Predicting Psychosocial Health of Children and Adolescents with Obesity in Germany: The Underappreciated Role of Physical Fitness
Abstract
1. Introduction
2. Materials and Methods
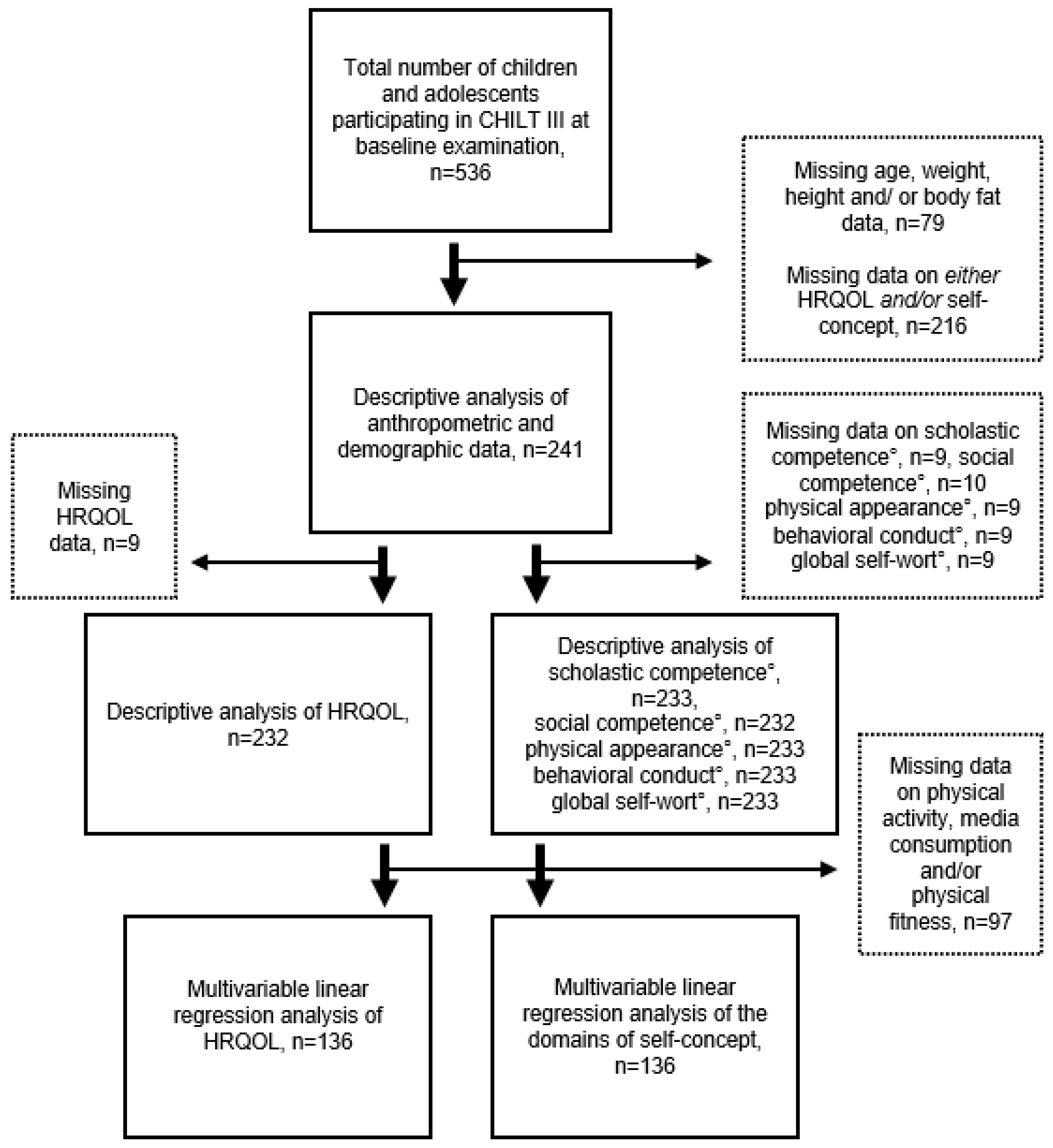
2.1. Sample Description
2.2. Anthropometric Data
2.3. Demographics and Lifestyle Patterns
2.4. Physical Fitness
2.5. Health-Related Quality of Life
2.6. Self-Concept
2.7. Statistical Analysis
3. Results
4. Discussion
4.1. Anthropometric and Demographic Determinants of Psychosocial Health of Children and Adolescents with Obesity
4.2. Associations between Physical Fitness, Physical Activity, and Psychosocial Health of Children and Adolescents with Obesity
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.-P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef]
- Rankin, J.; Matthews, L.; Cobley, S.; Han, A.; Sanders, R.; Wiltshire, H.D.; Baker, J.S. Psychological consequences of childhood obesity: Psychiatric comorbidity and prevention. Adolesc. Health Med. Ther. 2016, 7, 125–146. [Google Scholar] [CrossRef] [PubMed]
- Buttitta, M.; Rousseau, A.; Guerrien, A. A New Understanding of Quality of Life in Children and Adolescents with Obesity: Contribution of the Self-determination Theory. Curr. Obes. Rep. 2017, 6, 432–437. [Google Scholar] [CrossRef]
- Fonvig, C.E.; Hamann, S.A.; Nielsen, T.R.H.; Johansen, M.Ø.; Grønbæk, H.N.; Mollerup, P.M.; Holm, J.-C. Subjective evaluation of psychosocial well-being in children and youths with overweight or obesity: The impact of multidisciplinary obesity treatment. Qual. Life Res. 2017, 26, 3279–3288. [Google Scholar] [CrossRef]
- Sánchez-Miguel, P.A.; González, J.J.P.; Sánchez-Oliva, D.; Alonso, D.A.; Leo, F.M. The importance of body satisfaction to physical self-concept and body mass index in Spanish adolescents. Int. J. Psychol. 2019, 54, 521–529. [Google Scholar] [CrossRef]
- Sánchez-Miguel, P.A.; León-Guereño, P.; Tapia-Serrano, M.A.; Hortigüela-Alcalá, D.; López-Gajardo, M.A.; Vaquero-Solís, M. The Mediating Role of the Self-Concept between the Relationship of the Body Satisfaction and the Intention to Be Physically Active in Primary School Students. Front. Public Health 2020, 8, 113. [Google Scholar] [CrossRef]
- Wallander, J.L.; Taylor, W.C.; Grunbaum, J.A.; Franklin, F.A.; Harrison, G.G.; Kelder, S.H.; Schuster, M.A. Weight status, quality of life, and self-concept in African American, Hispanic, and white fifth-grade children. Obesity 2009, 17, 1363–1368. [Google Scholar] [CrossRef]
- Meixner, L.; Cohrdes, C.; Schienkiewitz, A.; Mensink, G.B.M. Health-related quality of life in children and adolescents with overweight and obesity: Results from the German KIGGS survey. BMC Public Health 2020, 20, 1722. [Google Scholar] [CrossRef]
- Buttitta, M.; Iliescu, C.; Rousseau, A.; Guerrien, A. Quality of life in overweight and obese children and adolescents: A literature review. Qual. Life Res. 2014, 23, 1117–1139. [Google Scholar] [CrossRef] [PubMed]
- Gow, M.L.; Tee, M.S.Y.; Garnett, S.P.; Baur, L.A.; Aldwell, K.; Thomas, S.; Lister, N.B.; Paxton, S.J.; Jebeile, H. Pediatric obesity treatment, self-esteem, and body image: A systematic review with meta-analysis. Pediatr. Obes. 2020, 15, e12600. [Google Scholar] [CrossRef] [PubMed]
- Perez-Sousa, M.A.; Olivares, P.R.; Garcia-Hermoso, A.; Gusi, N. Does anthropometric and fitness parameters mediate the effect of exercise on the HRQoL of overweight and obese children/adolescents? Qual. Life Res. 2018, 27, 2305–2312. [Google Scholar] [CrossRef]
- Reiss, F.; Meyrose, A.-K.; Otto, C.; Lampert, T.; Klasen, F.; Ravens-Sieberer, U. Socioeconomic status, stressful life situations and mental health problems in children and adolescents: Results of the German BELLA cohort-study. PLoS ONE 2019, 14, e0213700. [Google Scholar] [CrossRef]
- Cislak, A.; Safron, M.; Pratt, M.; Gaspar, T.; Luszczynska, A. Family-related predictors of body weight and weight-related behaviours among children and adolescents: A systematic umbrella review. Child Care Health Dev. 2012, 38, 321–331. [Google Scholar] [CrossRef]
- Poulsen, A.A.; Desha, L.; Ziviani, J.; Griffiths, L.; Heaslop, A.; Khan, A.; Leong, G.M. Fundamental movement skills and self-concept of children who are overweight. Int. J. Pediatr. Obes. 2011, 6, e464–e471. [Google Scholar] [CrossRef]
- Eddolls, W.T.B.; McNarry, M.A.; Lester, L.; Winn, C.O.N.; Stratton, G.; Mackintosh, K.A. The association between physical activity, fitness and body mass index on mental well-being and quality of life in adolescents. Qual. Life Res. 2018, 27, 2313–2320. [Google Scholar] [CrossRef] [PubMed]
- Barnett, T.A.; Contreras, G.; Ghenadenik, A.E.; Zawaly, K.; van Hulst, A.; Mathieu, M.-È.; Henderson, M. Identifying risk profiles for excess sedentary behaviour in youth using individual, family and neighbourhood characteristics. Prev. Med. Rep. 2021, 24, 101535. [Google Scholar] [CrossRef]
- Rodriguez-Ayllon, M.; Cadenas-Sanchez, C.; Esteban-Cornejo, I.; Migueles, J.H.; Mora-Gonzalez, J.; Henriksson, P.; Martín-Matillas, M.; Mena-Molina, A.; Molina-García, P.; Estévez-López, F.; et al. Physical fitness and psychological health in overweight/obese children: A cross-sectional study from the ActiveBrains project. J. Sci. Med. Sport 2018, 21, 179–184. [Google Scholar] [CrossRef]
- Vedul-Kjelsås, V.; Sigmundsson, H.; Stensdotter, A.-K.; Haga, M. The relationship between motor competence, physical fitness and self-perception in children. Child Care Health Dev. 2012, 38, 394–402. [Google Scholar] [CrossRef]
- Evaristo, O.S.; Moreira, C.; Lopes, L.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Oliveira, A.; Mota, J.; Santos, R. Cardiorespiratory fitness and health-related quality of life in adolescents: A longitudinal analysis from the LabMed Physical Activity Study. Am. J. Hum. Biol. 2019, 31, e23304. [Google Scholar] [CrossRef]
- Bermejo-Cantarero, A.; Álvarez-Bueno, C.; Martínez-Vizcaino, V.; Redondo-Tébar, A.; Pozuelo-Carrascosa, D.P.; Sánchez-López, M. Relationship between both cardiorespiratory and muscular fitness and health-related quality of life in children and adolescents: A systematic review and meta-analysis of observational studies. Health Qual. Life Outcomes 2021, 19, 127. [Google Scholar] [CrossRef]
- Mitchell, N.G.; Moore, J.B.; Bibeau, W.S.; Rudasill, K.M. Cardiovascular fitness moderates the relations between estimates of obesity and physical self-perceptions in rural elementary school students. J. Phys. Act. Health 2012, 9, 288–294. [Google Scholar] [CrossRef][Green Version]
- Babic, M.J.; Morgan, P.J.; Plotnikoff, R.C.; Lonsdale, C.; White, R.L.; Lubans, D.R. Physical activity and physical self-concept in youth: Systematic review and meta-analysis. Sports Med. 2014, 44, 1589–1601. [Google Scholar] [CrossRef]
- Perez-Sousa, M.A.; Olivares, P.R.; Escobar-Alvarez, J.A.; Parraça, J.A.; Gusi, N. Fitness as mediator between weight status and dimensions of health-related quality of life. Health Qual. Life Outcomes 2018, 16, 155. [Google Scholar] [CrossRef]
- Marques, A.; Mota, J.; Gaspar, T.; de Matos, M.G. Associations between self-reported fitness and self-rated health, life-satisfaction and health-related quality of life among adolescents. J. Exerc. Sci. Fit. 2017, 15, 8–11. [Google Scholar] [CrossRef]
- Lier, L.M.; Breuer, C.; Ferrari, N.; Friesen, D.; Maisonave, F.; Schmidt, N.; Graf, C. Individual Physical Activity Behaviour and Group Composition as Determinants of the Effectiveness of a Childhood Obesity Intervention Program. Obes. Facts 2021, 14, 100–107. [Google Scholar] [CrossRef]
- Kromeyer-Hauschild, K.; Wabitsch, M.; Kunze, D.; Geller, F.; Geiß, H.C.; Hesse, V.; von Hippel, A.; Jaeger, U.; Johnsen, D.; Korte, W.; et al. Perzentile für den Body-mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Mon. Kinderheilkd. 2001, 149, 807–818. [Google Scholar] [CrossRef]
- Lohman, T.G.; Roche, A.F.; Martorell, R. Anthropometric Standardization Reference Manual; Human Kinetics Books: Champaign, IL, USA, 1988; ISBN 9780873221214. [Google Scholar]
- Slaughter, M.H.; Lohman, T.G.; Boileau, R.; Horswill, C.A.; Stillman, R.J.; Van Loan, M.D.; Bemben, D.A. Skinfold equations for estimation of body fatness in children and youth. Hum. Biol. 1988, 60, 709–723. [Google Scholar]
- Chan, D.F.Y.; Li, A.M.; So, H.K.; Yin, J.; Nelson, E.A.S. New Skinfold-thickness Equation for Predicting Percentage Body Fat in Chinese Obese Children. Hong Kong J. Paediatr. 2008, 14, 96–102. [Google Scholar]
- Rodríguez, G.; Moreno, L.A.; Blay, M.G.; Blay, V.A.; Fleta, J.; Sarría, A.; Bueno, M. Body fat measurement in adolescents: Comparison of skinfold thickness equations with dual-energy X-ray absorptiometry. Eur. J. Clin. Nutr. 2005, 59, 1158–1166. [Google Scholar] [CrossRef]
- Wu, X.Y.; Han, L.H.; Zhang, J.H.; Luo, S.; Hu, J.W.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, e0187668. [Google Scholar] [CrossRef]
- Plachta-Danielzik, S.; Müller, M.J. Socio-Economic Aspects. In Metabolic Syndrome and Obesity in Childhood and Adolescence; Kiess, W., Wabitsch, M., Maffeis, C., Sharma, A.M., Eds.; S. KARGER AG: Basel, Switzerland, 2015; pp. 68–74. ISBN 978-3-318-02798-3. [Google Scholar]
- Bau, A.-M.; Sannemann, J.; Ernert, A.; Babitsch, B. Einflussfaktoren auf die gesundheitsbezogene Lebensqualität von 10- bis 15-jährigen Mädchen in Berlin. Gesundheitswesen 2011, 73, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Warschburger, P.; Fromme, C.; Petermann, F. Konzeption und Analyse eines gewichtsspezifischen Lebensqualitätsfragebogens für übergewichtige und adipöse Kinder und Jugendliche (GW-LQ-KJ). Z. Klin. Psychol. Psychiatr. Psychother. 2005, 4, 356–369. [Google Scholar]
- Wünsche, P.; Schneewind, K.A. Entwicklung eines Fragebogens zur Erfassung von Selbst- und Kompetenzeinschätzungen bei Kindern (FSK-K). Diagnostica 1989, 35, 217–235. [Google Scholar]
- Reinehr, T.; Kersting, M.; Wollenhaupt, A.; Alexy, U.; Kling, B.; Ströbele, K.; Andler, W. Evaluation der Schulung "OBELDICKS" für adipöse Kinder und Jugendliche. Klin. Padiatr. 2005, 217, 1–8. [Google Scholar] [CrossRef]
- Harrist, A.W.; Swindle, T.M.; Hubbs-Tait, L.; Topham, G.L.; Shriver, L.H.; Page, M.C. The Social and Emotional Lives of Overweight, Obese, and Severely Obese Children. Child Dev. 2016, 87, 1564–1580. [Google Scholar] [CrossRef] [PubMed]
| Variable | n (%) | Mean (SD) | Min | Max | |
|---|---|---|---|---|---|
| Sex | Female | 125 (51.9%) | |||
| Male | 116 (48.1%) | ||||
| Percentile | Obese | 212 (88.0%) | |||
| Overweight | 29 (12.0%) | ||||
| Migration Background | Yes/German | 209 (86.7%) | |||
| No/Non-German | 32 (13.3%) | ||||
| Parent’s Educational Degree 1 | High | 57 (23.7%) | |||
| Low | 184 (76.3%) | ||||
| Physical Variables | Age (years) | 241 | 12.5 (2.07) | 7.3 | 17.1 |
| Height (m) | 241 | 1.58 (0.11) | 1.23 | 1.89 | |
| Weight (kg) | 241 | 76.7 (19.9) | 37.4 | 148.4 | |
| BMI (kg/m2) | 241 | 30.9 (4.8) | 20.5 | 56.6 | |
| BMI Z-score | 241 | 2.45 (0.46) | 1.43 | 3.80 | |
| Body fat (%) | 241 | 42.1 (9.0) | 26.1 | 83.2 | |
| Relative Physical fitness (W/kg) | 241 | 1.7 (0.4) | 0.9 | 3.3 | |
| Lifestyle Variables | Physical Activity (hours/day) | 162 | 0.7 (0.6) | 0 | 2.9 |
| Media Consumption (hours/day) | 190 | 2.5 (1.8) | 0 | 8.5 | |
| Psychosocial Variables | HRQOL | 232 | 77.7 (14.3) | 29.1 | 100.0 |
| Scholastic Competence ° | 233 | 75.6 (16.7) | 25.0 | 100.0 | |
| Social Competence ° | 232 | 76.0 (18.6) | 25.0 | 100.0 | |
| Physical Appearance ° | 233 | 54.1 (15.6) | 25.0 | 100.0 | |
| Behavioral Conduct ° | 232 | 74.1 (16.4) | 29.2 | 100.0 | |
| Global Self-Worth ° | 233 | 72.3 (16.3) | 25.0 | 100.0 |
| Model | Final Predictor/s * | β (s.e.) | p-Value of Coefficient | R2 | Adj. R2 (p-Value of Final Model) |
|---|---|---|---|---|---|
| HRQOL (n = 136) | Relative Physical fitness (W/kg) | 0.216 (3.128) | 0.011 | 0.047 | 0.040 (0.011) |
| Scholastic Competence ° (n = 136) | Relative Physical fitness (W/kg) | 0.228 (3.289) | 0.008 | 0.052 | 0.045 (0.008) |
| Social Competence ° (n = 136) | Relative Physical fitness (W/kg) | 0.197 (3.786) | 0.023 | 0.038 | 0.031 (0.023) |
| Physical Appearance ° (n = 136) | Age (years) BMI Z-score Physical Activity (hours/week) | −0.276 (0.641) −0.334 (2.726) −0.164 (0.301) | 0.001 <0.001 0.040 | 0.190 | 0.171 (<0.001) |
| Behavioral Conduct ° (n = 136) | High Parental Educational Level a German/No Migration Background b | 0.204 (2.942) 0.169 (4.442) | 0.016 0.045 | 0.071 | 0.057 (0.008) |
| Global Self-Worth ° (n = 136) | Age (years) High Parental Educational Level a | −0.186 (0.719) 0.224 (3.005) | 0.028 0.008 | 0.077 | 0.063 (0.005) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eisenburger, N.; Friesen, D.; Haas, F.; Klaudius, M.; Schmidt, L.; Vandeven, S.; Joisten, C. Predicting Psychosocial Health of Children and Adolescents with Obesity in Germany: The Underappreciated Role of Physical Fitness. Int. J. Environ. Res. Public Health 2021, 18, 11188. https://doi.org/10.3390/ijerph182111188
Eisenburger N, Friesen D, Haas F, Klaudius M, Schmidt L, Vandeven S, Joisten C. Predicting Psychosocial Health of Children and Adolescents with Obesity in Germany: The Underappreciated Role of Physical Fitness. International Journal of Environmental Research and Public Health. 2021; 18(21):11188. https://doi.org/10.3390/ijerph182111188
Chicago/Turabian StyleEisenburger, Nina, David Friesen, Fabiola Haas, Marlen Klaudius, Lisa Schmidt, Susanne Vandeven, and Christine Joisten. 2021. "Predicting Psychosocial Health of Children and Adolescents with Obesity in Germany: The Underappreciated Role of Physical Fitness" International Journal of Environmental Research and Public Health 18, no. 21: 11188. https://doi.org/10.3390/ijerph182111188
APA StyleEisenburger, N., Friesen, D., Haas, F., Klaudius, M., Schmidt, L., Vandeven, S., & Joisten, C. (2021). Predicting Psychosocial Health of Children and Adolescents with Obesity in Germany: The Underappreciated Role of Physical Fitness. International Journal of Environmental Research and Public Health, 18(21), 11188. https://doi.org/10.3390/ijerph182111188






