The Evolution of Telepractice Use during the COVID-19 Pandemic: Perspectives of Pediatric Speech-Language Pathologists
Abstract
:1. Introduction
1.1. Service Disruption and Telepractice as an Alternative to In-Person Services
1.2. Client Family and Clinician Wellbeing during the Pandemic
1.3. The Rural Context of Service Disruption and Transition
1.4. Rapid Evolution of COVID-19-Related Policies
1.5. The Current Research
2. Interview Study
2.1. Participants
2.2. Instrument
2.3. Analytical Strategies
2.4. Results
2.4.1. Theme 1: Changes Due to the Pandemic
2.4.2. Theme 2: Telepractice Is Challenging
2.4.3. Theme 3: Worsening Wellbeing of Clinicians and Clients
2.4.4. Theme 4: Telepractice Should Continue When Appropriate
2.4.5. Theme 5: Suggestions for Future Services
3. Survey Study
3.1. Participants
3.2. Instruments
3.3. Results
4. Discussion
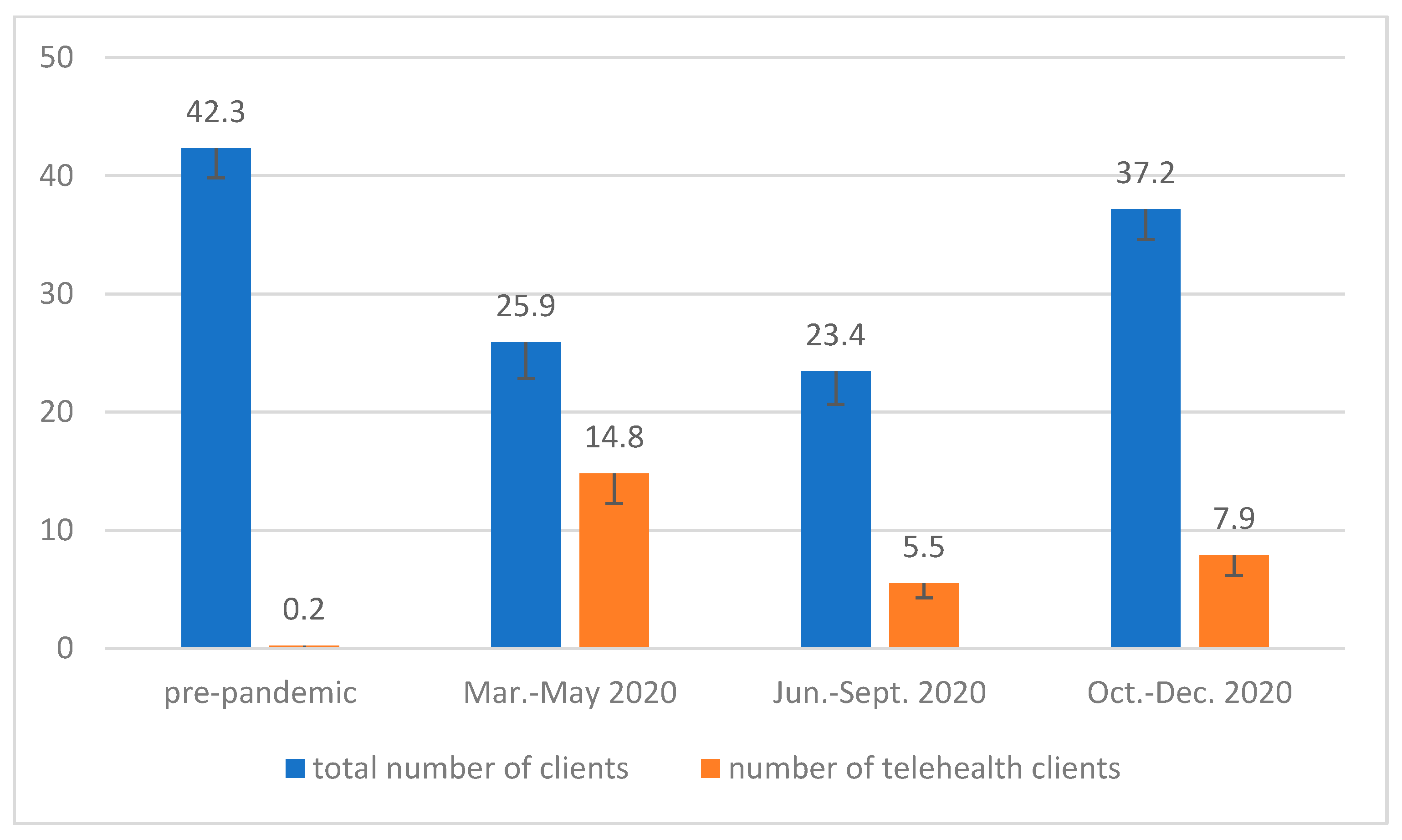
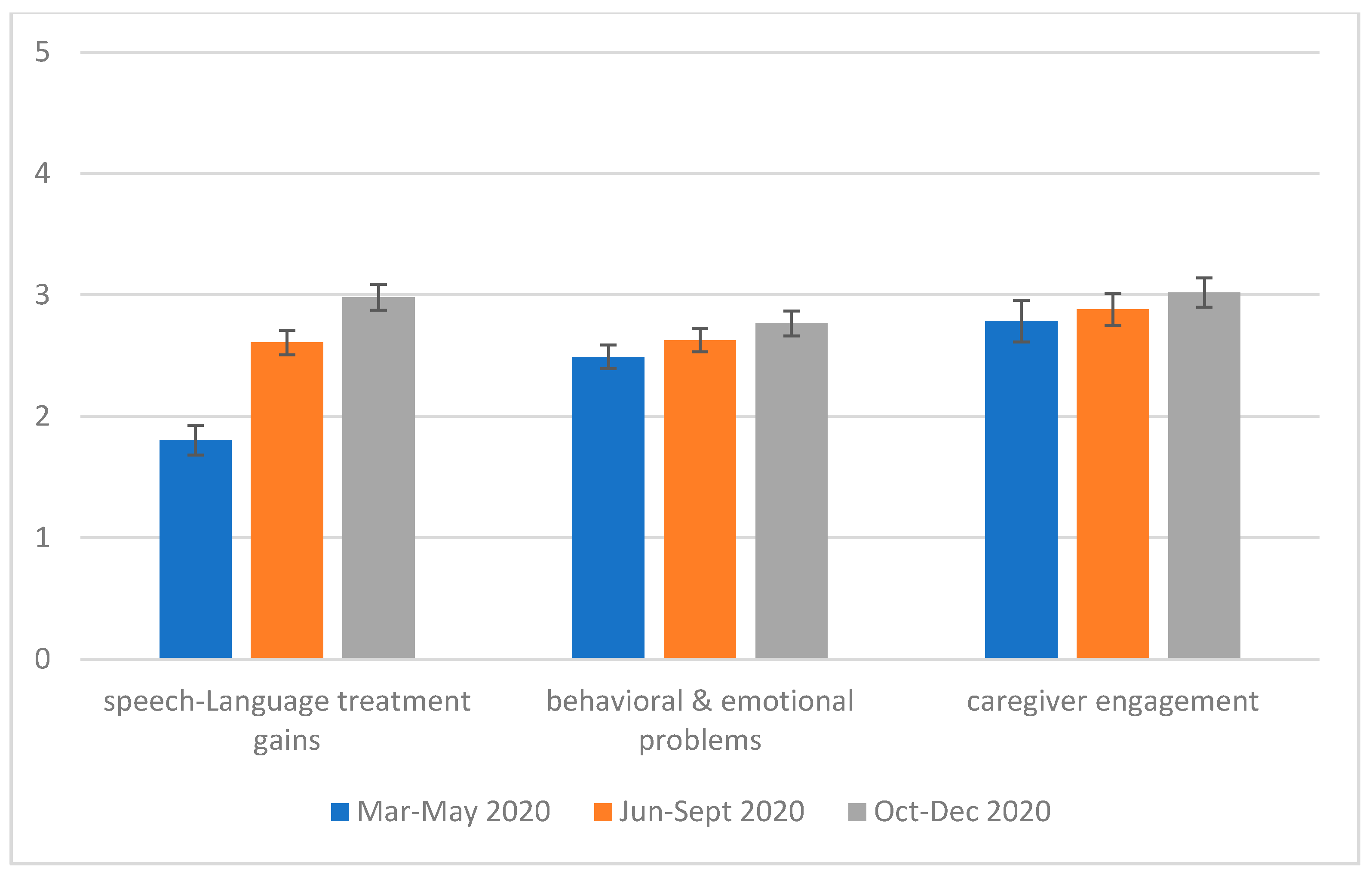
4.1. Service Disruption and Transition
4.2. Strengths and Weaknesses of Telepractice
4.3. Perceptions of Telepractice
4.4. Clinician and Client Wellbeing
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Themes | Subthemes | Codes | Number of SLPs |
|---|---|---|---|
| Changes due to the pandemic | Transition to telehealth | 8 | |
| Losing clients | 6 | ||
| Client regression on previous acquired skills | 6 | ||
| Client increased emotional and behavioral problems | 5 | ||
| Service gap after the pandemic outbreak | 5 | ||
| Shorter duration for sessions | 4 | ||
| Client routine disruption | 2 | ||
| Disinfection needs for clinicians providing in-person services | 2 | ||
| Transition to a coach-parent model | 1 | ||
| A different way to demonstrate intervention materials | 1 | ||
| Overall telehealth is challenging | Challenges | Less hands-on compared to in-person sessions | 8 |
| Hard to engage some children | 8 | ||
| Clinician/Parent lacked training of telehealth | 8 | ||
| Clinician/Parent low acceptance of telehealth (e.g., lacked confidence, telehealth efficacy) | 8 | ||
| Client family readiness | 7 | ||
| Internet access | 7 | ||
| Device availability | 6 | ||
| Clinician adjustment to design and plan telehealth sessions | 6 | ||
| More demands on parents | 6 | ||
| Swift changes | 5 | ||
| Limited insurance coverage for telehealth | 4 | ||
| Hard to engage new clients without establishing rapport in person | 3 | ||
| Hard to implement group sessions to facilitate peer interaction | 3 | ||
| Hard to get quality evaluation results/standardized tests | 3 | ||
| Hard to disseminate to rural households | 2 | ||
| No physical proximity | 2 | ||
| Easy for clients to forget appointment | 2 | ||
| Increased preparation time for telehealth sessions | 2 | ||
| Decreased interdisciplinary support (e.g., OT) | 1 | ||
| Less effective supervision of graduate students due to that supervisor is in a learning process | 1 | ||
| Harder to use AAC devices in teletherapy | 1 | ||
| Too much screen time does not promote in-depth learning | 1 | ||
| Benefits | Improved performance for some children through teletherapy | 9 | |
| More parent involvement to assist intervention | 8 | ||
| More convenience (e.g., reaching rural families, no traveling) | 8 | ||
| Parents could observe intervention strategies | 6 | ||
| Able to serve more clients | 5 | ||
| Having a window to understand how the families manage their situations at home | 3 | ||
| Allowing for continued services without a big gap after the pandemic | 3 | ||
| Addressing families’ needs at the moment | 2 | ||
| More efficient real-time supervision for graduate students (e.g., using chat box to provide instant feedback at the moment) | 1 | ||
| Worsening wellbeing of clinicians and clients | SLP wellbeing | Increased stress levels | 7 |
| Mitigated stress when getting used to the situation | 5 | ||
| Balance between family and work | 5 | ||
| Concerns about client wellbeing (e.g., adequate care) | 5 | ||
| SLPs’ family burdens to take care of their own kids and spouses | 4 | ||
| Potential financial burdens due to caseload reduction | 3 | ||
| Home life being minimally affected | 1 | ||
| Feeling unsafe getting back to in-person services | 1 | ||
| Client wellbeing | Stressful parents during the difficult times | 4 | |
| Significant impacts on client social-emotional wellbeing | 2 | ||
| Financial stress | 1 | ||
| Telehealth should continue in appropriate context | Optimism | Telehealth will continue in the future in appropriate context | 9 |
| Pessimism | Telehealth will not continue due to concerns with its efficacy | 1 | |
| Suggestions for future services | For telehealth services | Better internet connection for some families | 6 |
| Continued telehealth training and more resources available for clinicians | 3 | ||
| A hybrid model with tele- and in-person services to service clients | 2 | ||
| Increased insurance coverage for telehealth that is comparable to in-person services | 2 | ||
| Providing parent technology training | 2 | ||
| Devices available for clients | 2 | ||
| More research for evidence-based practice for telehealth | 2 | ||
| Equity of services for clients with and without access to telehealth services | 1 | ||
| For in-person services | Scheduling adjustment by taking into account of disinfecting time | 3 | |
| More supplies for disinfecting | 1 | ||
| Clients adhering more to CDC guidelines | 1 | ||
| Considering parents’ level of comfort | 1 | ||
| Clinician controlling sanitation in clinic to ensure the safety of in-person services | 1 |
References
- Abbott, A. COVID’s Mental-Health Toll: How Scientists Are Tracking a Surge in Depression. Nature 2021, 590, 194–195. [Google Scholar] [CrossRef]
- López-Bueno, R.; López-Sánchez, G.F.; Casajús, J.A.; Calatayud, J.; Tully, M.A.; Smith, L. Potential health-related behaviors for pre-school and school-aged children during COVID-19 lockdown: A narrative review. Prev. Med. 2020, 143, 106349. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of Covid-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239.e3. [Google Scholar] [CrossRef] [PubMed]
- Chadd, K.; Moyse, K.; Enderby, P. Impact of Covid-19 on the Speech and Language Therapy Profession and Their Patients. Front. Neurol. 2021, 12, 629190. [Google Scholar] [CrossRef] [PubMed]
- American Speech-Language-Hearing Association. ASHA COVID-19 Survey Results—March 2020; American Speech-Language-Hearing Association: Rockville, MD, USA, 2020. [Google Scholar]
- Center for Connected Health Policy. COVID-19 Telehealth Coverage Policies. Available online: https://www.cchpca.org/ (accessed on 9 August 2021).
- Verdon, S.; Wilson, L.; Smith-Tamaray, M.; McAllister, L. An Investigation of Equity of Rural Speech-Language Pathology Services for Children: A Geographic Perspective. Int. J. Speech-Lang. Pathol. 2011, 13, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Ingersoll, B.; Shannon, K.; Berger, N.; Pickard, K.; Holtz, B. Self-Directed Telehealth Parent-Mediated Intervention for Children with Autism Spectrum Disorder: Examination of the Potential Reach and Utilization in Community Settings. J. Med. Internet Res. 2017, 19, e248. [Google Scholar] [CrossRef] [PubMed]
- Sylvan, L.; Goldstein, E.; Crandall, M. Capturing a Moment in Time: A Survey of School-Based Speech-Language Pathologists’ Experiences in the Immediate Aftermath of the COVID-19 Public Health Emergency. Perspect. ASHA Spéc. Interes. Groups 2020, 5, 1735–1749. [Google Scholar] [CrossRef]
- Campbell, D.R.; Goldstein, H. Genesis of a New Generation of Telepractitioners: The COVID-19 Pandemic and Pediatric Speech-Language Pathology Services. Am. J. Speech-Lang. Pathol. 2021, 30, 2143–2154. [Google Scholar] [CrossRef] [PubMed]
- Weidner, K.; Lowman, J. Telepractice for Adult Speech-Language Pathology Services: A Systematic Review. Perspect. ASHA Spec. Interes. Groups 2020, 5, 326–338. [Google Scholar] [CrossRef] [Green Version]
- Wales, D.; Skinner, L.; Hayman, M. The Efficacy of Telehealth-Delivered Speech and Language Intervention for Primary School-Age Children: A Systematic Review. Int. J. Telerehabilit. 2017, 9, 55–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nonweiler, J.; Rattray, F.; Baulcomb, J.; Happé, F.; Absoud, M. Prevalence and Associated Factors of Emotional and Behavioural Difficulties during COVID-19 Pandemic in Children with Neurodevelopmental Disorders. Children 2020, 7, 128. [Google Scholar] [CrossRef]
- Scherer, N.; Verhey, I.; Kuper, H. Depression and Anxiety in Parents of Children with Intellectual and Developmental Disabilities: A Systematic Review and Meta-Analysis. PLoS ONE 2019, 14, e0219888. [Google Scholar] [CrossRef] [PubMed]
- Patrick, S.W.; Henkhaus, L.E.; Zickafoose, J.S.; Lovell, K.; Halvorson, A.; Loch, S.; Letterie, M.; Davis, M.M. Well-Being of Parents and Children during the COVID-19 Pandemic: A National Survey. Pediatrics 2020, 146, e2020016824. [Google Scholar] [CrossRef]
- Aggarwal, K.; Patel, R.; Ravi, R. Uptake of telepractice among speech-language therapists following COVID-19 pandemic in India. Speech Lang. Hear. 2020, 24, 228–234. [Google Scholar] [CrossRef]
- US Census Bureau. Quick Facts Mississippi. Available online: https://www.census.gov/quickfacts/MS (accessed on 20 June 2021).
- America’s Health Ranking. Annual Report 2019. Available online: https://assets.americashealthrankings.org/app/uploads/ahr_2019annualreport.pdf (accessed on 2 May 2021).
- Health Resources & Services Administration. HPSA Find. Available online: https://data.hrsa.gov/tools/shortage-area/hpsa-find (accessed on 9 April 2021).
- McDaniel, J.T.; Davis, T.; Yahaya, M.; Nuhu, K. Descriptive Epidemiology of Childhood Disability Prevalence by Sex in the Mississippi Delta and Appalachian Regions. J. Sch. Health 2019, 89, 969–976. [Google Scholar] [CrossRef]
- WCBI. Governor Tate Reeves Declares State of Emergency to Protect Public Health. Available online: https://www.wcbi.com/governor-tate-reeves-declares-state-emergency-protect-public-health/ (accessed on 3 March 2021).
- WAPT16ABC. Governor Reeves Issues Shelter-In-Place Order for Lauderdale County. Available online: https://www.wapt.com/article/shelter-in-place-order-issued-for-mississippi-county/31991081# (accessed on 3 March 2021).
- Mississippi Economic Council. Governor Reeves Extends Shelter-in-Place by 7 Days; Enables Safe Sales by “Non-Essential” Buisinesses. Available online: https://msmec.com/governor-reeves-extends-shelter-in-place-by-7-days-enables-safe-sales-by-non-essential-businesses/ (accessed on 3 March 2021).
- WJTV. Governor Tate Reeves Signs Executive Order Closing Schools for Academic Year. Available online: https://www.wjtv.com/video/governor-tate-reeves-signs-executive-order-closing-schools-for-academic-year/5423067/ (accessed on 3 March 2021).
- Cedric Magee. MDE District Restart and Recovery Plan Summary 2020–2021. Available online: https://www.mdek12.org/sites/default/files/Offices/MDE/OCGR/restart_recovery_responses_2020.08.05_430p_20226.pdf (accessed on 3 March 2021).
- Centers for Disease Control and Prevention (CDC). Facts about Developmental Disabilities. Available online: https://www.cdc.gov/ncbddd/developmentaldisabilities/facts.html (accessed on 3 March 2021).
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Corbin, J.; Strauss, A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 4th ed.; Sage: Thousand Oaks, CA, USA, 2015. [Google Scholar] [CrossRef]
- Federal Communications Commission. 2018 Broadband Deployment Report. Available online: https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2018-broadband-deployment-report (accessed on 3 March 2021).
- US Department of Agriculture. Trump Administration Invests more than $16 Million in High-Speed Broadband in Rural Mississippi. Available online: https://www.usda.gov/media/press-releases/2020/07/14/trump-administration-invests-more-16-million-high-speed-broadband (accessed on 3 March 2021).
- The Center for Social Inclusion. Broadband in Mississippi: Toward Policies for Access Equity. Available online: https://1library.net/document/yn7okx1z-how-to-get-broadband-in-mississippi.html (accessed on 3 March 2021).
- Tohidast, S.A.; Mansuri, B.; Bagheri, R.; Azimi, H. Provision of Speech-Language Pathology Services for the Treatment of Speech and Language Disorders in Children during the COVID-19 Pandemic: Problems, Concerns, and Solutions. Int. J. Pediatr. Otorhinolaryngol. 2020, 138, 110262. [Google Scholar] [CrossRef] [PubMed]
- Tucker, J.K. Perspectives of Speech-Language Pathologists on the Use of Telepractice in Schools: The Qualitative View. Int. J. Telerehabilit. 2012, 4, 47–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurland, J.; Liu, A.; Stokes, P. Effects of a Tablet-Based Home Practice Program with Telepractice on Treatment Outcomes in Chronic Aphasia. J. Speech Lang. Hear. Res. 2018, 61, 1140–1156. [Google Scholar] [CrossRef]
- Overby, M.S.; Baft-Neff, A. Perceptions of Telepractice Pedagogy in Speech-Language Pathology: A Quantitative Analysis. J. Telemed. Telecare 2017, 23, 550–557. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Liu, M.; Li, Y.; Chung, J.E. Teens’ Social Media Engagement during the COVID-19 Pandemic: A Time Series Examination of Posting and Emotion on Reddit. Int. J. Environ. Res. Public Health 2021, 18, 10079. [Google Scholar] [CrossRef] [PubMed]
- Aishworiya, R.; Kang, Y.Q. Including Children with Developmental Disabilities in the Equation during this COVID-19 Pandemic. J. Autism Dev. Disord. 2020, 51, 2155–2158. [Google Scholar] [CrossRef]
- Zhang, S.; Wu, S.; Wu, Q.; Durkin, D.W.; Marsiglia, F.F. Adolescent Drug Use Initiation and Transition into Other Drugs: A Retrospective Longitudinal Examination across Race/Ethnicity. Addict. Behav. 2021, 113, 106679. [Google Scholar] [CrossRef]

| Characteristics | Interview Sample (n = 10) | Survey Sample (n = 51) | pb | ||||
|---|---|---|---|---|---|---|---|
| Mean/% | SD | Range | Mean/% | SD | Range | ||
| Age (year) | 37.7 | 8.2 | 26–51 | 38.8 | 11.9 | 25–67 | 0.77 |
| Gender (female) | 100% | 100% | |||||
| Race | 0.80 | ||||||
| White | 90% | 88.2% | |||||
| African American | 10% | 7.8% | |||||
| Other | 0% | 4.0% | |||||
| Work setting a | 0.19 | ||||||
| Community agency | 40% | 15.7% | |||||
| Private practice | 30% | 19.6% | |||||
| School | 20% | 56.9% | |||||
| Hospital (including outpatient) | 10% | 3.9% | |||||
| Multiple settings | 0% | 3.9% | |||||
| Years of working as SLP | 14.4 | 8.7 | 3–30 | 13.8 | 11.6 | 1–45 | 0.89 |
| Measures | Percentage | Counts of SLPs |
|---|---|---|
| Likelihood of using telepractice in the future | ||
| Very unlikely | 17.6% | 9 |
| Unlikely | 33.3% | 17 |
| Similar | 19.6% | 10 |
| More likely | 19.6% | 10 |
| Much more likely | 9.8% | 5 |
| Do you feel that clients get comparable services through telepractice as they do for in-person services? | ||
| Yes, comparable | 25.5% | 13 |
| No, telepractice will never match in-person services | 35.3% | 18 |
| No, but telepractice is a good option for some purposes | 37.3% | 19 |
| Not sure | 1.9% | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hao, Y.; Zhang, S.; Conner, A.; Lee, N.Y. The Evolution of Telepractice Use during the COVID-19 Pandemic: Perspectives of Pediatric Speech-Language Pathologists. Int. J. Environ. Res. Public Health 2021, 18, 12197. https://doi.org/10.3390/ijerph182212197
Hao Y, Zhang S, Conner A, Lee NY. The Evolution of Telepractice Use during the COVID-19 Pandemic: Perspectives of Pediatric Speech-Language Pathologists. International Journal of Environmental Research and Public Health. 2021; 18(22):12197. https://doi.org/10.3390/ijerph182212197
Chicago/Turabian StyleHao, Ying, Saijun Zhang, Austin Conner, and Na Youn Lee. 2021. "The Evolution of Telepractice Use during the COVID-19 Pandemic: Perspectives of Pediatric Speech-Language Pathologists" International Journal of Environmental Research and Public Health 18, no. 22: 12197. https://doi.org/10.3390/ijerph182212197
APA StyleHao, Y., Zhang, S., Conner, A., & Lee, N. Y. (2021). The Evolution of Telepractice Use during the COVID-19 Pandemic: Perspectives of Pediatric Speech-Language Pathologists. International Journal of Environmental Research and Public Health, 18(22), 12197. https://doi.org/10.3390/ijerph182212197







