A Systematic Review of a Polyvagal Perspective on Embodied Contemplative Practices as Promoters of Cardiorespiratory Coupling and Traumatic Stress Recovery for PTSD and OCD: Research Methodologies and State of the Art
Abstract
:1. Introduction
1.1. Rationale
1.2. Objectives
2. Materials and Methods
2.1. PICOS
2.2. Search Strategy
2.3. Study Design
- They were carried out on humans diagnosed with PTSD or OCD (whether they were expert or naïve about mindfulness or compassion techniques).
- Any protocol of mindfulness-related or compassion-related intervention was used.
- Mindfulness-related or compassion-related interventions compared with control groups (other interventions, no intervention) were included.
- Physiological parameters associated with the central nervous system or cardio-respiratory system (i.e., cardio-respiratory synchronization, RSA, fMRI, EEG, HRV) and measured through a behavioral/psychological variable (investigated through a psychometric quantitative tool).
- Underaged (under 18 years) and/or older (over 65 years) subjects.
- Slow breathing procedures not related to mindfulness or compassion interventions.
- Physiological parameters that were not relevant for the review, or only a behavioral/psychological index alone was investigated.
- They considered case reports.
- A lack of rigor in the description of the methodological process (e.g., age, gender, how subjects were recruited, treatments and procedures used that are clearly stated, protocol duration, measured outcomes) and of the experimental tools (e.g., tools and setups used to measure outcomes), such that replicability is difficult.
- They were not published in a peer-reviewed journal.
- They were not available in English language and/or in full-text.
3. Results
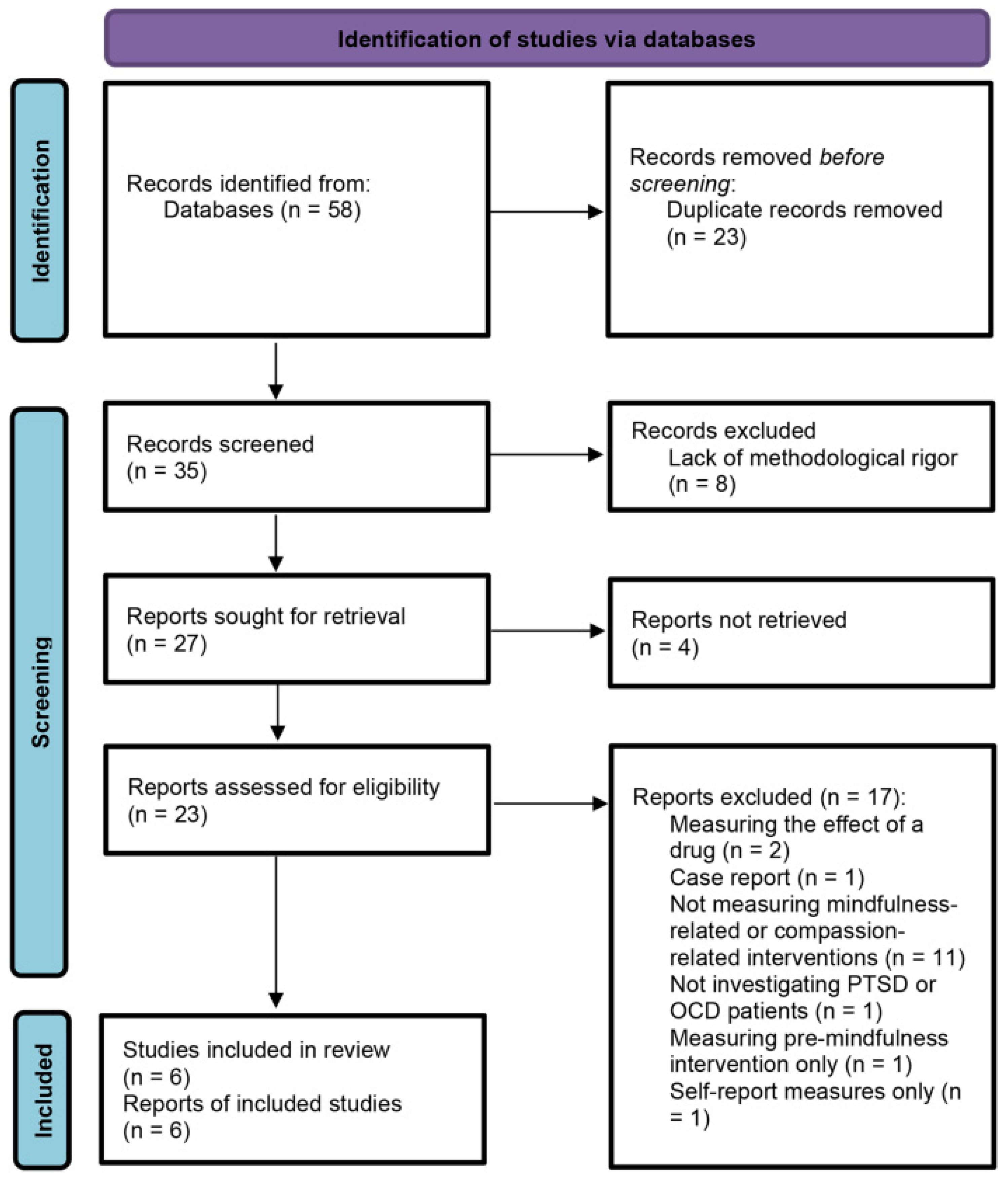
3.1. Search Results
3.2. Selection and Characteristics of the Considered Studies
3.3. Synthesized Findings
3.3.1. Cross-Sectional Studies
3.3.2. Pre-Post Studies
3.3.3. Cohort Studies
3.3.4. Randomized Controlled Trials (RCTs)
3.3.5. Risk of Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Porges, S.W. The Polyvagal Perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef] [PubMed]
- Porges, S.W. The Polyvagal Theory: New Insights into Adaptive Reactions of the Autonomic Nervous System. CCJM 2009, 76, S86–S90. [Google Scholar] [CrossRef]
- Poli, A.; Gemignani, A.; Conversano, C. The Psychological Impact of SARS-CoV-2 Quarantine: Observations through the Lens of the Polyvagal Theory. Clin. Neuropsychiatry 2020, 17, 112–114. [Google Scholar] [CrossRef]
- Kolacz, J.; Porges, S.W. Chronic Diffuse Pain and Functional Gastrointestinal Disorders After Traumatic Stress: Pathophysiology Through a Polyvagal Perspective. Front. Med. 2018, 5, 145. [Google Scholar] [CrossRef]
- Kolacz, J.; Kovacic, K.K.; Porges, S.W. Traumatic Stress and the Autonomic Brain-gut Connection in Development: Polyvagal Theory as an Integrative Framework for Psychosocial and Gastrointestinal Pathology. Dev. Psychobiol. 2019, 61, 796–809. [Google Scholar] [CrossRef] [PubMed]
- Porges, S.W. Social Engagement and Attachment. Ann. N. Y. Acad. Sci. 2003, 1008, 31–47. [Google Scholar] [CrossRef] [PubMed]
- Craig, A.D. How Do You Feel? Interoception: The Sense of the Physiological Condition of the Body. Nat. Rev. Neurosci. 2002, 3, 655–666. [Google Scholar] [CrossRef]
- Craig, A.D.B. How Do You Feel—Now? The Anterior Insula and Human Awareness. Nat. Rev. Neurosci. 2009, 10, 59–70. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Principles. Available online: https://www.who.int/about/who-we-are/constitution (accessed on 9 June 2021).
- Online Etymology Dictionary. Health. Available online: https://www.etymonline.com/word/health (accessed on 9 June 2021).
- Bruce, M.; Skrine Jeffers, K.; King Robinson, J.; Norris, K. Contemplative Practices: A Strategy to Improve Health and Reduce Disparities. IJERPH 2018, 15, 2253. [Google Scholar] [CrossRef] [Green Version]
- McCraty, R.; Zayas, M.A. Cardiac Coherence, Self-Regulation, Autonomic Stability, and Psychosocial Well-Being. Front. Psychol. 2014, 5, 1090. [Google Scholar] [CrossRef] [Green Version]
- Stellar, J.E.; Cohen, A.; Oveis, C.; Keltner, D. Affective and Physiological Responses to the Suffering of Others: Compassion and Vagal Activity. J. Pers. Soc. Psychol. 2015, 108, 572–585. [Google Scholar] [CrossRef] [Green Version]
- Zaccaro, A.; Piarulli, A.; Laurino, M.; Garbella, E.; Menicucci, D.; Neri, B.; Gemignani, A. How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing. Front. Hum. Neurosci. 2018, 12, 353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, R.P.; Gerbarg, P.L.; Muench, F. Breathing Practices for Treatment of Psychiatric and Stress-Related Medical Conditions. Psychiat. Clin. N. Am. 2013, 36, 121–140. [Google Scholar] [CrossRef] [PubMed]
- Streeter, C.C.; Gerbarg, P.L.; Saper, R.B.; Ciraulo, D.A.; Brown, R.P. Effects of Yoga on the Autonomic Nervous System, Gamma-Aminobutyric-Acid, and Allostasis in Epilepsy, Depression, and Post-Traumatic Stress Disorder. Med. Hypotheses 2012, 78, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Bruno, R.M.; Stea, F.; Sicari, R.; Ghiadoni, L.; Taddei, S.; Ungar, A.; Bonuccelli, U.; Tognoni, G.; Cintoli, S.; Del Turco, S.; et al. Vascular Function Is Improved After an Environmental Enrichment Program: The Train the Brain–Mind the Vessel Study. Hypertension 2018, 71, 1218–1225. [Google Scholar] [CrossRef]
- Boyd, J.E.; Lanius, R.A.; McKinnon, M.C. Mindfulness-Based Treatments for Posttraumatic Stress Disorder: A Review of the Treatment Literature and Neurobiological Evidence. J. Psychiatry Neurosci. 2018, 43, 7–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conversano, C.; Poli, A.; Ciacchini, R.; Hitchcott, P.; Bazzichi, L.; Gemignani, A. A Psychoeducational Intervention Is a Treatment for Fibromyalgia Syndrome. Clin. Exp. Rheumatol. 2019, 37, 98–104. [Google Scholar]
- Levine, G.N.; Lange, R.A.; Bairey-Merz, C.N.; Davidson, R.J.; Jamerson, K.; Mehta, P.K.; Michos, E.D.; Norris, K.; Ray, I.B.; Saban, K.L.; et al. Meditation and Cardiovascular Risk Reduction: A Scientific Statement from the American Heart Association. JAHA 2017, 6, e002218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abbott, R.A.; Whear, R.; Rodgers, L.R.; Bethel, A.; Thompson Coon, J.; Kuyken, W.; Stein, K.; Dickens, C. Effectiveness of Mindfulness-Based Stress Reduction and Mindfulness Based Cognitive Therapy in Vascular Disease: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. J. Psychosom. Res. 2014, 76, 341–351. [Google Scholar] [CrossRef] [Green Version]
- Anheyer, D.; Haller, H.; Barth, J.; Lauche, R.; Dobos, G.; Cramer, H. Mindfulness-Based Stress Reduction for Treating Low Back Pain: A Systematic Review and Meta-Analysis. Ann. Intern. Med. 2017, 166, 799. [Google Scholar] [CrossRef]
- Lauche, R.; Cramer, H.; Dobos, G.; Langhorst, J.; Schmidt, S. A Systematic Review and Meta-Analysis of Mindfulness-Based Stress Reduction for the Fibromyalgia Syndrome. J. Psychosom. Res. 2013, 75, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Cushing, R.E.; Braun, K.L. Mind–Body Therapy for Military Veterans with Post-Traumatic Stress Disorder: A Systematic Review. J. Altern. Complem. Med. 2018, 24, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Conversano, C.; Orrù, G.; Pozza, A.; Miccoli, M.; Ciacchini, R.; Marchi, L.; Gemignani, A. Is Mindfulness-Based Stress Reduction Effective for People with Hypertension? A Systematic Review and Meta-Analysis of 30 Years of Evidence. IJERPH 2021, 18, 2882. [Google Scholar] [CrossRef] [PubMed]
- Didonna, F.; Lanfredi, M.; Xodo, E.; Ferrari, C.; Rossi, R.; Pedrini, L. Mindfulness-Based Cognitive Therapy for Obsessive-Compulsive Disorder: A Pilot Study. J. Psychiatr. Pract. 2019, 25, 156–170. [Google Scholar] [CrossRef] [PubMed]
- Melli, G.; Poli, A.; Chiorri, C.; Olatunji, B.O. Is Heightened Disgust Propensity Truly a Risk Factor for Contamination-Related Obsessive-Compulsive Disorder? Behav. Ther. 2019, 50, 621–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melli, G.; Bulli, F.; Carraresi, C.; Tarantino, F.; Gelli, S.; Poli, A. The Differential Relationship between Mental Contamination and the Core Dimensions of Contact Contamination Fear. J. Anxiety Disord. 2017, 45, 9–16. [Google Scholar] [CrossRef]
- Melli, G.; Moulding, R.; Poli, A. Is It More Disgusting If I Think about It? Examining the Interaction of Obsessive Beliefs and Disgust Propensity in Clinical Obsessive-Compulsive Disorder. J. Obsessive-Compuls. Relat. Disord. 2016, 11, 74–81. [Google Scholar] [CrossRef]
- Poli, A.; Melli, G.; Radomsky, A.S. Different Disgust Domains Specifically Relate to Mental and Contact Contamination Fear in Obsessive-Compulsive Disorder: Evidence from a Path Analytic Model in an Italian Clinical Sample. Behav. Ther. 2019, 50, 380–394. [Google Scholar] [CrossRef]
- Poli, A.; Melli, G.; Ghisi, M.; Bottesi, G.; Sica, C. Anxiety Sensitivity and Obsessive-Compulsive Symptom Dimensions: Further Evidence of Specific Relationships in a Clinical Sample. Pers. Indiv. Differ. 2017, 109, 130–136. [Google Scholar] [CrossRef]
- Melli, G.; Carraresi, C.; Poli, A.; Marazziti, D.; Pinto, A. The Role of Guilt Sensitivity in OCD Symptom Dimensions. Clin. Psychol. Psychother. 2017, 24, 1079–1089. [Google Scholar] [CrossRef]
- Campbell, A.A.; Wisco, B.E.; Silvia, P.J.; Gay, N.G. Resting Respiratory Sinus Arrhythmia and Posttraumatic Stress Disorder: A Meta-Analysis. Biol. Psychol. 2019, 144, 125–135. [Google Scholar] [CrossRef]
- Pittig, A.; Arch, J.J.; Lam, C.W.R.; Craske, M.G. Heart Rate and Heart Rate Variability in Panic, Social Anxiety, Obsessive–Compulsive, and Generalized Anxiety Disorders at Baseline and in Response to Relaxation and Hyperventilation. Int. J. Psychophysiol. 2013, 87, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Beauchaine, T.P.; Bell, Z.E. Respiratory Sinus Arrhythmia as a Transdiagnostic Biomarker of Emotion Dysregulation. In The Oxford Handbook of Emotion Dysregulation; Beauchaine, T.P., Crowell, S.E., Eds.; Oxford University Press: New York, NY, USA, 2020; pp. 152–165. ISBN 978-0-19-068928-5. [Google Scholar]
- Conversano, C.; Ciacchini, R.; Orrù, G.; Di Giuseppe, M.; Gemignani, A.; Poli, A. Mindfulness, Compassion, and Self-Compassion Among Health Care Professionals: What’s New? A Systematic Review. Front. Psychol. 2020, 11, 1683. [Google Scholar] [CrossRef] [PubMed]
- Salzberg, S. Real Happines: The Power of Meditation; Workman: New York, NY, USA, 2011. [Google Scholar]
- Germer, C.K.; Siegel, R.D. Wisdom and Compassion in Psychotherapy. Deepening Mindfulness in Clinical Practice; Guilford Press: New York, NY, USA, 2014. [Google Scholar]
- Olendzki, A. The construction of mindfulness. In Mindfulness: Diverse Perspectives on Its Meanings, Origins and Applications; Williams, J.M.G., Kabat-Zinn, J., Eds.; Routledge: New York, NY, USA, 2013; pp. 55–70. [Google Scholar]
- Dahl, C.J.; Lutz, A.; Davidson, R.J. Reconstructing and Deconstructing the Self: Cognitive Mechanisms in Meditation Practice. Trends Cogn. Sci. 2015, 19, 515–523. [Google Scholar] [CrossRef] [Green Version]
- Gilbert, P. Compassion. Concepts, Research and Applications, 1st ed.; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Neff, K.D. The Development and Validation of a Scale to Measure Self-Compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Klimecki, O.M.; Leiberg, S.; Lamm, C.; Singer, T. Functional Neural Plasticity and Associated Changes in Positive Affect After Compassion Training. Cereb. Cortex 2013, 23, 1552–1561. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klimecki, O.M.; Leiberg, S.; Ricard, M.; Singer, T. Differential Pattern of Functional Brain Plasticity after Compassion and Empathy Training. Soc. Cogn. Affect. Neur. 2014, 9, 873–879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engen, H.G.; Singer, T. Compassion-Based Emotion Regulation Up-Regulates Experienced Positive Affect and Associated Neural Networks. Soc. Cogn. Affect. Neur. 2015, 10, 1291–1301. [Google Scholar] [CrossRef] [Green Version]
- Dykshoorn, K.L. Trauma-Related Obsessive–Compulsive Disorder: A Review. Health Psychol. Behav. Med. 2014, 2, 517–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmalzl, L.; Powers, C.; Henje Blom, E. Neurophysiological and Neurocognitive Mechanisms Underlying the Effects of Yoga-Based Practices: Towards a Comprehensive Theoretical Framework. Front. Hum. Neurosci. 2015, 9, 235. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A Critical Appraisal Tool for Systematic Reviews That Include Randomised or Non-Randomised Studies of Healthcare Interventions, or Both. BMJ Clin. Res. Ed. 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simon, D.; Adler, N.; Kaufmann, C.; Kathmann, N. Amygdala Hyperactivation during Symptom Provocation in Obsessive–Compulsive Disorder and Its Modulation by Distraction. NeuroImage Clin. 2014, 4, 549–557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, A.P.; Block, S.R.; Sripada, R.K.; Rauch, S.; Giardino, N.; Favorite, T.; Angstadt, M.; Kessler, D.; Welsh, R.; Liberzon, I. Altered Default Mode Network (DMN) Resting State Functional Connectivity Following a Mindfulness-Based Exposure Therapy for Posttraumatic Stress Disorder (PTSD) In Combat Veterans Of Afghanistan And Iraq. Depress. Anxiety 2016, 33, 289–299. [Google Scholar] [CrossRef]
- Bhatnagar, R.; Phelps, L.; Rietz, K.; Juergens, T.; Russell, D.; Miller, N.; Ahearn, E. The Effects of Mindfulness Training on Post-Traumatic Stress Disorder Symptoms and Heart Rate Variability in Combat Veterans. J. Altern. Complem. Med. 2013, 19, 860–861. [Google Scholar] [CrossRef]
- Kang, S.S.; Erbes, C.R.; Lamberty, G.J.; Thuras, P.; Sponheim, S.R.; Polusny, M.A.; Moran, A.C.; Van Voorhis, A.C.; Lim, K.O. Transcendental Meditation for Veterans with Post-Traumatic Stress Disorder. Psychol. Trauma 2018, 10, 675–680. [Google Scholar] [CrossRef]
- Wahbeh, H.; Goodrich, E.; Goy, E.; Oken, B.S. Mechanistic Pathways of Mindfulness Meditation in Combat Veterans with Posttraumatic Stress Disorder: Mechanistic Pathways of Mindfulness Meditation. J. Clin. Psychol. 2016, 72, 365–383. [Google Scholar] [CrossRef] [Green Version]
- Williams, R.M.; Ehde, D.M.; Day, M.; Turner, A.P.; Hakimian, S.; Gertz, K.; Ciol, M.; McCall, A.; Kincaid, C.; Pettet, M.W.; et al. The Chronic Pain Skills Study: Protocol for a Randomized Controlled Trial Comparing Hypnosis, Mindfulness Meditation and Pain Education in Veterans. Contemp. Clin. Trials 2020, 90, 105935. [Google Scholar] [CrossRef]
- Van Dillen, L.F.; Papies, E.K. From Distraction to Mindfulness: Psychological and Neural Mechanisms of Attention Strategies in Self-Regulation. In Handbook of Biobehavioral Approaches to Self-Regulation; Gendolla, G.H.E., Tops, M., Koole, S.L., Eds.; Springer: New York, NY, USA, 2015; pp. 141–154. ISBN 978-1-4939-1235-3. [Google Scholar]
- Boedhoe, P.S.W.; van Rooij, D.; Hoogman, M.; Twisk, J.W.R.; Schmaal, L.; Abe, Y.; Alonso, P.; Ameis, S.H.; Anikin, A.; Anticevic, A.; et al. Subcortical Brain Volume, Regional Cortical Thickness, and Cortical Surface Area Across Disorders: Findings from the ENIGMA ADHD, ASD, and OCD Working Groups. Am. J. Psychiatry 2020, 177, 834–843. [Google Scholar] [CrossRef] [PubMed]
- van den Heuvel, O.A.; Boedhoe, P.S.W.; Bertolin, S.; Bruin, W.B.; Francks, C.; Ivanov, I.; Jahanshad, N.; Kong, X.; Kwon, J.S.; O’Neill, J.; et al. An Overview of the First 5 Years of the ENIGMA Obsessive–Compulsive Disorder Working Group: The Power of Worldwide Collaboration. Hum. Brain Mapp. 2020, hbm.24972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weathers, F.W.; Ruscio, A.M.; Keane, T.M. Psychometric Properties of Nine Scoring Rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychol. Assess. 1999, 11, 124–133. [Google Scholar] [CrossRef]
- Weathers, F.W.; Keane, T.M.; Davidson, J.R.T. Clinician-Administered PTSD Scale: A Review of the First Ten Years of Research. Depress. Anxiety 2001, 13, 132–156. [Google Scholar] [CrossRef] [PubMed]
- Krystal, J.H. Adjunctive Risperidone Treatment for Antidepressant-Resistant Symptoms of Chronic Military Service–Related PTSD: A Randomized Trial. JAMA 2011, 306, 493. [Google Scholar] [CrossRef] [Green Version]
- Poli, A.; Maremmani, A.G.I.; Chiorri, C.; Mazzoni, G.-P.; Orrù, G.; Kolacz, J.; Porges, S.W.; Conversano, C.; Gemignani, A.; Miccoli, M. Item Reduction, Psychometric and Biometric Properties of the Italian Version of the Body Perception Questionnaire—Short Form (BPQ-SF): The BPQ-22. IJERPH 2021, 18, 3835. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetc, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Chapter 7: Systematic Reviews of Etiology and Risk. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020; ISBN 978-0-648-84880-6. [Google Scholar]
- Ma, L.-L.; Wang, Y.-Y.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological Quality (Risk of Bias) Assessment Tools for Primary and Secondary Medical Studies: What Are They and Which Is Better? Military Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef] [Green Version]
- Gawande, R.; To, M.N.; Pine, E.; Griswold, T.; Creedon, T.B.; Brunel, A.; Lozada, A.; Loucks, E.B.; Schuman-Olivier, Z. Mindfulness Training Enhances Self-Regulation and Facilitates Health Behavior Change for Primary Care Patients: A Randomized Controlled Trial. J Gen. Intern. Med. 2019, 34, 293–302. [Google Scholar] [CrossRef] [Green Version]
- Payne, P.; Crane-Godreau, M.A. The Preparatory Set: A Novel Approach to Understanding Stress, Trauma, and the Bodymind Therapies. Front. Hum. Neurosci. 2015, 9, 178. [Google Scholar] [CrossRef] [Green Version]
- Porges, S.W. Vagal pathways: Portals to compassion. In The Oxford Handbook of Compassion Science; Seppälä, E.M., Simon-Thomas, E., Brown, S.L., Worline, M.C., Cameron, C.D., Doty, J.R., Eds.; Oxford University Press: Oxford, UK, 2017. [Google Scholar] [CrossRef]
- Cook, D.A.; Hatala, R. Got Power? A Systematic Review of Sample Size Adequacy in Health Professions Education Research. Adv. Health Sci. Educ. 2015, 20, 73–83. [Google Scholar] [CrossRef]
- Leonard, N.R.; Jha, A.P.; Casarjian, B.; Goolsarran, M.; Garcia, C.; Cleland, C.M.; Gwadz, M.V.; Massey, Z. Mindfulness Training Improves Attentional Task Performance in Incarcerated Youth: A Group Randomized Controlled Intervention Trial. Front. Psychol. 2013, 4, 792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braboszcz, C.; Cahn, B.R.; Balakrishnan, B.; Maturi, R.K.; Grandchamp, R.; Delorme, A. Plasticity of Visual Attention in Isha Yoga Meditation Practitioners before and after a 3-Month Retreat. Front. Psychol. 2013, 4, 914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ben-Soussan, T.D.; Berkovich-Ohana, A.; Glicksohn, J.; Goldstein, A. A Suspended Act: Increased Reflectivity and Gender-Dependent Electrophysiological Change Following Quadrato Motor Training. Front. Psychol. 2014, 5, 55. [Google Scholar] [CrossRef] [Green Version]
- Tang, Y.-Y.; Hölzel, B.K.; Posner, M.I. The Neuroscience of Mindfulness Meditation. Nat. Rev. Neurosci. 2015, 16, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Josipovic, Z.; Baars, B.J. Editorial: What Can Neuroscience Learn from Contemplative Practices? Front. Psychol. 2015, 6, 1731. [Google Scholar] [CrossRef] [PubMed]
- Funder, D.C.; Ozer, D.J. Evaluating Effect Size in Psychological Research: Sense and Nonsense. Adv. Methods Pract. Psychol. Sci. 2019, 2, 156–168. [Google Scholar] [CrossRef]
- Birkhofer, A.; Schmidt, G.; Förstl, H. Herz und Hirn—Die Auswirkungen psychischer Erkrankungen und ihrer Therapie auf die Herzfrequenzvariabilität. Fortschr. Neurol. Psychiatr. 2004, 73, 192–205. [Google Scholar] [CrossRef] [PubMed]
- Bär, K.-J.; Greiner, W.; Jochum, T.; Friedrich, M.; Wagner, G.; Sauer, H. The Influence of Major Depression and Its Treatment on Heart Rate Variability and Pupillary Light Reflex Parameters. J. Affect. Disord. 2004, 82, 245–252. [Google Scholar] [CrossRef] [PubMed]
- O’Regan, C.; Kenny, R.A.; Cronin, H.; Finucane, C.; Kearney, P.M. Antidepressants Strongly Influence the Relationship between Depression and Heart Rate Variability: Findings from The Irish Longitudinal Study on Ageing (TILDA). Psychol. Med. 2015, 45, 623–636. [Google Scholar] [CrossRef] [Green Version]
- Farrokhyar, F.; Reddy, D.; Poolman, R.; Bhandari, M. Why Perform a Priori Sample Size Calculation? Can. J. Surg. 2013, 56, 207–213. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, S.A.J.; Lo, S.; Hollestein, L.M. Research Techniques Made Simple: Sample Size Estimation and Power Calculation. J. Investig. Dermatol. 2018, 138, 1678–1682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bohlmeijer, E.; Prenger, R.; Taal, E.; Cuijpers, P. The Effects of Mindfulness-Based Stress Reduction Therapy on Mental Health of Adults with a Chronic Medical Disease: A Meta-Analysis. J. Psychosom. Res. 2010, 68, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Chiesa, A.; Serretti, A. Mindfulness-Based Stress Reduction for Stress Management in Healthy People: A Review and Meta-Analysis. J. Altern. Complem. Med. 2009, 15, 593–600. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | PTSD and OCD patients. Expert or naïve for mindfulness or compassion techniques | Underaged (<18 years) and/or older (>65 years) subjects |
| Intervention | Any protocol of mindfulness-related or compassion-related intervention | Slow breathing techniques not related to mindfulness or compassion interventions |
| Comparison | Comparison of mindfulness-related or compassion-related interventions with control groups (other interventions, no intervention) | |
| Outcomes | Physiological parameters associated with cardio-respiratory system or central nervous system (i.e., EEG, fMRI, HRV, RSA, and cardio-respiratory synchronization), measured with a psychological/behavioral variable (investigated through a psychometric quantitative tool) | Physiological parameters that are not relevant for the review, or only a psychological/behavioral parameter alone has been investigated |
| Study design | Within subjects, cross sectional, RCTs, longitudinal, pre-post | A lack of rigor in the description of the methodology (e.g., age, gender, how subjects were recruited, treatments and procedures used that are clearly stated, protocol duration, measured outcomes) and of the experimental set-up (e.g., tools and setups used to measure outcomes), so that replicability is difficult. Case reports. |
| Database | Query | Research in | Items Found |
|---|---|---|---|
| PubMed |
| Title/abstract | 78,556 |
| Title/abstract | 725,931 | |
| Title/abstract | 107,609 | |
| 33 | ||
| 23 | ||
| 23 | ||
| Scopus |
| Title/abstract/Keywords | 14,203 |
| Title/Abstract/Keywords | 1,232,687 | |
| 20,114 | ||
| 42 | ||
| 37 | ||
| 35 |
| Study | Study Design | Mindfulness- or Compassion-Related Intervention Group | Control Group | Mean Age (Standard Deviation) [Control Group] | Mindfulness- or Compassion-Related Intervention | Mindfulness- or Compassion-Related Intervention Details | Comparison Intervention(s) | Comparison Intervention(s) Details |
|---|---|---|---|---|---|---|---|---|
| Simon et al., 2014 | Cross-sectional | 21 unmedicated OCD patients (13 females) | 21 healthy controls (13 females) | 33.1 (10.8) [33.1 (10.1)] | Distracting bar orientation task | Self-referential evaluation task | ||
| Bhatnagar et al., 2013 | Cohort | 8 PTSD patients (1 female) | No control group | 59.5 (range, 42–71 years) | MBSR | 8 weeks | No comparison intervention | |
| Kang et al., 2018 | Cohort | 29 PTSD patients (6 females) | No control group | 59.0 (12.8) | Transcendental Meditation (TM) | 8 weeks | No comparison intervention | |
| King et al., 2016 | Pre-Post | 14 PTSD patients (0 females) | 9 PTSD patients (0 females) | 32.43 (7.54) [31.37 (10.14)] | Mindfulness-Based Exposure Therapy (MBET) | 16 weeks | Present-Centered Group Therapy (PCGT) | 16 weeks |
| Williams et al., 2020 | RCT | 80 PTSD patients (females n° not reported) | 2 groups of 80 PTSD patients (females n° not reported) | Not reported | Mindfulness Meditation (MM) | 8 weeks | Hypnosis, Education condition | 8 weeks |
| Wahbeh et al., 2016 | RCT | 27 PTSD patients (2 females) | 3 groups of 25 PTSD patients (4 females) | 53.3 (12.6) [1. 52.2 (12.5) 2. 50.0 (12.8) 3. 53.0 (11.8)] | Mindfulness Meditation (MM) | 6 weeks | MM and Slow breathing (SB), SB, Sitting quietly (SQ) | 6 weeks |
| Study | Cardio-Respiratory System | Central Nervous System | Psychological/Behavioral Outcome | Statistical Analyses | Power Analysis |
|---|---|---|---|---|---|
| Simon et al., 2014 | Not investigated | Dampening of BOLD amygdala hyperactivity | Only OCD-related and aversive stimuli were rated less unpleasant during distraction | Repeated measures ANOVA with a Greenhouse–Geisser correction when sphericity was violated | Not reported |
| Bhatnagar et al., 2013 | Increased pNN50 measure of HRV | Not investigated | PTSD symptoms had decreased from baseline by an overall CAPS score of 14.8 points | Not reported | Not reported |
| Kang et al., 2018 | Not investigated | Increased low-frequency bands (1–7 Hz) of EEG spectral power at post-treatment and follow-up and only during meditation states | Reductions in PTSD symptoms, experiential avoidance, and depressive and somatic symptoms, as well as increases in measures of mindfulness and quality of life | Repeated measures ANOVA with a Hyunh-Feldt correction when sphericity was violated | Not reported |
| King et al., 2016 | Not investigated | Increased DMN rsFC with DLPFC and dorsal ACC regions following MBET | Reduction in PTSD symptoms; PCC-DLPFC correlated with improvement in PTSD avoidant and hyperarousal symptoms | Paired-sample t-test comparisons | Not reported |
| Williams et al., 2020 | Not investigated | EEG pre- and post- treatment (protocol only) | Mindfulness, Self-compassion, Pain catastrophizing and Pain acceptance measures (protocol only) | ANOVA (protocol only) | N = 240 to have at least 80% power, even at the largest standard deviation when using ANOVA |
| Wahbeh et al., 2016 | No change in HR and HRV within and between groups | Lower awakening cortisol within MM group | Subjective hyperarousal symptoms improvement within-group (but not between groups) for MM, MM+SB, and SQ; Intrusive thoughts decreased in MM compared with MM + SB and SB | Paired t-test; ANCOVA | N = 25 in each group, for the main effects of ANCOVA the adjusted effect size (f) is 0.46, which yields power of >0.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poli, A.; Gemignani, A.; Soldani, F.; Miccoli, M. A Systematic Review of a Polyvagal Perspective on Embodied Contemplative Practices as Promoters of Cardiorespiratory Coupling and Traumatic Stress Recovery for PTSD and OCD: Research Methodologies and State of the Art. Int. J. Environ. Res. Public Health 2021, 18, 11778. https://doi.org/10.3390/ijerph182211778
Poli A, Gemignani A, Soldani F, Miccoli M. A Systematic Review of a Polyvagal Perspective on Embodied Contemplative Practices as Promoters of Cardiorespiratory Coupling and Traumatic Stress Recovery for PTSD and OCD: Research Methodologies and State of the Art. International Journal of Environmental Research and Public Health. 2021; 18(22):11778. https://doi.org/10.3390/ijerph182211778
Chicago/Turabian StylePoli, Andrea, Angelo Gemignani, Federico Soldani, and Mario Miccoli. 2021. "A Systematic Review of a Polyvagal Perspective on Embodied Contemplative Practices as Promoters of Cardiorespiratory Coupling and Traumatic Stress Recovery for PTSD and OCD: Research Methodologies and State of the Art" International Journal of Environmental Research and Public Health 18, no. 22: 11778. https://doi.org/10.3390/ijerph182211778
APA StylePoli, A., Gemignani, A., Soldani, F., & Miccoli, M. (2021). A Systematic Review of a Polyvagal Perspective on Embodied Contemplative Practices as Promoters of Cardiorespiratory Coupling and Traumatic Stress Recovery for PTSD and OCD: Research Methodologies and State of the Art. International Journal of Environmental Research and Public Health, 18(22), 11778. https://doi.org/10.3390/ijerph182211778








