Perceptions and Experiences of Orthodox Health Practitioners and Hospital Administrators towards Integrating Traditional Medicine into the Ghanaian Health System
Abstract
:1. Introduction
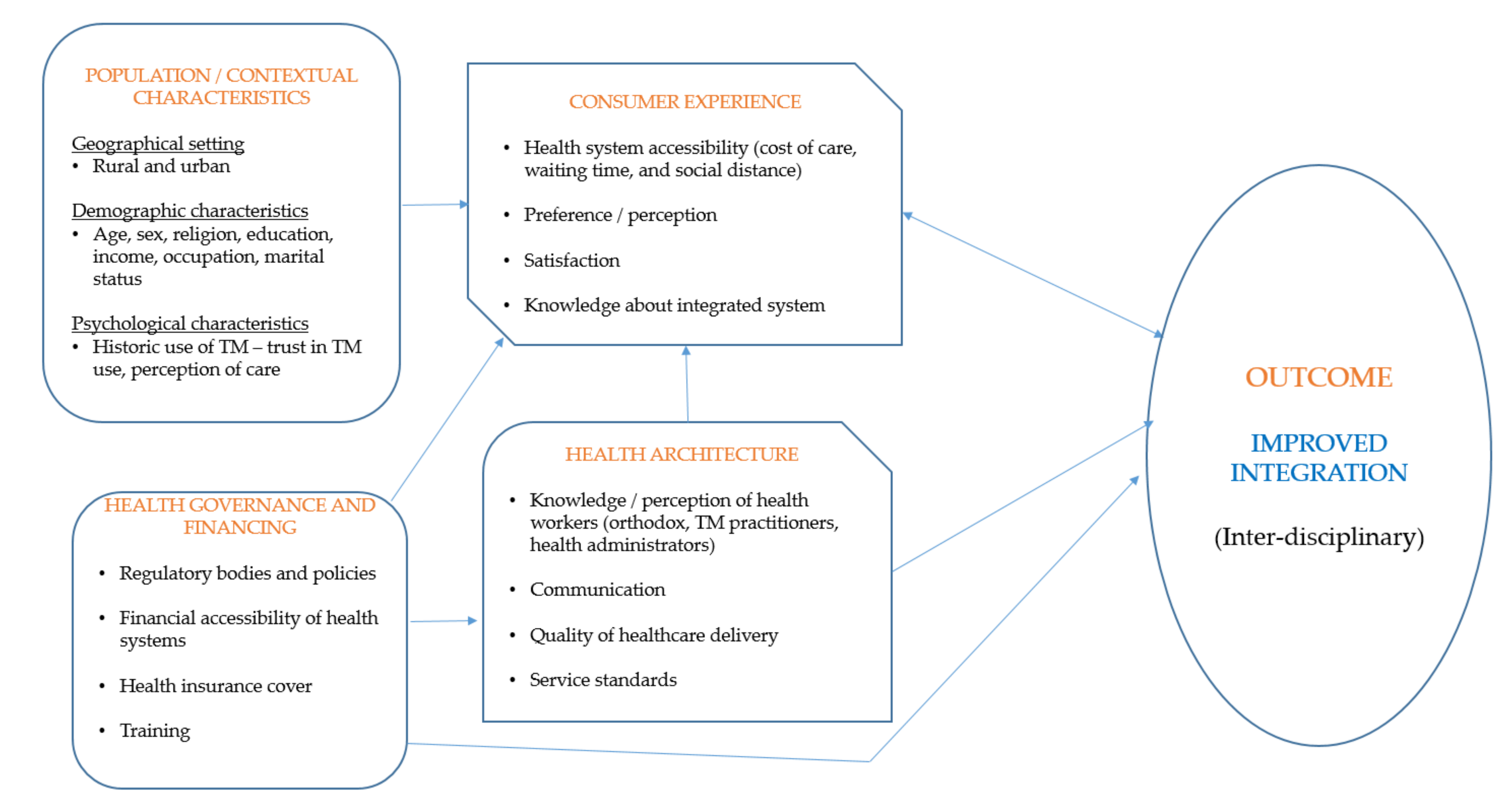
Theoretical Framework
2. Materials and Methods
2.1. Ethics Approval
2.2. Study Design
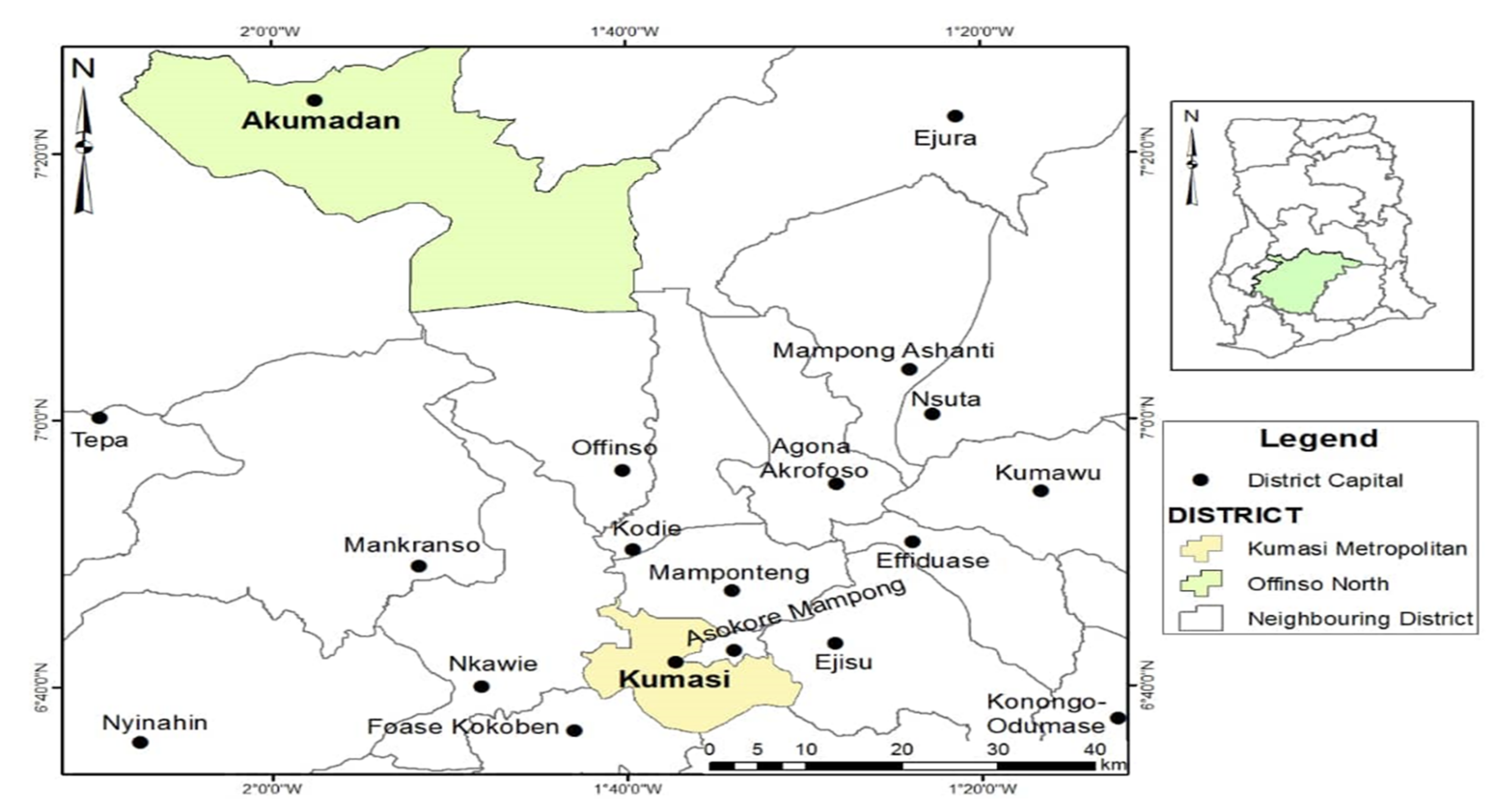
2.3. Study Setting
2.4. Target Population and Recruitment Strategy
2.5. Data Collection Period
2.6. Data Collection Procedure
2.7. Data Analysis
3. Results
3.1. Characteristics of Participants
3.2. Themes
3.2.1. Regulatory Bodies and Policies
“I know there is a law that has set up the TM Act; it captures all issues relating to TM practice in Ghana”.[Participant 4, PM, Offinso north]
“…after production, the FDA will come and check the procedures used and once the practitioner is done, they will test the safety of the medicine before they accept it and release it onto the market for sale”.[Participant 1, PM, Offinso north]
“From where I sit, I do not think they are doing much. As a facility, the regional health team comes to do monitoring and evaluation. When you look at those in the private practice, I think most of them do not have the license to practice and I am not aware of the council going to monitor their practice”.[Participant 2, HA, Kumasi]
3.2.2. Financial Accessibility of Health Systems
“Those TM that are in pharmacies and licensed chemical shops or clinics are expensive. TM treatments for malaria from these avenues are more costly compared to orthodox malaria treatment”.[Participant 1, NS, Offinso north]
“Comparatively, the TM clinic that my relative attends; it appears that the cost is higher compared to the orthodox clinics. The medications that she received there for two weeks cost about GHC 1200 which is on the high side if you compared to the orthodox medicine where the medications given were not expensive, not even up to GHC 300”.[Participant 2, HA, Kumasi]
“When people come for TM services/products, except for the folder, they pay for everything including the TM products. These products are expensive. So clients paying out of pocket is challenging because most of these people come here without holding even GHC 10 or GHC 20. They (clients) are unable to afford the TM at the TM unit hence accounting for low patronage”.[Participant 6, HA, Kumasi]
3.2.3. Health Insurance Cover
“The health insurance coverage is high, a lot of people are having the cards but the insurance covers only the cost of orthodox treatments and drugs”.[Participant 5, MD, Offinso north]
“It is very high. In terms of percentage, it will be like 70% because when you come in here to our hospital, about 90% of our IGF is from the health insurance. The insurance includes only the mainstream health services”.[Participant 6, HA, Kumasi]
3.2.4. Training
“Some TM practitioners are not well educated. They will say they inherited the skill from their fathers or grandfathers. Their level of formal training is not too encouraging. So why wont the doctors look down on TM practice”.[Participant 1, NS, Offinso north]
“When it comes to the TM, the training is low, people are calling themselves doctors and pharmacists but you do not know where they acquired their knowledge. They just spend some time with their grandparents and they call themselves doctors. So, there is no certificate!”.[Participant 1, HA, Kumasi]
“I know how an anti-malarial works but I do not know how the traditional anti-malarial works. I have never been exposed to it but you want me to accept it; I will never accept it and work with them. That is the barrier we are having”.[Participant 3, MD, Offinso north]
3.2.5. Knowledge about TM Integration
“There is a TM department at KNUST and it is a four-year program. I know the program is still going on. It is under the Faculty of Pharmacy”.[Participant 4, PM, Offinso north]
“At KNUST, there is a department for TM. They train people to become experts in the TM area”.[Participant 5, HA, Offinso north]
“At KNUST, there is a department for TM. They are into researching TM and how it can serve as an appropriate healthcare. I know they are under the Faculty of Pharmacy”.[Participant 2, MD, Kumasi]
“Tafo government hospital and I think Kumasi South hospital have this system. I mean the integrated system. I think it is something that the Ghana Health Service is trying to bring on board. I got to know about the integration through my interactions with colleagues”.[Participant 7, MD, Kumasi]
“I know of three facilities that operate this integrated system: Suntreso government hospital, Tafo government hospital and Kumasi South hospital. They sent a circular or memo around that from this day; they are bringing TM practitioners so that they would practice in the hospital/facility”[Participant 3, PM, Kumasi]
“I know that they have started in some hospitals but not all health facilities. I think the integrated facilities in the region are three. I cannot really remember the source of the information; maybe it was through a conversation”[Participant 1, NS, Offinso north]
“The TM unit is part of the hospital; it is part of the units in the hospital. They have their reporting system and at the end of the day, everything gets to the medical director. So, as an administrator I know that there is a structured TM clinic in this facility, therefore we are one of the facilities that deliver integrated services in the region. I became familiar with integrated facilities because I happen to work here”.[Participant 1, HA, Kumasi]
3.2.6. Perceptions about Traditional and Orthodox Health Systems
“In the past, before the coming of the Whites, our ancestors were using these TM and they were getting the results. So TM has been with Ghanaians for a long time. That is the oldest form of care in Ghana”.[Participant 3, MD, Offinso north]
“That has been our way of treating illnesses. The typical Ghanaian or African will not seek modern healthcare if they have an issue. They will try what they know first, that is the traditional therapies. When I was a child, I was asked to take the TM called ’Acheampong’. So, it has been part of us for a long time”.[Participant 5, PM, Offinso north]
“I can even say that most of them (TM) come with little or no side effects because they are like the foods that we eat. We all know paracetamol has side effects and so do other orthodox medicines. If you do not read the instructions carefully and you take the medicine, then you would feel dizzy. However, when it comes to the TM, although some of them come with little side effects, most of them do not have side effects”.[Participant 1, HA, Kumasi]
“So, the orthodox system comprise of activities that are supported by science. I cannot do whatever I like because I am a medical doctor. My actions should be science-based. But with the traditional way of treating diseases, laboratory tests are not taken into consideration before certain medications are given to the person who is accessing the care”.[Participant 7, MD, Kumasi]
“See, TM is already in existent in our system so people already know of it. So, there is ready market, which is somewhat good for the integration because it will not be new to people”.[Participant 5, MD, Offinso north]
“The availability of medicinal plants is an opportunity to boost integration. We do not have to export materials to sustain the TM field. Medicinal plants are already there. We making use of such plants and other things in our ecosystem is a great opportunity for integration”.[Participant 4, PM, Offinso north]
“These medicinal plants are all around us. Just look at even our health facility here, there are many plants around us. Most of them are medicines including the Nim tree so we cannot run out of raw materials for TM products, which to me could sustain the integrated system”.[Participant 1, NS, Offinso north]
3.2.7. Communication
“Patients hardly tell us their use of TM. I do not know whether it is because patients have the notion that, generally health workers at the hospital frown on TM usage”.[Participant 2, MD, Kumasi]
“You have to ask the client’s past medical history. If the patient has taken or applied any TM, they will tell you. So, you have to ask them and they will tell you”.[Participant 1, NS, Offinso north]
“…sometimes I feel like we the medical doctors are to be blamed in a way. The part that we do not do well is that we do not offer people enough information on what and when to do what and that is what the patients want. So, we sort of put them (patients) in a state where they have to find other means of care”.[Participant 6, MD, Kumasi]
“I have not referred any of my patients to seek care from any TM practitioner. I have not done that before. What I have realised is that, TM practitioners do not refer cases on time. They delay until the patient’s condition has deteriorated before they refer and they do that just by word of mouth”.[Participant 5, MD, Offinso north]
“We buy airtime and go to the radio station to talk about the integration. So we talk about the creation of TM unit in our facility”.[Participant 1, HA, Kumasi]
“I only got to know about the integrated system because of the TM department within the hospital. Aside that, I have not heard of the integration of TM from any other place, which I think is a problem. How do you practice something you do not know? How can people also access a service that they do not know it exist?”.[Participant 4, MD, Kumasi]
“As for the publicity, I think it is one of the challenges. Most people do not even know that when they come to the facility, they can have access to TM, except for the clients that are already aware. In this hospital and the others, we have not done enough to publicise the integration. I am the administrator and I know that we do not have directional signs. The publicity is not there”.[Participant 4, HA, Kumasi]
3.2.8. Quality of Healthcare Delivery
“Before a medical officer will get to you, there is something we do called triaging. We try to assess your medical situation and condition to get to the bottom of things. So, we ask couple of questions, do physical examinations and if necessary conduct laboratory tests to get to the root of ailments. We do all these things with the aim of delivery quality healthcare to the patient”.[Participant 7, MD, Kumasi]
“…mostly I call the doctors and tell them that I have realised that they are prescribing something to patients but I think it should be this or that. I am able to do that because of some commonalities in the practice. For example, there was a pregnant woman who came from a facility, different from ours. They had prescribed ‘ergometry’. If a pregnant woman takes that drug, then it is likely to cause an abortion. So, sometimes, it is not that the doctor does not know what he/she is doing but they might have been a slip of hand where the mind is going faster than the hand. So, I went to the facility and told the doctor that with all due respect, I saw ‘ergometry’ but I think it is ‘ergotamine’, and so he should confirm, so that the patient will come back and he did. You see! At the end, the patient received the best of care. We usually get favourable results where both the doctors and patients will come back to say thank you”.[Participant 2, PM, Kumasi]
“The patients who patronise services in this facility are open to make a choice whether they want the TM or orthodox medicine. So, there are options for them to choose from. Patients have access to alternative healthcare”.[Participant 3, PM, Kumasi]
“Before a TM product is accepted within the integrated system, it goes through some tests and research. It passes through the research centre at Mampong to meet all the standards for the FDA to give approval, so gradually we are separating the good TM from the fake ones”.[Participant 1, HA, Kumasi]
“Because it is at the hospital, it helps to promote the safety of TM services. At the end of the day, we do not just give TM anyhow. It is according to acceptable standards in healthcare. When a patient comes to the hospital, he/she will go for the folder and go through all the normal things/triaging before he/she sees the TM doctor”.[Participant 6, HA, Kumasi]
“In fact, the integration is a way of maintaining our indigenous medicines. It is serving as a way to come back to our traditions and culture”.[Participant 5, MD, Offinso north]
“When a client comes here for TM, he/she goes through the normal health checks at the Out Patient Department for them to check the vitals, weight and pressure. That way, we are able to collect information on people who access TM services, which is improving database on health accessibility”.[Participants 6, HA, Kumasi]
“Some people will come and they have hypertension and another person coming with erectile dysfunction. Yet, they will present one TM that can treat all these problems. I think about it and I ask myself how this is possible? So I do not trust those claims; hence do not have the desire to work with them (TM practitioners)”[Participant 6, MD, Kumasi]
“TM people at times make many claims about TM. They make so many claims that one TM can cure multiple diseases…. You see! These claims are dangerous to the practice of medicine”[Participant 5, PM, Offinso north]
“You will see so many TM practitioners around claiming that one medicine can cure almost everything. So, you wonder if that is truly so. So, it affects how other health practitioners trust the TM system, and if trust is diminished, it affects collaboration”.[Participant 4, HA, Kumasi]
3.2.9. Service Standards
“The challenge I have with TM is the quantification of their doses, and probably the hygienic state of its preparation. In addition, they (TM practitioners) do not normally state the side effects of the TM; neither do they provide an antidote to overdose. So, in the case of overdose, what do you do? You do not get answers to these questions. So how do you work with people in a field that they do not give you enough information to work with?”.[Participant 1, MD, Offinso north]
“The problem I have as a pharmacist is its (TM) standardisation. How do I know that this is the dosage? Sometimes, they will tell you to use a cup to measure and drink, which is not right”.[Participant 4, PM, Offinso north]
“Sometimes, the way it is prepared, the environment, the tidiness and all those things make it non-standardised”[Participant 3, HA, Offinso north]
“There is lack of protocol for integration. We know that there is integration but when do I refer patients. We should know that you have to refer a patient when the temperature is above this or that. The TM practitioners should know that they have to refer if their (clients) are having this or that symptoms. How do we know when to refer to a TM practitioner or a medical doctor? The absence of such a protocol makes interaction in the system problematic. Everyone is doing his/her own thing”.[Participant 2, PM, Kumasi]
“The issue is that, how do we integrate them into the salary structure and all that? So, fair wages and salaries commission would have to look at the progression for TM practitioners. The absence of a document spelling out all these dynamics make the integration far from perfect. Is it as if institutions are acting per their understanding, which is a big hindrance to integration”.[Participant 4, PM, Kumasi]
3.3. Recommendations Made by Participants to Enhance TM Integration into the Ghanaian Health System
3.3.1. Stringent and Well Implemented TM Regulatory System
“The FDA can have sub associations that can monitor some of these things. I think the law enforcement agencies too can also help. Once a while, the FDA can send people to the pharmacy stores to check if the board has accepted those drugs”.[Participant 2, MD, Kumasi]
“I think more stringent measures should be placed on TM preparation. It always comes out that the FDA has approved it. Yet, occasionally, you will see that the FDA will ban certain products. Even with the products that the FDA says have been banned, you will still find them on the market. This do not make people take its integration seriously. So, the post-market surveillance should be more. It will put the TM practitioners on their toes and they will not just release anything on the market. Once there is sanity in the TM system, people will endorse the integration”.[Participant 2, PM, Kumasi]
“For every product, there is the grand ml, the manufacturing date, expiry date, and how you will take it, the storage and those things. Therefore, when these things are clearly labelled on TM containers, then it will ensure that the user do not go beyond or below the dosage and it will improve TM practice and its integration”.[Participant 1, PM, Offinso north]
“…it is very critical to label TM with the expiry date. When practitioners do that, they boost the public’s confidence in taking TM products and it can fit well in the formal health system”.[Participant 7, MD, Kumasi]
“We should know the specific ingredients a TM product contain and the specific therapeutic effect it can address rather than being all over the place. When therapeutic effect is known then we will know, the specific disease conditions it will treat and its integration will be welcomed”.[Participant 4, MD, Kumasi]
3.3.2. Comprehensive Health Insurance
“It is like the hospital; when a pregnant woman comes to the hospital, I will take her to the maternity unit, which is not the hospital. We have different wings but we are all working in concert to achieve a common goal for our clients. So, if you have two different systems, then merging them in all spheres, be it education, research and service delivery would be great. So, I think integrative approach is the best because both practitioners would be exposed to the two systems”.[Participant 3, MD, Offinso north]
“TM inclusion in the NHIS will help! I told you that some of the TM are costly. I am referring to the approved ones at pharmacies and clinics. So, if the insurance can cater for that, then it will be good. It will enable people to patronise the approved TM products”.[Participant 1, NS, Offinso north]
3.3.3. Training of TM
“For integration to work, then they need to include the TM in our medical school curriculum. That way, I can appreciate what that field of medicine is about and working with TM practitioners would not be a problem”.[Participant 4, MD, Kumasi]
“It will be great to establish TM departments in all universities in Ghana. We have many people who want to go to the university so, if we increase the number of TM departments, we will get more professionals in the field of TM, and the system will be improved”.[Participant 5, HA, Offinso north]
“There is also the need to increase the human resource. We need to train more people in TM so that we will have more qualified TM practitioners to practice in the various hospitals”.[Participant 7, PM, Kumasi]
3.3.4. Improved Communication Strategy
“There should be more education through the media; especially radio and television to sensitise the people about the integration. So that people will come to understand that, there is an established health system where users can decide the type of healthcare they want”.[Participant 1, HA, Kumasi]
“We need to increase publicity about the integration of the two health systems. There is no point for the integration if it only exist on paper. We can sensitise health users and practitioners about the system through community radio stations and even television stations”.[Participant 2, NS, Offinso north]
4. Discussion
4.1. Implications for Practice
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COREQ | Consolidated Criteria for Reporting Qualitative Studies |
| FDA | Food and Drug Authority |
| GHC | Ghana Cedis |
| GHS | Ghana Health Service |
| IGF | Internally Generated Funds |
| KNUST | Kwame Nkrumah University of Science and Technology |
| MD | Medical Doctor |
| NHIS | National Health Insurance Scheme |
| NS | Nurse |
| OM | Orthodox Medicine |
| PM | Pharmacist |
| TM | Traditional Medicine |
References
- World Health Organization. Traditional and Modern Medicine: Harmonising the Two Approaches: A Report of the Consultation Meeting on Traditional and Modern Medicine: Harmonising the Two Approaches; WHO Regional Office for the Western Pacific: Beijing, China, 2000. [Google Scholar]
- World Health Organization. The Promotion and Development of Traditional Medicine: Report of WHO Meeting; World Health Organization: Geneva, Switzerland, 1978. [Google Scholar]
- World Health Organization. WHO Traditional Medicine Strategy 2002–2005; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Abel, C.; Busia, K. An exploratory ethnobotanical study of the practice of herbal medicine by the Akan peoples of Ghana. Altern. Med. Rev. 2005, 10, 112–122. [Google Scholar]
- Gyasi, R.M.; Gyasi, R.M.; Poku, A.A.; Boateng, S.; Amoah, P.A.; Mumin, A.A.; Obodai, J. Integration for coexistence? Implementation of intercultural health care policy in Ghana from the perspective of service users and providers. J. Integr. Med. 2017, 15, 44–55. [Google Scholar] [CrossRef]
- Park, Y.L.; Canaway, R. Integrating Traditional and Complementary Medicine with National Healthcare Systems for Universal Health Coverage in Asia and the Western Pacific. Health Syst. Reform. 2019, 5, 24–31. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. The World Medicine Situation 2011. In Global Health Trends: Global Burden of Diseases and Pharmaceutical Needs, 3rd ed.; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Gyasi, R.M.; Siaw, L.P.; Mensah, C.M. Prevalence and pattern of traditional medical therapy utilisation in Kumasi Metropolis and Sekyere South District, Ghana. J. Ethnopharmacol. 2015, 161, 138–146. [Google Scholar] [CrossRef]
- Gyasi, R.M.; Tagoe-Darko, E.; Mensah, C.M. Use of traditional mediicne by HIV/AIDS patients in Kumasi metropolis, Ghana: A cross-sectional survey. Am. Int. J. Complement. Res. 2013, 3, 117–129. [Google Scholar]
- Davis, E.L.; Oh, B.; Butow, P.N.; Mullan, B.A.; Clarke, S. Cancer patient disclosure and patient-doctor communication of complementary and alternative medicine use: A systematic review. Oncologist 2012, 17, 1475–1481. [Google Scholar] [CrossRef] [Green Version]
- Robinson, A.; McGrail, M.R. Disclosure of CAM use to medical practitioners: A review of qualitative and quantitative studies. Complement. Ther. Med. 2004, 12, 90–98. [Google Scholar] [CrossRef]
- Clement, Y.N.; Williams, A.F.; Khan, K.; Bernard, T.; Bhola, S.; Fortune, M. A gap between acceptance and knowledge of herbal remedies by physicians: The need for educational intervention. BMC Complement. Altern. Med. 2005, 5, 20. [Google Scholar] [CrossRef] [Green Version]
- Pirotta, M.; Kotsirilos, V.; Brown, J.; Adams, J.; Morgan, T.; Williamson, M. Complementary medicine in general practice: A national survey of GP attitudes and knowledge. Aust. Fam. Phys. 2010, 39, 946–950. [Google Scholar]
- Suchard, J.R.; Suchard, M.A.; Steinfeldt, J.L. Physician knowledge of herbal toxicities and adverse herb-drug interactions. Eur. J. Emerg. Med. 2004, 11, 193–197. [Google Scholar] [CrossRef]
- Hsiao, A.; Mitchell, D.; Wong, M.D.; Goldstein, S.M.; Hong-Jian, Y.; Andersen, R.M. Variations in complementary and alternative medicine (CAM) use across racial/ethnic groups and development of ethnic-specific measures of CAM use. J. Altern. Complement. Med. 2006, 12, 281–290. [Google Scholar] [CrossRef]
- Wetzel, M.S.; Eisenberg, M.D.; Kaptchuk, T.J. Courses involving complementary and alternative medicine at US medical schools. JAMA 1998, 280, 784–787. [Google Scholar] [CrossRef] [Green Version]
- Osemene, K.P.; Elujoba, A.A.; Ilori, M.O. A Comparative Assessment of Herbal and Orthodox Medicines in Nigeria. Res. J. Med. Sci. 2011, 5, 280–285. [Google Scholar] [CrossRef] [Green Version]
- Coulter, I.D.; Singh, B.B.; Riley, D.; Der-Martirosian, C. Interprofessional referral patterns in an integrated medical system. J. Manip. Physiol. Ther. 2005, 28, 170–174. [Google Scholar] [CrossRef]
- Vasconi, E.; Owoahene-Acheampong, S. Recognition and integration of Traditional Medicine in Ghana: A perspective. Res. Rev. 2010, 26, 1–17. [Google Scholar] [CrossRef]
- Wiese, M.; Oster, C.; Pincombe, J. Understanding the emerging relationship between complementary medicine and mainstream health care: A review of the literature. Health 2010, 14, 326–342. [Google Scholar] [CrossRef]
- Kwame, A. Integrating Traditional Medicine and Healing into the Ghanaian Mainstream Health System: Voices from Within. Qual. Health Res. 2021, 31, 1847–1860. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.S.; Malik, F. Integration of complementary and traditional mediicnes in public healthcare systems: Challenges and methodology. J. Med. Plants Res. 2013, 7, 2953–2959. [Google Scholar]
- Chang, L.; Basnyat, I. Negotiating biomedical and traditional Chinese medicine treatments among elderly Chinese Singaporean women. Qual. Health Res. 2015, 25, 241–252. [Google Scholar] [CrossRef]
- Agyei-Baffour, P.; Kudolo, A.; Quansah, D.Y.; Boateng, D. Integrating herbal medicine into mainstream healthcare in Ghana: Clients’ acceptability, perceptions and disclosure of use. BMC Complement. Altern. Med. 2017, 17, 9. [Google Scholar] [CrossRef] [Green Version]
- Boateng, M.A.; Danso-Appiah, A.; Turkson, K.B.; Tersbøl, B.P. Integrating biomedical and herbal medicine in Ghana—Experiences from the Kumasi South Hospital: A qualitative study. BMC Complement. Altern. Med. 2016, 16, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kretchy, I.A.; Okere, H.A.; Osafo, J.; Afrane, B.; Sarkodie, J.; Debrah, P. Perceptions of traditional, complementary and alternative medicine among conventional healthcare practitioners in Accra, Ghana: Implications for integrative healthcare. J. Integr. Med. 2016, 14, 380–388. [Google Scholar] [CrossRef]
- Ampomah, I.G.; Malau-Aduli, B.S.; Malau-Aduli, A.E.O.; Emeto, T.I. Effectiveness of Integrated Health Systems in Africa: A Systematic Review. Medicine 2020, 56, 271. [Google Scholar]
- Appiah, B.; Amponsah, I.K.; Poudyal, A.; Mensah, M.L.K. Identifying strengths and weaknesses of the integration of biomedical and herbal medicine units in Ghana using the WHO Health Systems Framework: A qualitative study. BMC Complement. Altern. Med. 2018, 18, 286. [Google Scholar] [CrossRef] [Green Version]
- Ahenkan, A.; Opoku-Mensah Abrampa, F.; Boon, K.E. Integrating traditional and orthodox medical practices in health care delivery in developing countries: Lessons from Ghana. Int. J. Herb. Med. 2019, 7, 23–30. [Google Scholar]
- Fugh-Berman, A. Herb-drug interactions. Lancet 2000, 355, 134–138. [Google Scholar] [CrossRef]
- Mignone, J.; Bartlett, J.; O’Neil, J.; Orchard, T. Best practices in intercultural health: Five case studies in Latin America. J. Ethnobiol. Ethnomed. 2007, 3, 31. [Google Scholar] [CrossRef] [Green Version]
- Vandebroek, I. Intercultural health and ethnobotany: How to improve healthcare for underserved and minority communities? J. Ethnopharmacol. 2013, 148, 746–754. [Google Scholar] [CrossRef]
- Peprah, P.; Agyemang-Duah, W.; Arimiyaw, A.W.; Morgan, A.K.; Nachibi, S.U. Removing barriers to healthcare through an intercultural healthcare system: Focus group evidence. J. Integr. Med. 2021, 19, 29–35. [Google Scholar] [CrossRef]
- Kumah, E.; Ankomah, S.E.; Antwi, F. The role of first-line managers in healthcare change management: A Ghanaian context. Inter. J. Biosci. Technol. Manag. 2016, 6, 20–33. [Google Scholar]
- Lin, V.; Canaway, R.; Carter, B. Interface, interaction and integration: How people with chronic disease in Australia manage CAM and conventional medical services. Health Expect. 2015, 18, 2651–2665. [Google Scholar] [CrossRef] [PubMed]
- Creswell, J.W. Five Qualitative Approaches to Inquiry. In Qualitative Inquiry and Research Design: Choosing among Five Approaches, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2007; pp. 53–80. [Google Scholar]
- Peprah, P.; Agyemang-Duah, W.; Arthur-Holmes, F.; Budu, H.I.; Abalo, E.M.; Okwei, R. ‘We are nothing without herbs’: A story of herbal remedies use during pregnancy in rural Ghana. BMC Complement. Altern Med. 2019, 19, 1–12. [Google Scholar] [CrossRef]
- Guba, E.G.; Lincoln, Y.S. Competing Paradigms in Qualitative Research; Denzin, N.K., Lincoln, Y.S., Eds.; Sage: Thousand Oaks, CA, USA, 1994; pp. 105–117. [Google Scholar]
- Ashiagbor, G.; Ofori-Asenso, R.; Forkuo, E.K.; Agyei-Frimpong, S. Measures of geographic accessibility to health care in the Ashanti Region of Ghana. Sci. Afr. 2020, 11, e00453. [Google Scholar] [CrossRef]
- Ghana Statistical Service. 2010 Population and Housing Census: Summary Report of Final Results; Ghana Statistical Service: Accra, Ghana, 2012; pp. 1–103. [Google Scholar]
- GIS Unit of Department of Geography and Regional Planning UCC. Cartographer Map of Ashanti Region Showing Study Settings; Department of Geography and Regional Planning UCC: Accra, Ghana, 2019. [Google Scholar]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough? Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Srivastava, A.; Thomson, S.B. Framework Analysis: A qualitative methodology for Applied Policy Research. J. Adm. Gov. 2009, 4, 72–79. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [Green Version]
- Buor, D. Accessibility and utilisation of health services in Ghana: An overview. Access. Util. Health Serv. Ghana 2004, 7, 272. [Google Scholar]
- Kale, R. Traditional healers in South Africa: A parallel healthcare system. BMJ 1995, 310, 1182–1185. [Google Scholar] [CrossRef]
- Ahlberg, B.M. Integrated Health Care Systems and Indigenous Medicine: Reflections from the Sub-Sahara African Region. Front. Sociol. 2017, 2, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Blanchet, N.J.; Fink, G.; Osei-Akoto, I. The effect of Ghana’s national health insurance scheme on health care utilisation. Ghana Med. J. 2012, 46, 76–84. [Google Scholar] [PubMed]
- Dixon, J.; Tenkorang, E.Y.; Luginaah, I.N.; Kuuire, V.Z.; Boateng, G.O. National health insurance scheme enrolment and antenatal care among women in Ghana: Is there any relationship? Trop. Med. Int. Health 2014, 19, 98–106. [Google Scholar] [CrossRef] [Green Version]
- Singh, K.; Osei-Akoto, I.; Otchere, F.; Sodzi-Tettey, S.; Barrington, C.; Huang, C. Ghana’s National Health insurance scheme and maternal and child health: A mixed methods study. BMC Health Serv. Res. 2015, 15, 108. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Meeting Report: Meeting on the Contribution of Traditional Medicine in Strengthening Primary Healthcare; World Health Organization: Manila, Philippines, 2017; Contract No.: RS/2017/GE/58 (PHL). [Google Scholar]
- Meissner, O. The traditional healer as part of the primary healthcare team? S. Afr. Med. J. 2004, 94, 901–903. [Google Scholar] [PubMed]
- Wreford, J. Missing Each Other: Problems and Potential for Collaborative Efforts between Biomedicine and Traditional Healers in South Africa in the Time of AIDS. Soc. Dynam. 2005, 31, 55–89. [Google Scholar] [CrossRef]
- Tabi, M.M.; Powell, M.; Hodnicki, D. Use of traditional healers and modern medicine in Ghana. Int. Nurs. Rev. 2006, 53, 52–58. [Google Scholar] [CrossRef]
- Galabuzi, C.; Agea, J.; Fungo, B.; Kamoga, R. Traditional medicine as an alternative form of health care system: A preliminary case study of Nangabo sub-county, central Uganda. Afr. J. Trad. Complement. Altern. Med. 2010, 7, 11–16. [Google Scholar] [CrossRef] [Green Version]
- Mensah, C.M.; Gyasi, M.R. Use of herbal medicine in the management of malaria in the urban-periphery, Ghana. J. Biol. Agr. 2012, 2, 113–122. [Google Scholar]
- Krah, E.; de Kruijf, J.; Ragno, L. Integrating Traditional Healers into the Health Care System: Challenges and Opportunities in Rural Northern Ghana. J. Community Health 2018, 43, 157–163. [Google Scholar] [CrossRef] [Green Version]
- Campbell-Hall, V.; Petersen, I.; Bhana, A.; Mjadu, S.; Hosegood, V.; Flisher, A.J. Collaboration between traditional practitioners and primary health care staff in South Africa: Developing a workable partnership for community mental health services. Transcult. Psychiatry 2010, 47, 610–628. [Google Scholar] [CrossRef] [PubMed]
- Kayombo, E.J.; Uiso, F.C.; Mbwambo, Z.H.; Mahunnah, R.L.; Moshi, M.J.; Mgonda, Y.H. Experience of initiating collaboration of traditional healers in managing HIV and AIDS in Tanzania. J. Ethnobiol. Ethnomed. 2007, 3, 6. [Google Scholar] [CrossRef]
- King, R.; UNAIDS. Collaborating with Traditional Healers for HIV Prevention and Care. In Sub-Saharan Africa Suggestions for Programme Managers and Field Workers; Contract No.: UNAIDS/06.28E; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Ministry of Health. Creating Wealth Through Health: A New Paradigm for Ghana’s Development; Ministry of Health: Accra, Ghana, 2005; pp. 1–59. [Google Scholar]
- Ben-Arye, E.; Karkabi, S.; Shapira, C.; Schiff, E.; Lavie, O.; Keshet, Y. Complementary medicine in the primary care setting: Results of a survey of gender and cultural patterns in Israel. Gend. Med. 2009, 6, 384–397. [Google Scholar] [CrossRef] [PubMed]
- Pachter, L.M. Culture and clinical care. Folk illness beliefs and behaviors and their implications for health care delivery. JAMA 1994, 271, 690–694. [Google Scholar] [CrossRef] [PubMed]
- Awodele, O.; Agbaje, E.; Ogunkeye, F.; Kolapo, A.; Awodele, D. Towards integrating traditional medicine (TM) into National Health Care Scheme (NHCS): Assessment of TM practitioners’ disposition in Lagos, Nigeria. J. Herb. Med. 2011, 1, 90–94. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ampomah, I.G.; Malau-Aduli, B.S.; Seidu, A.-A.; Malau-Aduli, A.E.O.; Emeto, T.I. Perceptions and Experiences of Orthodox Health Practitioners and Hospital Administrators towards Integrating Traditional Medicine into the Ghanaian Health System. Int. J. Environ. Res. Public Health 2021, 18, 11200. https://doi.org/10.3390/ijerph182111200
Ampomah IG, Malau-Aduli BS, Seidu A-A, Malau-Aduli AEO, Emeto TI. Perceptions and Experiences of Orthodox Health Practitioners and Hospital Administrators towards Integrating Traditional Medicine into the Ghanaian Health System. International Journal of Environmental Research and Public Health. 2021; 18(21):11200. https://doi.org/10.3390/ijerph182111200
Chicago/Turabian StyleAmpomah, Irene G., Bunmi S. Malau-Aduli, Abdul-Aziz Seidu, Aduli E. O. Malau-Aduli, and Theophilus I. Emeto. 2021. "Perceptions and Experiences of Orthodox Health Practitioners and Hospital Administrators towards Integrating Traditional Medicine into the Ghanaian Health System" International Journal of Environmental Research and Public Health 18, no. 21: 11200. https://doi.org/10.3390/ijerph182111200
APA StyleAmpomah, I. G., Malau-Aduli, B. S., Seidu, A.-A., Malau-Aduli, A. E. O., & Emeto, T. I. (2021). Perceptions and Experiences of Orthodox Health Practitioners and Hospital Administrators towards Integrating Traditional Medicine into the Ghanaian Health System. International Journal of Environmental Research and Public Health, 18(21), 11200. https://doi.org/10.3390/ijerph182111200







