Circumstances and Consequences of Violence-Related Injuries Presenting at Hospital. A Study at the Pediatric Emergency and Forensic Medicine Units of Maputo Central Hospital, Mozambique
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Setting
2.3. Case Definition and Data Collection
2.4. Data Treatment
2.5. Statistical Analyses
2.6. Ethical Approval
3. Results
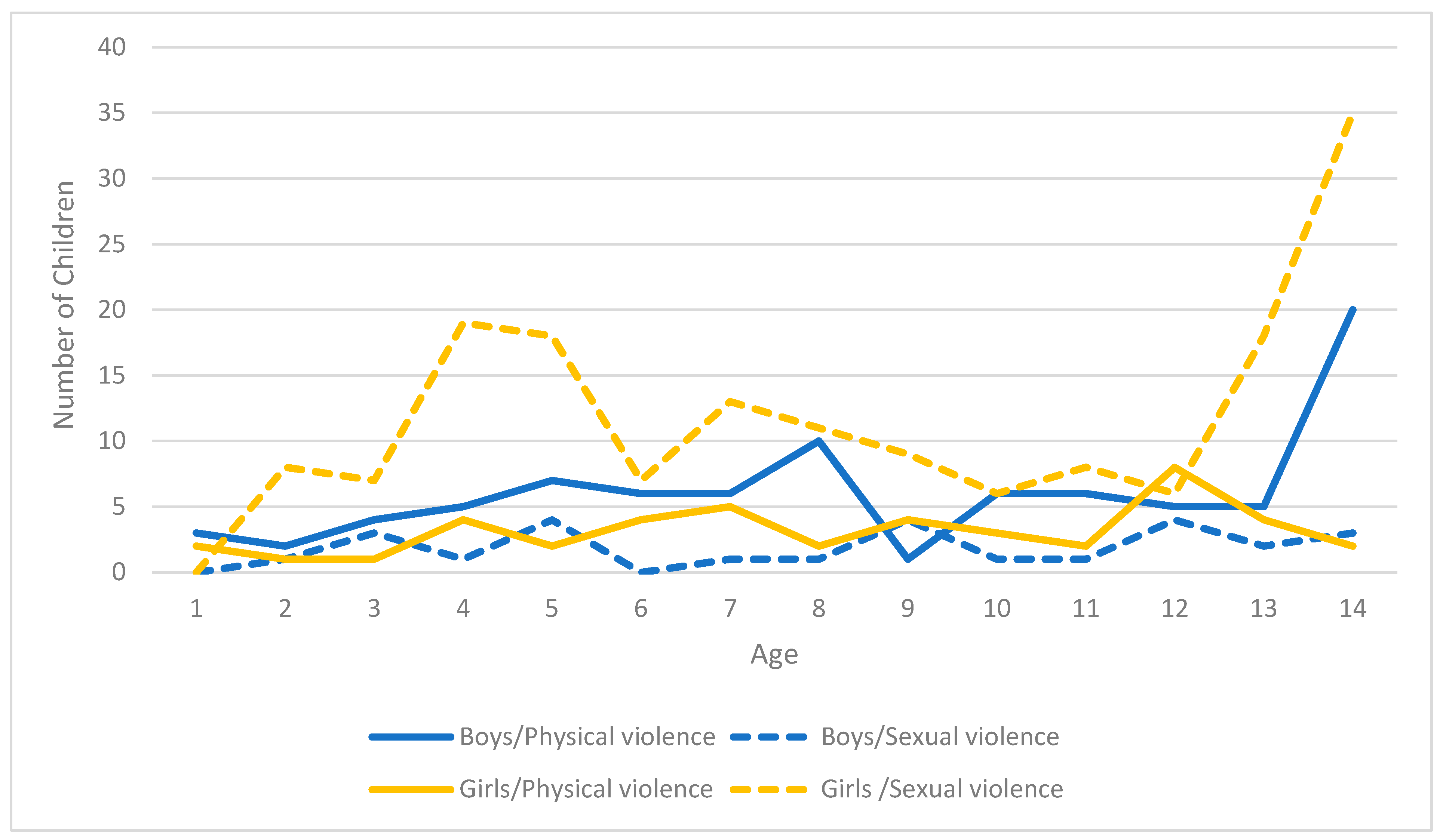
3.1. Age and Gender Distribution by Forms of Violence
3.2. Circumstances of Occurrence of the Injuries
3.3. Characteristics of the Injuries and Injury Treatment
4. Discussion
4.1. Main Findings
4.2. Comparisons with Other Studies
4.3. Strengths and Limitations
4.4. Implications of Research, Policy, and Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Violence Against Children; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/news-room/fact-sheets/detail/violence-against-children (accessed on 21 April 2020).
- Hillis, S.; Mercy, J.; Amobi, A.; Kress, H. Global Prevalence of Past-year Violence Against Children: A Systematic Review and Minimum Estimates. Pediatrics 2016, 137, e20154079. [Google Scholar] [CrossRef]
- Malta, D.C.; Bernal, R.T.I.; Teixeira, B.D.S.M.; Da Silva, M.M.A.; Freitas, M.I.D.F. Fatores associados a violências contra crianças em Serviços Sentinela de Urgência nas capitais brasileiras. Ciência Saúde Coletiva 2017, 22, 2889–2898. [Google Scholar] [CrossRef]
- Hillis, S.D.; Mercy, J.A.; Saul, J.R. The enduring impact of violence against children. Psychol. Health Med. 2016, 22, 393–405. [Google Scholar] [CrossRef]
- Zimbabwe National Statistics Agency. National Baseline Survey on Life Experiences of Adolescents Report (NBSLEA 2011); Zimbabwe National Statistics Agency: Harare, Zimbabwe, 2012. [Google Scholar]
- Moore, A.M.; Awusabo-Asare, K.; Madise, N.; John-Langba, J.; Kumi-Kyereme, A. Coerced First Sex among Adolescent Girls in Sub-Saharan Africa: Prevalence and Context. Afr. J. Reprod. Health 2007, 11, 62–82. [Google Scholar] [CrossRef]
- Instituto Nacional de Saúde (INS); Ministry of Health (MISAU); Ministry of Gender; Child and Social Action (MGCAS); Instituto Nacional de Estatística (INE); the USC for DC and P. Violence Against Children and Youth, Mozambique, 2019 (VACS 2019). Priority Indicator RePort; INS: Maputo, Mozambique, 2020.
- Lalor, K. Child sexual abuse in sub-Saharan Africa: A literature review. Child Abus. Negl. 2004, 28, 439–460. [Google Scholar] [CrossRef]
- Herrmann, B.; Navratil, F. Sexual Abuse in Prepubertal Children and Adolescents. Endocr. Dev. 2004, 7, 77–105. [Google Scholar] [CrossRef]
- Shehu, C.E.; Ekele, O.I.; Panti, A.A.; Ango, I.; Ekele, B.A.; Umar, M. The incidence, pattern and management of sexual assault in a tertiary hospital in North-western Nigeria. Int. J. Reprod. Contracept. Obstet. Gynecol. 2019, 8, 3715–3721. [Google Scholar] [CrossRef]
- Teles, N. The lack of social belonging: Reflections on violence against children in Mozambique. Aggress. Violent Behav. 2019, 46, 197–200. [Google Scholar] [CrossRef]
- van Deijk, R. Protecting Children: Comunity Attitudes to Child Sexual Abuse in Rural Mozambique; Save the Children: Maputo, Mozambique, 2007. [Google Scholar]
- Solomon, A.K. A synthesis model of community orientation toward child sexual abuse in the central region of Ghana. J. Afr. Stud. Dev. 2021, 13, 32–42. [Google Scholar] [CrossRef]
- Meursing, K.; Vos, T.; Coutinho, O.; Moyo, M.; Mpofu, S.; Oneko, O.; Mundy, V.; Dube, S.; Mahlangu, T.; Sibindi, F. Child sexual abuse in Matabeleland, Zimbabwe. Soc. Sci. Med. 1995, 41, 1693–1704. [Google Scholar] [CrossRef]
- Cox, S.; Andrade, G.; Lungelow, D.; Scholetelburg, W.; Rode, H. The child rape epidemic: Assessing the incidence at Red Cross Hospital, Cape Town, and establishing the need for a new national protocol. SAMJ 2007, 97, 992–994. Available online: https://open.uct.ac.za/handle/11427/24348 (accessed on 30 November 2020).
- Steele, S.J.; Abrahams, N.; Duncan, K.; Woollett, N.; Hwang, B.; O’Connell, L.; Van Cutsem, G.; Shroufi, A. The epidemiology of rape and sexual violence in the platinum mining district of Rustenburg, South Africa: Prevalence, and factors associated with sexual violence. PLoS ONE 2019, 14, e0216449. [Google Scholar] [CrossRef]
- WHO. World Report on Violence and Health; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Chiang, L.F.; Kress, H.; Sumner, A.S.; Gleckel, J.; Kawemama, P.; Gordon, R.N. Violence Against Children Surveys (VACS): Towards a global surveillance system. Inj. Prev. 2016, 22, i17–i22. [Google Scholar] [CrossRef]
- Javanaud, K. The consequences of violence towards children. Child Prot. Hub. 2016, 82, 1–3. Available online: https://childhub.org/sites/default/files/library/attachments/the_consequences_of_violence_28child_hub_review29.pdf (accessed on 13 April 2021).
- Reichenheim, M.E.; Hasselmann, M.H.; Moraes, C.L. Conseqüências da violência familiar na saúde da criança e do adolescente: Contribuições para a elaboração de propostas de ação. Cien. Saude. Colet. 1999, 4, 109–121. [Google Scholar] [CrossRef][Green Version]
- Burton, P.; Ward, C.L.; Artz, L.; Leoschut, L. The Optimus Study on Child Abuse, Violence and Neglect in South Africa. Optimus Study. 2016, 1, 1–32. [Google Scholar]
- Mathews, S.; Benvenuti, P. Violence against children in South Africa: Developing a prevention agenda. S. Afr. Child Gauge 2014, 2, 26–34. [Google Scholar]
- Fang, X.; Zheng, X.; Fry, D.A.; Ganz, G.; Casey, T.; Hsiao, C.; Ward, C.L. The Economic Burden of Violence against Children in South Africa. Int. J. Environ. Res. Public Health 2017, 14, 1431. [Google Scholar] [CrossRef]
- Ward, C.L.; Artz, L.; Leoschut, L.; Kassanjee, R.; Burton, P. Articles Sexual violence against children in South Africa: A nationally representative cross-sectional study of prevalence and correlates. Lancet Glob. Health 2018, 6, e460–e468. [Google Scholar] [CrossRef]
- Hsiao, C.; Fry, D.; Ward, C.L.; Ganz, G.; Casey, T.; Zheng, X.; Fang, X. Violence against children in South Africa: The cost of inaction to society and the economy. BMJ Glob. Health 2018, 3, e000573. [Google Scholar] [CrossRef] [PubMed]
- Marange, P. Cross-sectional comparisons of violence and injuries in an urban community, South Africa. Health Sci. 2017, 1–143. Available online: http://hdl.handle.net/10394/25553 (accessed on 8 November 2021).
- Jewkes, R.; Levin, J.; Mbananga, N.; Bradshaw, D. Rape of girls in South Africa. Lancet 2002, 359, 319–320. Available online: https://pubmed.ncbi.nlm.nih.gov/11830201/ (accessed on 13 April 2021). [CrossRef]
- Abrahams, N.; Mathews, S.; Lombard, C.; Martin, L.J.; Jewkes, R. Sexual homicides in South Africa: A national cross-sectional epidemiological study of adult women and children. PLoS ONE 2017, 12, e0186432. [Google Scholar] [CrossRef]
- Herbert, H.K.; van As, A.B.; Bachani, A.M.; Mtambeka, P.; Stevens, K.A.; Millar, A.J.W.; Hyder, A.A. Patterns of pediatric injury in South Africa. J. Trauma Acute Care Surg. 2012, 73, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Machisa, M.; Jina, R.; Labuschagne, G.; Vetten, L.; Loots, L.; Swemmer, S.; Meyersfeld, B.; Jewkes, R. Medico-Legal Findings from Examination of Rape Victms in South Africa Evidence and Recommendation from a Study of the Investigation, Prosecution and Adjudication of Reported Rape Cases in South Africa, 2012; SAMRC: Cape Town, South Africa, 2018. [Google Scholar]
- David, N.; Ezechi, O.; Wapmuk, A.; Gbajabiamila, T.; Ohihoin, A.; Herbertson, E.; Odeyemi, K. Child sexual abuse and disclosure in South Western Nigeria: A community based study. Afr. Health Sci. 2018, 18, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Badejoko, O.O.; Anyabolu, H.C.; Badejoko, B.O.; Ijarotimi, A.O.; Kuti, O.; Adejuyigbe, E.A. Sexual assault in Ile-Ife, Nigeria. Niger. Med. J. 2014, 55, 254–259. [Google Scholar] [CrossRef]
- Bugaje, M.; Ogunrinde, G.; Faruk, J. Child sexual abuse in Zaria, Northwestern Nigeria. Niger. J. Paediatr. 2012, 39. [Google Scholar] [CrossRef]
- Parkes, J.; Heslop, J.; Oando, S.; Sabaa, S.; Januario, F.; Figue, A. Conceptualising gender and violence in research: Insights from studies in schools and communities in Kenya, Ghana and Mozambique. Int. J. Educ. Dev. 2013, 33, 546–556. [Google Scholar] [CrossRef]
- Adeloye, D.; Bowman, K.; Chan, K.Y.; Patel, S.; Campbell, H.; Rudan, I. Global and regional child deaths due to injuries: An assessment of the evidence. J. Glob. Health 2018, 8, 1–11. [Google Scholar] [CrossRef]
- Vicente, J.G. Violação sexual de menores em Moçambique: Impunidade ou defesa de tradições? In Proceedings of the VI Congreso de La Asociación Latinoamericana de Población, Lima, Peru, 12 August 2014; pp. 1–16. [Google Scholar]
- Global Child Protection Area of Responsibility (CP AoR). Child Protection Risks and Needs in Mozambique; Child Protection: Maputo, Mozambique, 2019. [Google Scholar]
- Rock, A. National Response Efforts to Address Sexual Violence and Exploitation against Children in Mozambique: A Desktop Study; USAID’s AIDS Support and Technical Assistance Resources; Task Order: Arlington, VA, USA, 2013. [Google Scholar]
- Osório, P.C. A violência sexual e a violação de menores, uma discussão sobre os conceitos. WLSA Moçambique 2011, 1, 1–14. [Google Scholar]
- Girgira, T.; Tilahun, B.; Bacha, T. Time to presentation, pattern and immediate health effects of alleged child sexual abuse at two tertiary hospitals in Addis Ababa, Ethiopia. BMC Public Health 2014, 14, 92. [Google Scholar] [CrossRef]
- Worku, D.; Gebremariam, A.; Jayalakshmi, S. Child sexual abuse and its outcomes among high school students in southwest Ethiopia. Trop. Dr. 2006, 36, 137–140. [Google Scholar] [CrossRef]
- Save The Children (Sweden). Corporal Punishment of Children in Ethiopia; Save the Children: Addis Ababa, Ethiopia, 2011; Available online: https://resourcecentre.savethechildren.net/sites/default/files/documents/6743.pdf (accessed on 2 May 2021).
- Stavropoulos, J. Violence against Girls in Africa: A Retrospective Survey in Ethiopia, Kenya and Uganda; African Child Policy Forum: Addis Ababa, Ethiopia, 2006. [Google Scholar]
- Armstrong, A. Consent and compensation: The sexual abuse of girls in Zimbabwe. In Law, Culture, Tradition and Children’s Rights in Eastern and Southern Africa; Ncube, W., Ed.; Ashgate Dartmouth: Surrey, UK, 1998. [Google Scholar]
- Girl Child Network. Gravity of Girl Child Sexual Abuse in Zimbabwe: Towards Creating A Culture of Prevention. Unpublished work. 2004. [Google Scholar]
- Muridzo, N.G.; Malianga, E. Child sexual abuse in Zimbabwe: Prevention strategies for social workers. Afr. J. Soc. Work 2015, 5, 41–64. [Google Scholar]
- Wandera, S.O.; Clarke, K.; Knight, L.; Allen, E.; Walakira, E.; Namy, S.; Naker, D.; Devries, K. Violence against children perpetrated by peers: A cross-sectional school-based survey in Uganda. Child Abus. Negl. 2017, 68, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Burton, P. Suffering at School: Results of the Malawi Gender-Based Violence in Schools Survey; Institute of Security StudiesPretoria: Pretoria, South Africa, 2005; Available online: http://www.iss.co.za/pubs/Books/SufferingAtSchoolOct05/SufferingAtSchool.pdf (accessed on 5 May 2021).
- Lema, V.M. Sexual abuse of minors: Emerging medical and social problem in Malawi. East Afr. Med J. 1997, 74, 743–746. [Google Scholar]
- McCrann, D.; Lalor, K.; Katabaro, J.K. Childhood sexual abuse among university students in Tanzania. Child Abus. Negl. 2006, 30, 1343–1351. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Abeid, M.; Muganyizi, P.; Massawe, S.; Mpembeni, R.; Darj, E.; Axemo, P. Knowledge and attitude towards rape and child sexual abuse—A community-based cross-sectional study in Rural Tanzania. BMC Public Health 2015, 15, 1–12. [Google Scholar] [CrossRef]
- UNICEF Zambia. Rapid Assessment of the Incidence of Child Abuse in Zambia; UNICEF: Lusaka, Zambia, 2001. [Google Scholar]
- Lenane, A.M. Child Physical Abuse. Pediatric Clin. Advis. 2007, 2, 109–110. [Google Scholar] [CrossRef]
- FDC. Violencia contra menores em Moçambique—Revisão da literatura; Fundação para o Desenvolvimento da Comunidade: Maputo, Mozambique, 2008; pp. 1–72. [Google Scholar]
- ECSA-HC. Child sexual abuse in Sub-Saharan Africa: A review of the literature. Child Abus. Negl. 2004, 4, 439–460. [Google Scholar]
- INE. Resultados Definitivos Do Censo 2017: IV Recenseamento Geral Da População e Habitação; INE: Maputo, Mozambique, 2019.
- UNICEF. Situação das Crianças em Moçambique; UNICEF: Madrid, Spain, 2014; Available online: https://www.unicef.org/mozambique/media/571/file/SituaçãodasCriançasemMoçambique2014.pdf (accessed on 21 June 2020).
- MTES. Um Estudo Qualitativo Sobre o Fenomeno Do Trabalho e o Seu Impacto Em Mocambique (2014–2015); MTES: Maputo, Mozambique, 2016. [Google Scholar]
- ROSC. Necessidade de protecção especial das crianças orfas e vulneraveis em tempos de Covid-19. 2020, pp. 1–8. Available online: https://bettercarenetwork.org/sites/default/files/2021-04/POLICEBRIEF42020-7%281%29.pdf (accessed on 3 July 2021).
- Mosse, M.; Cortes, E. A Corrupção No Sector Da Saúde Em Moçambique; Centro de Integridade Pública de Moçambique: Maputo, Mozambique, 2006. [Google Scholar]
- Tsandzana, L.S. Percepções Sociais Sobre a Prática da Autópsia: Um Estudo na Medicina Legal do Hospital Central Maputo, Moçambique; Universidade Eduardo Mondlane: Maputo, Mozambique, 2013. [Google Scholar]
- WHO. Injury Surveillance Guidelines; Horder, Y., Peden, M., Krug, E., Lund, J.G., Eds.; Centers for Disease Contrl and Prevention: Geneva, Switzerland, 2001. [Google Scholar]
- Preacher, K.J. Calculation for the Chi-Square Test: An Interactive Calculation Tool for Chi-Square Tests of Goodness of Fit and Independence (Computer Software). 2001. Available online: http://quantpsy.org (accessed on 8 November 2021).
- Abo-Seria, M.; AbdelRahman, A.; Mostafa, H.; Farag, H. Study of Child Sexually Abused Cases in Cairo Governorates in the Period from (2012) to (2016). Ain Shams J. Forensic Med. Clin. Toxicol. 2019, 32, 31–39. [Google Scholar] [CrossRef]
- Haridas, S.; Nanandkar, S.D.S. Medicolegal Study of Alleged Rape Victim Cases in Mumbai Region. Int. J. Med. Toxicol. Forensic. Med. 2016, 6, 12–22. [Google Scholar] [CrossRef]
- Hyder, A.A.; Malik, F.A. Violence against Children: A Challenge for Public Health in Pakistan. J. Health Popul. Nutr. 2007, 25, 168–178. [Google Scholar] [PubMed]
- Gallaher, J.R.; Molyneux, E.; Charles, A.G. Sub-Saharan African hospitals have a unique opportunity to address intentional injury to children. Afr. J. Emerg. Med. 2016, 6, 59–60. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Badoe, E. A critical review of child abuse and its management in Africa. Afr. J. Emerg. Med. 2017, 7, S32–S35. [Google Scholar] [CrossRef] [PubMed]
- UNICEF; Campbell Collaboration. Evidence and Gap Map Research Brief. Innocent Res. Brief 2019, 14, 1–6. Available online: https://www.unicef-irc.org/publications/pdf/IRB2019-07.pdf (accessed on 30 March 2020).
- Mikton, C.; Butchart, A. Child maltreatment prevention: A systematic review of reviews. Bull World Health Organ. 2009, 87, 353–361. [Google Scholar] [CrossRef]
- WHO. Global Status Report on Violence Prevention; World Health Organization: Geneva, Switzerland, 2014; Available online: https://www.who.int/publications/i/item/9789241564793 (accessed on 5 April 2020).
- Kelly, K.; Jones, J. Forensic laboratory evidence in sexually abused children and adolescents. J. Investig. Med. 1999, 47, 585–588. Available online: https://jamanetwork.com/journals/jamapediatrics/fullarticle/205067 (accessed on 6 April 2020).
- WHO. Violence Precention: The Evidence; World Health Organization: Geneva, Switzerland, 2010; Available online: https://www.who.int/violence_injury_prevention/violence/4th_milestones_meeting/evidence_briefings_all.pdf (accessed on 6 April 2020).
- Heise, L. What works to prevent partner violence? An evidence overview. In Report for the UK Department for International Development, December; 2011; pp. 1–110. Available online: https://www.oecd.org/derec/49872444.pdf (accessed on 8 November 2021).
| Type of Violence | Pediatric Emergency n. = 143 | Forensic Medicine n. = 178 | Total n. = 321 | |||
|---|---|---|---|---|---|---|
| n. | % | n. | % | n. | % | |
| Sexual | 79 | 55.2 | 112 | 62.9 | 191 | 59.5 |
| Physical | 64 | 44.8 | 66 | 37.1 | 130 | 40.5 |
| Total | 143 | 100.0 | 178 | 100.0 | 321 | 100.0 |
| Circumstances of Occurrence | Sexual Violence n. = 191 | Physical Violence n. = 130 | ||||||
|---|---|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | p-Value | ||||
| n. = 26 | n. = 165 | % | n. = 86 | % | n. = 44 | % | ||
| Perpetrator | ||||||||
| Father | 0 | 25 | 15.1 | 23 | 26.7 | 9 | 20.4 | n.s. 1 |
| Mother | 0 | 0 | 0.0 | 14 | 16.3 | 5 | 11.5 | - |
| Other relative | 7 | 50 | 30.4 | 16 | 18.6 | 14 | 31.8 | 0.0922 |
| Person known | 12 | 48 | 29.1 | 24 | 27.9 | 14 | 31.8 | n.s. |
| Person unknown | 6 | 37 | 22.4 | 7 | 8.1 | 2 | 4.5 | 0.0004 |
| Do not know/missing | 1 | 5 | 3.0 | 2 | 2.3 | 0 | 0.0 | - |
| Number of perpetrator(s) | ||||||||
| 1 | 24 | 150 | 90.9 | 86 | 100.0 | 44 | 100.0 | n.s. |
| 2 or more | 2 | 15 | 9.1 | 0 | 0.0 | 0 | 0.0 | - |
| Place of occurrence | ||||||||
| Victim’s house | 8 | 70 | 42.4 | 52 | 60.5 | 27 | 61.4 | n.s. |
| Perpetrator’s house | 9 | 50 | 30.3 | 7 | 8.1 | 3 | 6.8 | n.s. |
| Street | 2 | 20 | 12.2 | 18 | 20.9 | 6 | 13.6 | n.s. |
| Other (e.g., public or religious environment) | 6 | 22 | 13.3 | 7 | 8.1 | 8 | 18.2 | 0.0001 |
| Do not know/missing | 1 | 3 | 1.8 | 2 | 2.4 | 0 | 0.0 | - |
| Day of week | ||||||||
| Weekday | 18 | 106 | 64.2 | 56 | 65.1 | 38 | 86.4 | 0.0115 |
| Weekend | 6 | 48 | 29.1 | 30 | 34.9 | 6 | 13.6 | 0.0115 |
| Do not know/missing | 2 | 11 | 6.7 | 0 | 0.0 | 0 | 0.0 | - |
| Time of day | ||||||||
| Morning | 0 | 20 | 12.1 | 30 | 34.9 | 17 | 38.6 | n.s. |
| Afternoon | 12 | 53 | 32.2 | 24 | 27.9 | 17 | 38.6 | n.s. |
| Evening | 13 | 85 | 51.5 | 29 | 33.7 | 10 | 22.7 | n.s. |
| Do not know/missing | 1 | 7 | 4.2 | 3 | 3.5 | 0 | 0.0 | - |
| Characteristics of Injuries | Sexual Violence n. = 191 | Physical Violence n. = 130 | ||||||
|---|---|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | p-Value | ||||
| n. = 26 | n. = 165 | % | n. = 86 | % | n. = 44 | % | ||
| Number of injuries | ||||||||
| 1 | 12 | 25 | 15.1 | 36 | 41.9 | 21 | 47.7 | n.s. 1 |
| 2 | 13 | 112 | 67.9 | 50 | 58.1 | 23 | 52.3 | n.s. |
| 3 or more | 1 | 28 | 17.0 | 0 | 0.0 | 0 | 0.0 | - |
| Nature of injury (yes) | ||||||||
| Bruises (yes) | 15 | 114 | 69.1 | 73 | 84.9 | 34 | 77.3 | n.s. |
| Hymnal rupture (yes) | 0 | 43 | 26.1 | 0 | 0.0 | 0 | 0.0 | - |
| Vaginal vulvar laceration (yes) | 0 | 40 | 24.2 | 0 | 0.0 | 0 | 0.0 | - |
| Genital hematoma (yes) | 0 | 37 | 22.4 | 0 | 0.0 | 0 | 0.0 | - |
| Anal fissure (yes) | 26 | 13 | 7.9 | 0 | 0.0 | 0 | 0.0 | - |
| Vulvar edemas (yes) | 0 | 26 | 15.8 | 0 | 0.0 | 0 | 0.0 | - |
| Fractures (yes) | 0 | 0 | 0.0 | 5 | 5.8 | 3 | 6.8 | - |
| Burns (yes) | 0 | 0 | 0.0 | 5 | 5.8 | 4 | 9.1 | - |
| Hyperemia (yes) | 0 | 0 | 0.0 | 3 | 3.5 | 3 | 6.8 | - |
| Perineal rupture | 0 | 3 | 1.8 | 0 | 0.0 | 0 | 0.0 | - |
| Part of body injured | ||||||||
| Genitals (yes) | 0 | 137 | 83.0 | 0 | 0.0 | 0 | 0.0 | - |
| Head (yes) | 2 | 5 | 3.0 | 45 | 52.3 | 24 | 54.5 | n.s. |
| Upper limbs (yes) | 2 | 6 | 3.7 | 28 | 32.6 | 19 | 43.2 | n.s. |
| Thorax and abdomen(yes) | 1 | 3 | 1.8 | 24 | 28.0 | 9 | 20.5 | n.s. |
| Lower limbs (yes) | 1 | 0 | 0.0 | 15 | 17.4 | 5 | 11.4 | n.s. |
| Anal (yes) | 26 | 14 | 8.5 | 0 | 0.0 | 0 | 0.0 | - |
| Severity | ||||||||
| Minor or superficial | 8 | 69 | 41.8 | 49 | 57.0 | 26 | 59.1 | n.s. |
| Moderate, requiring specialized care | 16 | 67 | 40.6 | 35 | 40.7 | 18 | 40.9 | n.s. |
| Severe, requiring intensive care | 2 | 29 | 17.6 | 2 | 2.3 | 0 | 0.0 | - |
| Disposition | ||||||||
| Medical consultation with immediate discharge (yes) | 29 | 127 | 78.0 | 41 | 41.9 | 32 | 68.2 | 0.005 |
| Psychological support (yes) | 17 | 76 | 46.0 | 38 | 44.2 | 20 | 45.5 | n.s. |
| Surgery(yes) | 2 | 27 | 16.3 | 0 | 0.0 | 0 | 0.0 | - |
| Hospitalization (yes) | 7 | 33 | 20.0 | 12 | 14.0 | 12 | 27.3 | n.s |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nhassengo, S.K.; Matsinhe, S.O.; Jethá, E.; Laflamme, L. Circumstances and Consequences of Violence-Related Injuries Presenting at Hospital. A Study at the Pediatric Emergency and Forensic Medicine Units of Maputo Central Hospital, Mozambique. Int. J. Environ. Res. Public Health 2021, 18, 12125. https://doi.org/10.3390/ijerph182212125
Nhassengo SK, Matsinhe SO, Jethá E, Laflamme L. Circumstances and Consequences of Violence-Related Injuries Presenting at Hospital. A Study at the Pediatric Emergency and Forensic Medicine Units of Maputo Central Hospital, Mozambique. International Journal of Environmental Research and Public Health. 2021; 18(22):12125. https://doi.org/10.3390/ijerph182212125
Chicago/Turabian StyleNhassengo, Sérgio Keita, Stela Ocuane Matsinhe, Eunice Jethá, and Lucie Laflamme. 2021. "Circumstances and Consequences of Violence-Related Injuries Presenting at Hospital. A Study at the Pediatric Emergency and Forensic Medicine Units of Maputo Central Hospital, Mozambique" International Journal of Environmental Research and Public Health 18, no. 22: 12125. https://doi.org/10.3390/ijerph182212125
APA StyleNhassengo, S. K., Matsinhe, S. O., Jethá, E., & Laflamme, L. (2021). Circumstances and Consequences of Violence-Related Injuries Presenting at Hospital. A Study at the Pediatric Emergency and Forensic Medicine Units of Maputo Central Hospital, Mozambique. International Journal of Environmental Research and Public Health, 18(22), 12125. https://doi.org/10.3390/ijerph182212125






