Maternal and Perinatal Outcomes among Maternity Waiting Home Users and Non-Users in Rural Rwanda
Abstract
:1. Introduction
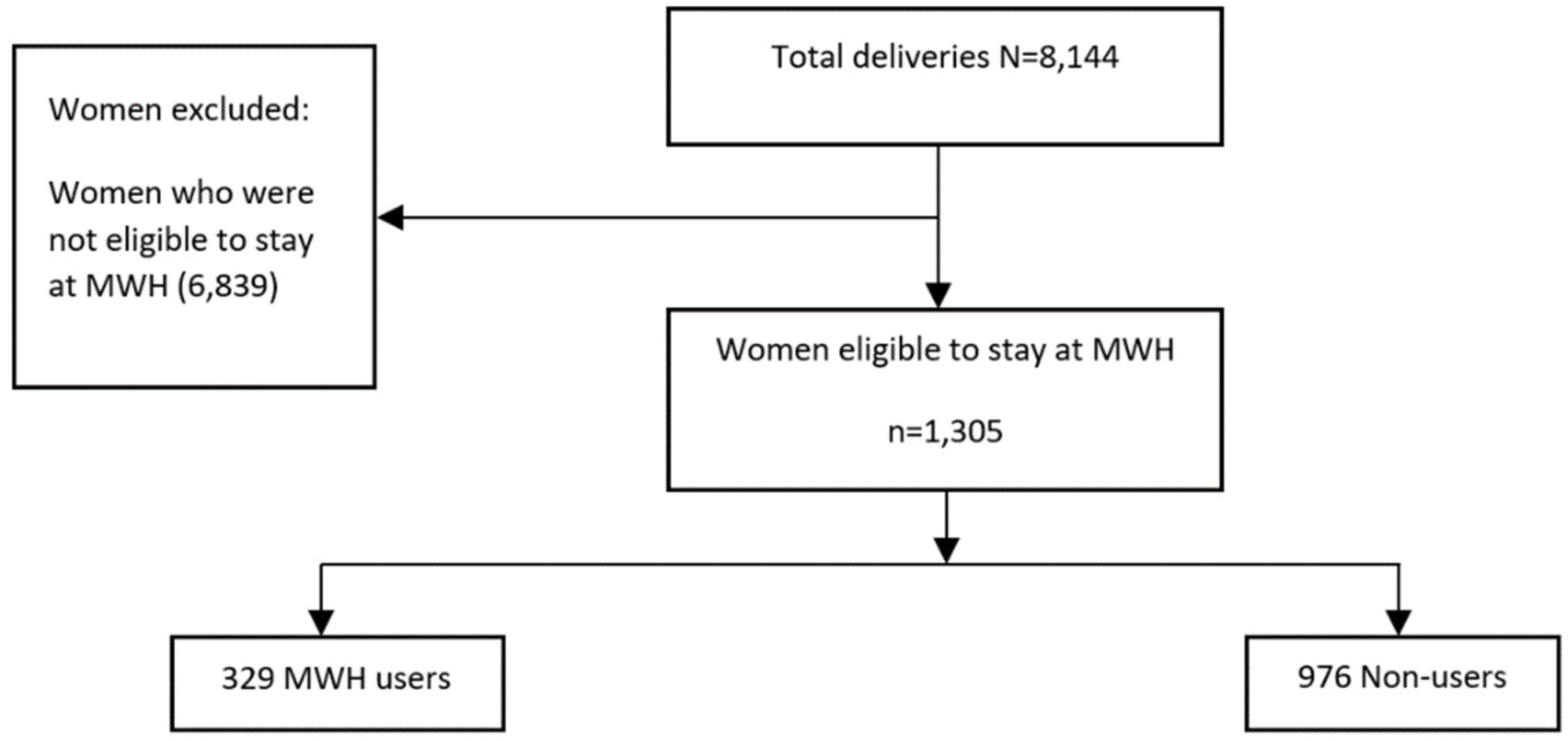
2. Materials and Methods
3. Results
3.1. Indications for Admission
3.2. Socio-Demographic Characteristics of Women (MWH-Users and Non-Users)
3.3. Maternal and Perinatal Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Trends in Maternal Mortality 2000 to 2017: Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: Executive Summary; Report No.: WHO/RHR/19.23; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Alkema, L.; Chou, D.; Hogan, D.; Zhang, S.; Moller, A.B.; Gemmill, A.; Fat, D.M.; Boerma, T.; Temmerman, M.; Mathers, C. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 2016, 387, 462–474. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. World Health Statistics 2016: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Essendi, H.; Mills, S.; Fotso, J.C. Barriers to formal emergency obstetric care services’ utilization. J. Urban Health 2011, 88 (Suppl. 2), S356–S369. [Google Scholar] [CrossRef] [Green Version]
- Tiruneh, G.T.; Getu, Y.N.; Abdukie, M.A.; Eba, G.G.; Keyes, E.; Bailey, P.E. Distribution of maternity waiting homes and their correlation with perinatal mortality and direct obstetric complication rates in Ethiopia. BMC Pregnancy Childbirth 2019, 19, 214. [Google Scholar] [CrossRef]
- van Lonkhuijzen, L.; Stekelenburg, J.; van Roosmalen, J. Maternity waiting facilities for improving maternal and neonatal outcome in low-resource countries. Cochrane Database Syst. Rev. 2012, 10, Cd006759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hussein, J.; Kanguru, L.; Astin, M.; Munjanja, S. The effectiveness of emergency obstetric referral interventions in developing country settings: A systematic review. PLoS Med. 2012, 9, e1001264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rwanda National Office of Population (ONAPO); National Institute of Statistics of Rwanda (NISR); Ministry of Health (MOH); ICF. Rwanda Demographic and Health Survey 2000; NISR: Kigali, Rwanda; ICF: Calverton, MD, USA, 2001. [Google Scholar]
- National Institute of Statistics of Rwanda (NISR); Ministry of Health (MOH); ICF. Rwanda Demographic and Health Survey 2019–2020 Key Indicators Report; Report No.: 978-99977-43-09-1; NISR: Kigali, Rwanda; ICF: Rockville, MD, USA, 2020. [Google Scholar]
- Sayinzoga, F.; Bijlmakers, L.; van Dillen, J.; Mivumbi, V.; Ngabo, F.; van der Velden, K. Maternal death audit in Rwanda 2009–2013: A nationwide facility-based retrospective cohort study. BMJ Open 2016, 6, e009734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalisa, R.; Rulisa, S.; van den Akker, T.; van Roosmalen, J. Maternal Near Miss and quality of care in a rural Rwandan hospital. BMC Pregnancy Childbirth 2016, 16, 324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Penn-Kekana, L.; Pereira, S.; Hussein, J.; Bontogon, H.; Chersich, M.; Munjanja, S.; Portela, A. Understanding the implementation of maternity waiting homes in low- and middle-income countries: A qualitative thematic synthesis. BMC Pregnancy Childbirth 2017, 17, 269. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Recommendations on Health Promotion Interventions for Maternal and Newborn Health 2015; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Dadi, T.L.; Bekele, B.B.; Kasaye, H.K.; Nigussie, T. Role of maternity waiting homes in the reduction of maternal death and stillbirth in developing countries and its contribution for maternal death reduction in Ethiopia: A systematic review and meta-analysis. BMC Health Serv. Res. 2018, 18, 748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bekele, B.B.; Dadi, T.L.; Tesfaye, T. The significant association between maternity waiting homes utilization and perinatal mortality in Africa: Systematic review and meta-analysis. BMC Res. Notes 2019, 12, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelly, J.; Kohls, E.; Poovan, P.; Schiffer, R.; Redito, A.; Winter, H.; MacArthur, C. The role of a maternity waiting area (MWA) in reducing maternal mortality and stillbirths in high-risk women in rural Ethiopia. Bjog 2010, 117, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Braat, F.; Vermeiden, T.; Getnet, G.; Schiffer, R.; van den Akker, T.; Stekelenburg, J. Comparison of pregnancy outcomes between maternity waiting home users and non-users at hospitals with and without a maternity waiting home: Retrospective cohort study. Int. Health 2018, 10, 47–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niringiye, A.; Ayebale, C. Impact Evaluation of the Ubudehe Programme in Rwanda: An Examination of the Sustainability of the Ubudehe Programme. J. Sustain. Dev. Afr. 2012, 14, 3. [Google Scholar]
- Sialubanje, C.; Massar, K.; Hamer, D.H.; Ruiter, R.A.C. Personal and environmental factors associated with the utilisation of maternity waiting homes in rural Zambia. BMC Pregnancy Childbirth 2017, 17, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mramba, L.; Nassir, F.A.; Ondieki, C.; Kimanga, D. Reasons for low utilization of a maternity waiting home in rural Kenya. Int. J. Gynaecol. Obstet. 2010, 108, 152–153. [Google Scholar] [CrossRef] [PubMed]
- Erickson, A.K.; Abdalla, S.; Serenska, A.; Demeke, B.; Darmstadt, G.L. Association between maternity waiting home stay and obstetric outcomes in Yetebon, Ethiopia: A mixed-methods observational cohort study. BMC Pregnancy Childbirth 2021, 21, 482. [Google Scholar] [CrossRef] [PubMed]
- Getachew, B.; Liabsuetrakul, T.; Gebrehiwot, Y. Association of maternity waiting home utilization with women’s perceived geographic barriers and delivery complications in Ethiopia. Int. J. Health Plan. Manag. 2020, 35, e96–e107. [Google Scholar] [CrossRef] [PubMed]
| Indications | Users, n = 329 (%) | Non-Users, n = 976 (%) | Total, n = 1305 |
|---|---|---|---|
| Previous CS | 87 (26.4) | 390 (40.0) | 477 |
| Post term pregnancy | 21 (6.4) | 58 (5.9) | 79 |
| PPROM * | 6 (1.8) | 49 (5.0) | 55 |
| Abdominal pain/lumbopelvic pain | 20 (6.1) | 32 (3.3) | 52 |
| Preterm labor | 15 (4.6) | 34 (3.5) | 49 |
| Pre-eclampsia | 8 (2.4) | 32 (3.3) | 40 |
| Excessive fundal height | 6 (1.8) | 32 (3.3) | 38 |
| Fetal abnormal lie/presentation | 11 (3.3) | 32 (3.3) | 43 |
| CPD ** | 6 (1.8) | 32 (3.3) | 38 |
| Suspected IUFD *** | 7 (2.1) | 19 (1.9) | 26 |
| History of prolonged labor | 4 (1.2) | 22 (2.3) | 26 |
| Fetal distress | 7 (2.1) | 31 (3.2) | 38 |
| Other | 97 (29.5) | 213 (21.8) | 310 |
| Not documented | 34 (10.3) | 0 (0.0) | 34 |
| Characteristics | MWH Users | MWH Non-Users | Total | X2 | p-Value | ||
|---|---|---|---|---|---|---|---|
| n = 329 | % | n = 976 | % | n = 1305 | |||
| Maternal age | |||||||
| ≤25 | 121 | 36.78 | 268 | 27.46 | 389 | 10.2 | 0.006 |
| 26–30 | 78 | 23.71 | 270 | 27.66 | 348 | ||
| ≥31 | 130 | 39.51 | 438 | 44.88 | 568 | ||
| Parity | |||||||
| P0 | 106 | 32.22 | 295 | 30.23 | 401 | 2.5 | 0.285 |
| P1–P3 | 202 | 61.4 | 637 | 65.27 | 839 | ||
| P4 and above | 21 | 6.38 | 44 | 4.51 | 65 | ||
| Marital status | |||||||
| Married | 224 | 68.09 | 762 | 78.07 | 986 | 23.6 | 0.000 |
| Single | 73 | 22.19 | 114 | 11.68 | 187 | ||
| Co-habiting | 4 | 1.22 | 13 | 1.33 | 17 | ||
| Separated/Divorced | 3 | 0.91 | 4 | 0.41 | 7 | ||
| Not documented | 25 | 7.6 | 83 | 8.5 | 108 | ||
| Occupation | |||||||
| Formal/Salaried employee | 4 | 1.22 | 19 | 1.95 | 23 | 3.1 | 0.364 |
| Subsistence farmer | 321 | 97.57 | 950 | 97.54 | 1271 | ||
| Business | 4 | 1.22 | 5 | 0.51 | 9 | ||
| Not documented | 0 | 0.0 | 2 | 0.20 | 2 | ||
| Health Insurance | |||||||
| Yes | 327 | 99.39 | 971 | 99.49 | 1298 | 0.04 | 0.837 |
| No | 2 | 0.61 | 5 | 0.51 | 7 | ||
| Prior stillbirth | |||||||
| Yes | 5 | 1.52 | 28 | 2.87 | 33 | 13.7 | 0.001 |
| No | 323 | 98.18 | 908 | 93.03 | 1231 | ||
| Not documented | 1 | 0.30 | 40 | 4.10 | 41 | ||
| Number of ANC * visits | |||||||
| ANC < 4 | 92 | 27.96 | 236 | 24.18 | 328 | 4.1 | 0.127 |
| ANC ≥ 4 | 55 | 16.71 | 209 | 21.41 | 264 | ||
| Not documented | 182 | 55.32 | 531 | 54.4 | 713 | ||
| History of prenatal maternal disease | |||||||
| Yes | 41 | 12.46 | 133 | 13.63 | 174 | 2.7 | 0.245 |
| No | 287 | 87.23 | 830 | 85.04 | 1117 | ||
| Not documented | 1 | 0.3 | 13 | 1.33 | 14 | ||
| Prior C/S ** | |||||||
| Yes | 128 | 38.91 | 463 | 47.44 | 591 | 7.2 | 0.007 |
| No | 201 | 61.09 | 513 | 52.56 | 714 | ||
| Outcomes | MWH Users n = 329 (%) | MWH Non-Users n = 976 (%) | OR (95% CI) | p-Value |
|---|---|---|---|---|
| Maternal | ||||
| Mode of delivery | ||||
| Spontaneous vaginal delivery | 127 (38.6) | 164 (16.8) | (Ref) | (Ref) |
| Cesarean section | 190 (57.75) | 749 (76.74) | 0.33 (0.25–0.43) | 0.000 |
| Vacuum extraction | 12 (3.65) | 63 (6.45) | 0.25 (0.13–0.46) | 0.000 |
| Type of maternal complication | ||||
| No maternal complication | 321 (97.6) | 854 (87.4) | (Ref) | (Ref) |
| PPH | 7 (2.13) | 55 (5.64) | 0.33 (0.15–0.75) | 0.008 |
| Eclampsia | 0 (0.0) | 4 (0.41) | - | - |
| Severe pre-eclampsia | 0 (0.0) | 3 (0.31) | - | - |
| Puerperal sepsis | 1 (0.3) | 12 (1.23) | 0.22 (0.02–1.71) | 0.149 |
| Ruptured uterus | 0 (0) | 9 (0.92) | - | - |
| Others | 0 (0.0) | 39 (4.0) | - | - |
| Maternal outcome | ||||
| Live | 329 (100) | 972 (99.59) | (Ref) | (Ref) |
| Death | 0 (0.0) | 4 (0.41) | - | - |
| Perinatal | ||||
| Birth Asphyxia | ||||
| No | 319 (96.9) | 928 (95.1) | (Ref) | (Ref) |
| Yes | 10 (3.1) | 48 (4.9) | 0.6 (0.3–1.21) | 0.157 |
| Immediate neonatal outcome | ||||
| Live birth | 326 (99.09) | 901 (92.32) | (Ref) | (Ref) |
| Stillbirth | 3 (0.91) | 75 (7.68) | 0.11 (0.04–0.35) | 0.000 |
| Type of stillbirth | ||||
| Fresh | 2 (66.67) | 41 (54.67) | (Ref) | (Ref) |
| Macerated | 0 (0) | 22 (29.33) | _ | _ |
| Not documented | 1 (33.33) | 12 (16) | 1.7 (0.14–20.5) | 0.673 |
| Neonatal outcomes | ||||
| Discharged | 325 (99.69) | 898 (99.67) | (Ref) | (Ref) |
| Died | 1 (0.31) | 3 (0.33) | 0.92 (0.1–8.9) | 0.943 |
| Referred | 3 (0.91) | 75 (7.68) | 0.11 (0.03–0.35) | 0.000 |
| Outcomes | MWH Users n = 329 (%) | MWH Non-Users n = 976 (%) | aOR (95% CI) | p-Value |
|---|---|---|---|---|
| Maternal | ||||
| Mode of delivery | ||||
| Spontaneous vaginal delivery | 127 (38.6) | 164 (16.8) | (Ref) | (Ref) |
| Cesarean section | 190 (57.75) | 749 (76.74) | 0.24 (0.18–0.33) | 0.000 |
| Vacuum extraction | 12 (3.65) | 63 (6.45) | 0.20 (0.10–0.40) | 0.000 |
| Perinatal | ||||
| Birth Asphyxia | ||||
| No | 319 (96.9) | 928 (95.1) | (Ref) | (Ref) |
| Yes | 10 (3.1) | 48 (4.9) | 0.46 (0.22–0.98) | 0.044 |
| Immediate neonatal outcome | ||||
| Live birth | 326 (99.09) | 901 (92.32) | (Ref) | (Ref) |
| Stillbirth | 3 (0.91) | 75 (7.68) | 0.05 (0.02–0.16) | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tayebwa, E.; Kalisa, R.; Ndibaza, A.F.; Cornelissen, L.; Teeselink, E.K.; Kim, Y.-M.; van Dillen, J.; Stekelenburg, J. Maternal and Perinatal Outcomes among Maternity Waiting Home Users and Non-Users in Rural Rwanda. Int. J. Environ. Res. Public Health 2021, 18, 11211. https://doi.org/10.3390/ijerph182111211
Tayebwa E, Kalisa R, Ndibaza AF, Cornelissen L, Teeselink EK, Kim Y-M, van Dillen J, Stekelenburg J. Maternal and Perinatal Outcomes among Maternity Waiting Home Users and Non-Users in Rural Rwanda. International Journal of Environmental Research and Public Health. 2021; 18(21):11211. https://doi.org/10.3390/ijerph182111211
Chicago/Turabian StyleTayebwa, Edwin, Richard Kalisa, Amedee Fidele Ndibaza, Lisa Cornelissen, Eefje Klein Teeselink, Young-Mi Kim, Jeroen van Dillen, and Jelle Stekelenburg. 2021. "Maternal and Perinatal Outcomes among Maternity Waiting Home Users and Non-Users in Rural Rwanda" International Journal of Environmental Research and Public Health 18, no. 21: 11211. https://doi.org/10.3390/ijerph182111211
APA StyleTayebwa, E., Kalisa, R., Ndibaza, A. F., Cornelissen, L., Teeselink, E. K., Kim, Y.-M., van Dillen, J., & Stekelenburg, J. (2021). Maternal and Perinatal Outcomes among Maternity Waiting Home Users and Non-Users in Rural Rwanda. International Journal of Environmental Research and Public Health, 18(21), 11211. https://doi.org/10.3390/ijerph182111211






