Frailty Related to the Exposure to Particulate Matter and Ozone: The Korean Frailty and Aging Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Frailty Measurements
2.3. Air Pollutant Variables
2.4. Other Variables
2.5. Statistical Analyses
3. Results
3.1. Air Pollutants Concentration and Meteorological Data
3.2. Demographic Characteristics of the Study Population
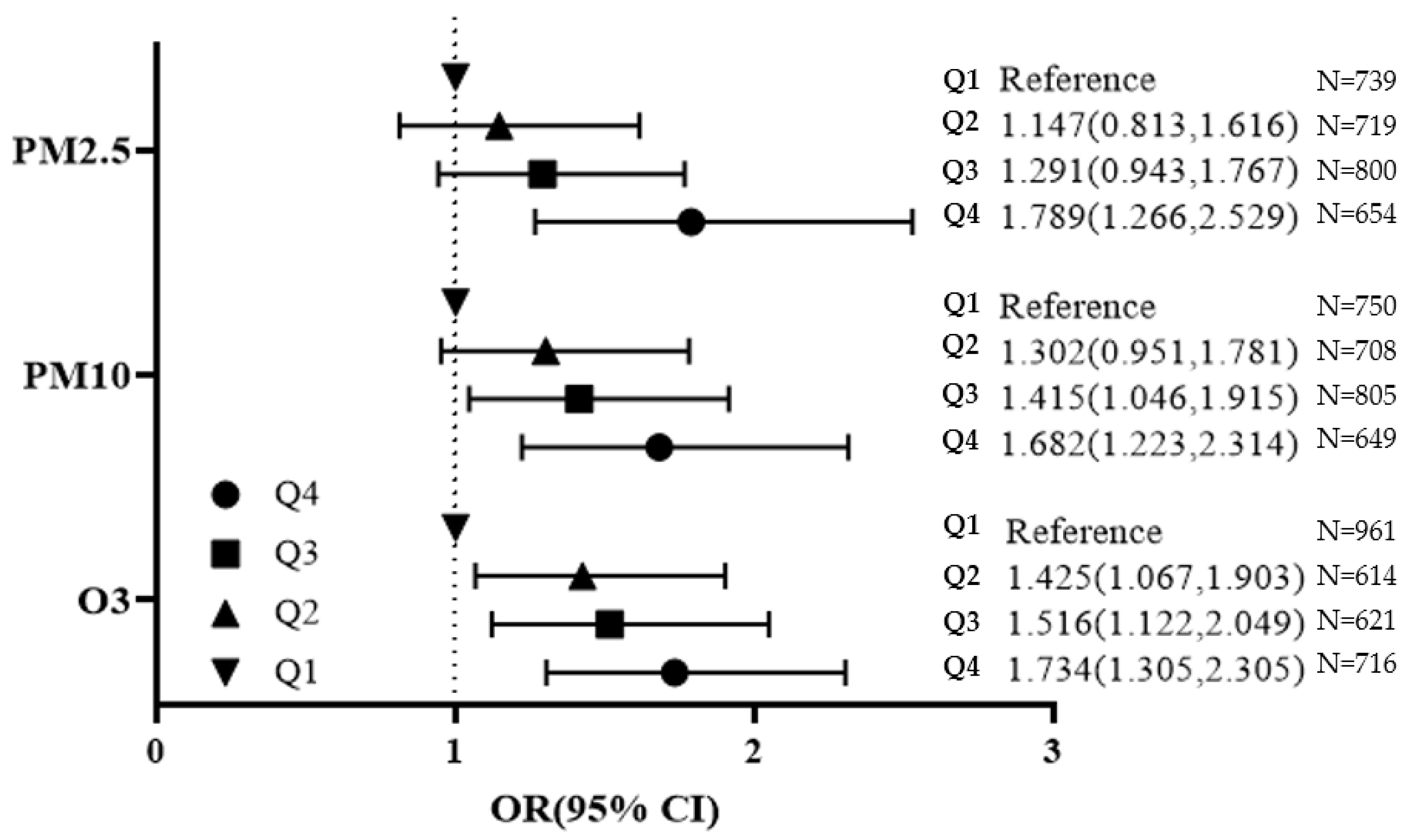
3.3. Association between Particular Matter, Ozone and Frailty
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Won, C.W.; Lee, Y.; Lee, S.; Kim, M. Development of Korean frailty index for primary care (KFI-PC) and its criterion validity. Ann. Geriatr. Med. Res. 2020, 24, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A 2001, 56, M146–M157. [Google Scholar] [CrossRef] [PubMed]
- Vermeiren, S.; Vella-Azzopardi, R.; Beckwée, D.; Habbig, A.K.; Scafoglieri, A.; Jansen, B.; Bautmans, I. Frailty and the prediction of negative health outcomes: A meta-analysis. J. Am. Med. Dir. Assoc. 2016, 17, 1163.e1–1163.e17. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Martin, F.C.; Bergman, H.; Woo, J.; Romero-Ortuno, R.; Walston, J.D. Management of frailty: Opportunities, challenges, and future directions. Lancet 2019, 394, 1376–1386. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
- Crocker, T.F.; Brown, L.; Clegg, A.; Farley, K.; Franklin, M.; Simpkins, S.; Young, J. Quality of life is substantially worse for community-dwelling older people living with frailty: Systematic review and meta-analysis. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2019, 28, 2041–2056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Air Quality Quidelines for Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide, Global Update 2005; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Wen, M.; Gu, D. Air pollution shortens life expectancy and health expectancy for older adults: The case of China. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2012, 67, 1219–1229. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; McLaughlin, S.J.; Li, L.W. Cumulative exposure to air pollution and subsequent mortality among older adults in China. J. Public Health 2019, 41, 518–526. [Google Scholar] [CrossRef]
- Song, W.M.; Liu, Y.; Liu, J.Y.; Tao, N.N.; Li, Y.F.; Liu, Y.; Wang, L.X.; Li, H.C. The burden of air pollution and weather condition on daily respiratory deaths among older adults in China, Jinan from 2011 to 2017. Medicine 2019, 98, e14694. [Google Scholar] [CrossRef]
- Liu, H.; Liu, S.; Xue, B.; Lv, Z.; Meng, Z.; Yang, X.; Xue, T.; Yu, Q.; He, K. Ground-level ozone pollution and its health impacts in China. Atmos. Environ. 2018, 173, 223–230. [Google Scholar] [CrossRef]
- Shin, J.; Park, J.Y.; Choi, J. Long-term exposure to ambient air pollutants and mental health status: A nationwide population-based cross-sectional study. PLoS ONE 2018, 13, e0195607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fougère, B.; Vellas, B.; Billet, S.; Martin, P.J.; Gallucci, M.; Cesari, M. Air pollution modifies the association between successful and pathological aging throughout the frailty condition. Ageing Res. Rev. 2015, 24, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.J.; Liu, C.Y.; Peng, L.N.; Lin, C.H.; Lin, H.P.; Chen, L.K. PM (2.5) air pollution contributes to the burden of frailty. Sci. Rep. 2020, 10, 14478. [Google Scholar] [CrossRef]
- De Zwart, F.; Brunekreef, B.; Timmermans, E.; Deeg, D.; Gehring, U. Air pollution and performance-based physical functioning in Dutch older adults. Environ. Health Perspect. 2018, 126, 017009. [Google Scholar] [CrossRef] [PubMed]
- Mitnitski, A.B.; Mogilner, A.J.; Rockwood, K. Accumulation of deficits as a proxy measure of aging. Sci. World J. 2001, 1, 323–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K.J.; Shin, J.; Choi, J. Cancer risk from exposure to particulate matter and ozone according to obesity and health-related behaviors: A nationwide population-based cross-sectional study. Cancer Epidemiol. Biomark. Prev. 2019, 28, 357–362. [Google Scholar] [CrossRef] [Green Version]
- Lakey, P.S.; Berkemeier, T.; Tong, H.; Arangio, A.M.; Lucas, K.; Pöschl, U.; Shiraiwa, M. Chemical exposure-response relationship between air pollutants and reactive oxygen species in the human respiratory tract. Sci. Rep. 2016, 6, 32916. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Lipfert, F.W. A new time-series methodology for estimating relationships between elderly frailty, remaining life expectancy, and ambient air quality. Inhal. Toxicol. 2012, 24, 89–98. [Google Scholar] [CrossRef]
- Jung, H.; Kim, M.; Lee, Y.; Won, C.W. Prevalence of Physical Frailty and Its Multidimensional Risk Factors in Korean Community-Dwelling Older Adults: Findings from Korean Frailty and Aging Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 7883. [Google Scholar] [CrossRef]
- Shin, J.; Kim, M.; Choi, J. Development and validation of a multidimensional frailty scale for clinical geriatric assessment. J. Nutr. Health Aging 2021, 25, 938–943. [Google Scholar] [CrossRef]
- Hwang, H.S.; Kwon, I.S.; Park, B.J.; Cho, B.; Yoon, J.L.; Won, C.W. The validity and reliability of Korean frailty index. J. Korean Geriatr. Soc. 2010, 14, 191–202. [Google Scholar] [CrossRef] [Green Version]
- Morley, J.E.; Malmstrom, T.K.; Miller, D.K. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J. Nutr. Health Aging 2012, 16, 601–608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.Y.; Park, J.H.; Lee, J.J.; Huh, Y.; Lee, S.B.; Han, S.K.; Choi, S.W.; Lee, D.Y.; Kim, K.W.; Woo, J.I. Standardization of the korean version of the geriatric depression scale: Reliability, validity, and factor structure. Psychiatry Investig. 2008, 5, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, B.H.; Bergen, A.E. Social support concepts and measures. J. Psychosom. Res. 2010, 69, 511–520. [Google Scholar] [CrossRef]
- Yoo, M.; Kim, S.; Kim, B.S.; Yoo, J.; Lee, S.; Jang, H.C.; Cho, B.L.; Son, S.J.; Lee, J.H.; Park, Y.S.; et al. Moderate hearing loss is related with social frailty in a community-dwelling older adults: The Korean frailty and aging cohort study (KFACS). Arch. Gerontol. Geriatr. 2019, 83, 126–130. [Google Scholar] [CrossRef]
- Mitchell, P.H.; Powell, L.; Blumenthal, J.; Norten, J.; Ironson, G.; Pitula, C.R.; Froelicher, E.S.; Czajkowski, S.; Youngblood, M.; Huber, M.; et al. A short social support measure for patients recovering from myocardial infarction: The ENRICHD social support inventory. J. Cardiopulm. Rehabil. Prev. 2003, 23, 398–403. [Google Scholar] [CrossRef]
- Kim, K.J.; Shin, J.; Choi, J.; Won, C.W. Discrepancies in the prevalence of known frailty scales: Korean frailty and aging cohort study. Ann. Geriatr. Med. Res. 2018, 22, 137–144. [Google Scholar] [CrossRef]
- Kim, C.S.D. A frailty instrument to predict disability, institutionalization, and mortality: Findings from the living profiles of older people survey. J. Korean Gerontol. Soc. 2015, 35, 451–474. [Google Scholar]
- Ensrud, K.E.; Ewing, S.K.; Taylor, B.C.; Fink, H.A.; Cawthon, P.M.; Stone, K.L.; Hillier, T.A.; Cauley, J.A.; Hochberg, M.C.; Rodondi, N.; et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch. Intern. Med. 2008, 168, 382–389. [Google Scholar] [CrossRef] [Green Version]
- Jung, H.-W.; Kim, S.; Jang, I.-Y.; Shin, D.W.; Lee, J.E.; Won, C.W. Screening value of timed up and go test for frailty and low physical performance in Korean older population: The Korean frailty and aging cohort study (KFACS). Ann. Geriatr. Med. Res. 2020, 24, 259–266. [Google Scholar] [CrossRef]
- Phu, S.; Kirk, B.; Bani Hassan, E.; Vogrin, S.; Zanker, J.; Bernardo, S.; Duque, G. The diagnostic value of the short physical performance battery for sarcopenia. BMC Geriatr. 2020, 20, 242. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.; Won, C.W. Prevalence of sarcopenia in community-dwelling older adults using the definition of the European working group on sarcopenia in older people 2: Findings from the Korean frailty and aging cohort study. Age Ageing 2019, 48, 910–916. [Google Scholar] [CrossRef] [PubMed]
- D′Hoore, W.; Sicotte, C.; Tilquin, C. Risk adjustment in outcome assessment: The Charlson comorbidity index. Methods Inf. Med. 1993, 32, 382–387. [Google Scholar]
- Myers, V.; Broday, D.M.; Steinberg, D.M.; Yuval; Drory, Y.; Gerber, Y. Exposure to particulate air pollution and long-term incidence of frailty after myocardial infarction. Ann. Epidemiol. 2013, 23, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Rückerl, R.; Hampel, R.; Breitner, S.; Cyrys, J.; Kraus, U.; Carter, J.; Dailey, L.; Devlin, R.B.; Diaz-Sanchez, D.; Koenig, W.; et al. Associations between ambient air pollution and blood markers of inflammation and coagulation/fibrinolysis in susceptible populations. Environ. Int. 2014, 70, 32–49. [Google Scholar] [CrossRef]
- Huttunen, K.; Siponen, T.; Salonen, I.; Yli-Tuomi, T.; Aurela, M.; Dufva, H.; Hillamo, R.; Linkola, E.; Pekkanen, J.; Pennanen, A.; et al. Low-level exposure to ambient particulate matter is associated with systemic inflammation in ischemic heart disease patients. Environ. Res. 2012, 116, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.; Han, S.H.; Choi, J. Exposure to ambient air pollution and cognitive impairment in community-dwelling older adults: The Korean frailty and aging cohort study. Int. J. Environ. Res. Public Health 2019, 16, 3767. [Google Scholar] [CrossRef] [Green Version]
- Fedarko, N.S. The biology of aging and frailty. Clin. Geriatr. Med. 2011, 27, 27–37. [Google Scholar] [CrossRef] [Green Version]
- Cohen, G.; Gerber, Y. Air pollution and successful aging: Recent evidence and new perspectives. Curr. Environ. Health Rep. 2017, 4, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Luger, E.; Dorner, T.E.; Haider, S.; Kapan, A.; Lackinger, C.; Schindler, K. Effects of a home-based and volunteer-administered physical training, nutritional, and social support program on malnutrition and frailty in older persons: A randomized controlled trial. J. Am. Med. Dir. Assoc. 2016, 17, 671.e9–671.e16. [Google Scholar] [CrossRef] [PubMed]
- Hart, E.A.C.; Lakerveld, J.; McKee, M.; Oppert, J.-M.; Rutter, H.; Charreire, H.; Veenhoven, R.; Bárdos, H.; Compernolle, S.; De Bourdeaudhuij, I.; et al. Contextual correlates of happiness in European adults. PLoS ONE 2018, 13, e0190387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, H.; Guo, Y.; Ruan, Z.; Kowal, P.; Di, Q.; Zheng, Y.; Xiao, J.; Hoogendijk, E.O.; Dent, E.; Vaughn, M.G.; et al. Association of indoor and outdoor air pollution with hand-grip strength among adults in six low- and middle-income countries. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2020, 75, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Roberts, N.L.; Mountjoy-Venning, W.C.; Anjomshoa, M.; Banoub, J.A.M.; Yasin, Y. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [Green Version]
- Gordon, E.H.; Peel, N.M.; Samanta, M.; Theou, O.; Howlett, S.E.; Hubbard, R.E. Sex differences in frailty: A systematic review and meta-analysis. Exp. Gerontol. 2017, 89, 30–40. [Google Scholar] [CrossRef]
- Tainio, M.; Jovanovic Andersen, Z.; Nieuwenhuijsen, M.J.; Hu, L.; de Nazelle, A.; An, R.; Garcia, L.M.T.; Goenka, S.; Zapata-Diomedi, B.; Bull, F.; et al. Air pollution, physical activity and health: A mapping review of the evidence. Environ. Int. 2021, 147, 105954. [Google Scholar] [CrossRef]
- Sun, S.; Cao, W.; Qiu, H.; Ran, J.; Lin, H.; Shen, C.; Siu-Yin Lee, R.; Tian, L. Benefits of physical activity not affected by air pollution: A prospective cohort study. Int. J. Epidemiol. 2020, 49, 142–152. [Google Scholar] [CrossRef]
- Allen, R.T.; Hales, N.M.; Baccarelli, A.; Jerrett, M.; Ezzati, M.; Dockery, D.W.; Pope, C.A., III. Countervailing effects of income, air pollution, smoking, and obesity on aging and life expectancy: Population-based study of U.S. Counties. Environ. Health 2016, 15, 86. [Google Scholar] [CrossRef] [Green Version]
- Lieb, C.M. The environmental kuznets curve and flow versus stock pollution: The neglect of future damages. Environ. Resour. Econ. 2004, 29, 483–506. [Google Scholar] [CrossRef] [Green Version]
- Sun, R.; Gu, D. Air pollution, economic development of communities, and health status among the elderly in urban China. Am. J. Epidemiol. 2008, 168, 1311–1318. [Google Scholar] [CrossRef]
- Gill, T.M.; Gahbauer, E.A.; Allore, H.G.; Han, L. Transitions between frailty states among community-living older persons. Arch. Intern. Med. 2006, 166, 418–423. [Google Scholar] [CrossRef] [PubMed]

| Variables | Mean | SD | IQR | Percentiles | ||||
|---|---|---|---|---|---|---|---|---|
| Minimum | 25th | 50th | 75th | Maximum | ||||
| Air Pollutants | ||||||||
| PM2.5, μg/m3 | 25.3 | 3.2 | 3.6 | 19.0 | 23.5 | 25.0 | 27.1 | 38.2 |
| PM10, μg/m3 | 48.0 | 4.9 | 5.4 | 36.8 | 46.7 | 48.7 | 52.1 | 66.3 |
| O3, ppb | 28.3 | 6.0 | 7.0 | 19.0 | 24.0 | 27.0 | 31.0 | 45.0 |
| Meteorological data | ||||||||
| Temperature, °C | 13.4 | 1.3 | 1.0 | 11.7 | 12.6 | 13.0 | 13.6 | 17.0 |
| Rainfall, mm | 1131.5 | 257.4 | 241.5 | 766.7 | 991.7 | 1023.4 | 1233.2 | 1734.6 |
| Humidity, % | 65.3 | 4.3 | 10.1 | 59.3 | 59.3 | 65.7 | 69.4 | 70.2 |
| Wind speed, m/s | 1.7 | 0.6 | 0.4 | 0.9 | 1.4 | 1.6 | 1.8 | 3.2 |
| Sunshine, hours | 6.4 | 0.5 | 0.5 | 5.0 | 6.2 | 6.6 | 6.7 | 6.8 |
| Variables | Robust | Pre-Frail | Frail | p-Values |
|---|---|---|---|---|
| Number, N (%) | 835 (28.7) | 1460 (50.1) | 617 (21.2) | |
| Age, years | 75.4 ± 3.7 | 76.0 ± 3.9 | 76.8 ± 3.8 | <0.001 |
| Sex | <0.001 | |||
| Male | 480 (57.5) | 679 (46.5) | 227 (36.8) | |
| Female | 355 (42.5) | 781 (53.5) | 390 (63.2) | |
| Smoking | <0.001 | |||
| Never | 453 (54.3) | 898 (61.5) | 425 (68.9) | |
| Former | 335 (40.1) | 482 (33.0) | 149 (24.1) | |
| Current | 47 (5.7) | 80 (5.5) | 43 (7.0) | |
| Alcohol intake | <0.001 | |||
| Never/Less than one time per week | 515 (61.7) | 1055 (72.3) | 478 (77.5) | |
| More than one time per week | 320 (38.3) | 405 (27.7) | 139 (22.5) | |
| Physical activity, kcal/week | <0.001 | |||
| Active | 753 (90.2) | 1190 (81.5) | 402 (65.2) | |
| Inactive | 82 (9.8) | 270 (18.5) | 215 (34.8) | |
| Education, years | <0.001 | |||
| <9 | 284 (34.0) | 696 (47.7) | 413 (66.9) | |
| ≥9 | 551 (66.0) | 764 (52.3) | 204 (33.1) | |
| Marital status | <0.001 | |||
| Married/with partner | 633 (75.8) | 974 (66.7) | 376 (60.9) | |
| Divorced/widowed/unmarried | 202 (24.2) | 486 (33.3) | 241 (39.1) | |
| Household income, won/month | <0.001 | |||
| <1,000,000 | 286 (34.3) | 644 (44.1) | 360 (58.3) | |
| ≥1,000,000 | 549 (65.7) | 816 (55.9) | 257 (41.7) | |
| Residential area | <0.001 | |||
| Urban | 263 (31.5) | 423 (29.0) | 122 (19.8) | |
| Suburban | 357 (42.8) | 600 (41.1) | 263 (42.6) | |
| Rural | 215 (25.7) | 437 (29.9) | 232 (37.6) | |
| Current employment | 0.072 | |||
| Yes | 200 (24.0) | 408 (27.9) | 152 (24.6) | |
| No | 635 (76.0) | 1052 (72.1) | 465 (75.4) | |
| Body mass index, kg/m2 | 24.5 ± 2.8 | 24.5 ± 3.0 | 24.1 ± 3.4 | 0.013 |
| Carlson’s comorbidity index | 3.17 ± 0.37 | 3.24 ± 0.43 | 3.29 ± 0.42 | <0.001 |
| Pollutants | ORs (95% CIs) | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||
| Robust vs. Frail | ||||
| PM2.5 | 1 μg/m3 | 1.055 (1.002,1.112) | 1.065 (0.974,1.165) | 0.81 (0.702,0.962) |
| PM10 | 1 μg/m3 | 1.095 (1.060,1.131) | 1.106 (1.056,1.158) | 1.188 (1.093,1.290) |
| O3 | 1 ppb | 1.041 (1.023,1.059) | 1.093 (1.031,1.160) | 1.021 (0.953,1.094) |
| PM2.5 | 1 SD | 1.326 (1.154,1.524) | 1.209 (0.923,1.583) | 0.554 (0.345,0.890) |
| PM10 | 1 SD | 1.574 (1.337,1.853) | 1.655 (1.314,2.083) | 2.364 (1.563,3.575) |
| O3 | 1 SD | 1.271 (1.146,1.410) | 1.709 (1.202,2.431) | 1.133 (0.751,1.710) |
| Robust vs. pre-frail | ||||
| PM2.5 | 1 μg/m3 | 1.053 (1.017,1.090) | 1.030 (0.970,1.094) | 0.802 (0.717,0.898) |
| PM10 | 1 μg/m3 | 1.062 (1.037,1.087) | 1.072 (1.040,1.105) | 1.168 (1.104,1.236) |
| O3 | 1 ppb | 1.005 (0.985,1.025) | 1.057 (1.015,1.101) | 0.999 (0.953,1.047) |
| PM2.5 | 1 SD | 1.167 (1.052,1.294) | 1.093 (0.912,1.310) | 0.516 (0.368,0.724) |
| PM10 | 1 SD | 1.348 (1.198,1.518) | 1.414 (1.216,1.645) | 2.175 (1.642,2.882) |
| O3 | 1 SD | 1.029 (0.912,1.161)) | 1.395 (1.093,1.781) | 0.992 (0.748,1.315) |
| Non-frail vs. frail | ||||
| PM2.5 | 1 μg/m3 | 1.051 (1.014,1.090) | 1.039 (0.968,1.116) | 0.905 (0.797,1.028) |
| PM10 | 1 μg/m3 | 1.052 (1.024,1.080) | 1.058 (1.019,1.098) | 1.098 (1.027,1.173) |
| O3 | 1 ppb | 1.024 (1.002,1.048) | 1.051 (1.001,1.102) | 1.017 (0.962,1.074) |
| PM2.5 | 1 SD | 1.162 (1.043,1.294) | 1.123 (0.908,1.388) | 0.742 (0.506,1.087) |
| PM10 | 1 SD | 1.287 (1.128,1.468) | 1.324 (1.100,1.593) | 1.593 (1.142,2.223) |
| O3 | 1 SD | 1.155 (1.010,1.322) | 1.344 (1.007,1.793) | 1.104 (0.793,1.536) |
| Pollutant | Weight Loss | Poor Health Status | Fatigue | Lack of Energy | Lower Social Network | Lower Social Support |
|---|---|---|---|---|---|---|
| PM2.5 | 0.929 (0.841,1.026) | 1.077 (1.012,1.145) | 0.998 (0.933,1.067) | 0.984 (0.927,1.044) | 1.098 (1.023,1.178) | 1.013 (0.932,1.102) |
| PM10 | 1.013 (0.966,1.063) | 1.045 (1.014,1.078) | 1.037 (1.004,1.072) | 1.037 (1.007,1.067) | 1.079 (1.041,1.119) | 1.024 (0.972,1.078) |
| O3 | 1.117 (1.034,1.205) | 0.997 (0.957,1.038) | 1.075 (1.026,1.126) | 1.064 (1.022,1.108) | 0.977 (0.928,1.028) | 0.922 (0.868,0.978) |
| Pollutant | FFP * | FI | KFI | SOF Frailty Index |
|---|---|---|---|---|
| PM2.5 | 1.544 (0.602,3.960) | 1.711 (0.671,1.359) | 0.661 (0.224,1.950) | 0.784 (0.202,3.041) |
| PM10 | 1.689 (1.066,2.676) | 1.516 (0.950,2.418) | 0.923 (0.544,1.567) | 1.253 (0.625,2.510) |
| O3 | 1.888 (0.971,3.670) | 0.969 (0.475,1.977) | 0.895 (0.436,1.836) | 4.367 (1.451,13.139) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, J.; Choi, J. Frailty Related to the Exposure to Particulate Matter and Ozone: The Korean Frailty and Aging Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 11796. https://doi.org/10.3390/ijerph182211796
Shin J, Choi J. Frailty Related to the Exposure to Particulate Matter and Ozone: The Korean Frailty and Aging Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(22):11796. https://doi.org/10.3390/ijerph182211796
Chicago/Turabian StyleShin, Jinyoung, and Jaekyung Choi. 2021. "Frailty Related to the Exposure to Particulate Matter and Ozone: The Korean Frailty and Aging Cohort Study" International Journal of Environmental Research and Public Health 18, no. 22: 11796. https://doi.org/10.3390/ijerph182211796
APA StyleShin, J., & Choi, J. (2021). Frailty Related to the Exposure to Particulate Matter and Ozone: The Korean Frailty and Aging Cohort Study. International Journal of Environmental Research and Public Health, 18(22), 11796. https://doi.org/10.3390/ijerph182211796







