How Phantom Networks, Provider Qualities, and Poverty Sway Medicaid Dental Care Access: A Geospatial Analysis of Manhattan
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection and Processing
2.2. Statistical and Geospatial Analysis
3. Results
3.1. The Verdict for MCO Directories
3.2. What Happened When Filtering for Patient-Centered Providers?
3.3. Is Poverty Associated with the Medicaid Dental Supply?
3.4. Is Poverty Associated with Phantom Networks?
4. Discussion
4.1. Insights and Future Research
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Taylor, G.; Borgnakke, W. Periodontal disease: Associations with diabetes, glycemic control and complications. Oral Dis. 2008, 14, 191–203. [Google Scholar] [CrossRef]
- Bingham, C.O.; Moni, M. Periodontal disease and rheumatoid arthritis. Curr. Opin. Rheumatol. 2013, 25, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.S.; Joshipura, K.; Giovannucci, E.; Michaud, D.S. A review of the relationship between tooth loss, periodontal disease, and cancer. Cancer Causes Control 2008, 19, 895–907. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, L.L.; Fu, R.; Buckley, D.I.; Freeman, M.; Helfand, M. Periodontal Disease and Coronary Heart Disease Incidence: A Systematic Review and Meta-analysis. J. Gen. Intern. Med. 2008, 23, 2079–2086. [Google Scholar] [CrossRef] [PubMed]
- Holmlund, A.; Lampa, E.; Lind, L. Oral health and cardiovascular disease risk in a cohort of periodontitis patients. Atherosclerosis 2017, 262, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Suh, J.S.; Kim, S.; Boström, K.I.; Wang, C.Y.; Kim, R.H.; Park, N.H. Periodontitis-induced systemic inflammation exacerbates atherosclerosis partly via endothelial–mesenchymal transition in mice. Int. J. Oral Sci. 2019, 11, 21. [Google Scholar] [CrossRef] [PubMed]
- Slots, J. Periodontology: Past, present, perspectives. Periodontology 2000 2013, 62, 7–19. [Google Scholar] [CrossRef]
- Friedman, P.K.; Lamster, I.B. Tooth loss as a predictor of shortened longevity: Exploring the hypothesis. Periodontology 2000 2016, 72, 142–152. [Google Scholar] [CrossRef]
- Murrin, S. Most Children with Medicaid in Four States Are Not Receiving Required Dental Services; Technical Report; Office of Inspector General: Washington, DC, USA, 2016.
- Ahlberg, J.; Tuominen, R.; Murtomaa, H. Periodontal status among male industrial workers in southern Finland with or without access to subsidized dental care. Acta Odontol. Scand. 1996, 54, 166–170. [Google Scholar] [CrossRef]
- Axelsson, P.; Nystrom, B.; Lindhe, J. The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J. Clin. Periodontol. 2004, 31, 749–757. [Google Scholar] [CrossRef]
- Chapple, I.L.C.; Van der Weijden, F.; Doerfer, C.; Herrera, D.; Shapira, L.; Polak, D.; Madianos, P.; Louropoulou, A.; Machtei, E.; Donos, N.; et al. Primary prevention of periodontitis: Managing gingivitis. J. Clin. Periodontol. 2015, 42, S71–S76. [Google Scholar] [CrossRef] [PubMed]
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Hinton, E.; Paradise, J. Access to Dental Care in Medicaid: Spotlight on Nonelderly Adults; Technical Report; The Kaiser Commission on Medicaid and the Uninsured: Menlo Park, CA, USA, 2016. [Google Scholar]
- Lipson, D.J.; Libersky, J.; Bradley, K.; Lewis, C.; Siegwarth, A.W.; Lester, R. Promoting Access in Medicaid and CHIP Managed Care: A Toolkit for Ensuring Provider Network Adequacy and Service Availability; Technical Report; U.S. Centers for Medicare and Medicaid Services (CMS): Baltimore, MD, USA, 2017.
- Daw, J. Fighting the phantoms of managed care: Legislation in California and a legal case in Virginia address managed care’s practice of maintaining phantom provider panels. J. Monit. Psychol. 2002, 33, 21. [Google Scholar]
- Holstein, R.; Paul, D.P. ‘Phantom Networks’ of Managed Behavioral Health Providers: An Empirical Study of Their Existence and Effect on Patients in Two New Jersey Counties. Hosp. Top. 2012, 90, 65–73. [Google Scholar] [CrossRef]
- Barry, C.L.; Venkatesh, M.; Busch, S.H. Assessing New Patient Access to Mental Health Providers in HMO Networks. Psychiatr. Serv. 2008, 59, 1413–1418. [Google Scholar] [CrossRef]
- Levinson, D.R. Access to Care: Provider Availability in Medicaid Managed Care; Technical Report; U.S. Office of Inspector General (OIG): Washington, DC, USA, 2014.
- Resneck, J.S.; Quiggle, A.; Liu, M.; Brewster, D.W. The Accuracy of Dermatology Network Physician Directories Posted by Medicare Advantage Health Plans in an Era of Narrow Networks. JAMA Dermatol. 2014, 150, 1290. [Google Scholar] [CrossRef] [PubMed]
- Haeder, S.F.; Weimer, D.L.; Mukamel, D.B. Secret Shoppers Find Access To Providers And Network Accuracy Lacking For Those in Marketplace And Commercial Plans. Health Aff. 2016, 35, 1160–1166. [Google Scholar] [CrossRef]
- U.S. Centers for Medicare and Medicaid Services CMS. Online Provider Directory Review Report: First Round; Technical Report; U.S. Centers for Medicare and Medicaid Services (CMS): Baltimore, MD, USA, 2017.
- U.S. Centers for Medicare and Medicaid Services CMS. Online Provider Directory Review Report: Second Round; Technical Report; U.S. Centers for Medicare and Medicaid Services (CMS): Baltimore, MD, USA, 2018.
- U.S. Centers for Medicare and Medicaid Services CMS. Online Provider Directory Review Report: Third Round; Technical Report; U.S. Centers for Medicare and Medicaid Services (CMS): Baltimore, MD, USA, 2018.
- Health Policy Institute HPI. The Oral Health Care System: A State-by-State Analysis; Technical Report; American Dental Association (ADA): Chicago, IL, USA, 2015. [Google Scholar]
- Vujicic, M. Is the number of Medicaid providers really that important? J. Am. Dent. Assoc. 2016, 147, 221–223. [Google Scholar] [CrossRef][Green Version]
- Mofidi, M.; Rozier, R.G.; King, R.S. Problems with Access to Dental Care for Medicaid-Insured Children: What Caregivers Think. Am. J. Public Health 2002, 92, 53–58. [Google Scholar] [CrossRef]
- Scott, M.K.; Bingham, D.; Doherty, M. The Good Practice: Treating Underserved Dental Patients While Staying Afloat; Technical Report; California HealthCare Foundation: Oakland, CA, USA, 2008. [Google Scholar]
- Institute of Medicine. Transforming Health Care Schedulingand Access: Getting to Now; The National Academies Press: Washington, DC, USA, 2015. [Google Scholar]
- Meeske, J.A.; Brickhouse, T.H.; Casamassimo, P.; Wright, M.R.; Litch, C.S.; Essling, M. Pediatric Dentist Toolkit for Seeing Patients with Medicaid: Changing Children’s Lives One Smile at a Time; Technical Report; American Academy of Pediatric Dentistry (AAPD): Chicago, IL, USA, 2017. [Google Scholar]
- Oral Health Technical Advisory Group. Policy Issues the Delivery of Dental Services to Medicaid Children and their Families; Technical Report; U.S. Centers for Medicare and Medicaid Services (CMS): Baltimore, MD, USA, 2008.
- New York State Education Department (NYSED). NYS Dentistry: License Requirements. 2020. Available online: http://www.op.nysed.gov/prof/dent/dentlic.htm (accessed on 20 November 2021).
- New York State Department of Health NYSDOH. New York State Medicaid Program Dental Policy and Procedure Code Manual; Technical Report; eMedNY: Rensselaer, NY, USA, 2019. [Google Scholar]
- Chinn, C.H.; Rossy, S.; Best, E. Analysis of InsureKidsNow.gov dental providers in New York State. Pediatr. Dent. 2013, 35, 451–455. [Google Scholar]
- McKernan, S.C.; Reynolds, J.C.; Kuthy, R.A.; Kateeb, E.T.; Adrianse, N.B.; Damiano, P.C. Factors Affecting Iowa Dentist Participation in Medicaid; Capacity of the Private Oral Health Safety Net; Technical Report; University of Lowa: Iowa City, IA, USA, 2013. [Google Scholar] [CrossRef]
- Chaiyachati, K.H.; Hom, J.K.; Wong, C.; Nasseh, K.; Chen, X.; Beggin, A.; Zygmunt, E.; Vujicic, M.; Grande, D. Access to primary and dental care among adults newly enrolled in Medicaid. Am. J. Manag. Care 2019, 25, 135–139. [Google Scholar] [PubMed]
- Reynolds, J.C.; McKernan, S.C.; Damiano, P.C.; Kuthy, R.A. A tale of two public dental benefit programs: Iowa dentist participation in traditional Medicaid versus a Medicaid expansion program. BMC Oral Health 2019, 19, 89. [Google Scholar] [CrossRef]
- McKernan, S.C.; Reynolds, J.C.; Singhal, A.; Kuthy, R.; Damiano, P.C. Access to Dental Care and the Oral Health Safety Net; Technical Report; University of Lowa: Iowa City, IA, USA, 2013. [Google Scholar] [CrossRef]
- Baird, M.; Baird, M.; Vesely, J. Access to Dental Providers in Pennsylvania: Exploration of the County-Level Distribution of Dental Providers and Populations in 2013; RAND Corporation: Santa Monica, CA, USA, 2016. [Google Scholar] [CrossRef]
- Nasseh, K.; Eisenberg, Y.; Vujicic, M. Geographic access to dental care varies in Missouri and Wisconsin. J. Public Health Dent. 2017, 77, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Maxey, H.L.; Norwood, C.W.; Vaughn, S.X.; Wang, Y.; Marsh, S.; Williams, J. Dental safety net capacity: An innovative use of existing data to measure dentists’ clinical engagement in state Medicaid programs. J. Public Health Dent. 2018, 78, 266–274. [Google Scholar] [CrossRef]
- Health Policy Institute HPI. Geographic Access to Dental Care: New York; Technical Report; American Dental Association (ADA): Chicago, IL, USA, 2019. [Google Scholar]
- Garg, S.; Rubin, T.; Jasek, J.; Weinstein, J.; Helburn, L.; Kaye, K. How willing are dentists to treat young children? J. Am. Dent. Assoc. 2013, 144, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.O.R. Reducing Disparities in Dental Care for Low-income Hispanic Children. J. Health Care Poor Underserved 2005, 16, 431–443. [Google Scholar] [CrossRef]
- Okunseri, C.; Okunseri, E.; Fischer, M.C.; Sadeghi, S.N.; Xiang, Q.; Szabo, A. Nontraumatic dental condition-related visits to emergency departments on weekdays, weekends and night hours: Findings from the National Hospital Ambulatory Medical Care Survey. Clin. Cosmet. Investig. Dent. 2013, 5, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Wall, T.; Vujicic, M. Emergency Department Use for Dental Conditions Continues to Increase; Technical Report; American Dental Association (ADA): Chicago, IL, USA, 2015. [Google Scholar]
- Cully, J.L.; Doyle, M.; Thikkurissy, S. Impact of an Alternative Hours Dental Clinic for Adolescents. Pediatr. Dent. 2018, 40, 288–290. [Google Scholar]
- Futuredontics. What Dental Patients Want; Technical Report; Futuredontics Inc.: Los Angeles, CA, USA, 2015. [Google Scholar]
- Lincoln Finanical Group. Lincoln Financial Group Dental Study Informs Both Dentists and Employers of Consumers’ Needs and Wants; Technical Report; Lincoln National Corporation: Radnor, PA, USA, 2017. [Google Scholar]
- Susi, L.; Mascarenhas, A.K. Using a geographical information system to map the distribution of dentists in Ohio. J. Am. Dent. Assoc. 2002, 133, 636–642. [Google Scholar] [CrossRef]
- Saman, D.M.; Arevalo, O.; Johnson, A.O. The dental workforce in Kentucky: Current status and future needs. J. Public Health Dent. 2010, 70, 188–196. [Google Scholar] [CrossRef]
- Continelli, T.; Dionne, M.; Uangelier, M.; Moore, J. A Profile of Active Dentists in New York; Technical Report; Center for Health Workforce Studies: Rensselaer, NY, USA, 2013. [Google Scholar]
- Health Policy Institute HPI. Projected Supply of Dentists: New York; Technical Report; American Dental Association (ADA): Chicago, IL, USA, 2017. [Google Scholar]
- Munson, B.; Vujicic, M. Supply of Full-Time Equivalent Dentists in the U.S. Expected to Increase Steadily; Technical Report; American Dental Association (ADA): Chicago, IL, USA, 2018. [Google Scholar]
- Dumas, S.A.; Polk, D. Pediatric dental clinic location and utilization in a high-resource setting. J. Public Health Dent. 2015, 75, 183–190. [Google Scholar] [CrossRef]
- McKernan, S.C.; Pooley, M.J.; Momany, E.T.; Kuthy, R.A. Travel burden and dentist bypass among dentally insured children. J. Public Health Dent. 2016, 76, 220–227. [Google Scholar] [CrossRef]
- Cao, S.; Gentili, M.; Griffin, P.M.; Griffin, S.O.; Serban, N. Disparities in Preventive Dental Care Among Children in Georgia. Prev. Chronic Dis. 2017, 14, 170176. [Google Scholar] [CrossRef]
- Edward, J.; Biddle, D.J. Using Geographic Information Systems (GIS) to Examine Barriers to Healthcare Access for Hispanic and Latino Immigrants in the U.S. South. J. Racial Ethn. Health Disparities 2017, 4, 297–307. [Google Scholar] [CrossRef]
- Wehby, G.L.; Shane, D.M.; Joshi, A.; Momany, E.; Chi, D.L.; Kuthy, R.A.; Damiano, P.C. The Effects of Distance to Dentists and Dentist Supply on Children’s Use of Dental Care. Health Serv. Res. 2017, 52, 1817–1834. [Google Scholar] [CrossRef] [PubMed]
- McKernan, S.; Reynolds, J.; Ingleshwar, A.; Pooley, M.; Kuthy, R.; Damiano, P. Transportation Barriers and Use of Dental Services among Medicaid-Insured Adults. JDR Clin. Transl. Res. 2018, 3, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, F. Measures of Spatial Accessibility to Health Care in a GIS Environment: Synthesis and a Case Study in the Chicago Region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef]
- Luo, W. Using a GIS-based floating catchment method to assess areas with shortage of physicians. Health Place 2004, 10, 1–11. [Google Scholar] [CrossRef]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef]
- Kim, Y.; Byon, Y.J.; Yeo, H. Enhancing healthcare accessibility measurements using GIS: A case study in Seoul, Korea. PLoS ONE 2018, 13, e0193013. [Google Scholar] [CrossRef] [PubMed]
- Center for Health Care Strategies CHCS. Medicaid Adult Benefits: An Overview; Technical Report; Center for Health Care Strategies, Inc. (CHCS): Hamilton, NJ, USA, 2019. [Google Scholar]
- National Association of Dental Plans NADP. NADP Provider Networks and Accessibility Requirements by State; Technical Report; National Association of Dental Plans (NADP): Dallas, TX, USA, 2017. [Google Scholar]
- New York State Department of Financial Services NYSDFS. Network Adequacy Standards and Guidance. 2019. Available online: https://www.dfs.ny.gov/apps_and_licensing/health_insurers/network_adequacy_oon_standards_guidance (accessed on 20 November 2021).
- U.S. Census Bureau. QuickFacts: New York County (Manhattan Borough), New York. 2019. Available online: https://www.census.gov/quickfacts/fact/table/newyorkcountynewyork/SEX255219 (accessed on 20 November 2021).
- U.S. Census Bureau. QuickFacts: New York. 2019. Available online: https://www.census.gov/quickfacts/NY (accessed on 20 November 2021).
- U.S. Census Bureau. QuickFacts: United States. 2019. Available online: https://www.census.gov/quickfacts/fact/table/US/PST045219 (accessed on 20 November 2021).
- Austensen, M.; Been, V.; O’Regan, K.M.; Rosoff, S.; Yager, J. 2016 Focus: Poverty in New York City; Technical Report; NYU Furman Center: New York, NY, USA, 2016. [Google Scholar]
- Mertz, E.A.; Grumbach, K. Identifying Communities with Low Dentist Supply in California. J. Public Health Dent. 2001, 61, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Borrell, L.N.; Northridge, M.E.; Miller, D.B.; Golembeski, C.A.; Spielman, S.E.; Sclar, E.D.; Lamster, I.B. Oral health and health care for older adults: A spatial approach for addressing disparities and planning services. Spec. Care Dent. 2006, 26, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Paradise, J. Improving Access to Oral Health Care for Adults in Medicaid: Key Themes from a Policy Roundtable; Technical Report; The Henry J. Kaiser Family Foundation: Menlo Park, CA, USA, 2016; Available online: https://www.kff.org/report-section/improving-access-to-oral-health-care-for-adults-in-medicaid-key-themes-from-a-policy-roundtable-report/ (accessed on 20 November 2021).
- Health Policy Institute HPI. State-Level Dentist Workforce Projections Data and Methods; Technical Report; American Dental Association (ADA): Chicago, IL, USA, 2017. [Google Scholar]
- Brown, E.J.; Polsky, D.; Barbu, C.M.; Seymour, J.W.; Grande, D. Racial Disparities In Geographic Access To Primary Care in Philadelphia. Health Aff. 2016, 35, 1374–1381. [Google Scholar] [CrossRef]
- Bruns, D. Random Number Weighted Probability. 2019. Available online: https://exceljet.net/formula/random-number-weighted-probability (accessed on 20 November 2021).
- Environmental Systems Research Institute (ESRI). Create and Use a Network Dataset with Public Transit Data. 2019. Available online: https://pro.arcgis.com/en/pro-app/help/analysis/networks/create-and-use-a-network-dataset-with-public-transit-data.htm (accessed on 20 November 2021).
- Transit Screen. New York City MTA. 2019. Available online: https://transitfeeds.com/p/mta (accessed on 20 November 2021).
- BIG APPLE. LION Single Line Street Base Map. 2019. Available online: https://www1.nyc.gov/site/planning/data-maps/open-data/dwn-lion.page (accessed on 20 November 2021).
- Manson, S.; Schroeder, J.; Riper, D.V. IPUMS National Historical Geographic Information System: Version 14.0 [Database]; IPUMS: Minneapolis, MN, USA, 2019. [Google Scholar] [CrossRef]
- California Department of Health Care Services (DHCS). Network Adequacy. 2019. Available online: https://www.dhcs.ca.gov/formsandpubs/Pages/NetworkAdequacy.aspx (accessed on 20 November 2021).
- Vo, A. Two-Step Floating Catchment. 2015. Available online: https://agis.maps.arcgis.com/home/item.html?id=4fe25317dd9c45c1ba5100680991f22f (accessed on 20 November 2021).
- Marin, M. One-Sample t Test & Confidence Interval in R with Example: R Tutorial 4.1. 2013. Available online: https://www.youtube.com/watch?v=kvmSAXhX9Hs (accessed on 20 November 2021).
- Kassambara, A. Correlation Test Between Two Variables in R. 2017. Available online: http://www.sthda.com/english/wiki/correlation-test-between-two-variables-in-r (accessed on 20 November 2021).
- Kassambara, A. Normality Test in R. 2017. Available online: http://www.sthda.com/english/wiki/normality-test-in-r (accessed on 20 November 2021).
- Chok, N.S. Pearson’s Versus Spearman’s and Kendall’s Correlation Coefficients for Continuous Data. Master’s Thesis, University of Pittsburgh, Pittsburgh, PA, USA, 2010. Available online: http://d-scholarship.pitt.edu/8056/1/Chokns_etd2010.pdf (accessed on 20 November 2021).
- Lund, A.; Lund, M. Kendall’s Tau-b Using SPSS Statistics. 2018. Available online: https://statistics.laerd.com/spss-tutorials/kendalls-tau-b-using-spss-statistics.php (accessed on 20 November 2021).
- Tay, K. Spearman’s Rho and Kendall’s Tau. 2019. Available online: https://statisticaloddsandends.wordpress.com/2019/07/08/spearmans-rho-and-kendalls-tau/ (accessed on 20 November 2021).
- Center on Urban Poverty and Community Development. Census Poverty and Income Indicators; Technical Report; Case Western Reserve University: Cleveland, OH, USA, 2006. [Google Scholar]
- Anselin, L.; Syabri, I.; Kho, Y. GeoDa: An Introduction to Spatial Data Analysis. Geogr. Anal. 2006, 38, 5–22. [Google Scholar] [CrossRef]
- U.S. Health Resources and Service Adiministration (HRSA). What is Shortage Designation? 2021. Available online: https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation (accessed on 20 November 2021).
- U.S. Census Bureau. How the Census Bureau Measures Poverty. 2021. Available online: https://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html (accessed on 20 November 2021).
- New York State Department of Financial Services (NYSDFS). Out-of-Network Law (OON) Guidance (Part H of Chapter 60 of the Laws of 2014). 2015. Available online: https://www.dfs.ny.gov/apps_and_licensing/health_insurers/outofnetwork_law_oon_guidance (accessed on 20 November 2021).
- McAndrew, C. Improving the Accuracy of Health Insurance Plans’ Provider Directories; Technical Report; Families USA: Washington, DC, USA, 2015. [Google Scholar]
- Medicaid and CHIP Payment and Access Commission MACPAC. Managed Care’s Effect on Outcomes; Technical Report; Medicaid and CHIP Payment and Access Commission (MACPAC): Washington, DC, USA, 2019.
- Berenson, R.A.; Rich, E.C. US Approaches to Physician Payment: The Deconstruction of Primary Care. J. Gen. Intern. Med. 2010, 25, 613–618. [Google Scholar] [CrossRef]
- Sparer, M. Medicaid Managed Care: Costs, Access, and Quality of Care; Technical Report; Robert Wood Johnson Foundation: Princeton, NJ, USA, 2012. [Google Scholar]
- Duggan, M.; Hayford, T. Has the Shift to Managed Care Reduced Medicaid Expenditures? Evidence from State and Local-Level Mandates. J. Policy Anal. Manag. 2013, 32, 505–535. [Google Scholar] [CrossRef]
- Green, E.P. Payment systems in the healthcare industry: An experimental study of physician incentives. J. Econ. Behav. Organ. 2014, 106, 367–378. [Google Scholar] [CrossRef]
- Glazer, J.; McGuire, T.G. Optimal Risk Adjustment in Markets with Adverse Selection: An Application to Managed Care. Am. Econ. Rev. 2000, 90, 1055–1071. [Google Scholar] [CrossRef]
- Kuziemko, I.; Meckel, K.; Rossin-Slater, M. Do Insurers Risk-Select Against Each Other? Evidence from Medicaid and Implications for Health Reform; Technical Report; National Bureau of Economic Research: Cambridge, MA, USA, 2013. [Google Scholar] [CrossRef]
- Warder, C.J.; Edelstein, B.L. Evaluating levels of dentist participation in Medicaid. J. Am. Dent. Assoc. 2017, 148, 26–32.e2. [Google Scholar] [CrossRef]
- Serban, N.; Tomar, S.L. ADA Health Policy Institute’s methodology overestimates spatial access to dental care for publicly insured children. J. Public Health Dent. 2018, 78, 291–295. [Google Scholar] [CrossRef]
- Becker, B.W.; Kaldenberg, D.O.; McAlexander, J.H. Site Selection by Professional Services Providers: The Case of Dental Practices. J. Mark. Theory Pract. 1997, 5, 35–44. [Google Scholar] [CrossRef]
- Carpenter, B.E.; Neun, S.P. An analysis of the location decision of young primary care physicians. Atl. Econ. J. 1999, 27, 135–149. [Google Scholar] [CrossRef]
- Waldman, H.B. Some factors that endodontists may consider when selecting a practice location. J. Endod. 1999, 25, 264–267. [Google Scholar] [CrossRef]
- Diecidue, R.J. Evaluating a Dental Practice for Purchase or Associateship. Dent. Clin. N. Am. 2008, 52, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Nunes, E.; McKinnon, L.D. Lending to dental professionals (part two): How to value a practice. RMA J. 2013, 96, 32. [Google Scholar]
- Schafer, J.A.J. The Business of Private Medical Practice: Doctors, Specialization, and Urban Change in Philadelphia, 1900–1940; Rutgers University Press: New Brunswick, NJ, USA; London, UK, 2014. [Google Scholar]
- Badger, G.R.; Fryer, C.E.S.; Giannini, P.J.; Townsend, J.A.; Huja, S. Helping Dental Students Make Informed Decisions About Private Practice Employment Options in a Changing Landscape. J. Dent. Educ. 2015, 79, 1396–1401. [Google Scholar] [CrossRef] [PubMed]
- Alrayyes, S.M.; Garrett, A.M.; LeHew, C.W.; Compton, A.A. Where Do Pediatric Dental Residents Intend to Practice? Exploring the Influence of Loan Repayment Programs and Other Factors. J. Dent. Educ. 2019, 83, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Fry, R.; Taylor, P. The Rise of Residential Segregation by Income; Technical Report; Pew Research Center: Washington, DC, USA, 2012. [Google Scholar]
- Bischoff, K.; Reardon, S.F. Residential Segregation by Income, 1970–2009; Technical Report; Brown University, Russell Sage Foundation: New York, NY, USA, 2013. [Google Scholar]
- Asiamah, N.; Mensah, H.K.; Oteng-Abayie, E.F. Do Larger Samples Really Lead to More Precise Estimates? A Simulation Study. Am. J. Educ. Res. 2017, 5, 9–17. [Google Scholar] [CrossRef]

| 1 | Affinity Health Plan |
| 2 | AmidaCare |
| 3 | Empire Blue Cross Blue Shield/Amerigroup HealthPlus |
| 4 | Emblem Health Insurance Plan of Greater New York |
| 5 | Fidelis Care |
| 6 | HealthFirst Prepaid Health Services Plan |
| 7 | MetroPlus Health Plan/MetroPlus Health Plan Special Needs |
| 8 | United Healthcare Plan of New York |
| 9 | Visiting Nurse Services Choice Plan |
| 10 | Wellcare of New York |
| MCO-Listed Facilities: 259 | |||
| Respondents | 118 | Response Rate | 45.6% |
| MCO-Listed Dentists: 868 | |||
| Listed Facility Dentists | 509 | Percent of MCO Dentists | 58.6% |
| Verified Dentists | 70 | Verified Percent | 13.8% |
| Phantom Dentists | 351 | Phantom Percent | 69.0% |
| Eliminated Dentists | 88 | Eliminated Percent | 17.3% |
| Hidden Dentists: 9 | |||
| New Verified Total | 79 | Verified Percent Increase | 12.9% |
| Rank | Reason for Elimination | Count | Percent |
|---|---|---|---|
| 1 | Dentists serve children only | 49 | 9.6% |
| 2 | Dentists work less than 20 h per week | 39 | 7.7% |
| 88 Eliminated Dentists out of 509 Listed Dentists | |||
| Rank | Reason for Phantom Classification | Count | Percent |
|---|---|---|---|
| 1 | Dentists do not work at listed facilities | 113 | 22.2% |
| 2 | Dentists serve a limited population | 92 | 18.1% |
| 3 | Licensed dentists do not provide services | 82 | 16.1% |
| 4 | Dentists are not general providers | 47 | 9.2% |
| 5 | Dentists refuse the listed insurance | 17 | 3.3% |
| 351 Phantom Dentists out of 509 Listed Dentists | |||
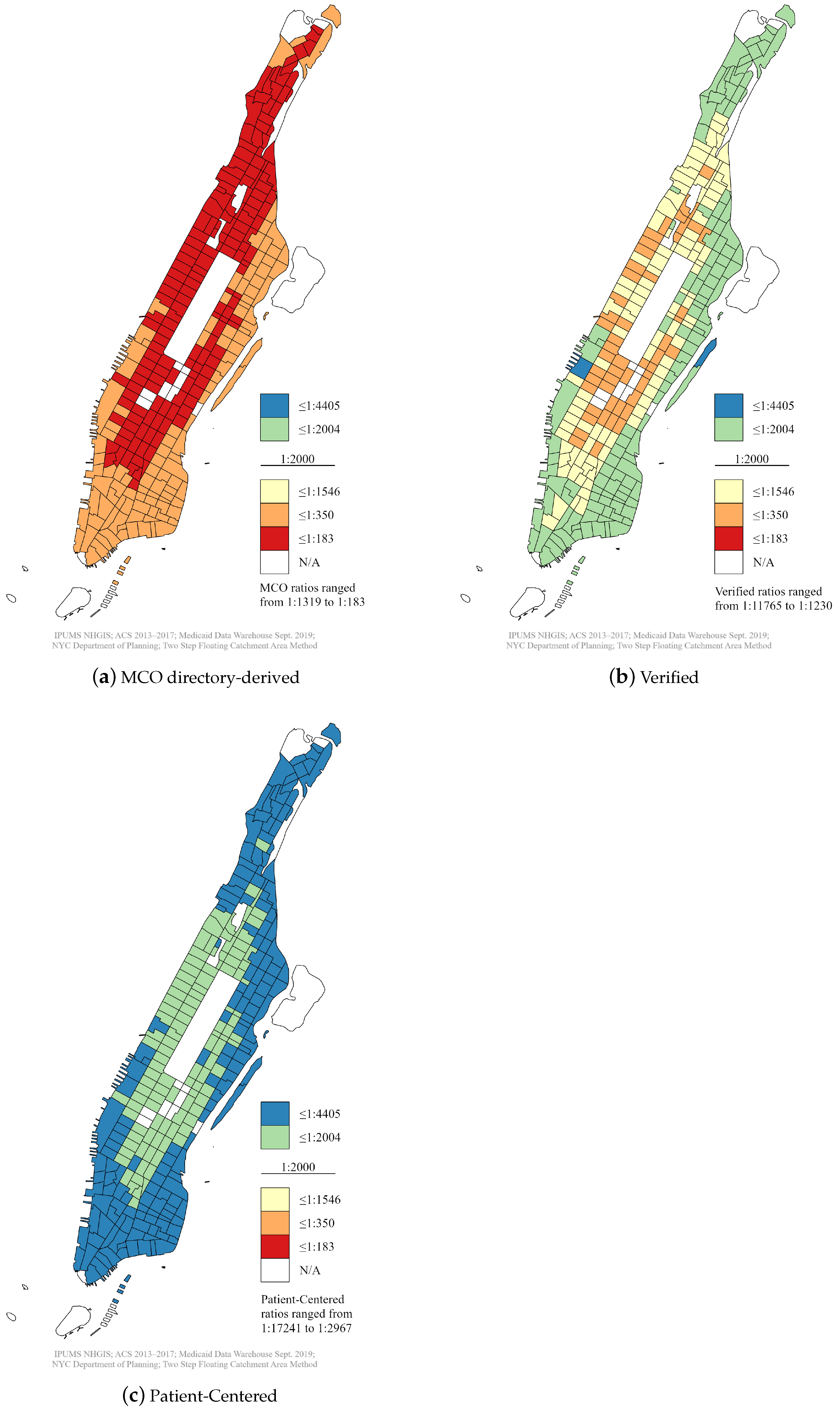
| MCO Directory Providers (Figure 1a) | |
| t = 46.0 | Data frame = 270 |
| p-value < 2.2 × 10−16 | Mean = 0.0032 (1:315) |
| Alternative hypothesis H0: | True mean > 5 × 10−4 (1:2000) |
| 95% confidence interval: | 0.0031, ∞ |
| The test rejects the hypothesis that 2000 Medicaid patients have access to less than one | |
| general dentist. | |
| Verified Providers (Figure 1b) | |
| t = 2.1 | Data frame = 270 |
| p-value = 0.01646 | Mean = 0.00052 (1:1927) |
| Alternative hypothesis H0: | True mean > 5 × 10−4 (1:2000) |
| 95% confidence interval: | 0.0005, ∞ |
| The test rejects the hypothesis that 2000 Medicaid patients have access to less than one | |
| general dentist. | |
| Patient-Centered Dentists (Figure 1c) | |
| t = −73.6 | Data frame = 270 |
| p-value = 1 | Mean = 0.00022 (1:4587) |
| Alternative hypothesis H0: | True mean > 5 × 10−4 (1:2000) |
| 95% confidence interval: | , 0.00021 |
| The test cannot reject the hypothesis that 2000 Medicaid patients have access to less than one | |
| general dentist. | |
| Patient-Centered Facility Criteria | Yes | No | Percent |
|---|---|---|---|
| Accept New Patients | 46 | 4 | 92% |
| Serve All Ages | 47 | 3 | 94% |
| Provide Full Services | 46 | 4 | 92% |
| Offer Extended Hours | 35 | 15 | 70% |
| Work Full-Time | 35 | 15 | 70% |
| Place No Caps on Patients | 49 | 1 | 98% |
| All Criteria | 20 | 30 | 40% |
| 50 verified facilities representing 79 verified dentists | |||
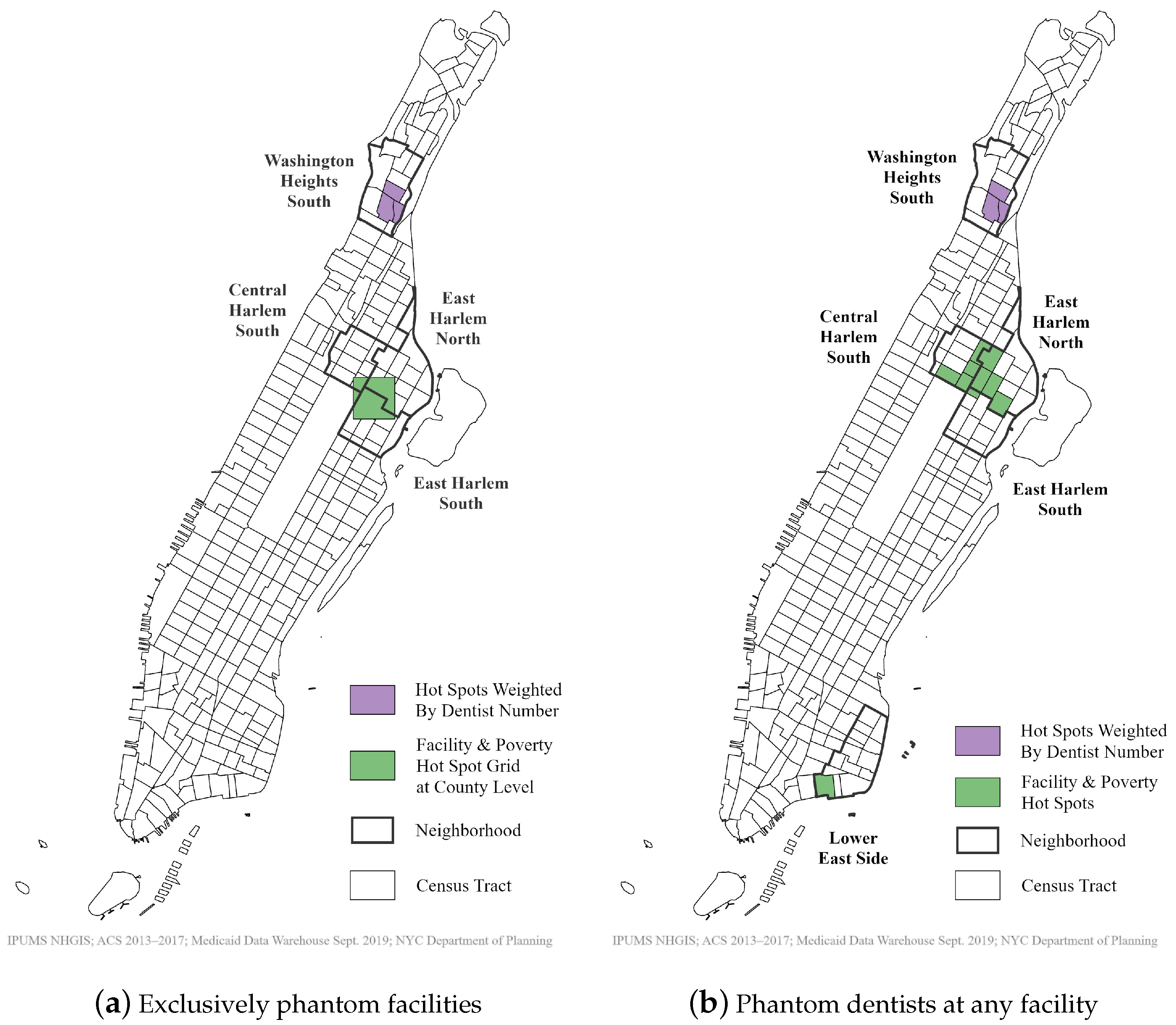
| Poverty Numbers and Count of Exclusively Phantom Facilities | |
| Moran’s Index: 0.44 | |
| z-score: 13.64 | Clustered Pattern |
| p-value: 0.00 | |
| Poverty Numbers and Count of Phantom Dentists at Exclusively Phantom Facilities | |
| Moran’s Index: 0.37 | |
| z-score: 12.27 | Clustered Pattern |
| p-value: 0.00 | |
| Poverty Numbers and Count of Any Facility with Phantom Dentists | |
| Moran’s Index: 0.53 | |
| z-score: 16.58 | Clustered Pattern |
| p-value: 0.00 | |
| Poverty Numbers and Count of Phantom Dentists at Any Facility | |
| Moran’s Index: 0.38 | |
| z-score: 12.34 | Clustered Pattern |
| p-value: 0.00 | |
| Neighborhood Hot Spot | Poverty Percent | Purely Phantom Facilities | All Facilities with Phantom Dentists | Dentists at Purely Phantom Facilities | Phantom Dentists at All Facilities |
|---|---|---|---|---|---|
| East Harlem North | 38.2% | 6 | 9 | - | - |
| Lower East Side | 30.1% | - | 5 | - | - |
| East Harlem South | 28.7% | 6 | 7 | - | - |
| Central Harlem South | 24.6% | 3 | 10 | - | - |
| Washington Heights South | 24.6% | - | - | 100 | 100 |
| Neighborhood Average | 19.5% | 3 | 5 | 15 | 19 |
| Phantom Network | Kendall’s Tau | p-Value | Spearman’s Rho | p-Value |
|---|---|---|---|---|
| Exclusively Phantom Facilities * | 0.1141 | 0.0161 | 0.1485 | 0.0144 |
| Number of Phantom Dentists | 0.1313 | 0.0037 | 0.1768 | 0.0035 |
| Any Facility with Phantom Dentists ** | 0.2329 | 3.913 × 10−7 | 0.3072 | 2.472 × 10−7 |
| Number of Phantom Dentists | 0.2300 | 1.441 × 10−7 | 0.3173 | 9.395 × 10−8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kelley, D.; Sun, S. How Phantom Networks, Provider Qualities, and Poverty Sway Medicaid Dental Care Access: A Geospatial Analysis of Manhattan. Int. J. Environ. Res. Public Health 2021, 18, 12383. https://doi.org/10.3390/ijerph182312383
Kelley D, Sun S. How Phantom Networks, Provider Qualities, and Poverty Sway Medicaid Dental Care Access: A Geospatial Analysis of Manhattan. International Journal of Environmental Research and Public Health. 2021; 18(23):12383. https://doi.org/10.3390/ijerph182312383
Chicago/Turabian StyleKelley, Destiny, and Shipeng Sun. 2021. "How Phantom Networks, Provider Qualities, and Poverty Sway Medicaid Dental Care Access: A Geospatial Analysis of Manhattan" International Journal of Environmental Research and Public Health 18, no. 23: 12383. https://doi.org/10.3390/ijerph182312383
APA StyleKelley, D., & Sun, S. (2021). How Phantom Networks, Provider Qualities, and Poverty Sway Medicaid Dental Care Access: A Geospatial Analysis of Manhattan. International Journal of Environmental Research and Public Health, 18(23), 12383. https://doi.org/10.3390/ijerph182312383







