Examining the Influence of Social Interactions and Community Resources on Caregivers’ Burden in Stroke Settings: A Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
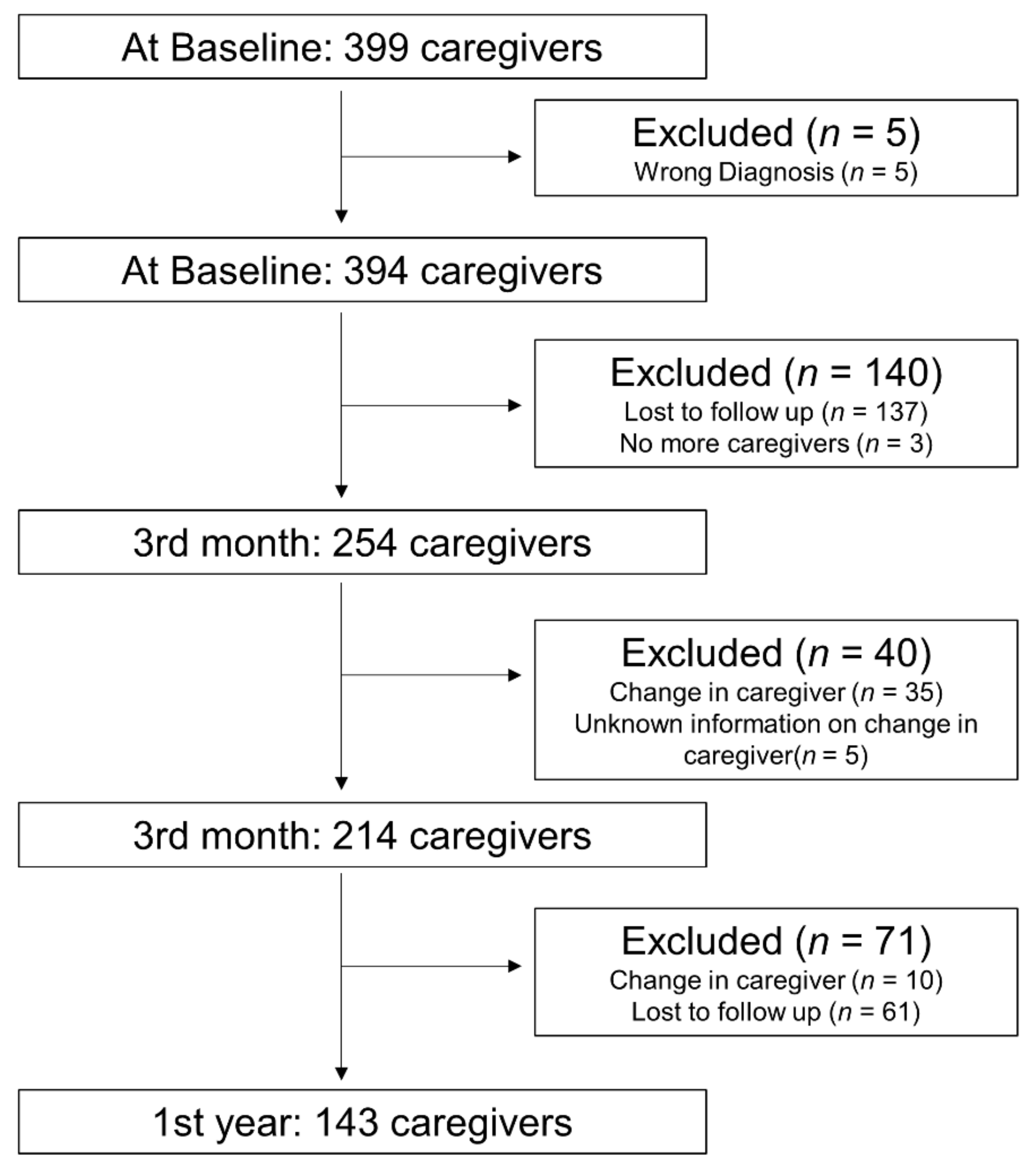
2.1. Participants and Data Collection
2.2. Dependent Variables
2.3. Independent Variables of Interest
2.4. Control Variables
2.5. Statistical Analysis
3. Results
3.1. Factors Associated with Caregivers’ Burden
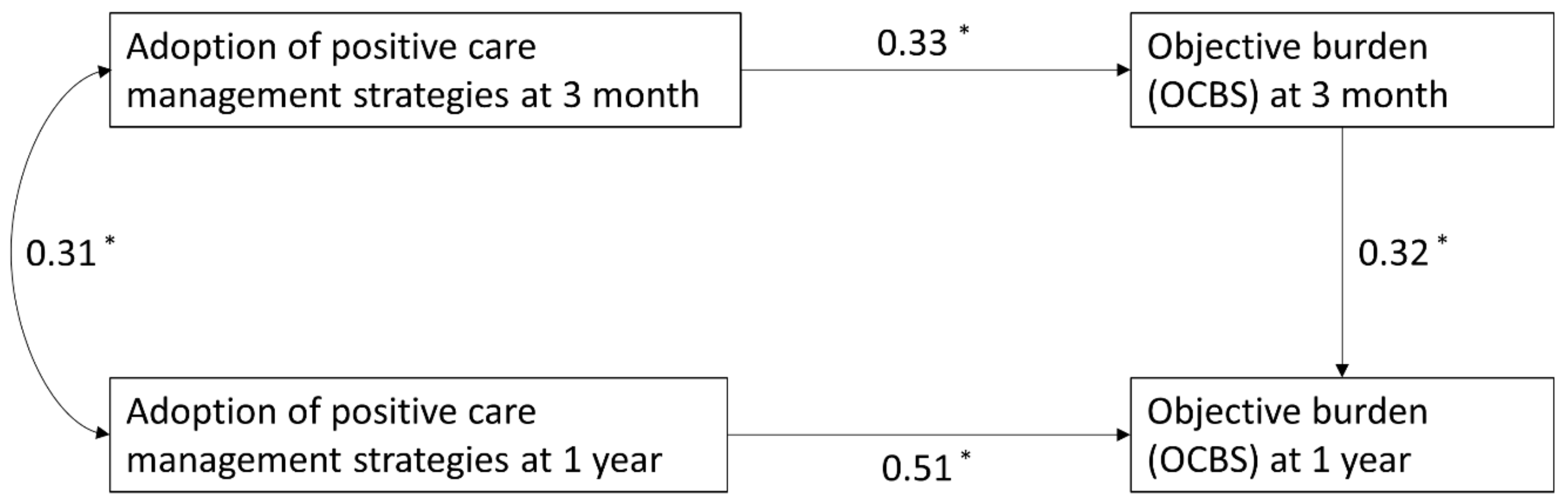
3.2. Pathway Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, Regional, and National Burden of Stroke and Its Risk Factors, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Turana, Y.; Tengkawan, J.; Chia, Y.C.; Nathaniel, M.; Wang, J.-G.; Sukonthasarn, A.; Chen, C.-H.; Van Minh, H.; Buranakitjaroen, P.; Shin, J.; et al. Hypertension and Stroke in Asia: A Comprehensive Review from HOPE Asia. J. Clin. Hypertens. 2021, 23, 513–521. [Google Scholar] [CrossRef]
- National Registry of Diseases Office. Singapore Stroke Regist. In Singapore Stroke Registry Annual Report 2019; National Registry of Diseases Office: Singapore, 2021; pp. 1–50. [Google Scholar]
- Rigby, H.; Gubitz, G.; Phillips, S. A Systematic Review of Caregiver Burden Following Stroke. Int. J. Stroke 2009, 4, 285–292. [Google Scholar] [CrossRef]
- Jaracz, K.; Grabowska-Fudala, B.; Górna, K.; Jaracz, J.; Moczko, J.; Kozubski, W. Burden in Caregivers of Long-Term Stroke Survivors: Prevalence and Determinants at 6 Months and 5 Years after Stroke. Patient Educ. Couns. 2015, 98, 1011–1016. [Google Scholar] [CrossRef] [PubMed]
- Vincent, C.; Desrosiers, J.; Landreville, P.; Demers, L. Burden of Caregivers of People with Stroke: Evolution and Predictors. Cerebrovasc. Dis. 2009, 27, 456–464. [Google Scholar] [CrossRef]
- Ilse, I.B.; Feys, H.; de Wit, L.; Putman, K.; de Weerdt, W. Stroke Caregivers’ Strain: Prevalence and Determinants in the First Six Months after Stroke. Disabil. Rehabil. 2008, 30, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Draper, B.M.; Poulos, C.J.; Cole, A.M.D.; Poulos, R.G.; Ehrlich, F. A Comparison of Caregivers for Elderly Stroke and Dementia Victims. J. Am. Geriatr. Soc. 1992, 40, 896–901. [Google Scholar] [CrossRef]
- Shannon Ang, R.M. Expressive Social Support Buffers the Impact of Care-Related Work Interruptions on Caregivers’ Depressive Symptoms Shannon. Aging Ment. Health 2018, 22, 755–763. [Google Scholar] [CrossRef]
- Zhu, W.; Jiang, Y. A Meta-Analytic Study of Predictors for Informal Caregiver Burden in Patients With Stroke. J. Stroke Cerebrovasc. Dis. 2018, 27, 3636–3646. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, R.J.; Gonyea, J.G.; Hooyman, N.R. Caregiving and the Experience of Subjective and Objective Burden. Fam. Relat. Interdiscip. J. Appl. Fam. Stud. 1985, 34, 19–26. [Google Scholar] [CrossRef]
- Oliva-Moreno, J.; Peña-Longobardo, L.M.; Mar, J.; Masjuan, J.; Soulard, S.; Gonzalez-Rojas, N.; Becerra, V.; Casado, M.Á.; Torres, C.; Yebenes, M.; et al. Determinants of Informal Care, Burden, and Risk of Burnout in Caregivers of Stroke Survivors the CONOCES Study. Stroke 2018, 49, 140–146. [Google Scholar] [CrossRef]
- Mccullagh, E.; Brigstocke, G.; Donaldson, N.; Kalra, L. Determinants of Caregiving Burden and Quality of Life in Caregivers of Stroke Patients. Stroke 2005, 36, 2181–2186. [Google Scholar] [CrossRef] [PubMed]
- Tooth, L.; Mckenna, K.; Barnett, A.; Prescott, C.; Murphy, S.; Mckenna, K.; Barnett, A.; Prescott, C.; Caregiver, S.M. Caregiver Burden, Time Spent Caring and Health Status in the First 12 Months Following Stroke. Brain Inj. 2010, 19, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Jiang, Y. Determinants of Caregiver Burden of Patients with Haemorrhagic Stroke in China. Int. J. Nurs. Pract. 2019, 25, 1–8. [Google Scholar] [CrossRef]
- Domingues, N.S.; Verreault, P.; Hudon, C. Reducing Burden for Caregivers of Older Adults with Mild Cognitive Impairment: A Systematic Review. Am. J. Alzheimers Dis. Other Demen. 2018, 33, 401–414. [Google Scholar] [CrossRef]
- Zwingmann, I.; Hoffmann, W.; Michalowsky, B.; Dreier-Wolfgramm, A.; Hertel, J.; Wucherer, D.; Eichler, T.; Kilimann, I.; Thiel, F.; Teipel, S.; et al. Supporting Family Dementia Caregivers: Testing the Efficacy of Dementia Care Management on Multifaceted Caregivers’ Burden. Aging Ment. Health 2018, 22, 889–896. [Google Scholar] [CrossRef] [PubMed]
- Achilike, S.; Beauchamp, J.E.S.; Cron, S.G.; Okpala, M.; Payen, S.S.; Baldridge, L.; Okpala, N.; Montiel, T.C.; Varughese, T.; Love, M.; et al. Caregiver Burden and Associated Factors among Informal Caregivers of Stroke Survivors. J. Neurosci. Nurs. 2020, 52, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Kandeger, A.; Guler, H.A.; Egilmez, U.; Guler, O. To Change: Predictors of Caregiver Burden after Stroke in Nigeria: Effect on Psychosocial Well-Being. Indian J. Psychiatry 2018, 59, 2017–2018. [Google Scholar] [CrossRef]
- Kumar, R.; Kaur, S.; Burden, K.R. Its Predictors and Quality of Life in Caregivers of Stroke Survivors at Rural Community, Punjab, India. J. Neurol. Neurorehabilit. Res. 2016, 1, 1–7. [Google Scholar] [CrossRef]
- Barrett, P.; Hale, B.; Butler, M. Family Care and Social Capital: Transitions in Informal Care; Springer: Dordrecht, The Netherlands, 2014. [Google Scholar] [CrossRef]
- Nurjono, M.; Shrestha, P.; Ang, I.Y.H.; Shiraz, F.; Eh, K.X.; Toh, S.A.E.S.; Vrijhoef, H.J.M. Shifting Care from Hospital to Community, a Strategy to Integrate Care in Singapore: Process Evaluation of Implementation Fidelity. BMC Health Serv. Res. 2020, 20, 452. [Google Scholar] [CrossRef]
- Thiyagarajan, J.A.; De Carvalho, I.A.; Peña-Rosas, J.P.; Chadha, S.; Mariotti, S.P.; Dua, T.; Albanese, E.; Bruyère, O.; Cesari, M.; Dangour, A.; et al. Redesigning Care for Older People to Preserve Physical and Mental Capacity: WHO Guidelines on Community-Level Interventions in Integrated Care. PLoS Med. 2019, 16, e1002948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prime Minister’s Office. Population in Brief 2020; Prime Minister’s Office: Singapore, 2020. [Google Scholar]
- Lau, S. Collectivism’s Individualism: Value Preference, Personal Control, and the Desire for Freedom among Chinese in Mainland China, Hong Kong, and Singapore. Pers. Individ. Dif. 1992, 13, 361–366. [Google Scholar] [CrossRef]
- Tyagi, S.; Koh, G.C.H.; Luo, N.; Tan, K.B.; Hoenig, H.; Matchar, D.B.; Yoong, J.; Chan, A.; Lee, K.E.; Venketasubramanian, N.; et al. Dyadic Approach to Supervised Community Rehabilitation Participation in an Asian Setting Post-Stroke: Exploring the Role of Caregiver and Patient Characteristics in a Prospective Cohort Study. BMJ Open 2020, 10, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bédard, M.; Molloy, D.W.; Squire, L.; Dubois, S.; Lever, J.A.; O’donnell, M. The Zarit Burden Interview: A New Short Version and Screening Version. Gerontologist 2001, 41, 652–657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seng, B.K.; Luo, N.; Ng, W.Y.; Lim, J.; Chionh, H.L.; Goh, J.; Yap, P. Validity and Reliability of the Zarit Burden Interview in Assessing Caregiving Burden. Ann. Acad Med. Singap. 2010, 39, 758–763. [Google Scholar] [PubMed]
- Bakas, T.; Austin, J.K.; Jessup, S.L.; Williams, L.S.; Oberst, M.T. Time and Difficulty of Tasks Provided by Family Caregivers of Stroke Survivors. J. Neurosci. Nurs. 2004, 36, 95–106. [Google Scholar] [CrossRef]
- Lawrence, R.H.; Tennstedt, S.L.; Assmann, S.F. Quality of the Caregiver-Care Recipient Relationship: Does It Offset Negative Consequences of Caregiving for Family Caregivers? Psychol. Aging 1998, 13, 150–158. [Google Scholar] [CrossRef]
- Pearlin, L.I.; Mullan, J.T.; Semple, S.J.; Skaff, M.M. Caregiving and the Stress Process: An Overview of Concepts and Their Measures. Gerontologist 1990, 30, 583–594. [Google Scholar] [CrossRef] [PubMed]
- Hinrichsen, G.A.; Niederehe, G. Dementia Management Strategies and Adjustment of Family Members of Older Patients. Gerontologist 1994, 34, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Yap, P.; Ng, W.Y.; Luo, N. Exploring the Use of the Dementia Management Strategies Scale in Caregivers of Persons with Dementia in Singapore. Aging Ment. Health 2013, 17, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the Sensitivity of the Barthel Index for Stroke Rehabilitation. J. Clin. Epidemiol. 1989, 42, 703–709. [Google Scholar] [CrossRef]
- Chan, A.; Raman, P.; Ma, S.; Malhotra, R. Loneliness and All-Cause Mortality in Community-Dwelling Elderly Singaporeans. Demogr. Res. 2015, 32, 1361–1382. [Google Scholar] [CrossRef] [Green Version]
- Acock, A.C. Discovering Structural Equation Modeling Using Stata; Stata Press: College Station, TX, USA, 2013. [Google Scholar]
- Yeung, E.H.L.; Szeto, A.; Richardson, D.; Lai, S.-h.; Lim, E.; Cameron, J.I. The Experiences and Needs of Chinese-Canadian Stroke Survivors and Family Caregivers as They Re-Integrate into the Community. Health Soc. Care Community 2015, 23, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Qiu, X.; Sit, J.W.H.; Koo, F.K. The Influence of Chinese Culture on Family Caregivers of Stroke Survivors: A Qualitative Study. J. Clin. Nurs. 2018, 27, e309–e319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boots, L.M.M.; De Vugt, M.E.; Kempen, G.I.J.M.; Verhey, F.R.J. Effectiveness of a Blended Care Self-Management Program for Caregivers of People with Early-Stage Dementia (Partner in Balance): Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Chodosh, J.; Colaiaco, B.A.; Connor, K.I.; Cope, D.W.; Liu, H.; Ganz, D.A.; Richman, M.J.; Cherry, D.L.; Blank, J.M.; Carbone, R.D.P.; et al. Dementia Care Management in an Underserved Community: The Comparative Effectiveness of Two Different Approaches. J. Aging Health 2015, 27, 864–893. [Google Scholar] [CrossRef]
- Gitlin, L.N.; Winter, L.; Dennis, M.P.; Hodgson, N.; Hauck, W.W. Targeting and Managing Behavioral Symptoms in Individuals with Dementia: A Randomized Trial of a Nonpharmacological Intervention. J. Am. Geriatr. Soc. 2010, 58, 1465–1474. [Google Scholar] [CrossRef]
- Kruithof, W.J.; Post, M.W.M.; van Mierlo, M.L.; van den Bos, G.A.M.; de Man-van Ginkel, J.M.; Visser-Meily, J.M.A. Caregiver Burden and Emotional Problems in Partners of Stroke Patients at Two Months and One Year Post-Stroke: Determinants and Prediction. Patient Educ. Couns. 2016, 99, 1632–1640. [Google Scholar] [CrossRef]
- McPherson, C.J.; Wilson, K.G.; Chyurlia, L.; Leclerc, C. The Caregiving Relationship and Quality of Life among Partners of Stroke Survivors: A Cross-Sectional Study. Health Qual. Life Outcomes 2011, 9, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Reid, C.E.; Moss, S.; Hyman, G. Caregiver Reciprocity: The Effect of Reciprocity, Carer Self-Esteem and Motivation on the Experience of Caregiver Burden. Aust. J. Psychol. 2005, 57, 186–196. [Google Scholar] [CrossRef]
- Ostwald, S.K.; Bernal, M.P.; Cron, S.G.; Godwin, K.M. Stress Experienced by Stroke Survivors and Spousal Caregivers during the First Year after Discharge from Inpatient Rehabilitation. Top. Stroke Rehabil. 2009, 16, 93–104. [Google Scholar] [CrossRef] [Green Version]
- Netto, R.N.; Goh Yen, J.; Philip, Y.L.K. Growing and Gaining through Caring for a Loved One with Dementia. Dementia 2009, 8, 245–261. [Google Scholar] [CrossRef]
- Liew, T.M.; Luo, N.; Ng, W.Y.; Chionh, H.L.; Goh, J.; Yap, P. Predicting Gains in Dementia Caregiving. Dement. Geriatr. Cogn. Disord. 2010, 29, 115–122. [Google Scholar] [CrossRef]
- Lee, J.; Chuen, S.T.; Kee, S.C. A Practical Guide for Multivariate Analysis of Dichotomous Outcomes. Ann. Acad Med. Singap. 2009, 38, 714–719. [Google Scholar]
| Characteristics of Patients | n = 214 | |
|---|---|---|
| Mean age, year (SD) | 62.8 (11.5) | |
| Sex | Male | 137 (64.0%) |
| Female | 77 (36.0%) | |
| Ethnicity | Chinese | 119 (55.6%) |
| Malay | 70 (32.7%) | |
| Indian | 21 (9.8%) | |
| Others | 4 (1.9%) | |
| Median Barthel Index during admission | 75 (40–94.5) | |
| Characteristics of Patients | n= 214 | |
| Mean Age, years (SD) | 49.0 (13.0) | |
| Sex | Male | 59 (27.6%) |
| Female | 155 (72.4%) | |
| Ethnicity | Chinese | 114 (53.8%) |
| Malay | 74 (34.9%) | |
| Indian | 19 (9.0%) | |
| Others | 5 (2.4%) | |
| Educational qualification | No qualification | 8 (3.7%) |
| Primary | 50 (23.4%) | |
| Secondary | 89 (41.8%) | |
| Post-Secondary/Polytechnic | 52 (24.4%) | |
| University | 14 (6.6%) | |
| Employment status | Employed Full time | 91 (42.9%) |
| Employed part time | 22 (10.4%) | |
| Unemployed | 99 (46.7%) | |
| Relationship with patient | Spousal | 119 (55.9%) |
| Children | 74 (34.7%) | |
| Others | 20 (9.4%) | |
| Median ZBI score (IQR) | 11 (6–19) | |
| Median CES-D (IQR) | 7 (3–9) | |
| 3rd Month # (n = 214) | 1st Year ^ (n = 143) | ||
|---|---|---|---|
| Variables Related to Caregivers | No. (%) | No. (%) | |
| Median ZBI Score (IQR) | 7 (5–13) | 5 (0–11) | |
| ZBI Classification | Low burden (ZBI < 17) | 185 (87.7%) | 119 (85.0%) |
| High Burden (ZBI ≥ 17) | 26 (12.3%) | 21 (15.0%) | |
| Median OCBS (IQR) | 31 (23–42) | 29 (19–37) | |
| OCBS Classification | Low burden (OCBS < 30) | 83 (46.4%) | 70 (51.1%) |
| High Burden (OCBS ≥ 30) | 96 (53.6%) | 67 (48.9%) | |
| Median Quality of care relationship (IQR) | 12 (10–12) | 12 (9–12) | |
| Mean Positive Care management strategies (SD) | 36.1 (10.8) | 31.3 (12.2) | |
| Median Negative Care management strategies (IQR) | 8 (8–13) | 8 (8–13) | |
| Median Family Conflict: Attitudes and Actions Toward the Caregiver (IQR) | 12 (8–16) | 10 (8–12) | |
| Median Family Conflict: Attitudes and Actions Toward the Patient (IQR) | 12 (8–16) | 8 (8–12) | |
| Median CES-D of caregivers (IQR) | 4 (2–7) | 3 (1–5) | |
| Assistance to caregiver | No | 71 (34.8%) | 66 (46.2%) |
| Yes | 133 (65.2%) | 77 (53.9%) | |
| Use of formal services | No | 150 (72.1%) | 89 (65.0%) |
| Yes | 58 (27.9%) | 48 (35.0%) | |
| Variables Related to Patients | |||
| Median Barthel Index (IQR) | 99.5 (75.5–100) | 99 (80.5–100) |
| Unadjusted Model | Adjusted Model † | ||||
|---|---|---|---|---|---|
| Variable Related to Caregivers | RR (95% CI) | p-Value | RR (95% CI) | p-Value | |
| Assistance to caregiver | No (Reference) | ||||
| Yes | 2.65 (1.28–5.51) | 0.009 * | |||
| Quality of care relationship | 0.79 (0.69–0.90) | <0.001* | 0.81 (0.70–0.94) | 0.004 * | |
| Positive Care management strategies | 1.03 (1.00–1.05) | 0.028 * | 1.05 (1.02–1.07) | 0.002 * | |
| Negative Care management strategies | 1.01 (1.00–1.02) | 0.015 * | |||
| Attitudes and Actions Toward the Caregiver | 0.95 (0.90–1.00) | 0.068 | |||
| Attitudes and Actions Toward the Patient | 0.93 (0.88–0.99) | 0.019 * | |||
| Use of formal services | No (Reference) | ||||
| Yes | 1.16 (0.67–2.01) | 0.600 | |||
| CES-D of caregivers | 1.21 (1.15–1.28) | <0.001 * | 1.23 (1.17–1.29) | <0.001 * | |
| Variables related to patients | RR (95% CI) | p-value | RR (95% CI) | p-value | |
| Barthel Index | 0.987 (0.980–0.993) | <0.001 * | 0.994 (0.987–1.001) | 0.092 | |
| Timepoint | 3rd month (Reference) | ||||
| 1st year | 1.22 (0.75–1.98) | 0.421 | 2.30 (1.40–3.78) | 0.001 * | |
| Unadjusted Model | Adjusted Model †,‡ | ||||
|---|---|---|---|---|---|
| Variable Related to Caregivers | RR (95% CI) | p-Value | RR (95% CI) | p-Value | |
| Assistance to caregiver | No (Reference) | ||||
| Yes | 2.94 (2.10–4.10) | <0.001 * | 2.45 (1.72–3.49) | <0.001 * | |
| Quality of care relationship | 1.00 (0.93–1.07) | 0.992 | |||
| Positive Care management strategies | 1.03 (1.02–1.04) | <0.001 * | 1.03 (1.02–1.04) | <0.001 * | |
| Negative Care management strategies | 1.006 (1.000–1.012) | 0.027 * | |||
| Attitudes and Actions Toward the Caregiver | 0.973 (0.949–0.998) | 0.038 * | |||
| Attitudes and Actions Toward the Patient | 0.974 (0.950–0.998) | 0.036 * | |||
| Use of formal services | No (Reference) | ||||
| Yes | 1.27 (1.01–1.59) | 0.041 * | |||
| CES-D of caregivers | 1.05 (1.02–1.08) | <0.001 * | 1.02 (0.99–1.05) | 0.302 | |
| Variables related to patients | RR (95% CI) | p-value | RR (95% CI) | p-value | |
| Barthel Index | 0.990 (0.987–0.992) | <0.001 * | 0.994 (0.991–0.997) | <0.001 * | |
| Timepoint | 3rd month (Reference) | ||||
| 1st year | 0.91 (0.75–1.11) | 0.364 | 1.11 (0.89–1.38) | 0.368 | |
| Direct Effect | Standardized Coefficient (95% CI) | p-Value |
|---|---|---|
| OCBS (3rd month) | 0.32 (0.16 to 0.47) | <0.001 * |
| Adoption of positive care management strategies (one-year) | 0.51 (0.37 to 0.65) | <0.001 * |
| Indirect Effect | Standardized Coefficient (95% CI) | p-Value |
| Adoption of positive care management strategies (3rd month) | 0.11 (0.01 to 0.20) | 0.025 * |
| Fit Statistics | Value | |
| Root mean squared error of approximation (RMSEA) | 0.077 | |
| Comparative fit index (CFI) | 0.962 | |
| Standardized root mean squared residual (SRMR) | 0.035 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koh, Y.S.; Koh, G.C.-H.; Matchar, D.B.; Hong, S.-I.; Tai, B.C. Examining the Influence of Social Interactions and Community Resources on Caregivers’ Burden in Stroke Settings: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 12310. https://doi.org/10.3390/ijerph182312310
Koh YS, Koh GC-H, Matchar DB, Hong S-I, Tai BC. Examining the Influence of Social Interactions and Community Resources on Caregivers’ Burden in Stroke Settings: A Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(23):12310. https://doi.org/10.3390/ijerph182312310
Chicago/Turabian StyleKoh, Yen Sin, Gerald Choon-Huat Koh, David Bruce Matchar, Song-Iee Hong, and Bee Choo Tai. 2021. "Examining the Influence of Social Interactions and Community Resources on Caregivers’ Burden in Stroke Settings: A Prospective Cohort Study" International Journal of Environmental Research and Public Health 18, no. 23: 12310. https://doi.org/10.3390/ijerph182312310
APA StyleKoh, Y. S., Koh, G. C.-H., Matchar, D. B., Hong, S.-I., & Tai, B. C. (2021). Examining the Influence of Social Interactions and Community Resources on Caregivers’ Burden in Stroke Settings: A Prospective Cohort Study. International Journal of Environmental Research and Public Health, 18(23), 12310. https://doi.org/10.3390/ijerph182312310





