A Rapid Realist Review of Effective Mental Health Interventions for Individuals with Chronic Physical Health Conditions during the COVID-19 Pandemic Using a Systems-Level Mental Health Promotion Framework
Abstract
:1. Introduction
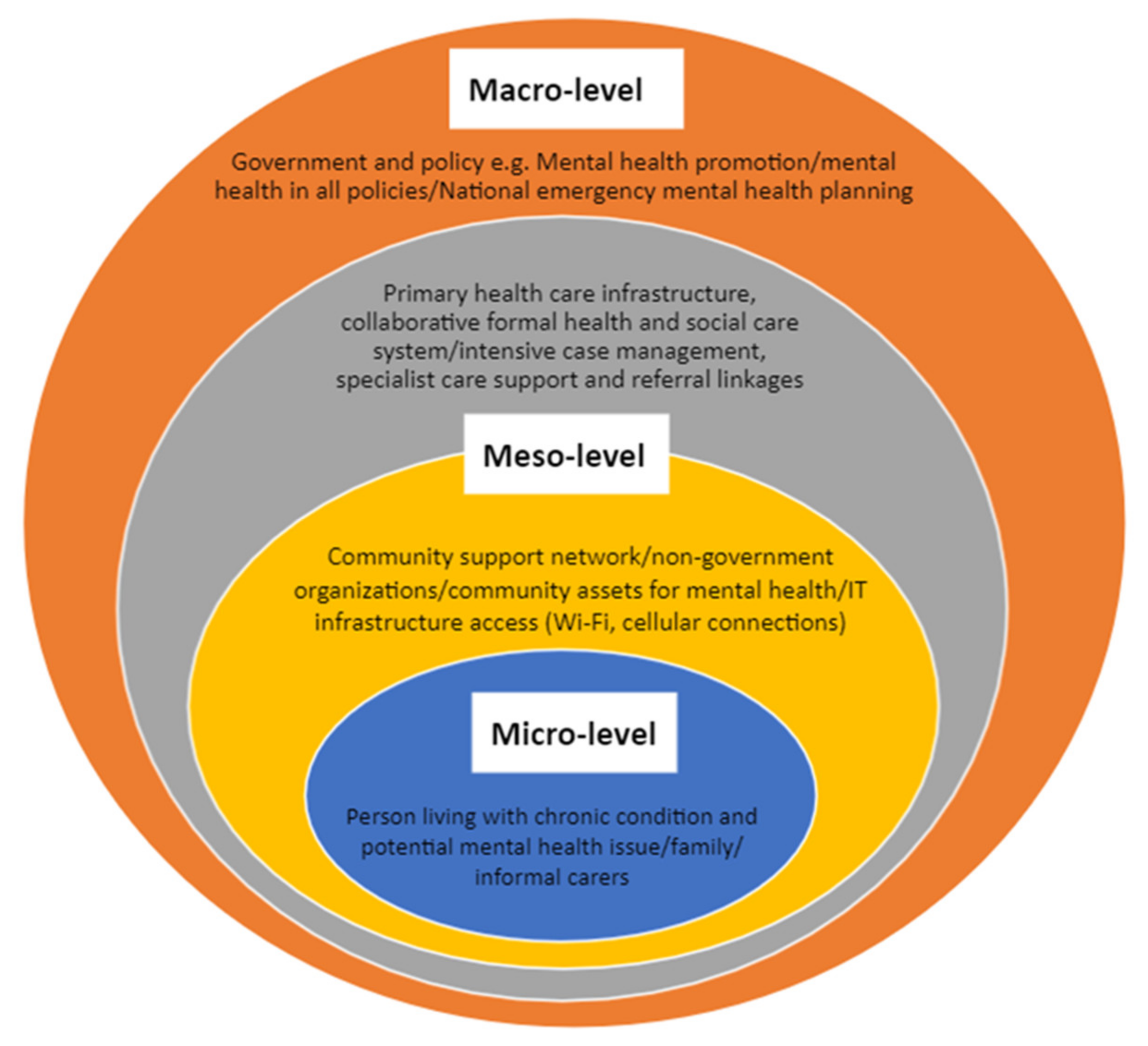
1.1. Background
1.2. Study Aim
2. Materials and Methods
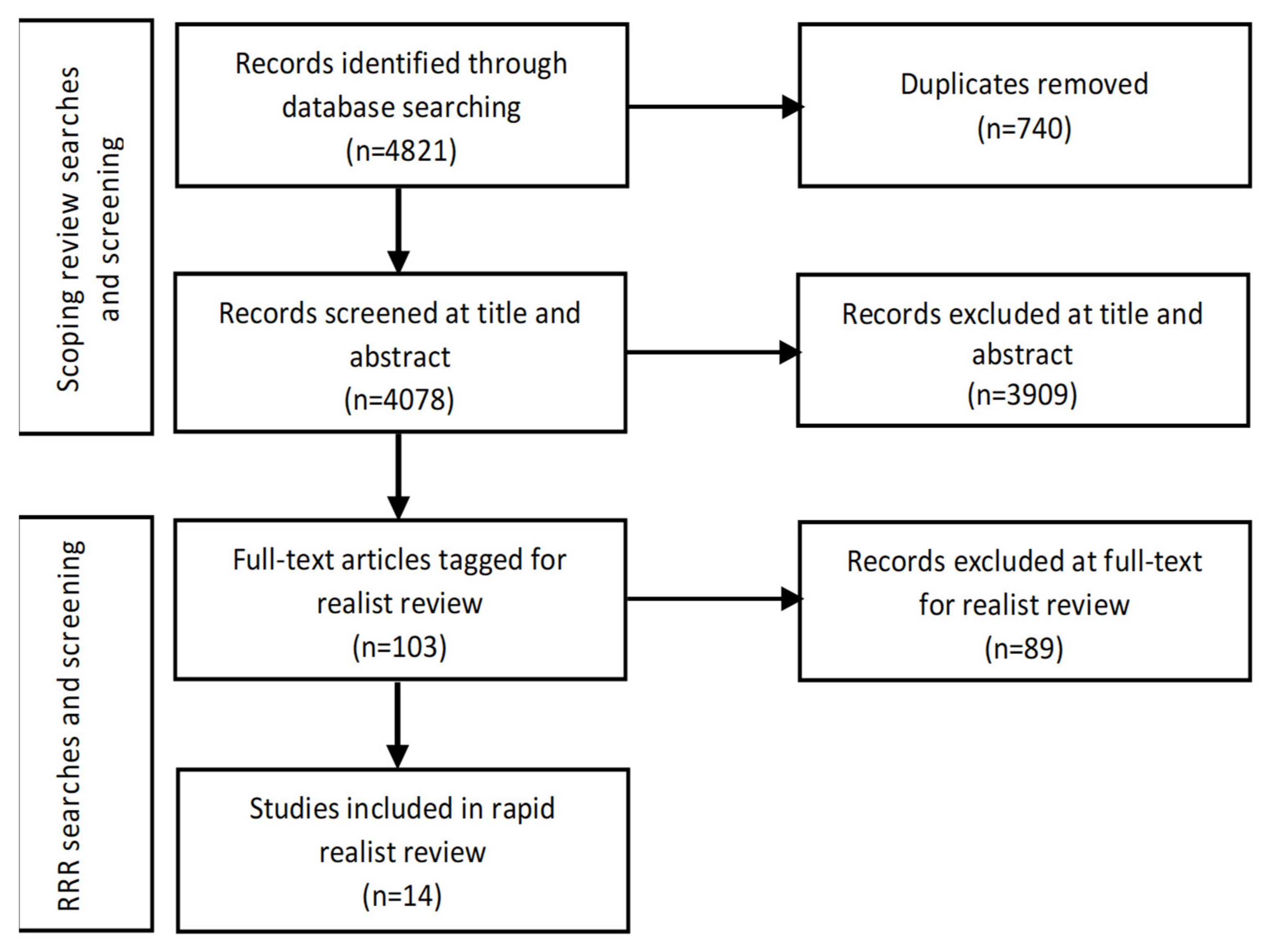
2.1. Search, Selection, and Appraisal Processes
2.2. Data Extraction and Analysis
2.3. Patient and Public Involvement/Stakeholder Engagement
3. Results
3.1. Study Characterisics
3.2. Programme Theory Development
3.2.1. Trust
“The COVID-19 pandemic has made health services and policy makers rethink the way we deliver services and organise resources in the best possible ways.”[17] (p. 23)
“Primary care doctors providing patient-centred, longitudinal care are in a unique position to provide psychological support and treatment during the current pandemic, since continuity of care is associated with lower mortality rates and better patient outcomes.”[20] (p. 2)
3.2.2. Social Connectedness
3.2.3. Accountability
3.2.4. Resilience
3.3. Purposive Literature Search of Pre-COVID Realist Reviews
3.3.1. Trust Pre-COVID-19 and during COVID-19
3.3.2. Social Connectedness Pre-COVID-19 and during COVID-19
3.3.3. Accountability Pre-COVID-19 and during COVID-19
“Programs and program strategies that support autonomy and self-directions in treatment and use of services will likely lead to longer-term positive health changes compared to programs that are fixed…”(p. 983)
3.3.4. Resilience Pre-COVID-19 and during COVID-19
3.3.5. Power-Sharing
“Civic engagement has the potential to transform mental health systems…It can also lead to improved information about, and access to, mental health care as well as enhancing relationships between patients and clinicians.”(p. 2)
4. Discussion and Implications
4.1. Implications
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moreno, C.; Wykes, T.; Galderisi, S.; Nordentoft, M.; Crossley, N.; Jones, N.; Cannon, M.; Correll, C.U.; Byrne, L.; Carr, S.; et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 813–824. [Google Scholar] [CrossRef]
- Otu, A.; Charles, C.H.; Yaya, S. Mental health and psychosocial well-being during the COVID-19 pandemic: The invisible elephant in the room. Int. J. Ment. Health Syst. 2020, 14, 38. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Morstead, T.; Sin, N.; Klaiber, P.; Umberson, D.; Kamble, S.; DeLongis, A. Psychological distress in North America during COVID-19: The role of pandemic-related stressors. Soc. Sci. Med. 2021, 270, 113687. [Google Scholar] [CrossRef] [PubMed]
- Berger, Z.D.; Evans, N.G.; Phelan, A.L.; Silverman, R.D. Covid-19: Control measures must be equitable and inclusive. BMJ 2020, 368, m1141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Considerations for Implementing and Adjusting Public Health and Social Measures in the Context of COVID-19. 2021. Available online: https://www.who.int/publications/i/item/considerations-in-adjusting-public-health-and-social-measures-in-the-context-of-covid-19-interim-guidance (accessed on 3 September 2021).
- Umucu, E.; Tansey, T.N.; Brooks, J.; Lee, B. The protective role of character strengths in COVID-19 stress and well-being in individuals with chronic conditions and disabilities: An exploratory study. Rehabil. Couns. Bull. 2021, 64, 67–74. [Google Scholar] [CrossRef]
- Hashim, M.J.; Alsuwaidi, A.R.; Khan, G. Population risk factors for COVID-19 mortality in 93 countries. J. Epidemiol. Glob. Health 2020, 10, 204. [Google Scholar] [CrossRef]
- Hossain, M.M.; Tasnim, S.; Sultana, A.; Faizah, F.; Mazumder, H.; Zou, L.; McKyer, E.L.J.; Ahmed, H.U.; Ma, P. Epidemiology of mental health problems in COVID-19: A review. F1000Research 2020, 9, 636. [Google Scholar] [CrossRef]
- Davison, K.M.; Thakkar, V.; Lin, S.L.; Stabler, L.; MacPhee, M.; Carroll, S.; Collins, B.; Rezler, Z.; Colautti, J.; Xu, C.C.; et al. Interventions to Support Mental Health among Those with Health Conditions That Present Risk for Severe Infection from Coronavirus Disease 2019 (COVID-19): A Scoping Review of English and Chinese-Language Literature. Int. J. Environ. Res. Public Health 2021, 18, 7265. [Google Scholar] [CrossRef]
- Chevance, A.; Gourion, D.; Hoertel, N.; Llorca, P.M.; Thomas, P.; Bocher, R.; Moro, M.R.; Laprevote, V.; Benyamina, A.; Fossati, P.; et al. Ensuring mental health care during the SARS-CoV-2 epidemic in France: A narrative review. L’encephale 2020, 46, 193–201. [Google Scholar] [CrossRef]
- Kienzler, H. Mental health in all policies in contexts of war and conflict. Lancet Public Health 2019, 4, e547–e548. [Google Scholar] [CrossRef] [Green Version]
- Tonelli, M.; Tang, K.C.; Forest, P.G. Canada needs a “Health in All Policies” action plan now. CMAJ 2020, 192, E61–E67. [Google Scholar] [CrossRef] [Green Version]
- Pawson, R. Evidence-based policy: The promise of realist synthesis. Evaluation 2002, 8, 340–358. [Google Scholar] [CrossRef] [Green Version]
- Pawson, R.; Tilley, N. Realistic Evaluation; Sage Publications: London, UK, 1997. [Google Scholar]
- Wong, G.; Greenhalgh, T.; Westhorp, G.; Buckingham, J.; Pawson, R. RAMESES publication standards: Realist syntheses. BMC Med. 2013, 11, 21. [Google Scholar] [CrossRef] [Green Version]
- Pearson, M.; Chilton, R.; Wyatt, K.; Abraham, C.; Ford, T.; Woods, H.B.; Anderson, R. Implementing health promotion programmes in schools: A realist systematic review of research and experience in the United Kingdom. Implement. Sci. 2015, 10, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Chakraborty, N. The COVID-19 pandemic and its impact on mental health. Prog. Neurol. Psychiatry 2020, 24, 21–24. [Google Scholar] [CrossRef]
- Khan, S.; Siddique, R.; Li, H.; Ali, A.; Shereen, M.A.; Bashir, N.; Xue, M. Impact of coronavirus outbreak on psychological health. J. Glob. Health 2020, 10, 010331. [Google Scholar] [CrossRef]
- Wang, A.; Zhao, W.; Xu, Z.; Gu, J. Timely blood glucose management for the outbreak of 2019 novel coronavirus disease (COVID-19) is urgently needed. Diabetes Res. Clin. Pract. 2020, 4, 162. [Google Scholar] [CrossRef]
- Razai, M.S.; Oakeshott, P.; Kankam, H.; Galea, S.; Stokes-Lampard, H. Mitigating the psychological effects of social isolation during the covid-19 pandemic. BMJ 2020, 369, m1904. [Google Scholar] [CrossRef]
- Pulvirenti, F.; Cinetto, F.; Milito, C.; Bonanni, L.; Pesce, A.M.; Leodori, G.; Garzi, G.; Miglionico, M.; Tabolli, S.; Quinti, I. Health-related quality of life in common variable immunodeficiency Italian patients switched to remote assistance during the COVID-19 pandemic. J. Allergy Clin. Immunol. Pract. 2020, 8, 1894–1899. [Google Scholar] [CrossRef]
- Casale, S.; Flett, G.L. Interpersonally-based fears during the COVID-19 pandemic: Reflections on the fear of missing out and the fear of not mattering constructs. Clin. Neuropsychiatry 2020, 17, 88–93. [Google Scholar] [CrossRef]
- Goodman-Casanova, J.M.; Marian, J.; Dura-Perez, E.; Guzman-Parra, J.; Cuesta-Vargas, A.; Mayoral-Cleries, F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: Survey study. J. Med. Internet Res. 2020, 22, e19434. [Google Scholar] [CrossRef] [PubMed]
- Padala, S.P.; Jendro, A.M.; Orr, L.C. Facetime to reduce behavioral problems in a nursing home resident with Alzheimer’s dementia during COVID-19. Psychiatry Res. 2020, 288, 113028. [Google Scholar] [CrossRef] [PubMed]
- Rozanova, J.; Shenoi, S.; Zaviryukha, I.; Zeziulin, O.; Kiriazova, T.; Rich, K.; Mamedova, E.; Yariy, V. Social support is key to retention in care during Covid-19 pandemic among older people with HIV and substance use disorders in Ukraine. Subst. Use Misuse 2020, 55, 1902–1904. [Google Scholar] [CrossRef] [PubMed]
- Rodler, S.; Apfelbeck, M.; Schulz, G.B.; Ivanova, T.; Buchner, A.; Staehler, M.; Heinemann, V.; Stief, C.; Casuscelli, J. Telehealth in uro-oncology beyond the pandemic: Toll or lifesaver? Eur. Urol. Focus 2020, 6, 1097–1103. [Google Scholar] [CrossRef]
- Umucu, E.; Lee, B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil. Psychol. 2020, 65, 193–198. [Google Scholar] [CrossRef]
- Vanni, G.; Materazzo, M.; Pelliciaro, M.; Ingallinella, S.; Rho, M.; Santori, F.; Cotesta, M.; Caspi, J.; Makarova, A.; Pisolese, C.A.; et al. Breast cancer and COVID-19: The effect of fear on patients’ decision-making process. In Vivo 2020, 34, 1651–1659. [Google Scholar] [CrossRef]
- Chong, T.W.; Curran, E.; Ames, D.; Lautenschlager, N.T.; Castle, D.J. Mental health of older adults during the COVID-19 pandemic: Lessons from history to guide our future. Int. Psychogeriatr. 2020, 32, 1249–1250. [Google Scholar] [CrossRef]
- Abayneh, S.; Lempp, H.; Manthorpe, J.; Hanlon, C. Development of programme theory for integration of service user and caregiver involvement in mental health system strengthening: Protocol for realist systematic review. Int. J. Ment. Health Syst. 2018, 12, 41. [Google Scholar] [CrossRef]
- Blair, A.; Ross, N.A.; Gariepy, G.; Schmitz, N. How do neighborhoods affect depression outcomes? A realist review and a call for the examination of causal pathways. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 873–887. [Google Scholar] [CrossRef]
- Dalkin, S.; Forster, N.; Hodgson, P.; Lhussier, M.; Philipson, P.; Carr, S. Exposing the impact of intensive advice services on health: A realist evaluation. Health Soc. Care Community 2019, 27, 767–776. [Google Scholar] [CrossRef]
- De Weger, E.; Van Vooren, N.; Luijkx, K.; Baan, C.; Drewes, H. Achieving successful community engagement: A rapid realist review. BMC Health Serv. Res. 2018, 18, 285. [Google Scholar] [CrossRef]
- Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Speigel, J. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: A realist review. Int. J. Environ. Res. Public Health 2019, 16, 4396. [Google Scholar] [CrossRef] [Green Version]
- Husk, K.; Blockley, K.; Lovell, R.; Bethel, A.; Lang, I.; Byng, R.; Garside, R. What approaches to social prescribing work, for whom, and in what circumstances? A realist review. Health Soc. Care Community 2020, 28, 309–324. [Google Scholar] [CrossRef] [Green Version]
- James, K.; Brooks, H.; Susanti, H.; Waddingham, J.; Irmansyah, I.; Keliat, B.-A.; Utomo, B.; Rose, D.; Colucci, E.; Lovell, K. Implementing civic engagement within mental health services in South East Asia: A systematic review and realist synthesis of current evidence. Int. J. Ment. Health Syst. 2020, 14, 17. [Google Scholar] [CrossRef]
- Keady, J.; Campbell, S.; Barnes, H.; Ward, R.; Li, X.; Swarbrick, C.; Burrow, S.; Elvish, R. Neighbourhoods and dementia in the health and social care context: A realist review of the literature and implications for UK policy development. Rev. Clin. Gerontol. 2012, 22, 150–163. [Google Scholar] [CrossRef]
- Lamontagne-Godwin, F.; Burgess, C.; Clement, S.; Gasston-Hales, M.; Greene, C.; Manyande, A.; Taylor, D.; Walters, P.; Barley, E. Interventions to increase access to or uptake of physical health screening in people with severe mental illness: A realist review. BMJ Open 2018, 8, e019412. [Google Scholar] [CrossRef]
- O’Campo, P.; Kirst, M.; Schaefer-McDaniel, N.; Firestone, M.; Scott, A.; McShane, K. Community-based services for homeless adults experiencing concurrent mental health and substance use disorders: A realist approach to synthesizing evidence. J. Urban Health 2009, 86, 965–989. [Google Scholar] [CrossRef] [Green Version]
- Tyler, I.; Lynam, J.; O’Campo, P.; Manson, H.; Lynch, M.; Dashti, B.; Turner, N.; Feller, A.; Ford-Jones, E.; Makin, S.; et al. It takes a village: A realist synthesis of social pediatrics program. Int. J. Public Health 2019, 64, 691–701. [Google Scholar] [CrossRef] [Green Version]
- Rogers, E.M. Diffusion of Innovations; The Free Press of Glencoe: New York, NY, USA, 1962. [Google Scholar]
- Hinton, D.E.; Patel, A. Cultural adaptations of cognitive behavioral therapy. Psychiatr. Clin. 2017, 40, 701–714. [Google Scholar] [CrossRef]
- Crumlish, N.; O’Rourke, K. A systematic review of treatments for post-traumatic stress disorder among refugees and asylum-seekers. J. Nerv. Ment. Dis. 2010, 198, 237–251. [Google Scholar] [CrossRef]
- Zimmerman, M.A.; Rappaport, J. Citizen participation, perceived control, and psychological empowerment. Am. J. Commun. Psychol. 1988, 16, 725–750. [Google Scholar] [CrossRef] [PubMed]
- Valente, T.W.; Fujimoto, K. Bridging: Locating critical connectors in a network. Soc. Netw. 2010, 32, 212–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maunder, R.G.; Leszcz, M.; Savage, D.; Adam, M.A.; Peladeau, N.; Romano, D.; Rose, M.; Schulman, R.B. Applying the lessons of SARS to pandemic influenza. Can. J. Public Health. 2008, 99, 486–488. [Google Scholar] [CrossRef] [PubMed]
- Carman, K.L.; Dardess, P.; Maurer, M.; Sofaer, S.; Adams, K.; Bechtel, C.; Sweeney, J. Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Aff. 2013, 32, 223–231. [Google Scholar] [CrossRef]
- McDermott, J.; Resnick, D.; Naylor, N. Resilience: From policy responses to resilient policy systems. In Global Food Policy Report; International Food Policy Research Institute: Washington, DC, USA, 2021; pp. 24–35. [Google Scholar]
| Authors and Year | Country | Topic of Paper |
|---|---|---|
| Chevance et al. 2020 [10] | France | Ensuring mental health care |
| Chakraborty 2020 [17] | UK | Mental health exacerbation |
| Khan et al. 2020 [18] | China | Psychological health |
| Wang et al. 2020 [19] | China | Blood glucose management |
| Razai et al. 2020 [20] | UK | Mitigating social isolation |
| Pulvirenti et al. 2020 [21] | Italy | Remote assistance for immunodeficient patients |
| Casale and Flett 2020 [22] | Italy, Canada | Interpersonally based fears |
| Goodman-Casanova et al. 2020 [23] | Spain | Telehealth home support |
| Padala et al. 2020 [24] | US | FaceTime use with Alzheimer’s patients |
| Rozanova et al. 2020 [25] | Ukraine | Social support for vulnerable seniors with HIV and substance use |
| Rodler et al. 2020 [26] | Germany | Telehealth |
| Umucu and Lee 2020 [27] | US | Coping strategies |
| Vanni et al. 2020 [28] | Italy | Decision-making process |
| Chong et al. 2020 [29] | Australia | Social isolation and older adults |
| Mechanism | Socioecological Level | Context–Mechanism–Outcome (CMO) |
|---|---|---|
| Trust | Macro Policy/Government | When the government ensures timely access to valid information and mental health support services (C), negative emotions, such as anxiety and fear are decreased (O) due to trust (M) in the government’s capacity to meet public needs. |
| Meso Community/Primary Care | When well-known, established community services and providers are used to promote mental health interventions (C), public engagement and uptake of services is increased (O), due to community/provider trust (M). | |
| Micro Individual/Family | When support workers already have relationships with clients, their families and carers (C), clients and families are more apt to follow guidance (O) due to trust (M) in worker knowledge of their specific needs. | |
| Social Connectedness | Macro Policy/Government | When the government funds volunteer and trained staff outreach (C), at-risk individuals (e.g., isolated seniors in their homes) are at decreased risk for mental and physical health deterioration (O) due to social connectedness (M). |
| Meso Community/Primary Care | When primary care providers use social prescribing with patients (C) patients are better able to meet their mental and physical health needs (O), because they are socially connected (M) to a range of community services. | |
| Micro Individual/Family | When individuals are at risk of emotional and behavioural difficulties due to isolation (C), negative experiences from confinement are reduced (O) by staying socially connected (M) via support networks and technology use. | |
| Accountability | Macro Policy/Government | When public health officers provide factual, timely information to the media (C) the public concerns about COVID-19 are decreased (O) due to government accountability for communications about public health response. |
| Resilience | Macro Policy/Government | When regulatory and communications barriers are lowered (C), the public has means to stay social connected (O) due to government resilience (M) |
| Meso Community/Primary care | When primary care providers and community services are re-organised to consider access of services for at-risk patients (C), recurrences of mental health exacerbations can be decreased (O) due to service resilience (M). When primary care providers use mental health screening tools with patients (C), proactive mental health promotion strategies can be implemented (O) due to resilient attention (M) to increased anxiety and depression during COVID-19 | |
| Micro Individual/Family | When individuals learn how to use adaptive coping strategies, such as acceptance and self-distraction (C), there are lower levels or negative emotions from COVID-19 (e.g., anxiety, depression (O) due to personal resilience (M). |
| Authors and Year | Country | Topic Focus of Review |
|---|---|---|
| Abayneh et al. 2018 [30] | Ethiopia | Service user and caregiver involvement |
| Blair et al. 2014 [31] | Canada | Neighbourhood variables and depression |
| Dalkin et al. 2018 [32] | UK | Impact of intensive advice services on health |
| De Weger et al. 2018 [33] | The Netherlands | Community engagement in developing health and care systems |
| Gray et al. 2019] [34] | South Africa, and Canada | Promoting mental health and wellbeing among healthcare workers |
| Husk et al. 2020 [35] | UK | Approaches to social prescribing |
| James et al. 2020 [36] | Indonesia/UK | Civic engagement within mental health services |
| Keady et al. 2012 [37] | UK | Neighbourhood variables and dementia |
| Lamontagne-Godwin et al. 2018 [38] | UK | Physical health screening in people with severe mental illness |
| O’Campo et al. 2009 [39] | Canada | Community-based services for homeless adults experiencing concurrent mental health and substance use disorders |
| Tyler et al. 2019 [40] | Canada | Social paediatric initiatives |
| Mechanism | Summary | Recommendation |
|---|---|---|
| Trust | Trust depends on pre-existing relationships or networks. Trust relationships across levels depend on timely access to needed information and services. | Policy makers and practitioners implementing mental health interventions are more likely to develop effective programs if they, first and foremost, invest in ongoing and long-standing relationships with key stakeholders with whom they share decision-making. This will allow the programs to be more appropriate, responsive, resilient to crisis, and to have greater uptake. |
| Accountability | Stakeholder engagement increases accountability and uptake of collaboratively planned services. | Accountability at each systems level can be promoted by engaging key stakeholders in shared decision-making. However, it is important to consider using models of community engagement and participatory models which aim to ‘level’ the playing field between stakeholders. |
| Social Connectedness | Social connection is vital to improved health and well-being. | Technological innovations and services, such as social prescribing need to be formalised, advertised, and promoted at each systems level. |
| Resilience | The pandemic triggered quick, responsive organisational and service resilience. Sustainable resilience may depend on relational reserves and long-standing, and ongoing relationship-building with key stakeholders, especially users. | Building and maintaining resilience should be a focus across all levels of complex health systems, with on-going examination and mitigation of stresses and upstream/downstream impacts. |
| Power-sharing | Although we did not find this mechanism in our RRR of the scoping review literature during the pandemic, we believe that this mechanism is closely related to the other mechanisms, especially trust, accountability, and resilience. | The best way to share power at each systems level is via participatory models of planning, implementation and evaluation of mental health services. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stabler, L.; MacPhee, M.; Collins, B.; Carroll, S.; Davison, K.; Thakkar, V.; Fuller-Thomson, E.; Lin, S.; Hey, B. A Rapid Realist Review of Effective Mental Health Interventions for Individuals with Chronic Physical Health Conditions during the COVID-19 Pandemic Using a Systems-Level Mental Health Promotion Framework. Int. J. Environ. Res. Public Health 2021, 18, 12292. https://doi.org/10.3390/ijerph182312292
Stabler L, MacPhee M, Collins B, Carroll S, Davison K, Thakkar V, Fuller-Thomson E, Lin S, Hey B. A Rapid Realist Review of Effective Mental Health Interventions for Individuals with Chronic Physical Health Conditions during the COVID-19 Pandemic Using a Systems-Level Mental Health Promotion Framework. International Journal of Environmental Research and Public Health. 2021; 18(23):12292. https://doi.org/10.3390/ijerph182312292
Chicago/Turabian StyleStabler, Lorna, Maura MacPhee, Benjamin Collins, Simon Carroll, Karen Davison, Vidhi Thakkar, Esme Fuller-Thomson, Shen (Lamson) Lin, and Brandon Hey. 2021. "A Rapid Realist Review of Effective Mental Health Interventions for Individuals with Chronic Physical Health Conditions during the COVID-19 Pandemic Using a Systems-Level Mental Health Promotion Framework" International Journal of Environmental Research and Public Health 18, no. 23: 12292. https://doi.org/10.3390/ijerph182312292
APA StyleStabler, L., MacPhee, M., Collins, B., Carroll, S., Davison, K., Thakkar, V., Fuller-Thomson, E., Lin, S., & Hey, B. (2021). A Rapid Realist Review of Effective Mental Health Interventions for Individuals with Chronic Physical Health Conditions during the COVID-19 Pandemic Using a Systems-Level Mental Health Promotion Framework. International Journal of Environmental Research and Public Health, 18(23), 12292. https://doi.org/10.3390/ijerph182312292







_Lin.jpg)

