Short Communication: Opportunities and Challenges for Early Person-Centered Care for Older Patients in Emergency Settings
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Approach
2.2. Data Collection and Analysis
2.3. Ethical Considerations
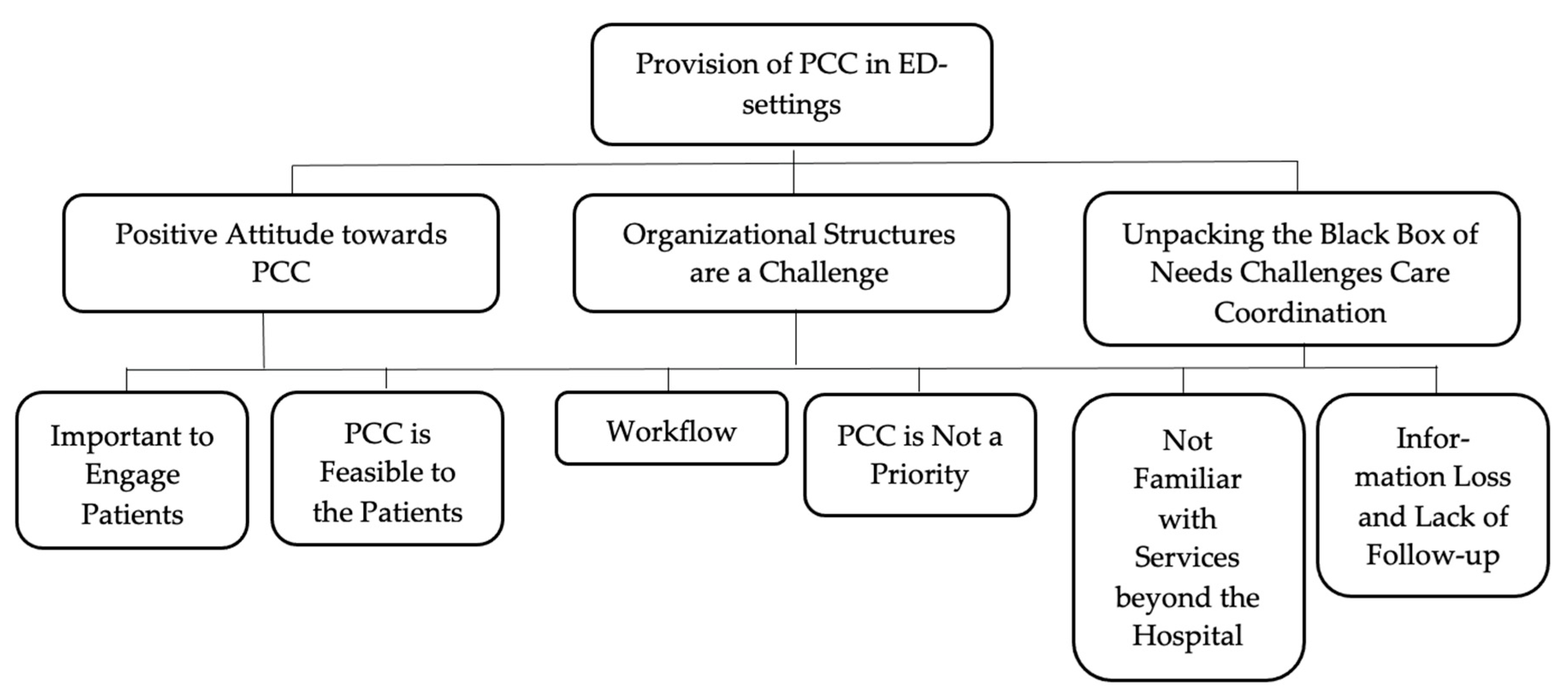
3. Results
3.1. Positive Attitude towards PCC
3.2. Organizational Structures Are a Challenge
3.3. Unpacking the Black Box of Needs Challenges Care Coordination
4. Discussion
4.1. Engagement of Patients and Long Hours of Waiting as Opportunities
4.2. Organizational Structures, Such as Workflow and Lack of Prioritizing PCC, as Challenges
4.3. Information Loss and Uncertainties with Services beyond the Hospital Setting Challenges Care Coordination
4.4. Future Directions
- Future studies into the feasibility and effects of structured approaches for providing PCC for older adults in ED settings are necessary.
- Future research into the identification of organizational models for PCC is necessary, including an exploration of how and when, during the ED visit, PCC is achievable and which health care professionals should be involved.
- Providing PCC for older adults in EDs requires staff education, geriatric-specific knowledge, and optimized coordination across sectors.
- Increased involvement of the geriatric nurses situated in the ED may facilitate PCC to a greater extent, both within the ED and across sectors.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. Department of Economic and Social Affairs Population Division. World Population Ageing 2019; United Nations: New York, NY, USA, 2020. [Google Scholar]
- Downing, A.; Wilson, R. Older people’s use of Accident and Emergency services. Age Ageing 2005, 34, 24–30. [Google Scholar] [CrossRef] [Green Version]
- Samaras, N.; Chevalley, T.; Samaras, D.; Gold, G. Older Patients in the Emergency Department: A Review. Ann. Emerg. Med. 2010, 56, 261–269. [Google Scholar] [CrossRef]
- Hunt, L.J. Improving care for older adults in the Emergency Department warrants greater investment in geriatric nursing-Stat! Geriatr. Nurs. 2020, 41, 345–346. [Google Scholar] [CrossRef]
- Perry, A.; Tejada, J.M.; Melady, D. An Approach to the Older Patient in the Emergency Department. Clin. Geriatr. Med. 2018, 34, 299–311. [Google Scholar] [CrossRef]
- Lennox, A.; Braaf, S.; Smit, D.V.; Cameron, P.; Lowthian, J.A. Caring for older patients in the emergency department: Health professionals’ perspectives from Australia—The Safe Elderly Emergency Discharge project. Emerg. Med. Australas. 2019, 31, 83–89. [Google Scholar] [CrossRef] [Green Version]
- Flynn, D.S.; Jennings, J.; Moghabghab, R.; Nancekivell, T.; Tsang, C.; Cleland, M.; Shipman-Vokner, K. Raising the bar of care for older people in Ontario emergency departments. Int. J. Older People Nurs. 2010, 5, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Häseler-Ouart, K.; Arefian, H.; Hartmann, M.; Kwetkat, A. Geriatric assessment for older adults admitted to the emergency department: A systematic review and meta-analysis. Exp. Gerontol. 2021, 144, 111184. [Google Scholar] [CrossRef] [PubMed]
- Lowthian, J.; Straney, L.D.; Brand, C.A.; Barker, A.L.; De Villiers Smit, P.; Newnham, H.; Hunter, P.; Smith, C.; Cameron, P.A. Unplanned early return to the emergency department by older patients: The Safe Elderly Emergency Department Discharge (SEED) project. Age Ageing 2016, 45, 255–261. [Google Scholar] [CrossRef] [Green Version]
- Aminzadeh, F.; Dalziel, W.B. Older Adults in the Emergency Department: A Systematic Review of Patterns of Use, Adverse Outcomes, and Effectiveness of Interventions. Ann. Emerg. Med. 2002, 39, 238–247. [Google Scholar] [CrossRef] [Green Version]
- Montori, V.M.; Kunneman, M.; Brito, J.P. Shared Decision Making and Improving Health Care. The Answer Is Not In. J. Am. Med. Assoc. 2017, 318, 617–618. [Google Scholar] [CrossRef] [PubMed]
- Barry, M.J.; Edgman-Levitan, S. Shared decision making—The pinnacle of patient-centered care. N. Engl. J. Med. 2012, 366, 780–781. [Google Scholar] [CrossRef] [Green Version]
- McCormack, B. A conceptual framework for person-centred practice with older people. Int. J. Nurs. Pract. 2003, 9, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century; The National Academies Press: Washington, DC, USA, 2001. [Google Scholar]
- Eklund, J.H.; Holmström, I.K.; Kumlin, T.; Kaminsky, E.; Skoglund, K.; Höglander, J.; Sundler, A.J.; Condén, E.; Meranius, M.S. “Same same or different?” A review of reviews of person-centered and patient-centered care. Patient Educ. Couns. 2019, 102, 3–11. [Google Scholar] [CrossRef]
- Ouchi, K.; George, N.; Schuur, J.D.; Aaronson, E.L.; Lindvall, C.; Bernstein, E.; Sudore, R.L.; Schonberg, M.A.; Block, S.D.; Tulsky, J.A. Goals-of-Care Conversations for Older Adults With Serious Illness in the Emergency Department: Challenges and Opportunities. Ann. Emerg. Med. 2019, 74, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Harding, S. Comprehensive geriatric assessment in the emergency department. Age Ageing 2020, 49, 936–938. [Google Scholar] [CrossRef] [PubMed]
- Cullison, K.; Carpenter, C.R.; Milne, W.K. Hot Off the Press: Use of Shared Decision-making for Management of Acute Musculoskeletal Pain in Older Adults Discharged from the Emergency Department. Acad. Emerg. Med. 2016, 23, 956–958. [Google Scholar] [CrossRef] [Green Version]
- Probst, M.A.; Tschatscher, C.F.; Lohse, C.M.; Bellolio, F.M.; Hess, E.P. Factors Associated with Patient Involvement in Emergency Care Decisions: A Secondary Analysis of the Chest Pain Choice Multicenter Randomized Trial. Acad. Emerg. Med. 2018, 25, 1107–1117. [Google Scholar] [CrossRef] [Green Version]
- Schoenfeld, E.M.; Kanzaria, H.K.; Quigley, D.D.; St Marie, P.; Nayyar, N.; Sabbagh, S.H.; Gress, K.L.; Probst, M.A. Patient Preferences regarding Shared Decision-making in the Emergency Department—Findings from a multi-site survey. Acad. Emerg. Med. 2018, 25, 1118–1128. [Google Scholar] [CrossRef] [Green Version]
- Pham, J.C.; Trueger, S.N.; Hilton, J.; Khare, R.K.; Smith, J.P.; Bernstein, S.L. Interventions to Improve Patient-centered Care During Times of Emergency Department Crowding. Acad. Emerg. Med. 2011, 18, 1289–1294. [Google Scholar] [CrossRef]
- Saidinejad, M. The Patient-Centered Emergency Department. Adv. Pediatr. 2018, 65, 105–120. [Google Scholar] [CrossRef]
- Huijg, J.M.; van Delden, A.L.; van der Ouderaa, F.J.; Westendorp, R.G.; Joris, P.; Lindenberg, J. Being Active, Engaged, and Healthy: Older Persons’ Plans and Wishes to Age Successfully. J. Gerontol. B Psychol. Sci. Soc. Sci. 2016, 72, 228–236. [Google Scholar] [CrossRef] [Green Version]
- Bernard, R.H. Research Methods in Anthropology: Qualitative and Quantitative Approaches, 4th ed.; AltaMira Press: New York, NY, USA, 2006; pp. 310–346. [Google Scholar]
- Spradley, J. Participant Observation; Waveland Press Inc.: Long Grove, IL, USA, 2016; p. 195. [Google Scholar]
- Malterud, K. Qualitative research: Standards, challenges, and guidelines. Qual. Res. Ser. 2001, 358, 483–488. [Google Scholar] [CrossRef]
- Creswell, J.; Clark, V.L. Designing and Conducting Mixed Methods Research; Sage Publications Inc.: Los Angeles, CA, USA, 2018. [Google Scholar]
- Attride-Stirling, J. Thematic networks: An analytic tool for qualitative research. Qual. Res. 2001, 1, 385–405. [Google Scholar] [CrossRef]
- Hogan, T.M.; Losman, E.D.; Carpenter, C.R.; Sauvigne, K.; Irmiter, C.; Emanuel, L.; Leipzig, R.M. Development of Geriatric Competencies for Emergency Medicine Residents Using an Expert Consensus Process. Acad. Emerg. Med. 2010, 17, 316–324. [Google Scholar] [CrossRef] [Green Version]
- Flynn, D.; Knoedler, M.A.; Hess, E.P.; Murad, M.H.; Erwin, P.J.; Montori, V.M.; Thomson, R.G. Engaging patients in Health Care Decisions in the Emergency Department through Shared Decision-making: A Systematic Review. Acad. Emerg. Med. 2012, 19, 959–967. [Google Scholar] [CrossRef] [PubMed]
- Ekman, I.; Swedberg, K.; Taft, C.; Lindseth, A.; Norberg, A.; Brink, E.; Carlsson, J.; Dahlin-Ivanoff, S.; Johansson, I.L.; Kjellgren, K. Person-centered care—Ready for prime time. Eur. J. Cardiovasc. Nurs. 2011, 10, 248–251. [Google Scholar] [CrossRef]
- Bachnick, S.; Ausserhofer, D.; Baernholdt, M.; Simon, M. Patient-centered care, nurse work environment and implicit rationing of nursing care in Swiss acute care hospitals: A cross-sectional multi-center study. Int. J. Nurs. Stud. 2018, 81, 98–106. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Costello, D.M.; Naik, A.D.; Davenport, C.; Hernandez-Bigos, K.; Van Liew, J.R.; Esterson, J.; Kiwak, E.; Dindo, L. Outcome Goals and Health Care Preferences of Older Adults with Multiple Chronic Conditions. JAMA Netw. Open 2021, 4, e211271. [Google Scholar] [CrossRef]
- Kirk, J.W.; Sivertsen, D.M.; Petersen, J.; Nilsen, P.; Petersen, H.V. Barriers and facilitators for implementing a new screening tool in an emergency department: A qualitative study applying the Theoretical Domains Framework. J. Clin. Nurs. 2016, 25, 2786–2797. [Google Scholar] [CrossRef]
- Hwang, U.; Morrison, S.R. The Geriatric Emergency Department. J. Am. Geriatr. Soc. 2007, 55, 1873–1876. [Google Scholar] [CrossRef]
- Gonçalves-Bradley, D.C.; Lannin, N.A.; Clemson, L.M.; Cameron, I.D.; Shepperd, S. Discharge planning from hospital. Cochrane Database Syst. Rev. 2016, CD000313. [Google Scholar] [CrossRef] [PubMed]
| Examples | ||
|---|---|---|
| Emerging Theme | Excerpts from Interviews and Informal Interviews | Clinical Example from Fieldwork |
| Positive Attitude towards PCC - Important to Engage Patients and PCC is Feasible to the Patients | “(…) I find it really important to try to engage the patients to uncover how we may accommodate their needs in the best possible way according to the resources currently available.” (Nurse 2). “[Using a PCC approach] We would get to know the patients in another way than usual. Our regular questions differ from nurse to nurse: it all depends on what you ask and what you respond to. (…) So, it could be beneficial if we became more aware of the issues and payed more attention to the older adults.” (Nurse 6). “So, I believe that it [PCC conversations] is feasible for the patients. If some of the things that are the most important to them can be fulfilled—then I think it can create better care and maybe prevent some things, such as hospitalization. Maybe they [the patients] can better cater to some of the things that they are encouraged to do during hospitalization following a PCC conversation (…)”. (Nurse 2). | Multiple older ED patients are staying in their respective beds for longer periods, enabling unhurried conversations without interruption from either nurses, physicians, or other health care professionals (Field notes, ED, November 2019). Yet again my experience suggests that PCC conversations would be relevant for several older ED patients who often have the physical and mental ability to engage and participate in a holistic conversation (Field notes, ED, November 2019). |
| Organizational Structures are a Challenge - Workflow and PCC is Not a Priority | “We do not only have one patient—we also have six others and different emergency rooms we must run to. And we don’t know what we’ll receive in five minutes. We have no scheduled tasks. (…) For us, it’s about prioritizing. I can easily postpone a blood glucose test if another patient needs my help more. I can easily postpone giving medicine until noon if some of my colleagues need help with something. So, it [PCC conversations] is not going to be prioritized—that’s what I’m trying to say.” (Nurse 4). | Entering the ED, I am met by a busy hallway with nurses walking back and forth. Pharmacists are walking from patient to patient with medication. Physicians are visiting patients and entering the staff office, where they confer with colleagues and write up medical records (Field notes, ED, September 2019). Today, the temporality is high—the nurses have several additional tasks beyond acute treatment, and less time to write up medical records. Little time is spent with the patients (Field notes, ED, November 2019). Person-centered care is not a priority. Acute treatment, on the other hand, is a priority. The nurse that I am accompanying today tells me that she asks herself: “Will this task save lives?”—her priorities are the medical tasks that can ultimately save lives (Field notes, ED, December 2019). |
| Unpacking the Black Box of Needs Challenges Care Coordination - Not Familiar with Services beyond the Hospital and Information Loss and Lack of Follow-up | “Someone has to follow up on the needs that we uncover [during PCC conversations]. And in the emergency department we do not know exactly what the municipality can offer and what can be accommodated (…).” (Nurse 3). “The municipality must accommodate it [the needs uncovered]. (…). And there is a communicative path between us and them [the municipality] (…) that’s a lot of work, and there are also a lot of things that can go wrong. And if we uncover unmet needs and say: ‘Well, we will pass this on to the municipality, if it’s okay with you?’, and then we pass it on, and the municipality cannot accommodate it, then there might be some disappointment associated with it.” (Nurse 2). | The geriatric nurses express concerns related to time spent when entering PCC conversations and further doubts as to whether the conversations with the older patients will reveal needs that they cannot accommodate. They express concern that they are not familiar with the existing services of the municipality, which complicates referral to cross-sectoral services (Field notes, geriatric team, September 2019). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jensen, A.N.; Andersen, O.; Gamst-Jensen, H.; Kristiansen, M. Short Communication: Opportunities and Challenges for Early Person-Centered Care for Older Patients in Emergency Settings. Int. J. Environ. Res. Public Health 2021, 18, 12526. https://doi.org/10.3390/ijerph182312526
Jensen AN, Andersen O, Gamst-Jensen H, Kristiansen M. Short Communication: Opportunities and Challenges for Early Person-Centered Care for Older Patients in Emergency Settings. International Journal of Environmental Research and Public Health. 2021; 18(23):12526. https://doi.org/10.3390/ijerph182312526
Chicago/Turabian StyleJensen, Andrea N., Ove Andersen, Hejdi Gamst-Jensen, and Maria Kristiansen. 2021. "Short Communication: Opportunities and Challenges for Early Person-Centered Care for Older Patients in Emergency Settings" International Journal of Environmental Research and Public Health 18, no. 23: 12526. https://doi.org/10.3390/ijerph182312526
APA StyleJensen, A. N., Andersen, O., Gamst-Jensen, H., & Kristiansen, M. (2021). Short Communication: Opportunities and Challenges for Early Person-Centered Care for Older Patients in Emergency Settings. International Journal of Environmental Research and Public Health, 18(23), 12526. https://doi.org/10.3390/ijerph182312526






