Amjad, N.; Khan, M.S. Prevalence of cardiovascular diseases in Punjab, Pakistan: A cross-sectional study. J. Public Health 2018, 26, 523–529. [Google Scholar] [CrossRef]
- Joshi, P.; Islam, S.; Pais, P.; Reddy, S.; Dorairaj, P.; Kazmi, K.; Pandey, M.R.; Haque, S.; Mendis, S.; Rangarajan, S. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 2007, 297, 286–294. [Google Scholar] [CrossRef]
- Zhang, Q.-j.; Gupta, K.C. Neural Networks for RF and Microwave Design (Book+ Neuromodeler Disk); Artech House, Inc.: London, UK, 2000. [Google Scholar]
- Sordo, M.; Zeng, Q. On sample size and classification accuracy: A performance comparison. In Proceedings of the International Symposium on Biological and Medical Data Analysis, Aveiro, Portugal, 10–11 November 2005; pp. 193–201. [Google Scholar]
- Liu, C.; Cheng, Y. An application of the support vector machine for attribute-by-attribute classification in cognitive diagnosis. Appl. Psychol. Meas. 2018, 42, 58–72. [Google Scholar] [CrossRef] [PubMed]


| Sr. No | Features | Frequency (%) |
|---|---|---|
| 1 | Gender (f2) | |
| Male | 312 (67.8) | |
| Female | 148 (32.2) | |
| 2 | Parental history of CVDs (f3) | |
| Yes | 78 (17.0) | |
| No | 382 (83.0) | |
| 3 | Diabetes mellitus (f4) | |
| Present | 115 (25%) | |
| Absent | 345(75%) | |
| 4 | Hypertension (f5) | |
| Present | 114 (24.8) | |
| Absent | 346 (75.2) | |
| 5 | Smoking history (f6) | |
| Smoker | 142 (30.9) | |
| Never smoker | 318 (69.1) | |
| 6 | Physical inactivity (f7) | |
| Low profile physical activity | 160 (34.8) | |
| Moderate to high physical activity | 300 (65.2) | |
| 7 | Self-reported general stress (f8) | |
| Sometimes to very stressful | 137 (29.8) | |
| Not at all to rarely stressful | 323 (70.2) | |
| 8 | Abdominal obesity (f9) | |
| Obese | 100 (21.7) | |
| Non-obese | 360 (78.3) | |
| 9 | Consumption of high-salt foods (f10) | |
| Consumption of high-salt foods or snacks ≥ 1 time a day | 194 (42.2) | |
| Consumption of high-salt foods or snacks < 1 time a day | 266 (57.8) | |
| 10 | Low fruit consumption (f11) | |
| <1-time fruit per day | 316 (68.7) | |
| ≥1-time fruit per day | 144 (31.3) | |
| 11 | Low vegetable consumption (f12) | |
| <1-time vegetables daily | 163 (35.4) | |
| ≥1-time vegetables daily | 297 (64.4) | |
| 12 | High fried foods/trans fats consumption(f13) | |
| Deep-fried foods/snacks/fast foods ≥ 3 times a week | 180 (39.1) | |
| Deep-fried foods/snacks/fast foods < 3 times a week | 280 (60.9) | |
| 13 | Red meat/poultry consumption (f14) | |
| ≥2 times daily | 58 (12.6) | |
| <2 times daily | 402 (87.4) | |
| 14 | Second-hand smoke exposure (f15) | |
| More than 1 h of passive smoke exposure per week | 226 (49.0) | |
| Less than 1 h of passive smoke exposure per week | 234 (51.0) |
| Models | ANN | Linear SVM | RBF-SVM | RF | Baseline RPM | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Confusion Matrix | Case | Control | Case | Control | Case | Control | Case | Control | Case | Control |
| Case | 178 | 52 | 186 | 44 | 185 | 45 | 185 | 45 | 185 | 45 |
| Control | 35 | 195 | 44 | 186 | 54 | 176 | 55 | 175 | 49 | 181 |
| Sensitivity | 0.780 | 0.809 | 0.804 | 0.804 | 0.804 | |||||
| Specificity | 0.848 | 0.809 | 0.765 | 0.761 | 0.787 | |||||
| Accuracy | 81.09 | 80.86 | 78.50 | 78.30 | 79.56 | |||||
| AUC | 0.871 | 0.864 | 0.853 | 0.856 | 0.859 | |||||
| Kappa-statistic | 0.622 | 0.617 | 0.570 | 0.565 | 0.592 | |||||
| RMSE | 0.378 | 0.382 | 0.392 | 0.386 | 0.389 | |||||
| NRI | 3.7% | 2.7% | −2.2% | −2.6% | ||||||
| Models * | Sensitivity | Specificity | Accuracy | AUC | Kappa-Statistic | RMSE | BS | Number of Criteria Fulfilled |
|---|---|---|---|---|---|---|---|---|
| ANN | −2.40% | 6.10% | 1.53% | 1.20% | 2.97% | 0.378 | 0.143 | 5/6 |
| Linear SVM | 0.50% | 2.20% | 1.30% | 0.50% | 2.50% | 0.382 | 0.146 | 6/6 |
| RBF-SVM | 0.00% | −2.20% | −1.06% | −0.60% | −2.20% | 0.392 | 0.154 | 0/6 |
| RF | 0.00% | −2.60% | −1.26% | −0.30% | −2.68% | 0.386 | 0.149 | 1/6 |
| 0.389 | 0.151 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sajid, M.R.; Almehmadi, B.A.; Sami, W.; Alzahrani, M.K.; Muhammad, N.; Chesneau, C.; Hanif, A.; Khan, A.A.; Shahbaz, A. Development of Nonlaboratory-Based Risk Prediction Models for Cardiovascular Diseases Using Conventional and Machine Learning Approaches. Int. J. Environ. Res. Public Health 2021, 18, 12586. https://doi.org/10.3390/ijerph182312586
Sajid MR, Almehmadi BA, Sami W, Alzahrani MK, Muhammad N, Chesneau C, Hanif A, Khan AA, Shahbaz A. Development of Nonlaboratory-Based Risk Prediction Models for Cardiovascular Diseases Using Conventional and Machine Learning Approaches. International Journal of Environmental Research and Public Health. 2021; 18(23):12586. https://doi.org/10.3390/ijerph182312586
Chicago/Turabian StyleSajid, Mirza Rizwan, Bader A. Almehmadi, Waqas Sami, Mansour K. Alzahrani, Noryanti Muhammad, Christophe Chesneau, Asif Hanif, Arshad Ali Khan, and Ahmad Shahbaz. 2021. "Development of Nonlaboratory-Based Risk Prediction Models for Cardiovascular Diseases Using Conventional and Machine Learning Approaches" International Journal of Environmental Research and Public Health 18, no. 23: 12586. https://doi.org/10.3390/ijerph182312586
APA StyleSajid, M. R., Almehmadi, B. A., Sami, W., Alzahrani, M. K., Muhammad, N., Chesneau, C., Hanif, A., Khan, A. A., & Shahbaz, A. (2021). Development of Nonlaboratory-Based Risk Prediction Models for Cardiovascular Diseases Using Conventional and Machine Learning Approaches. International Journal of Environmental Research and Public Health, 18(23), 12586. https://doi.org/10.3390/ijerph182312586







