Trends and Inequalities in the Incidence of Acute Myocardial Infarction among Beijing Townships, 2007–2018
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Data Sources
2.3. Statistical Analysis
3. Results
3.1. Temporal Trends in AMI Incidence
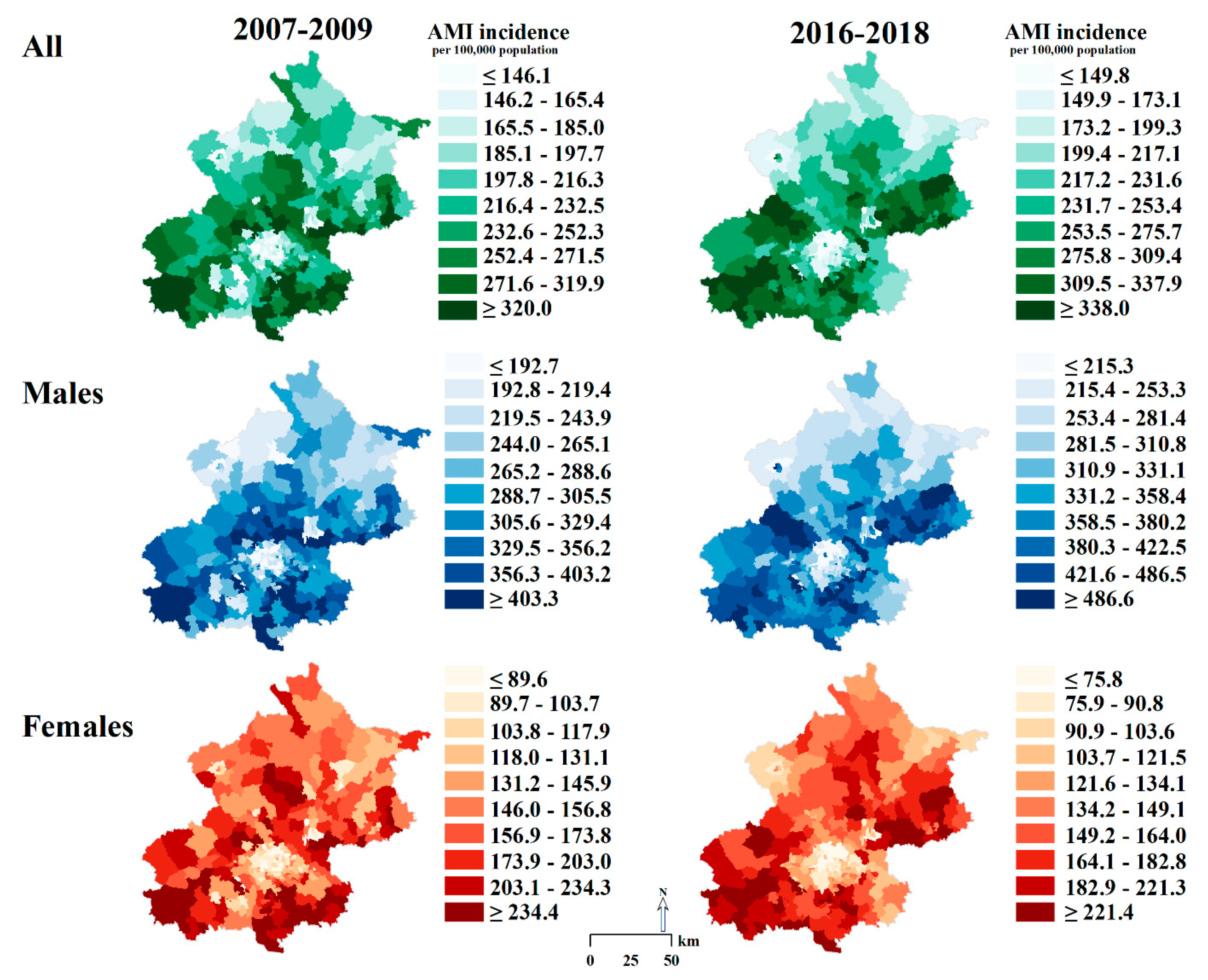
3.2. Geographic Pattern and Inequality in AMI Incidence
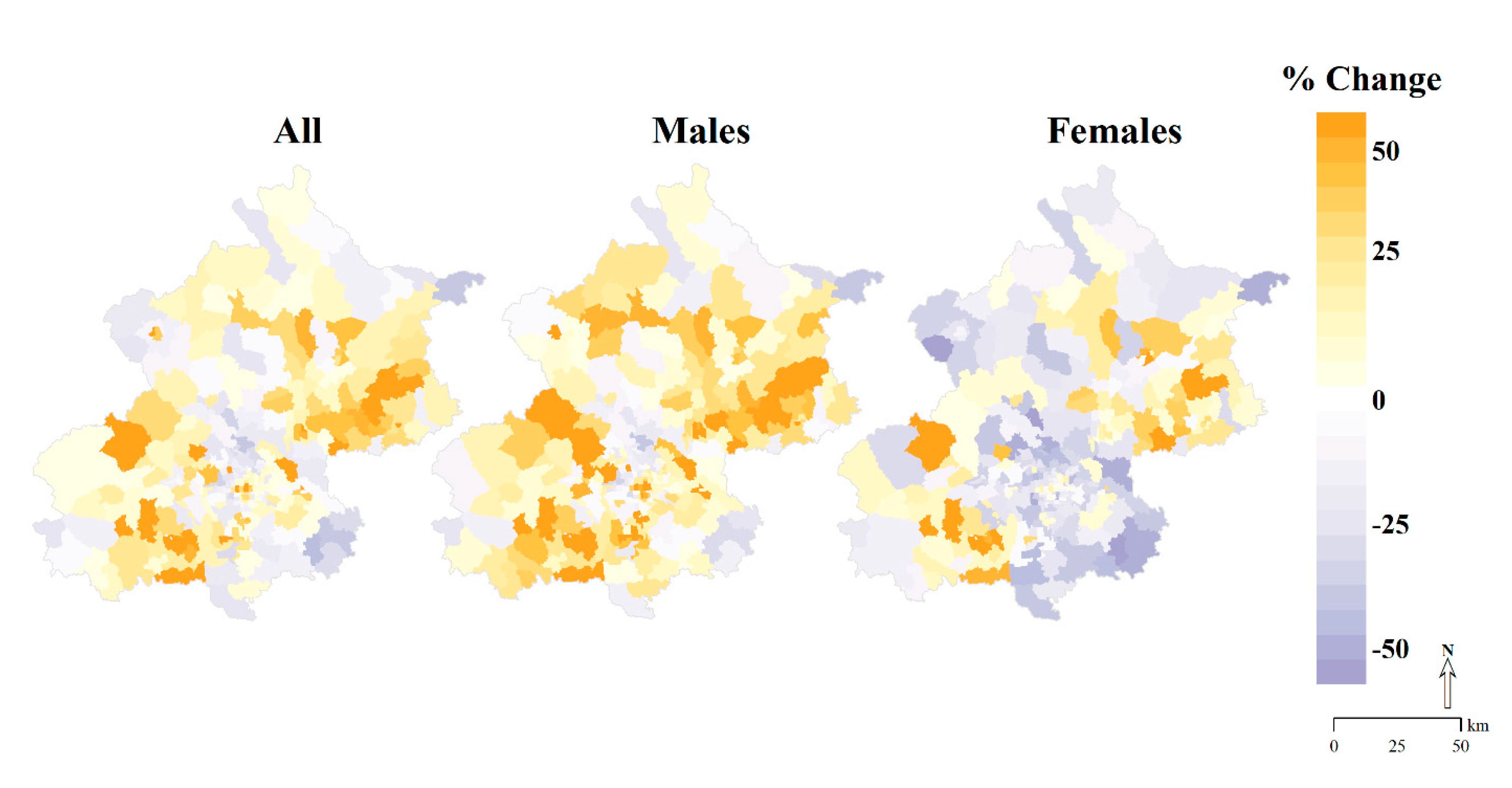
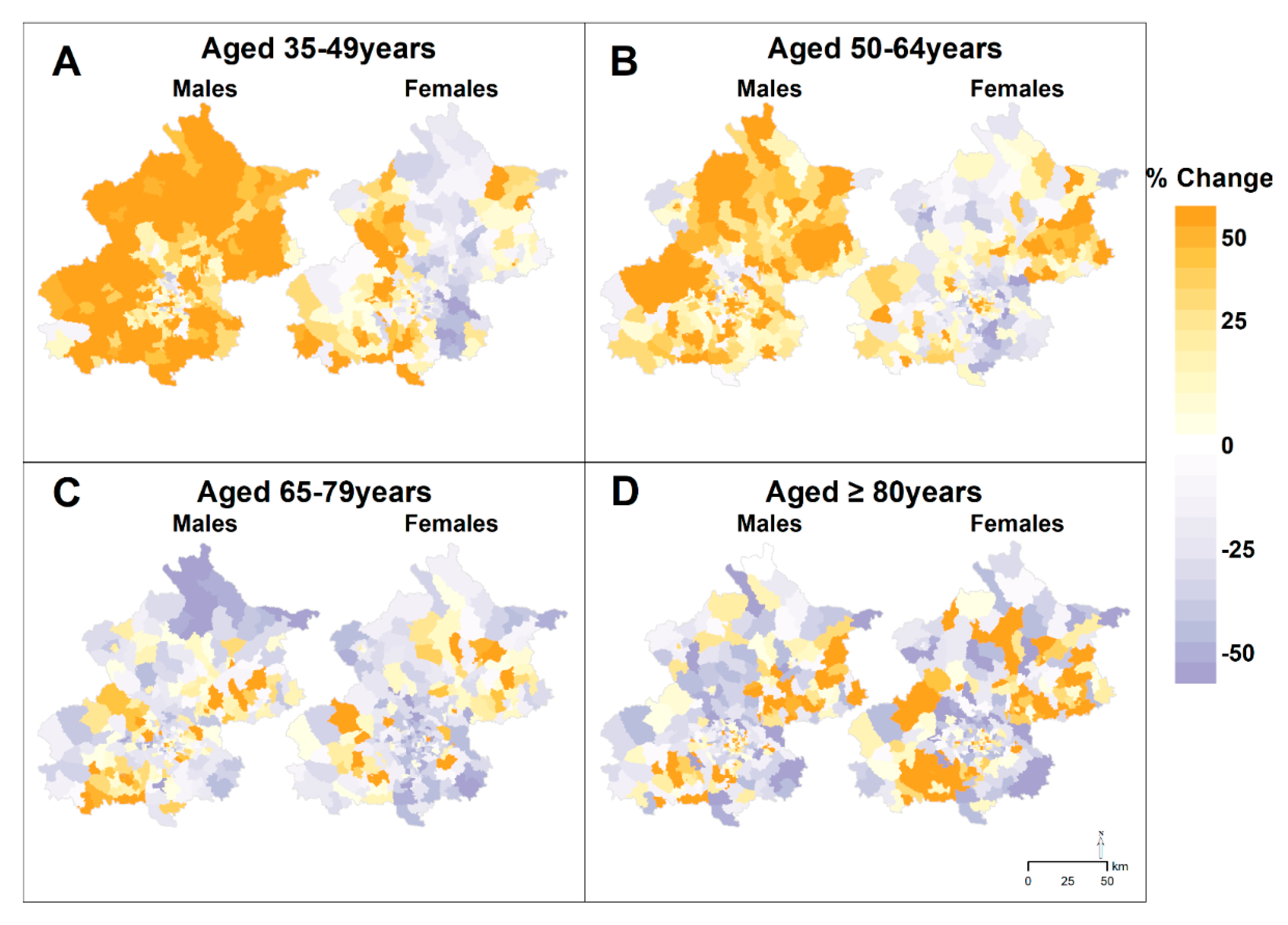
3.3. Geographic Patterns in Changes of AMI Incidence
3.4. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef]
- Dégano, I.R.; Salomaa, V.; Veronesi, G.; Ferriéres, J.; Kirchberger, I.; Laks, T.; Havulinna, A.S.; Ruidavets, J.-B.; Ferrario, M.M.; Meisinger, C.; et al. Twenty-five-year trends in myocardial infarction attack and mortality rates, and case-fatality, in six European populations. Heart 2015, 101, 1413–1421. [Google Scholar] [CrossRef] [PubMed]
- Rosamond, W.D.; Chambless, L.E.; Heiss, G.; Mosley, T.H.; Coresh, J.; Whitsel, E.; Wagenknecht, L.; Ni, H.; Folsom, A.R. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation 2012, 125, 1848–1857. [Google Scholar] [CrossRef] [PubMed]
- Geldsetzer, P.; Manne-Goehler, J.; Theilmann, M.; Davies, J.I.; Awasthi, A.; Danaei, G.; Gaziano, T.A.; Vollmer, S.; Jaacks, L.M.; Bärnighausen, T.; et al. Geographic and sociodemographic variation of cardiovascular disease risk in India: A cross-sectional study of 797,540 adults. PLoS Med. 2018, 15, e1002581. [Google Scholar] [CrossRef]
- Bai, L.; Shin, S.; Burnett, R.T.; Kwong, J.C.; Hystad, P.; van Donkelaar, A.; Goldberg, M.S.; Lavigne, E.; Copes, R.; Martin, R.V.; et al. Exposure to ambient air pollution and the incidence of congestive heart failure and acute myocardial infarction: A population-based study of 5.1 million Canadian adults living in Ontario. Environ. Int. 2019, 132, 105004. [Google Scholar] [CrossRef]
- Roth, G.A.; Dwyer-Lindgren, L.; Bertozzi-Villa, A.; Stubbs, R.W.; Morozoff, C.; Naghavi, M.; Mokdad, A.H.; Murray, C.J.L. Trends and patterns of geographic variation in cardiovascular mortality among US counties, 1980–2014. JAMA 2017, 317, 1976–1992. [Google Scholar] [CrossRef]
- Casper, M.; Kramer, M.R.; Quick, H.; Schieb, L.J.; Vaughan, A.S.; Greer, S. Changes in the geographic patterns of heart disease mortality in the United States: 1973 to 2010. Circulation 2016, 133, 1171–1180. [Google Scholar] [CrossRef]
- Asaria, P.; Fortunato, L.; Fecht, D.; Tzoulaki, I.; Abellan, J.J.; Hambly, P.; Hoogh, K.d.; Ezzati, M.; Elliott, P. Trends and inequalities in cardiovascular disease mortality across 7932 English electoral wards, 1982–2006: Bayesian spatial analysis. Int. J. Epidemiol. 2012, 41, 1737–1749. [Google Scholar] [CrossRef]
- Viik-Kajander, M.; Moltchanova, E.; Salomaa, V.; Tuomilehto, J.; Ketonen, M.; Palomäki, P.; Miettinen, H.; Pyörälä, K.; Karvonen, M. Geographical variation in the incidence of acute myocardial infarction in eastern Finland--a Bayesian perspective. Ann. Med. 2003, 35, 43–50. [Google Scholar] [CrossRef]
- Xie, W.; Li, G.; Zhao, D.; Xie, X.; Wei, Z.; Wang, W.; Wang, M.; Li, G.; Liu, W.; Sun, J.; et al. Relationship between fine particulate air pollution and ischaemic heart disease morbidity and mortality. Heart 2015, 101, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ma, R.; Ban, J.; Lu, F.; Guo, M.; Zhong, Y.; Jiang, N.; Chen, C.; Li, T.; Shi, X. Risk of cardiovascular hospital admission after exposure to fine particulate pollution. J. Am. Coll. Cardiol. 2021, 78, 1015–1024. [Google Scholar] [CrossRef]
- Asaria, P.; Elliott, P.; Douglass, M.; Obermeyer, Z.; Soljak, M.; Majeed, A.; Ezzati, M. Acute myocardial infarction hospital admissions and deaths in England: A national follow-back and follow-forward record-linkage study. Lancet Public Health 2017, 2, e191–e201. [Google Scholar] [CrossRef]
- Liu, R.; Liu, X.; Yang, P.; Du, X.; He, L.; Chen, T.; Li, X.; Xie, G.; Wu, S.; Su, J.; et al. Influenza-associated cardiovascular mortality in older adults in Beijing, China: A population-based time-series study. BMJ Open. 2020, 10, e042487. [Google Scholar] [CrossRef]
- Chen, J.; Normand, S.L.; Wang, Y.; Drye, E.E.; Schreiner, G.C.; Krumholz, H.M. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: Progress and continuing challenges. Circulation 2010, 121, 1322–1328. [Google Scholar] [CrossRef]
- WHO MONICA Project. MONICA Manual, Part IV: Event Registration. Available online: https://www.thl.fi/publications/monica/manual/part4/iv-1.htm (accessed on 13 October 2021).
- Bearak, J.M.; Burke, K.L.; Jones, R.K. Disparities and change over time in distance women would need to travel to have an abortion in the USA: A spatial analysis. Lancet Public Health 2017, 2, e493–e500. [Google Scholar] [CrossRef]
- Amsalu, E.; Liu, M.; Li, Q.; Wang, X.; Tao, L.; Liu, X.; Luo, Y.; Yang, X.; Zhang, Y.; Li, W.; et al. Spatial-temporal analysis of cause-specific cardiovascular hospital admission in Beijing, China. Int. J. Environ. Health Res. 2021, 31, 595–606. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wu, Y.; Wu, J.; Wang, M.; Wang, X.; Wang, J.; Wu, T.; Wu, Y.; Hu, Y. Trends in prevalence and incidence of type 2 diabetes among adults in Beijing, China, from 2008 to 2017. Diabet. Med. 2021, 38, e14487. [Google Scholar] [CrossRef]
- Li, G.; Hu, H.; Dong, Z.; Xie, J.; Zhou, Y. Urban and suburban differences in hypertension trends and self-care: Three population-based cross-sectional studies from 2005–2011. PLoS ONE 2015, 10, e0117999. [Google Scholar] [CrossRef]
- Cai, L.; Zhang, L.; Liu, A.; Li, S.; Wang, P. Prevalence, awareness, treatment, and control of dyslipidemia among adults in Beijing, China. J. Atheroscler. Thromb. 2012, 19, 159–168. [Google Scholar] [CrossRef]
- Zhang, Y.; Moran, A.E. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension 2017, 70, 736–742. [Google Scholar] [CrossRef]
- Cai, L.; Han, X.; Qi, Z.; Li, Z.; Zhang, Y.; Wang, P.; Liu, A. Prevalence of overweight and obesity and weight loss practice among Beijing adults, 2011. PLoS ONE 2014, 9, e98744. [Google Scholar] [CrossRef]
- He, L.; Tang, X.; Song, Y.; Li, N.; Li, J.; Zhang, Z.; Liu, J.; Yu, L.; Xu, H.; Zhang, J.; et al. Prevalence of cardiovascular disease and risk factors in a rural district of Beijing, China: A population-based survey of 58,308 residents. BMC Public Health 2012, 12, 34. [Google Scholar] [CrossRef]
- Zhou, X.; Li, Y.; Zhang, X.; Guan, Y.Y.; Puentes, Y.; Zhang, F.; Speliotes, E.K.; Ji, L. Independent markers of nonalcoholic fatty liver disease in a gentrifying population-based Chinese cohort. Diabetes Metab. Res. Rev. 2019, 35, e3156. [Google Scholar] [CrossRef] [PubMed]
- Callaghan, B.C.; Gao, L.; Li, Y.; Zhou, X.; Reynolds, E.; Banerjee, M.; Pop-Busui, R.; Feldman, E.L.; Ji, L. Diabetes and obesity are the main metabolic drivers of peripheral neuropathy. Ann. Clin. Transl. Neurol. 2018, 5, 397–405. [Google Scholar] [CrossRef] [PubMed]
- The People’s Government of Beijing Municipality. Beijing’s Stipulation on the Scope of Public Place Smoking Ban Beijing. 2008. Available online: http://www.beijing.gov.cn/zhengce/zfwj/zfwj/szfl/201905/t20190523_75989.html (accessed on 13 October 2021).
- Yang, S.; He, Y.; Liu, M.; Wang, Y.; Wu, L.; Wang, J.; Zhang, D.; Zeng, J.; Jiang, B.; Li, X. Changes in and patterns of smoking exposure in an elderly urban population in Beijing: 2001–2010. PLoS ONE 2015, 10, e0118500. [Google Scholar] [CrossRef][Green Version]
- Wu, Y.; Wang, Z.; Zheng, Y.; Wang, M.; Wang, S.; Wang, J.; Wu, J.; Wu, T.; Chang, C.; Hu, Y. The impact of comprehensive tobacco control policies on cardiovascular diseases in Beijing, China. Addiction 2021, 116, 2175–2184. [Google Scholar] [CrossRef]
- Beijing Municipal Health Commission Information Center/Policy Research Center. Beijing Health Statistical Yearbook 2007–2018. Available online: http://www.phic.org.cn/tjsj/wstjjb/ (accessed on 13 October 2021).
- Ministry of Ecology and Environment of the People’s Republic of China. Regulations of Beijing Municipality on Atmospheric Pollution Prevention and Control. Available online: http://www.mee.gov.cn/home/ztbd/rdzl/dqst/mbzrs/201504/P020150422602290709204.pdf (accessed on 13 October 2021).
- The People’s Government of Beijing Municipality. Beijing 2013–2017 Clean Air Action Plan. Available online: http://www.beijing.gov.cn/zhengce/zfwj/zfwj/szfwj/201905/t20190523_72673.html (accessed on 13 October 2021).
- Zhang, L.; An, J.; Liu, M.; Li, Z.; Liu, Y.; Tao, L.; Liu, X.; Zhang, F.; Zheng, D.; Gao, Q.; et al. Spatiotemporal variations and influencing factors of PM2.5 concentrations in Beijing, China. Environ. Pollut. 2020, 262, 114276. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Sudharsanan, N.; Huang, F.; Liu, Y.; Geldsetzer, P.; Bärnighausen, T. Impact of community based screening for hypertension on blood pressure after two years: Regression discontinuity analysis in a national cohort of older adults in China. BMJ 2019, 366, l4064. [Google Scholar] [CrossRef]
- Su, M.; Zhang, Q.; Bai, X.; Wu, C.; Li, Y.; Mossialos, E.; Mensah, G.A.; Masoudi, F.A.; Lu, J.; Li, X.; et al. Availability, cost, and prescription patterns of antihypertensive medications in primary health care in China: A nationwide cross-sectional survey. Lancet 2017, 390, 2559–2568. [Google Scholar] [CrossRef]
- Tang, S.; Ehiri, J.; Long, Q. China’s biggest, most neglected health challenge: Non-communicable diseases. Infect. Dis. Poverty 2013, 2, 7. [Google Scholar] [CrossRef] [PubMed]
- Caswell, J.M. Exploring spatial trends in Canadian incidence of hospitalization due to myocardial infarction with additional determinants of health. Public Health 2016, 140, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Odoi, E.W.; Nagle, N.; Roberson, S.; Kintziger, K.W. Geographic disparities and temporal changes in risk of death from myocardial infarction in Florida, 2000–2014. BMC Public Health 2019, 19, 505. [Google Scholar] [CrossRef]
- Odoi, A.; Busingye, D. Neighborhood geographic disparities in heart attack and stroke mortality: Comparison of global and local modeling approaches. Spat. Spatiotemporal Epidemiol. 2014, 11, 109–123. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, A.S.; Quick, H.; Pathak, E.B.; Kramer, M.R.; Casper, M. Disparities in temporal and geographic patterns of declining heart disease mortality by race and sex in the United States, 1973–2010. J. Am. Heart Assoc. 2015, 4, e002567. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhao, D.; Xie, W.; Xie, X.; Guo, M.; Wang, M.; Wang, W.; Liu, W.; Liu, J. Recent trends in hospitalization for acute myocardial infarction in Beijing: Increasing overall burden and a transition from ST-segment elevation to non-ST-segment elevation myocardial infarction in a population-based study. Medicine (Baltimore) 2016, 95, e2677. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhao, D.; Xie, W.; Xie, X.; Guo, M.; Wang, M.; Wang, W.; Liu, W.; Liu, J. Bayesian image restoration, with two applications in spatial statistics. Ann. Inst. Stat. Math. 1991, 43, 1–20. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | 2007–2009 | 2010–2012 | 2013–2015 | 2016–2018 | ||||
|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | |
| Total a | 216.3 | (176.0, 259.5) | 239.5 | (192.9, 289.4) | 236.2 | (184.5, 297.3) | 231.6 | (188.4, 286.1) |
| Males b | 288.6 | (230.1, 337.6) | 316.4 | (253.1, 376.7) | 318.9 | (253.7, 393.2) | 331.1 | (267.5, 396.9) |
| 35–49 years | 96.5 | (76.7, 113.9) | 118.8 | (95.4, 142.6) | 137.0 | (103.7, 170.9) | 148.8 | (108.6, 183.4) |
| 50–64 years | 279.8 | (215.2, 342.8) | 317.5 | (258.3, 378.2) | 336.1 | (264.8, 416.7) | 372.6 | (297.6, 447.6) |
| 65–79 years | 686.2 | (577.7, 855.5) | 729.6 | (577.7, 911.4) | 669.3 | (541.5, 894.8) | 645.2 | (506.0, 831.5) |
| ≥80 years | 1282.0 | (976.1, 1852.0) | 1378.0 | (1021.0, 1832.0) | 1262.0 | (958.8, 1733.0) | 1301.0 | (970.0, 1718.0) |
| Females b | 145.9 | (108.5, 186.1) | 162.8 | (116.6, 206.6) | 148.2 | (106.5, 199.4) | 134.1 | (98.3, 174.3) |
| 35–49 years | 12.2 | (8.2, 15.7) | 12.3 | (7.5, 16.3) | 12.6 | (8.0, 18.4) | 12.3 | (7.2, 16.0) |
| 50–64 years | 85.3 | (37.4, 134.4) | 100.3 | (63.6, 124.5) | 87.2 | (54.4, 116.8) | 83.1 | (57.3, 105.8) |
| 65–79 years | 525.5 | (393.0, 639.3) | 562.9 | (421.2, 695.6) | 500.6 | (370.7, 657.5) | 445.9 | (315.8, 574.5) |
| ≥80 years | 1220.0 | (917.2, 1670.0) | 1372.0 | (940.0, 1974.0) | 1317.0 | (937.9, 1883.0) | 1192.0 | (881.4, 1687.0) |
| 2007–2009 | 2010–2012 | 2013–2015 | 2016–2018 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | 10th Percentile | 90th Percentile | 90th–10th a | 90th/ 10th b | 10th Percentile | 90th Percentile | 90th–10th a | 90th/ 10th b | 10th Percentile | 90th Percentile | 90th–10th a | 90th/ 10th b | 10th Percentile | 90th Percentile | 90th–10th a | 90th/ 10th b |
| Total c | 146.1 | 319.9 | 173.8 | 2.2 | 147.5 | 352.1 | 204.6 | 2.4 | 147.5 | 355.5 | 208.0 | 2.4 | 149.8 | 337.9 | 188.1 | 2.3 |
| Males d | 192.7 | 403.2 | 210.5 | 2.1 | 205.1 | 446.1 | 241.0 | 2.2 | 211.8 | 470.3 | 258.5 | 2.2 | 215.3 | 486.5 | 271.2 | 2.3 |
| 35–49 years | 63.2 | 135.8 | 72.6 | 2.1 | 77.9 | 159.3 | 81.4 | 2.0 | 82.6 | 203.1 | 120.5 | 2.5 | 79.2 | 221.4 | 142.2 | 2.8 |
| 50–64 years | 180.3 | 408.6 | 228.3 | 2.3 | 203.5 | 433.1 | 229.6 | 2.1 | 202.8 | 482.6 | 279.8 | 2.4 | 241.7 | 535.9 | 294.2 | 2.2 |
| 65–79 years | 472.4 | 1053.0 | 580.6 | 2.2 | 458.7 | 1193.0 | 734.3 | 2.6 | 456.4 | 1087.0 | 630.6 | 2.4 | 411.6 | 998.7 | 587.1 | 2.4 |
| ≥ 80 years | 829.9 | 2413.0 | 1583.1 | 2.9 | 798.6 | 2589.0 | 1790.4 | 3.2 | 693.1 | 2425.0 | 1731.9 | 3.5 | 745.8 | 2357.0 | 1611.2 | 3.2 |
| Females d | 89.6 | 234.3 | 144.7 | 2.6 | 85.5 | 262.5 | 177.0 | 3.1 | 80.8 | 248.8 | 168.0 | 3.1 | 75.8 | 221.3 | 145.5 | 2.9 |
| 35–49 years | 6.3 | 17.9 | 11.6 | 2.8 | 6.0 | 22.1 | 16.1 | 3.7 | 5.8 | 27.2 | 21.4 | 4.7 | 5.8 | 19.9 | 14.1 | 3.4 |
| 50–64 years | 37.4 | 134.4 | 97.0 | 3.6 | 38.9 | 153.3 | 114.4 | 3.9 | 37.2 | 147.7 | 110.5 | 4.0 | 41.3 | 131.1 | 89.8 | 3.2 |
| 65–79 years | 312.1 | 830.4 | 518.3 | 2.7 | 316.3 | 932.4 | 616.1 | 2.9 | 291.6 | 855.3 | 563.7 | 2.9 | 231.0 | 721.3 | 490.3 | 3.1 |
| ≥80 years | 707.9 | 2638.0 | 1930.1 | 3.7 | 723.4 | 3042.0 | 2318.6 | 4.2 | 705.5 | 2655.0 | 1949.5 | 3.8 | 679.8 | 2430.0 | 1750.2 | 3.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, J.; Deng, Q.; Guo, M.; Ezzati, M.; Baumgartner, J.; Bixby, H.; Chan, Q.; Zhao, D.; Lu, F.; Hu, P.; et al. Trends and Inequalities in the Incidence of Acute Myocardial Infarction among Beijing Townships, 2007–2018. Int. J. Environ. Res. Public Health 2021, 18, 12276. https://doi.org/10.3390/ijerph182312276
Chang J, Deng Q, Guo M, Ezzati M, Baumgartner J, Bixby H, Chan Q, Zhao D, Lu F, Hu P, et al. Trends and Inequalities in the Incidence of Acute Myocardial Infarction among Beijing Townships, 2007–2018. International Journal of Environmental Research and Public Health. 2021; 18(23):12276. https://doi.org/10.3390/ijerph182312276
Chicago/Turabian StyleChang, Jie, Qiuju Deng, Moning Guo, Majid Ezzati, Jill Baumgartner, Honor Bixby, Queenie Chan, Dong Zhao, Feng Lu, Piaopiao Hu, and et al. 2021. "Trends and Inequalities in the Incidence of Acute Myocardial Infarction among Beijing Townships, 2007–2018" International Journal of Environmental Research and Public Health 18, no. 23: 12276. https://doi.org/10.3390/ijerph182312276
APA StyleChang, J., Deng, Q., Guo, M., Ezzati, M., Baumgartner, J., Bixby, H., Chan, Q., Zhao, D., Lu, F., Hu, P., Su, Y., Sun, J., Long, Y., & Liu, J. (2021). Trends and Inequalities in the Incidence of Acute Myocardial Infarction among Beijing Townships, 2007–2018. International Journal of Environmental Research and Public Health, 18(23), 12276. https://doi.org/10.3390/ijerph182312276








