Patient Satisfaction Determinants of Inpatient Healthcare
Abstract
1. Introduction
2. Background of the Study
3. Materials and Methods
3.1. Data Collection and Questionnaire
3.2. Methods
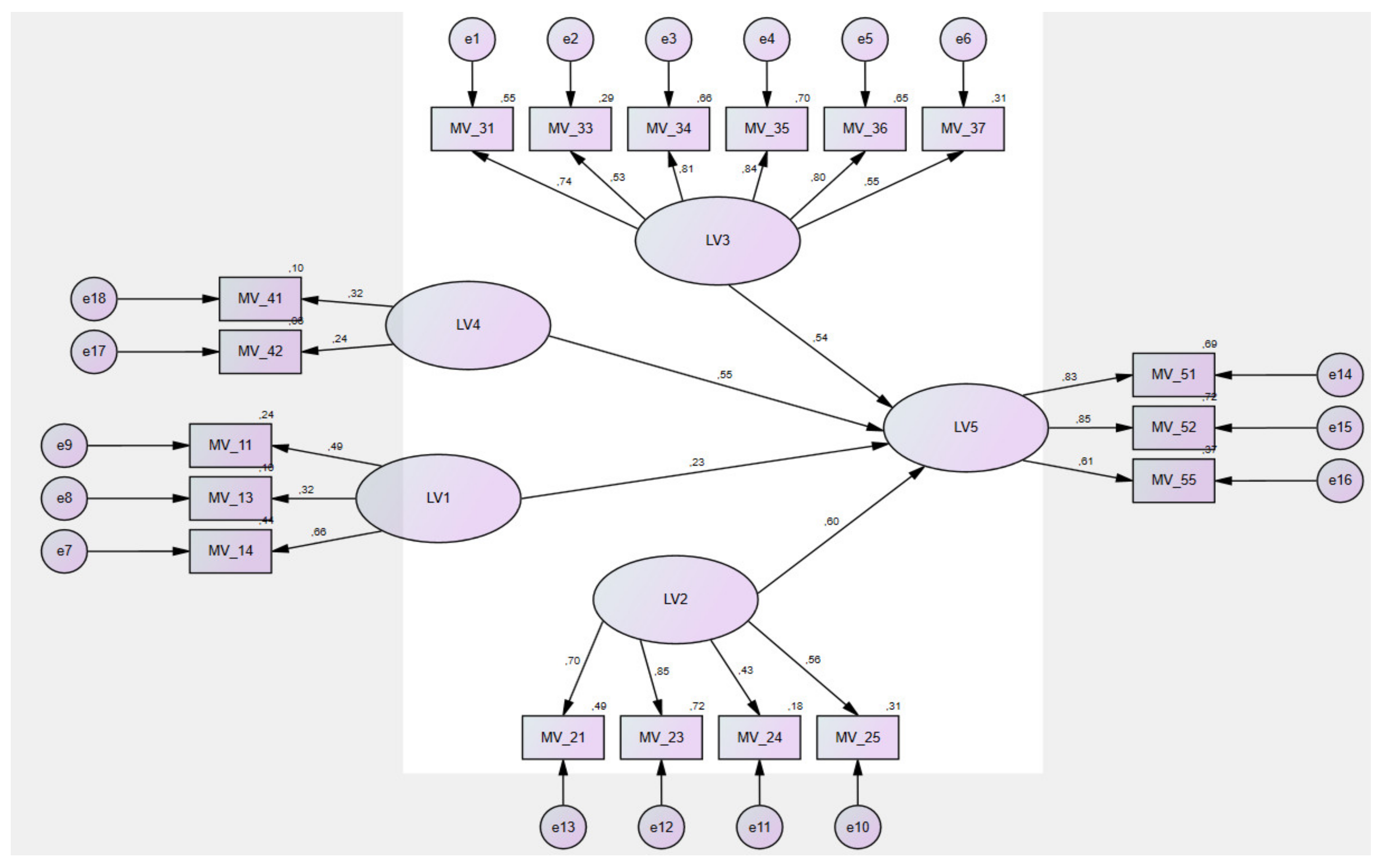
3.3. Variables
- -
- Satisfaction with hospital, department, room and board (LV1): MV_11—waiting time for room allocation from the moment the patient came to the hospital (type of answer (TA): ten-point scale (from I waited very long—0 to I did not wait at all—10); MV_12—patient harassment due to night noise of other patients (TA: yes—0; no—1); MV_13—patient harassment due to night noise of medical staff (TA: yes—0; no—1); MV_14—cleanliness of the hospital room and ward (TA: ten-point scale from not clean at all—0 to very clean—10); MV_15—choice of meal in the hospital (TA: no—0; yes, sometimes—1; yes, always—2).
- -
- Satisfaction with medical staff (nurses, doctor’s expertise, nurses and other staff) (LV2): MV_21—assessment of trust in the attending physician (TA: ten-point scale from worst trust—0 to best trust—10); MV_22—communication of the physician in front of the patient as if the patient was not present there (TA: yes—0; no—1); MV_23—assessment of trust in the nurse (TA: ten-point scale from worst trust—0 to best trust—10); MV_24—communication of medical staff in front of the patient as if the patient was not present there (TA: yes—0; no—1); MV_25—sufficient number of nurses who cared for patients (ten-point scale since there was never a nurse—0 after the maximum number of nurses was always—10); MV_26—awareness of the exchange of work shifts of nurses taking care of the patient’s healthcare (TA: no—0; sometimes—1; yes—2).
- -
- Satisfaction with the quality of the treatment provided (LV3): MV_31—evaluation of collaboration between the members of the nursing staff (TA: ten-point scale from no cooperation—0 to the best cooperation—10); MV_32—difference in the provision of information to the patient by the medical staff for the same thing (TA: ten-point scale from it regularly happened to me—0 to never happened to me—10); MV_33—involvement of the patient in the decision making process about their treatment to the extent that the patient would require (TA: ten-point scale from no involvement—0 to the highest involvement—10); MV_34—patient confidence in the decisions about health or treatment (TA: ten-point scale from no trust—0 to the greatest trust—10); MV_35—evaluation of the availability of information about the patient’s health condition or treatment (ten-point scale from I did not receive any information—0 to I received sufficient information—10); MV_36—assessment of the comprehensibility of information about the patient’s health condition or treatment from medical staff (ten-point scale from were not at all comprehensible—0 to were completely comprehensible—10); MV_37—evaluation of sufficient privacy when communicating about the health condition or treatment of the patient (ten-point scale from I had no privacy—0 to I always had sufficient privacy—10).
- -
- Satisfaction with release from the hospital (LV4): MV_41—satisfaction with informing the patient about the date of hospital release (TA: ten-point scale I was not satisfied at all—0 after I was very satisfied—10); MV_42—patient release delay on the day when they should have been released for any reason (TA: yes—0; no—1); MV_43—written information to the patient about what the patient should/should not do after their release from the hospital (TA: no—0; yes—1).
- -
- Satisfaction with inpatient care (LV5): MV_51—overall feeling of the patient that he was treated in the hospital with respect and dignity (TA: ten-point scale from I had a bad feeling—0 to I had a great feeling—10); MV_52—evaluation of the overall care in the hospital (TA: ten-point scale from the care was at an unsatisfactory level—0 to the care was at an excellent level—10); MV_53—patient request to evaluate the quality of the patient’s treatment during the hospital stay (TA: no—0; yes—1); MV_54—informing the patient by the hospital about how to proceed in a case of a complaint about the healthcare quality (TA: no—0; yes—1); MV_55—evaluation of healthcare by the other hospital staff (e.g., cleaners, concierge, kitchen staff and so on) (TA: ten-point scale from I had a bad feeling—0 to I had a great feeling—10). Selected factor, as is satisfaction with the hospital, department, room and board (LV1; hypothesis (H)–(H1); satisfaction with medical staff (LV2; H2); satisfaction with the quality of the treatment provided (LV3; H3) and satisfaction with release from the hospital (LV4; H4) has a statistically significant effect on satisfaction with inpatient care (LV5).
4. Research Results
4.1. Reliability and Validity Analysis
4.2. Kaiser–Meyer–Olkin (KMO) and Bartlett’s Analyses
4.3. Total Variance Explained—TVE
4.4. Structural Equation Modelling—SEM
4.5. Hypothesised Direct Relationship
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledegments
Conflicts of Interest
References
- Jennings, B.M.; Heiner, S.L.; Loan, L.A.; Hemman, E.A.; Swanson, K.M. What Really Matters to Healthcare Consumers. JONA J. Nurs. Adm. 2005, 35, 173–180. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Verulava, T.; Sibashvili, N. Accessibility to psychiatric services in georgia. Afr. J. Psychiatry 2015, 18, 1–5. [Google Scholar]
- Verulava, T.; Jincharadze, N.; Jorbenadze, R. Role of primary health care in re-hospitalization of patients with heart failure. Georgian Med. News 2017, 264, 135–139. [Google Scholar]
- Gavurova, B.; Rigelsky, M.; Ivankova, V. Perceived health status and economic growth in terms of gender-oriented inequalities in the OECD countries. Econ. Sociol. 2020, 13, 245–257. [Google Scholar] [CrossRef]
- Ucieklak-Jeż, P.; Bem, A. Does “Rural” Always Mean the Same? Macrosocial Determinants of Rural Populations’ Health in Poland. Int. J. Environ. Res. Public Health 2020, 17, 397. [Google Scholar] [CrossRef]
- Bem, A.; Siedlecki, R.; Prędkiewicz, P.; Gazzola, P.; Ryszawska, B.; Ucieklak-Jeż, P. Hospitals’ Financial Health in Rural and Urban Areas in Poland: Does It Ensure Sustainability? Sustainability 2019, 11, 1932. [Google Scholar] [CrossRef]
- Preędkiewicz, P.; Bem, A.; Ucieklak-Jezż, P.; Siedlecki, R. Public or Private? Which Source of Financing Helps to Achieve Higher Health System Efficiency? In Contemporary Trends and Challenges in Finance; Jajuga, K., Locarek Junge, H., Orlowski, L.T., Staehr, K., Eds.; Springer: Cham, Switzerland, 2019; pp. 191–199. [Google Scholar] [CrossRef]
- Lieskovska, V.; Megyesiova, S.; Petrovcikova, K. Marketing as a tool of health care support. In Proceedings of the 12th International Scientific Conference on Reproduction of Human Capital—Mutual Links and Connections (RELIK), Prague, Czech Republic, 7–8 November 2019; pp. 302–312. [Google Scholar]
- Megyesiova, S.; Lieskovska, V. Analysis of the Sustainable Development Indicators in the OECD Countries. Sustainability 2018, 10, 4554. [Google Scholar] [CrossRef]
- Megyesiova, S.; Lieskovska, V. Premature Mortality for Chronic Diseases in the EU Member States. Int. J. Environ. Res. Public Health 2019, 16, 4021. [Google Scholar] [CrossRef]
- Gavurova, B.; Kovac, V.; Khouri, S. Purpose of patient satisfaction for efficient management of healthcare provision. Pol. J. Manag. Stud. 2020, 22, 134–146. [Google Scholar] [CrossRef]
- Riklikiene, O.; Didenko, O.; Ciutiene, R.; Daunoriene, A.; Ciarniene, R. Balancing nurses’ workload: A case study with nurse anaesthetists and intensive care nurses. Econ. Sociol. 2020, 13, 11–25. [Google Scholar] [CrossRef]
- Jakubowska, A.; Bilan, S.; Werbiński, J. Chronic diseases and labour resources: “Old and new” European Union member states. J. Int. Stud. 2021, 14, 129–138. [Google Scholar] [CrossRef]
- Sopko, J.; Kočišová, K. Key Indicators and Determinants in the Context of the Financial Aspects of Health Systems in Selected Countries. Adiktologie 2019, 19, 189–202. [Google Scholar]
- Briestenský, R.; Ključnikov, A. Identification of the Key Factors for Successful Hospital Management in Slovakia. Adiktologie 2019, 19, 203–211. [Google Scholar]
- Farzianpour, F.; Byravan, R.; Amirian, S. Evaluation of Patient Satisfaction and Factors Affecting It: A Review of the Literature. Health 2015, 07, 1460–1465. [Google Scholar] [CrossRef][Green Version]
- Santuzzi, N.R.; Brodnik, M.S.; Rinehart-Thompson, L.; Klatt, M. Patient Satisfaction: How Do Qualita-tive Com-ments Relate to Quantitative Scores on a Satisfaction Survey? Qual. Manag. Health Care 2009, 18, 3–18. [Google Scholar] [CrossRef]
- Yin, T.; Yin, D.-L.; Xiao, F.; Xin, Q.-Q.; Li, R.-L.; Zheng, X.-G.; Yang, H.-M.; Wang, L.-H.; Ding, X.-Y.; Chen, B.-W. Socioeconomic status moderates the association between patient satisfaction with community health service and self-management behaviors in patients with type 2 diabetes. Medicine 2019, 98, e15849. [Google Scholar] [CrossRef]
- Hu, L.; Ding, H.; Liu, S.; Wang, Z.; Hu, G.; Liu, Y. Influence of patient and hospital characteristics on inpatient satisfaction in China's tertiary hospitals: A cross-sectional study. Health Expect. 2019, 23, 115–124. [Google Scholar] [CrossRef]
- Chumbler, N.R.; Otani, K.; Desai, S.P.; Herrmann, P.A.; Kurz, R.S. Hospitalized Older Adults’ Patient Satisfaction: Inpatient care experiences. SAGE Open 2016, 6. [Google Scholar] [CrossRef]
- Carr, A.B.; Nicolau, D.P. The challenges of patient satisfaction: Influencing factors and the patient—Provider relationship in the United States. Expert Rev. Anti-Infect. Ther. 2017, 15, 955–962. [Google Scholar] [CrossRef]
- Hamka, S.W. Effect of Service Quality and Customer Satisfaction Patients in General Hospitals of Makassar City Region. J. Phy. 2018, 1028, 12107. [Google Scholar] [CrossRef]
- Mitropoulos, P.; Vasileiou, K.; Mitropoulos, I. Understanding quality and satisfaction in public hospital services: A nationwide inpatient survey in Greece. J. Retail. Consum. Serv. 2018, 40, 270–275. [Google Scholar] [CrossRef]
- Eisfeld, H.; Bauer, F.; Dubois, C.; Schmidt, T.; Kastrati, K.; Hochhaus, A.; Hübner, J. Importance of and Satisfaction with Information about Their Disease in Cancer Patients. J. Cancer Educ. 2019, 35, 403–411. [Google Scholar] [CrossRef]
- Gonzalez-Zacarias, A.A.; Mavarez-Martinez, A.; Arias-Morales, C.E.; Stoicea, N.; Rogers, B. Impact of Demographic, Socioeconomic, and Psychological Factors on Glycemic Self-Management in Adults with Type 2 Diabetes Mellitus. Front. Public Health 2016, 4, 195. [Google Scholar] [CrossRef]
- Su, R.; Cai, L.; Cui, W.; He, J.; You, D.; Golden, A. Multilevel Analysis of Socioeconomic Determinants on Diabetes Prevalence, Awareness, Treatment and Self-Management in Ethnic Minorities of Yunnan Province, China. Int. J. Environ. Res. Public Health 2016, 13, 751. [Google Scholar] [CrossRef]
- Tates, K.; Antheunis, M.L.; Kanters, S.; Nieboer, T.E.; Gerritse, M.B. The Effect of Screen-to-Screen Versus Face-to-Face Consultation on Doctor-Patient Communication: An Experimental Study with Simulated Patients. J. Med Internet Res. 2017, 19, e421. [Google Scholar] [CrossRef]
- Bjertnaes, O.A.; Sjetne, I.S.; Iversen, H.H. Overall patient satisfaction with hospitals: Effects of patient-reported experiences and fulfilment of expectations. BMJ Qual. Saf. 2011, 21, 39–46. [Google Scholar] [CrossRef]
- Marimon, F.; Gil-Doménech, D.; Bastida, R. Fulfilment of expectations mediating quality and satisfaction: The case of hospital service. Total. Qual. Manag. Bus. Excel. 2017, 30, 201–220. [Google Scholar] [CrossRef]
- Chakraborty, S.; Church, E.M. Patient hospital experience and satisfaction on social media. Int. J. Qual. Serv. Sci. 2021, 13, 417–432. [Google Scholar] [CrossRef]
- Chakraborty, S.; Church, E.M. Social media hospital ratings and HCAHPS survey scores. J. Health Organ. Manag. 2020, 34, 162–172. [Google Scholar] [CrossRef]
- Alkazemi, M.F.; Bayramzadeh, S.; Alkhubaizi, N.B.; Alayoub, A. The physical environment and patient satisfaction ratings on social media: An exploratory study. Facilities 2019, 38, 86–97. [Google Scholar] [CrossRef]
- Geletta, S. Measuring patient satisfaction with medical services using social media generated data. Int. J. Health Care Qual. Assur. 2018, 31, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Rai, T.S. Social media use and mental health. Science 2019, 364, 1147.3–1148. [Google Scholar] [CrossRef]
- Rastegar-Mojarad, M.; Ye, Z.; Wall, D.; Murali, N.; Lin, S. Collecting and Analyzing Patient Experiences of Health Care from Social Media. JMIR Res. Protoc. 2015, 4, e78. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Hu, L.; Guo, R.; Wang, H.; Cao, M.; Chen, X.; Liu, Y. The Influence of Patient and Hospital Characteristics on Inpatient Satisfaction at Beijing District-Level Hospitals. Patient Prefer. Adherence 2021, 15, 1451–1460. [Google Scholar] [CrossRef]
- Kraska, R.A.; Weigand, M.; Geraedts, M. Associations between hospital characteristics and patient satisfaction in Germany. Health Expect. 2016, 20, 593–600. [Google Scholar] [CrossRef]
- Mann, R.K.; Siddiqui, Z.; Kurbanova, N.; Qayyum, R. Effect of HCAHPS reporting on patient satisfaction with physician communication. J. Hosp. Med. 2015, 11, 105–110. [Google Scholar] [CrossRef]
- Davidson, K.; Shaffer, J.A.; Ye, S.; Falzon, L.; Emeruwa, I.O.; Sundquist, K.; Inneh, I.A.; Mascitelli, S.L.; Manzano, W.M.; Vawdrey, D.K.; et al. Interventions to improve hospital patient satisfaction with healthcare providers and systems: A systematic review. BMJ Qual. Saf. 2016, 26, 596–606. [Google Scholar] [CrossRef]
- Weidmer, B.A.; Brach, C.; Slaughter, M.E.; Hays, R.D. Development of Items to Assess Patients’ Health Literacy Experiences at Hospitals for the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Hospital Survey. Med. Care 2012, 50, S12–S21. [Google Scholar] [CrossRef]
- Brega, A.G.; Hamer, M.K.; Albright, K.; Brach, C.; Saliba, D.; Abbey, D.; Gritz, R.M. Organizational Health Literacy: Quality Improvement Measures with Expert Consensus. Health Lit. Res. Pract. 2019, 3, e127–e146. [Google Scholar] [CrossRef]
- Bremer, D.; Klockmann, I.; Jaß, L.; Härter, M.; von dem Knesebeck, O.; Lüdecke, D. Which criteria characterize a health literate health care organization?—A scoping review on organizational health literacy. BMC Health Serv. Res. 2021, 21, 1–14. [Google Scholar] [CrossRef]
- Siddiqui, Z.K.; Wu, A.W.; Kurbanova, N.; Qayyum, R. Comparison of Hospital Consumer Assessment of Healthcare Providers and Systems patient satisfaction scores for specialty hospitals and general medical hospitals: Confounding effect of survey response rate. J. Hosp. Med. 2014, 9, 590–593. [Google Scholar] [CrossRef]
- Jöreskog, K.G. A general method for estimating a linear structural equation system. ETS Res. Bull. Ser. 1970, 1970, i-41. [Google Scholar] [CrossRef]
- Fan, X.; Thompson, B.; Wang, L. Effects of sample size, estimation methods, and model specification on structural equation modeling fit indexes. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 56–83. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural equation modelling: Guidelines for determining model fit. Electronic J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar]
- Kaiser, H.F. An index of factorial simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling With AMOS, EQS, and LISREL: Comparative Approaches to Testing for the Factorial Validity of a Measuring Instrument. Int. J. Test. 2001, 1, 55–86. [Google Scholar] [CrossRef]
- Hair, J.F.; Hauff, S.; Hult, G.T.M.; Richter, N.F.; Ringle, C.M.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling; Sage: Thousand Oaks, CA, USA. [CrossRef]
- Lu, J.; Ren, L.; Zhang, C.; Wang, C.; Ahmed, R.R.; Streimikis, J. Corporate social responsibility and employee behavior: Evidence from mediation and moderation analysis. Corp. Soc. Responsib. Environ. Manag. 2020, 27, 1719–1728. [Google Scholar] [CrossRef]
- Martínez-López, F.J.; Gázquez-Abad, J.C.; Sousa, C.M.P. Structural equation modelling in marketing and business research: Critical issues and practical recommendations. Eur. J. Mark. 2013, 47, 115–152. [Google Scholar] [CrossRef]
- Shah, R.; Goldstein, S.M. Use of structural equation modeling in operations management research: Looking back and forward. J. Oper. Manag. 2005, 24, 148–169. [Google Scholar] [CrossRef]
- Olsson, U.H.; Foss, T.; Troye, S.V.; Howell, R.D. The Performance of ML, GLS, and WLS Estimation in Structural Equation Modeling Under Conditions of Misspecification and Nonnormality. Struct. Equ. Model. A Multidiscip. J. 2000, 7, 557–595. [Google Scholar] [CrossRef]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef]
- Ahmed, R.R.; Hussain, S.; Pahi, M.H.; Usas, A.; Jasinskas, E. Social Media Handling and Extended Technology Acceptance Model (ETAM): Evidence from SEM-based Multivariate Approach. Transform. Bus. Econ. 2019, 18, 246–271. [Google Scholar]
- Zhang, L.; Chen, H.; Li, M.; Wang, J.; Xue, C.; Ding, T.; Liu, Y.; Nong, X. Factors influencing inpatients’ satisfaction with hospitalization service in public hospitals in Shanghai, People’s Republic of China. Patient Prefer. Adherence 2016, 10, 469–477. [Google Scholar] [CrossRef]
- Newell, S.; Jordan, Z. The patient experience of patient-centered communication with nurses in the hospital setting: A qualitative systematic review protocol. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 76–87. [Google Scholar] [CrossRef]
- Nguyen, J.; Hunter, J.; Smith, L.; Harnett, J.E. Can We All Speak the Same ‘Language’ for Our Patients’ Sake? Feedback on Interprofessional Communication and Related Resources. Glob. Adv. Health Med. 2021, 10, 2164956121992338. [Google Scholar] [CrossRef]
- Ismail, F.; Perlis, U.M.; Omar, B.; Malaysia, U.S. Kesan Gaya Komunikasi Doktor Perubatan Terhadap Kepuasan Pesakit (The Effects of Physician Communication Style on Patient Satisfaction). J. Komunikasi Malays. J. Commun. 2018, 34, 73–95. [Google Scholar] [CrossRef]
- Brédart, A.; Bouleuc, C.; Dolbeault, S. Doctor-patient communication and satisfaction with care in oncology. Curr. Opin. Oncol. 2005, 17, 351–354. [Google Scholar] [CrossRef]
- Lau, F.L. Can communication skills workshops for emergency department doctors improve patient satisfaction? J. Accid. Emerg. Med. 2000, 17, 251–253. [Google Scholar] [CrossRef] [PubMed]
- Grayson-Sneed, K.A.; Dwamena, F.C.; Smith, S.; Laird-Fick, H.S.; Freilich, L.; Smith, R.C. A questionnaire identifying four key components of patient satisfaction with physician communication. Patient Educ. Couns. 2016, 99, 1054–1061. [Google Scholar] [CrossRef] [PubMed]
- Artati, R.D.; Pasinringi, S.A.; Jafar, N. The Effect of Doctors-Patients' Verbal and Non verbal Communication on Patients' Satisfaction in Outpatient Installation of Mother and Child Centre RS Dr. Wahidin Sudirohusodo Makassar. In Proceedings of the International Conference on Healthcare Service Management (ICHSM), Tsukuba, Japan, 8–10 June 2018. [Google Scholar] [CrossRef]
- Naoum, S. Doctor-Patient Communication: Benefits, problems and strategies for improvement. Sci. Chron. 2018, 23, 265–275. [Google Scholar]
- Wei, D.; Xu, A.; Wu, X. The mediating effect of trust on the relationship between doctor–patient communication and patients’ risk perception during treatment. PsyCh J. 2019, 9, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Boquiren, V.M.; Hack, T.F.; Beaver, K.; Williamson, S. What do measures of patient satisfaction with the doctor tell us? Patient Educ. Couns. 2015, 98, 1465–1473. [Google Scholar] [CrossRef]
- Yang, S.C.; Zwar, N.; Vagholkar, S.; Dennis, S.; Redmond, H. Factors influencing general practice follow-up attendances of patients with complex medical problems after hospitalization. Fam. Pract. 2009, 27, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Willems, J.; Ingerfurth, S. The quality perception gap between employees and patients in hospitals. Health Care Manag. Rev. 2018, 43, 157–167. [Google Scholar] [CrossRef]
- Hellesø, R.; Lorensen, M.; Sorensen, L.; Norman, L.; Bang, K. Management of information between two nursing contexts. Stud. Health Technol. Inform. 2006, 122, 600–604. [Google Scholar]
- Semyonov-Tal, K. Complaints and Satisfaction of Patients in Psychiatric Hospitals: The Case of Israel. J. Patient Exp. 2021, 8, 2374373521997221. [Google Scholar] [CrossRef]
- Mainous, A.G.; Diaz, V.A.; Everett, C.J.; Knoll, M.E. Impact of Insurance and Hospital Ownership on Hospital Length of Stay Among Patients With Ambulatory Care-Sensitive Conditions. Ann. Fam. Med. 2011, 9, 489–495. [Google Scholar] [CrossRef]
- Andemeskel, Y.M.; Elsholz, T.; Gebreyohannes, G.; Tesfamariam, E.H. Patient satisfaction with peri-operative anesthesia care and associated factors at two National Referral Hospitals: A cross sectional study in Eritrea. BMC Health Serv. Res. 2019, 19, 669. [Google Scholar] [CrossRef]
- Showers, N.; Simon, E.P.; Blumenfeld, S.; Holden, G. Predictors of Patient and Proxy Satisfaction with Discharge Plans. Soc. Work. Health Care 1995, 22, 19–35. [Google Scholar] [CrossRef]
- Perry, L.; Middleton, S. An investigation of family carers' needs following stroke survivors' discharge from acute hospital care in Australia. Disabil. Rehabil. 2011, 33, 1890–1900. [Google Scholar] [CrossRef]
- Brühwiler, L.D.; Beeler, P.E.; Böni, F.; Giger, R.; Wiedemeier, P.G.; Hersberger, K.E.; Lutters, M. A RCT evaluating a pragmatic in-hospital service to increase the quality of discharge prescriptions. Int. J. Qual. Health Care 2019. [Google Scholar] [CrossRef]
- Warouw, H.J. The Quality of Nursing Service and Patients’ Satisfaction In The Inpatient Room of Pancaran Kasih Gmim Hospital Manado. Int. J. Health Med. Curr. Res. 2017, 2, 269–274. [Google Scholar]
- Persson, E.; Anderberg, P.; Ekwall, A.K. A room of one′s own—Being cared for in a hospital with a single-bed room design. Scand. J. Caring Sci. 2014, 29, 340–346. [Google Scholar] [CrossRef]
- Tzeng, H.-M.; Yin, C.-Y. The Extrinsic Risk Factors for Inpatient Falls in Hospital Patient Rooms. J. Nurs. Care Qual. 2008, 23, 233–241. [Google Scholar] [CrossRef]
- Kleefstra, S.M.; Zandbelt, L.C.; De Haes, H.J.C.J.M.; Kool, R.B. Trends in patient satisfaction in Dutch university medical centers: Room for improvement for all. BMC Health Serv. Res. 2015, 15, 112. [Google Scholar] [CrossRef]
- Devlin, A.S.; Andrade, C.C.; Carvalho, D. Qualities of Inpatient Hospital Rooms: Patients' Perspectives. HERD Health Environ. Res. Des. J. 2015, 9, 190–211. [Google Scholar] [CrossRef]
- Raven, M.C.; Gillespie, C.C.; Dibennardo, R.; Van Busum, K.; Elbel, B. Vulnerable Patients' Perceptions of Health Care Quality and Quality Data. Med. Decis. Mak. 2011, 32, 311–326. [Google Scholar] [CrossRef]
| LVs | MVs | TV | FL | CA | CR | AVE |
|---|---|---|---|---|---|---|
| LV1: Satisfaction with hospital, department, room and board | MV_11 | IV | 0.727 | 0.847 | 0.775 | 0.535 |
| MV_13 | 0.697 | |||||
| MV_14 | 0.769 | |||||
| LV2: Satisfaction with medical staff (nurses, physician’s expertise and other staff) | MV_21 | IV | 0.759 | 0.798 | 0.811 | 0.520 |
| MV_23 | 0.817 | |||||
| MV_24 | 0.629 | |||||
| MV_25 | 0.663 | |||||
| LV3: Satisfaction with the quality of treatment provided | MV_31 | IV | 0.803 | 0.926 | 0.894 | 0.589 |
| MV_33 | 0.606 | |||||
| MV_34 | 0.836 | |||||
| MV_35 | 0.852 | |||||
| MV_36 | 0.831 | |||||
| MV_37 | 0.637 | |||||
| LV4: Satisfaction with leaving the hospital | MV_41 | IV | 0807 | 0.847 | 0.734 | 0.581 |
| MV_42 | 0.714 | |||||
| LV5: Satisfaction with inpatient care | MV_51 | DV | 0.908 | 0.902 | 0.919 | 0.792 |
| MV_52 | 0.922 | |||||
| MV_55 | 0.837 |
| The Goodness of Fit Measures | Absolute Fit Indices | Relative Fit Indices | Non-Centrality-Based Indices | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CMIN/df | p-Value | GFI | NFI | IFI | TLI | CFI | RMSEA | RNI | |
| Measurement Model | 2.625 | 0.038 | 0.959 | 0.937 | 0.974 | 0.969 | 0.973 | 0.022 | 0.964 |
| Structural Model | 2.782 | 0.041 | 0.953 | 0.921 | 0.968 | 0.963 | 0.927 | 0.024 | 0.959 |
| Criterion (Threshold values) | <5.0 | <0.05 | >0.95 | >0.90 | >0.95 | >0.95 | >0.95 | <0.05 | >0.95 |
| H | Independent Variable (IV) | Regression Paths | β | SE | T | p-Value | Decision |
|---|---|---|---|---|---|---|---|
| H1 | LV1: Satisfaction with hospital, department, room and board | LV1 † → LV5 | 0.233 | 0.039 | 6.689 | 0.000 * | Supported |
| H2 | LV2: Satisfaction with medical staff (nurses, physician’s expertise and other staff) | LV2 † → LV5 | 0.597 | 0.041 | 16.974 | 0.000 * | Supported |
| H3 | LV3: Satisfaction with the quality of treatment provided | LV3 † → LV5 | 0.538 | 0.025 | 20.363 | 0.000 * | Supported |
| H4 | LV4: Satisfaction with leaving the hospital | LV4 † → LV5 | 0.547 | 0.043 | 11.721 | 0.000 * | Supported |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gavurova, B.; Dvorsky, J.; Popesko, B. Patient Satisfaction Determinants of Inpatient Healthcare. Int. J. Environ. Res. Public Health 2021, 18, 11337. https://doi.org/10.3390/ijerph182111337
Gavurova B, Dvorsky J, Popesko B. Patient Satisfaction Determinants of Inpatient Healthcare. International Journal of Environmental Research and Public Health. 2021; 18(21):11337. https://doi.org/10.3390/ijerph182111337
Chicago/Turabian StyleGavurova, Beata, Jan Dvorsky, and Boris Popesko. 2021. "Patient Satisfaction Determinants of Inpatient Healthcare" International Journal of Environmental Research and Public Health 18, no. 21: 11337. https://doi.org/10.3390/ijerph182111337
APA StyleGavurova, B., Dvorsky, J., & Popesko, B. (2021). Patient Satisfaction Determinants of Inpatient Healthcare. International Journal of Environmental Research and Public Health, 18(21), 11337. https://doi.org/10.3390/ijerph182111337






