The Impact of Gastrointestinal Symptoms on Patients’ Well-Being: Best–Worst Scaling (BWS) to Prioritize Symptoms of the Gastrointestinal Symptom Score (GIS)
Abstract
1. Background
2. Objectives
3. Methods
3.1. Study Design
3.1.1. Pre-Investigation
3.1.2. Principal Investigation
3.2. Method: Best–Worst Scaling (BWS)
3.3. Decision Model
3.4. Data Collection and Recruitment
3.5. Ethical Requirements and Approval
3.6. Experimental Design
3.7. Survey Instrument
- Sociodemographic characteristics (e.g., age, gender, educational level, previous therapy and several questions concerning health status, disease and treatment experiences).
- Explanation/description of the ten gastrointestinal symptoms.
- Questions regarding the frequency of occurrence of gastrointestinal symptoms using a 5-level Likert scale.
- Assessment of the impact of gastrointestinal symptoms on well-being with BWS.
3.8. Statistical Analysis
4. Results
4.1. Study Population
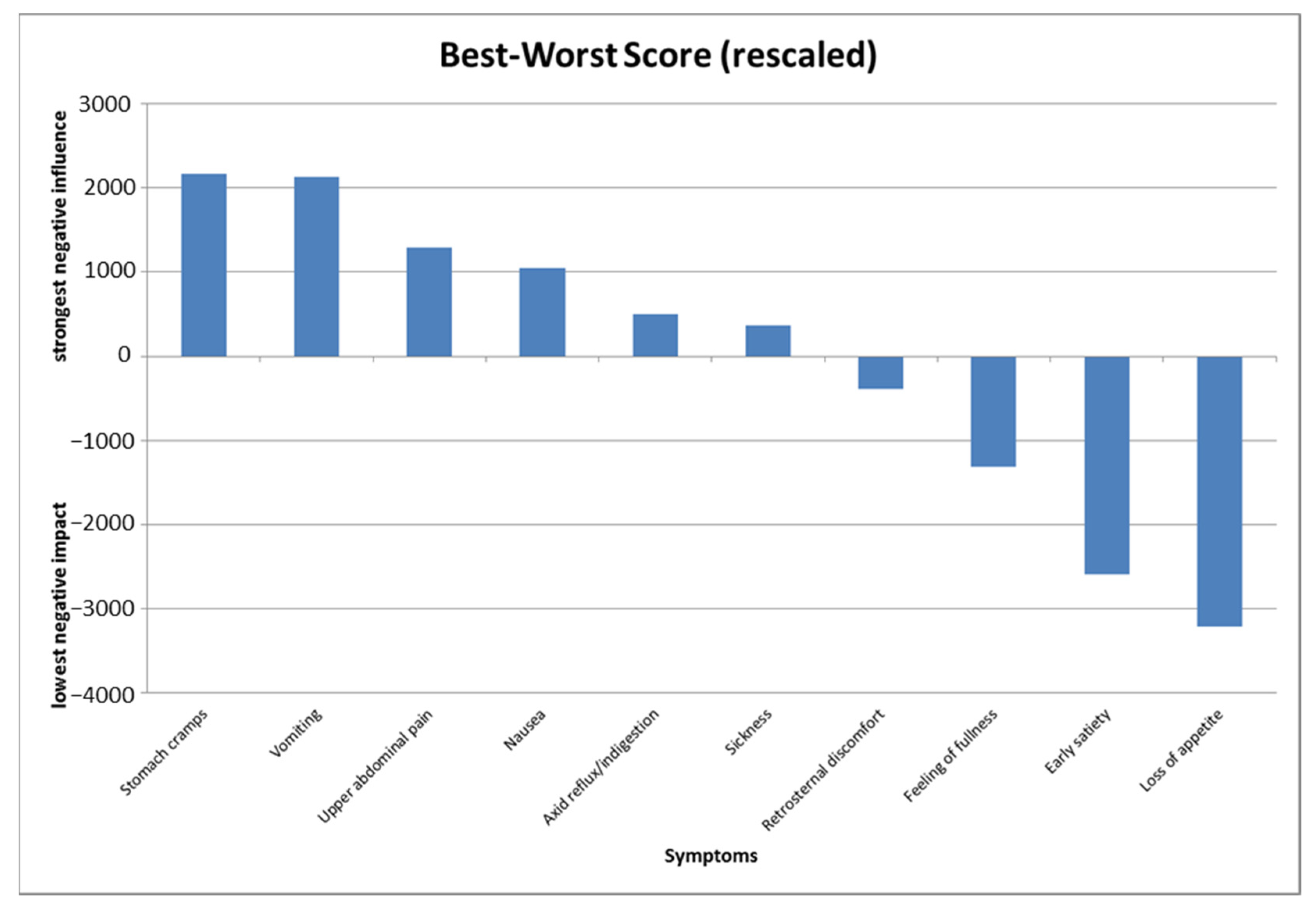
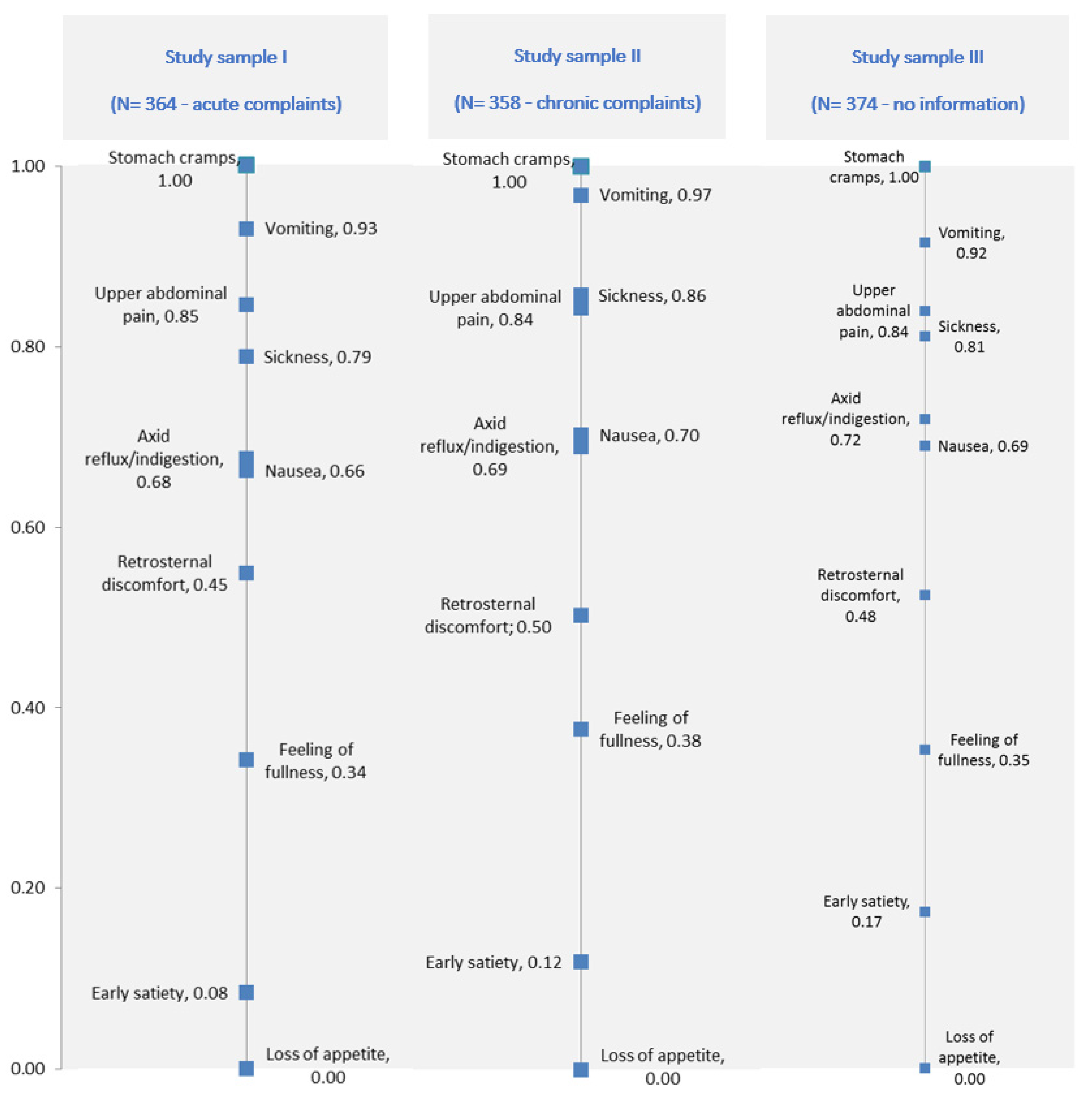
4.2. Patient Priority Data
5. Discussion
5.1. Study Importance and Implications
5.2. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

References
- Lovell, R.M.; Ford, A. Global prevalence of and risk factors for irritable bowel syndrome: A meta-analysis. Clin. Gastroenterol. Hepatol. 2012, 10, 712–721.e4. [Google Scholar] [CrossRef]
- Caballero-Plasencia, A.M.; Valenzuela-Barranco, M.; Herrerías-Gutiérrez, J.M.; Esteban-Carretero, J.M. Altered gastric emptying in patients with irritable bowel syndrome. Eur. J. Nucl. Med. Mol. Imaging 1999, 26, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Olden, K. Are psychological factors of aetiological importance in functional dyspepsia? Bailieres Clin. Gastroenterol. 1998, 12, 557–571. [Google Scholar] [CrossRef]
- Tougas, G.; Chen, Y.; Hwang, P.; Liu, M.M.; Eggleston, A. Prevalence and impact of upper gastrointestinal symptoms in the Canadian population: Findings from the DIGEST study. Am. J. Gastroenterol. 1999, 94, 2845–2854. [Google Scholar] [CrossRef] [PubMed]
- Wells, N.E.J.; Hahn, B.A.; Whorwell, P. Clinical economics review: Irritable bowel syndrome. Aliment. Pharmacol. Ther. 1997, 11, 1019–1030. [Google Scholar] [CrossRef] [PubMed]
- Talley, N.; Verlinden, M.; Jones, M. Quality of life in functional dyspepsia: Responsiveness of the Nepean Dyspepsia Index and development of a new 10-item short form. Aliment. Pharmacol. Ther. 2001, 15, 207–216. [Google Scholar] [CrossRef]
- El-Serag, H.B.; Talley, N.J. Health-related quality of life in functional dyspepsia. Aliment. Pharmacol. Ther. 2003, 18, 387–393. [Google Scholar] [CrossRef]
- Monés, J.; Adan, A.; Segú, J.L.; López, J.S.; Artés, M.; Guerrero, T. Quality of life in functional dyspepsia. Dig. Dis. Sci. 2002, 47, 20–26. [Google Scholar] [CrossRef]
- Kulich, K.R.; Madisch, A.; Pacini, F.; Piqué, J.M.; Regula, J.; Van Rensburg, C.J.; Újszászy, L.; Carlsson, J.; Halling, K.; Wiklund, I.K. Reliability and validity of the gastrointestinal symptom rating scale (GSRS) and quality of life in reflux and dyspepsia (QOLRAD) questionnaire in dyspepsia: A six-country study. Health Qual. Life Outcomes 2008, 6, 12. [Google Scholar] [CrossRef]
- Ottillinger, B.; Storr, M.; Malfertheiner, P.; Allescher, H.-D. STW 5 (Iberogast®)—A safe and effective standard in the treatment of functional gastrointestinal disorders. Wien. Med. Wochenschr. 2013, 163, 65–72. [Google Scholar] [CrossRef]
- Adam, B.; Liebregts, T.; Saadat-Gilani, K.; Vinson, B.; Holtmann, G. Validation of the gastrointestinal symptom score for the assessment of symptoms in patients with functional dyspepsia. Aliment. Pharmacol. Ther. 2005, 22, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Melzer, J.; Rösch, W.; Reichling, J.; Brignoli, R.; Saller, R. Meta-analysis: Phytotherapy of functional dyspepsia with the herbal drug preparation STW 5 (Iberogast). Aliment. Pharmacol. Ther. 2004, 20, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Madisch, A.; Holtmann, G.; Mayr, G.; Vinson, B.; Hotz, J. Treatment of functional dyspepsia with a herbal preparation. Digestion 2004, 69, 45–52. [Google Scholar] [CrossRef]
- Mühlbacher, A.C.; Kaczynski, A. The expert perspective in treatment of functional gastrointestinal conditions: A multi-criteria decision analysis using AHP and BWS. J. Multi-Criteria Decis. Anal. 2016, 23, 112–125. [Google Scholar] [CrossRef]
- Mühlbacher, A.C.; Kaczynski, A. Expert perspective on the treatment of functional dyspepsia and motility disorders: A multi-criteria decision analysis using the analytic hierarchy process (Ahp). Value Health 2015, 18, A698. [Google Scholar] [CrossRef][Green Version]
- Flynn, T.N. Valuing citizen and patient preferences in health: Recent developments in three types of best–worst scaling. Expert Rev. Pharm. Outcomes Res. 2010, 10, 259–267. [Google Scholar] [CrossRef]
- Marti, J. A best–worst scaling survey of adolescents’ level of concern for health and non-health consequences of smoking. Soc. Sci. Med. 2012, 75, 87–97. [Google Scholar] [CrossRef]
- Marley, A.A.J. The Best-Worst Method for the Study of Preferences: Theory and Application. Ph.D. Thesis, Department of Psychology, University of Victoria, Victoria, BC, Canada, 2009. [Google Scholar]
- Thurstone, L.L. A law of comparative judgment. Psychol. Rev. 1927, 34, 273–286. [Google Scholar] [CrossRef]
- Lancsar, E.; Louviere, J. Estimating Individual Level Discrete Choice Models and Welfare Measures Using Best-Worst Choice Experiments and Sequential Best-Worst MNL; University of Technology, Centre for the Study of Choice (Censoc): Sydney, Australia, 2008; pp. 1–24. [Google Scholar]
- Louviere, J.J.; Flynn, T.N. Using best-worst scaling choice experiments to measure public perceptions and preferences for healthcare reform in Australia. Patient Patient-Cent. Outcomes Res. 2010, 3, 275–283. [Google Scholar] [CrossRef]
- Marley, A.; Flynn, T.N.; Louviere, J. Probabilistic models of set-dependent and attribute-level best–worst choice. J. Math. Psychol. 2008, 52, 281–296. [Google Scholar] [CrossRef]
- Mühlbacher, A.C.; Kaczynski, A.; Zweifel, P.; Johnson, F.R. Experimental measurement of preferences in health and healthcare using best-worst scaling: An overview. Health Econ. Rev. 2015, 6, 1–14. [Google Scholar] [CrossRef]
- Johnson, R.M.; Orme, B.K. How Many Questions Should You Ask in Choice-Based Conjoint Studies; Research Paper Series; Sawtooth Software: Beaver Creek, CO, USA, 1996. [Google Scholar]
- Smith, N.F.; Street, D.J. The use of balanced incomplete block designs in designing randomized response surveys. Aust. New Zealand J. Stat. 2003, 45, 181–194. [Google Scholar] [CrossRef]
- Cochran, W.G.; Cox, G.M. Experimental Design; Wiley Classics Library: New York, NY, USA, 1992. [Google Scholar]
- Marley, A.; Louviere, J. Some probabilistic models of best, worst, and best–worst choices. J. Math. Psychol. 2005, 49, 464–480. [Google Scholar] [CrossRef]
- Holtmann, G.; Vinson, B.R.; Braun-Lang, U.; Grote, E.; Gerken, G. Validierung eines gastrointestinalen Symptomscores (GIS) zur standardisierten Erfassung dyspeptischer Beschwerden bei Patienten mit funktioneller Dyspepsie. Z. Für Gastroenterol. 2004, 42, P003. [Google Scholar] [CrossRef]
- Braden, B.; Caspary, W.; Börner, N.; Vinson, B.; Schneider, A.R.J. Clinical effects of STW 5 (Iberogast) are not based on acceleration of gastric emptying in patients with functional dyspepsia and gastroparesis. Neurogastroenterol. Motil. 2009, 21, 632–638.e25. [Google Scholar] [CrossRef]
- Madisch, A.; Holtmann, G.; Plein, K.; Hotz, J. Treatment of irritable bowel syndrome with herbal preparations: Results of a double-blind, randomized, placebo-controlled, multi-centre trial. Aliment. Pharmacol. Ther. 2004, 19, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Raedsch, R.H.J.; Bock, P.; Vinson, B.; Gundermann, K.-J. Wirksamkeit und Unbedenklichkeit des Phytopharmakons STW 5 versus Metoclopramid bei funktioneller Dyspepsie unter Praxisbedingungen. Eine retrolektive Kohortenstudie. Gastroenterology 2007, 45, 1041–1048. [Google Scholar] [CrossRef]
- Rösch, W.; Vinson, B.; Sassin, I. A randomised clinical trial comparing the efficacy of a herbal preparation STW 5 with the prokinetic drug cisapride in patients with dysmotility type of functional dyspepsia. Z. Für Gastroenterol. 2002, 40, 401–408. [Google Scholar] [CrossRef]
- Von Arnim, U.; Peitz, U.; Vinson, B.; Gundermann, K.J.; Malfertheiner, P. STW 5, a phytopharmacon for patients with functional dyspepsia: Results of a multicenter, place-bo-controlled double-blind study. Am. J. Gastroenterol. 2007, 102, 1268–1275. [Google Scholar] [CrossRef] [PubMed]
- Helm, R.; Steiner, M. Präferenzmessung: Methodengestützte Entwicklung Zielgruppenspezifischer Produktinnovationen; Kohlhammer Verlag: Stuttgart, Germany, 2008. [Google Scholar]
- Louviere, J.J.; Islam, T.; Wasi, N.; Street, D.; Burgess, L. Designing discrete choice experiments: Do optimal designs come at a price? J. Consum. Res. 2008, 35, 360–375. [Google Scholar] [CrossRef]
- Blinman, P.; Alam, M.; Duric, V.; McLachlan, S.-A.; Stockler, M.R. Patients’ preferences for chemotherapy in non-small-cell lung cancer: A systematic review. Lung Cancer 2010, 69, 141–147. [Google Scholar] [CrossRef] [PubMed]
| Symptom | Explanation |
|---|---|
| Nausea | Mood disorder that is also known as a “queasy” feeling in the stomach area and is accompanied by the urge to vomit. |
| Vomiting | Surge-like emptying of stomach contents through the mouth. |
| Sickness | Feeling of having to vomit and the immediate predecessor of vomiting. |
| Feeling of fullness | Bloated feeling, the supersaturation or overload of the stomach. |
| Abdominal cramps | Strong, colicky abdominal cramps, that decrease and increase repeatedly in their strength. |
| Early Satiety | Early onset feeling of overfilling the stomach. The saturation occurs immediately after ingestion. |
| Acid Reflux/Indigestion | From epigastric rising burning and painful sensation that can radiate to the neck and throat, often in connection with acidic or bitter regurgitation. |
| Loss of Appetite | Missing or limited need for food intake. |
| Retrosternal Discomfort | Unpleasant, painful or dragging sensation behind the breastbone. |
| Upper Abdominal pain | Pain that occurs between the costal arch, i.e., in the upper abdomen. |
| Characteristics | Absolute Number (%) |
|---|---|
| Gender | |
| Male | 596 (54.4) |
| Female | 500 (45.6) |
| Age | |
| 20–29 years | 109 (9.9) |
| 30–39 years | 264 (24.1) |
| 40–49 years | 322 (29.4) |
| 50–59 years | 266 (24.4) |
| >60 years | 135 (12.4) |
| Mean/SD | 45.3/11.7 |
| Material Status | |
| Married | 679 (62.0) |
| Widowed | 26 (2.4) |
| Divorced or separated | 103 (9.4) |
| Single | 155 (14.1) |
| In a relationship, but not married | 133 (12.1) |
| Others | 0 (0.0) |
| Employment Status | |
| Employed full-time | 818 (74.6) |
| Employed part-time | 114 (10.4) |
| Self-employed | 29 (2.6) |
| Homemaker | 36 (3.3) |
| Student | 32 (2.9) |
| Retired | 51 (4.7) |
| Disabled/Unable to work | 8 (0.7) |
| Unemployed but looking for work | 7 (0.6) |
| Unemployed and not looking for work | 1 (0.1) |
| Body Heights (cm) | |
| Mean/SD | 174/75 |
| Weight (kg) | |
| Mean/SD | 77/24 |
| General State of Health | |
| Very good | 29 (2.6) |
| Good | 443 (40.4) |
| Satisfactory | 419 (38.2) |
| Not very good | 168 (15.3) |
| Bad | 37 (3.4) |
| Frequency of Occurrence | Never | Rarely (1 Time per Month or Less) | Occasionally (More Than 1 Time per Month) | Often (Several Times per Week) | Always (Every Day) | |
|---|---|---|---|---|---|---|
| Symptom | ||||||
| Nausea | 227 (20.7%) | 403 (38.8%) | 354 (32.3%) | 108 (9.9%) | 4 (0.4%) | |
| Vomiting | 527 (48.1%) | 355 (32.4%) | 198 (18.1%) | 16 (1.5%) | 0 (0%) | |
| Sickness | 456 (41.6%) | 369 (33.7%) | 217 (19.8%) | 54 (4.9%) | 0 (0%) | |
| Feeling of Fullness | 170 (15.5%) | 212 (19.3%) | 382 (34.8%) | 296 (27.0%) | 36 (3.3%) | |
| Stomach Cramps | 147 (13.4%) | 287 (26.2%) | 399 (36.4%) | 251 (22.9%) | 12 (1.1%) | |
| Early Satiety | 211 (19.2%) | 267 (24.4%) | 424 (38.7%) | 164 (15.0%) | 30 (2.7%) | |
| Acid Reflux/Indigestion | 227 (20.7%) | 224 (20.4%) | 375 (34.2%) | 242 (22.1%) | 28 (2.6%) | |
| Loss of Appetite | 239 (21.8%) | 379 (34.6%) | 328 (29.9%) | 137 (12.5%) | 13 (1.2%) | |
| Retrosternal Discomfort | 361 (32.9%) | 359 (32.8%) | 289 (26.4%) | 84 (7.7%) | 3 (0.3%) | |
| Upper Abdominal Pain | 115 (10.5%) | 272 (24.8%) | 400 (36.5%) | 283 (25.8%) | 26 (2.4%) | |
| Attribute | Best Counts | Worst Counts | B–W Score | B–W Score Rescaled | Average B–W Score | Sqrt (B + 0.1/W + 0.1) | Sqrt (B + 0.1/W + 0.1) Rescaled |
|---|---|---|---|---|---|---|---|
| Sickness | 537 | 897 | −360 | 360 | −0.08 | −0.26 | 0.68 |
| Vomiting | 285 | 2418 | −2133 | 2133 | −0.49 | −1.07 | 0.94 |
| Nausea | 356 | 1404 | −1048 | 1048 | −0.24 | −0.69 | 0.82 |
| Feeling of Fullness | 1642 | 331 | 1311 | −1311 | 0.30 | 0.80 | 0.36 |
| Stomach Cramps | 185 | 2359 | −2174 | 2174 | −0.50 | −1.27 | 1.00 |
| Early Satiety | 2723 | 126 | 2597 | −2597 | 0.59 | 1.54 | 0.13 |
| Acid Reflux/Indigestion | 636 | 1140 | −504 | 504 | −0.11 | −0.29 | 0.70 |
| Loss of Appetite | 3279 | 66 | 3213 | −3213 | 0.73 | 1.95 | 0.00 |
| Retrosternal Discomfort | 961 | 577 | 384 | −384 | 0.09 | 0.26 | 0.53 |
| Upper Abdominal pain | 356 | 1642 | −1286 | 1286 | −0.29 | −0.76 | 0.84 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mühlbacher, A.C.; Kaczynski, A. The Impact of Gastrointestinal Symptoms on Patients’ Well-Being: Best–Worst Scaling (BWS) to Prioritize Symptoms of the Gastrointestinal Symptom Score (GIS). Int. J. Environ. Res. Public Health 2021, 18, 11715. https://doi.org/10.3390/ijerph182111715
Mühlbacher AC, Kaczynski A. The Impact of Gastrointestinal Symptoms on Patients’ Well-Being: Best–Worst Scaling (BWS) to Prioritize Symptoms of the Gastrointestinal Symptom Score (GIS). International Journal of Environmental Research and Public Health. 2021; 18(21):11715. https://doi.org/10.3390/ijerph182111715
Chicago/Turabian StyleMühlbacher, Axel Christian, and Anika Kaczynski. 2021. "The Impact of Gastrointestinal Symptoms on Patients’ Well-Being: Best–Worst Scaling (BWS) to Prioritize Symptoms of the Gastrointestinal Symptom Score (GIS)" International Journal of Environmental Research and Public Health 18, no. 21: 11715. https://doi.org/10.3390/ijerph182111715
APA StyleMühlbacher, A. C., & Kaczynski, A. (2021). The Impact of Gastrointestinal Symptoms on Patients’ Well-Being: Best–Worst Scaling (BWS) to Prioritize Symptoms of the Gastrointestinal Symptom Score (GIS). International Journal of Environmental Research and Public Health, 18(21), 11715. https://doi.org/10.3390/ijerph182111715





