Design and Validation of the INCUE Questionnaire: Assessment of Primary Healthcare Nurses’ Basic Training Needs in Palliative Care
Abstract
1. Introduction
2. Materials and Methods
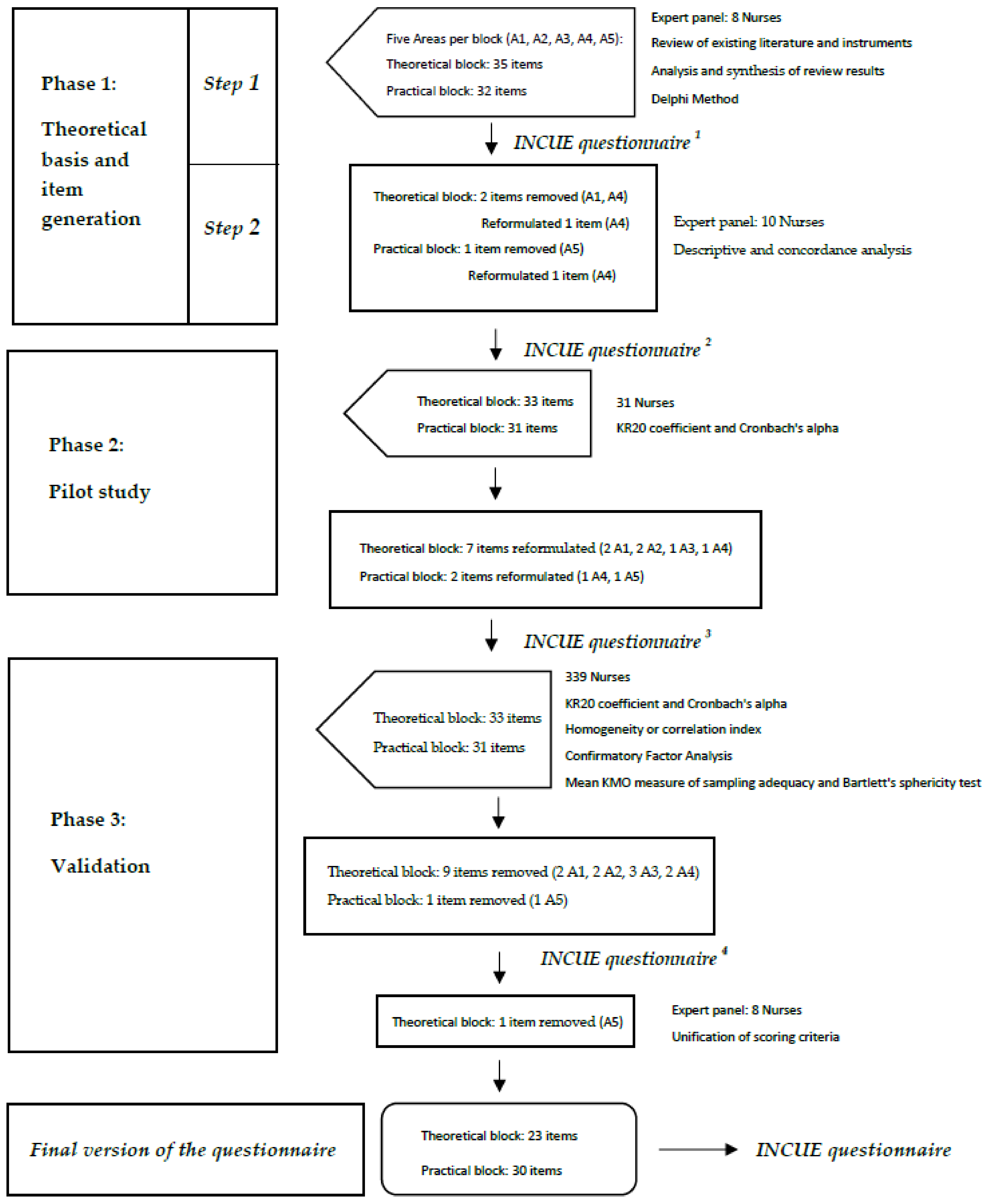
2.1. Phase 1: Theoretical Basis and Generation of Items
2.2. Phase 2: Pilot Study
2.3. Phase 3: Validation
2.4. Sample and Data Collection
2.5. Ethical Considerations
3. Results
3.1. Phase 1: Theoretical Basis and Generation of Items
3.1.1. Step 1
3.1.2. Step 2
3.2. Phase 2: Pilot Study
3.3. Phase 3: Validation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- OMS. Cuidados Paliativos. Available online: https://www.who.int/cancer/palliative/es/ (accessed on 18 April 2021).
- Sepúlveda, C.; Marlin, A.; Yoshida, T.; Ullrich, A. Palliative care. J. Pain Symptom Manage. 2002, 24, 91–96. [Google Scholar] [CrossRef]
- Better Palliative Care for Older People. Available online: https://apps.who.int/iris/handle/10665/107563 (accessed on 15 April 2021).
- Ministerio de Sanidad Política Social e Igualdad. Estrategia en Cuidados Paliativos del Sistema Nacional de Salud. Available online: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/docs/paliativos/cuidadospaliativos.pdf (accessed on 15 April 2021).
- González López-Valcárcel, B. Formación y Empleo de Profesionales Sanitarios en España. Un Análisis de Desequilibrios. Gac Sanit. 2000, 14, 237–246. [Google Scholar] [CrossRef]
- Gómez Batiste-Alentorn, X.; Amblás-Novellas, J.; Lasmarías Martínez, C.; Calsina-Berna, A. Manual de Atención Integral de Personas con Enfermedades Crónicas Avanzadas: Aspectos Clínicos, 1st ed.; Elsevier: Barcelona, Spain, 2017. [Google Scholar]
- Deravin Malone, L.; Anderson, J.; Croxon, L. Are newly graduated nurses ready to deal with death and dying? A literature review. Nurs Palliat Care. 2016, 1, 89–93. [Google Scholar] [CrossRef][Green Version]
- Mallory, J.L. The impact of a palliative care educational component on attitudes toward care of the dying in undergraduate nursing students. J. Prof. Nurs. 2003, 19, 305–312. [Google Scholar] [CrossRef]
- Kwekkeboom, K.L.; Vahl, C.; Eland, J. Companionship and education: A nursing student experience in palliative care. J. Nurs Educ. 2005, 44, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Mutto, E.M.; Errázquin, A.; Rabhansl, M.M.; Villar, M.J. Nursing education: The experience, attitudes, and impact of caring for dying patients by undergraduate Argentinian nursing students. J. Palliat. Med. 2010, 13, 1445–1450. [Google Scholar] [CrossRef] [PubMed]
- White, K.R.; Coyne, P.J. Nurses’ perceptions of educational gaps in delivering end-of-life care. Oncol. Nurs. Forum. 2011, 38, 711–717. [Google Scholar] [CrossRef] [PubMed]
- Prem, V.; Karvannan, H.; Kumar, S.P.; Karthikbabu, S.; Syed, N.; Sisodia, V.; Saroja, J. Study of nurses’ knowledge about palliative care: A quantitative cross-sectional survey. Indian J. Palliat Care. 2012, 18, 122–127. [Google Scholar] [PubMed]
- Marchán Espinosa, S. Afrontamiento del profesional de enfermería ante la muerte de pacientes en unidades de paliativos y oncología. Nure Investig. Rev. Científica De Enfermería 2016, 13, 1–12. [Google Scholar]
- Jors, K.; Seibel, K.; Bardenheuer, H.; Buchheidt, D.; Mayer-Steinacker, R.; Viehrig, M.; Xander, C.; Becker, G. Education in end-of-life care: What do experienced professionals find important? J. Cancer Educ. 2016, 31, 272–278. [Google Scholar] [CrossRef]
- De Vlieger, M.; Gorchs, N.; Larkin, P.; Porchet, F. Palliative nurse education: Towards a common language. Palliat. Med. 2004, 18, 401–403. [Google Scholar] [CrossRef] [PubMed]
- Codorniú, N.; Guanter, L.; Utor, L. Competencias Enfermeras en Cuidados Paliativos, 1st ed.; SECPAL: Madrid, Spain, 2013. [Google Scholar]
- Ross, M.M.; McDonald, B.; McGuinness, J. The palliative care quiz for nursing (PCQN): The development of an instrument to measure nurses’ knowledge of palliative care. J. Adv. Nurs. 1996, 23, 126–137. [Google Scholar] [CrossRef]
- Bransford, J.D.; Schwartz, D.L. Rethinking transfer: A simple proposal with multiple implications. Rev. Res. Educ. 1999, 24, 61. [Google Scholar]
- Feíto Grande, L. Ética y Enfermería; Universidad Pontifica de Comillas: Madrid, Spain, 2009; pp. 203–205. [Google Scholar]
- García Salvador, I. Capacitación Y Necesidades Formativas Básicas En Cuidados Paliativos De Enfermería En Hospital De Agudos; XI Jornadas SECPAL: Valencia, Spain, 2015. [Google Scholar]
- Lester, D. The collett-lester fear of death scale: The original version and a revision. Death Stud. 1990, 14, 451–468. [Google Scholar] [CrossRef]
- Bugen, L.A. Coping: Effects of death education. Omega 1981, 11, 175–183. [Google Scholar] [CrossRef]
- Río-Valle, J.S. Validación De La Versión Española De La Escala De Afrontamiento De La Muerte Y Del Perfil Revisado De Actitudes Hacia La Muerte: Estudio Comparativo Y Transcultural. Puesta En Marcha De Un Programa De Intervención. Ph.D. Thesis, Universidad de Granada, Granada, Spain, 2007. [Google Scholar]
- Sullivan, A.M.; Lakoma, M.D.; Block, S.D. The status of medical education in end-of-life care: A national report. J. Gen. Intern. Med. 2003, 18, 685–695. [Google Scholar] [CrossRef]
- Bermejo, J.C.; Villacieros, M.; Hassoun, H. Actitudes hacia el cuidado de pacientes al final de la vida y miedo a la muerte en una muestra de estudiantes sociosanitarios. Med. Pal. 2018, 25, 168–174. [Google Scholar] [CrossRef]
- Abu Hasheesh, M.O.; Al-Sayed AboZeid, S.; Goda El-Zaid, S.; Alhujaili, A.D. Nurses’ characteristics and their attitudes toward death and caring for dying patients in a public hospital in Jordan. Health Sci, J. 2013, 7, 384–394. [Google Scholar]
- Frommelt, K.H.M. Attitudes toward care of the terminally ill: An educational intervention. Am. J. Hosp. Palliat. Care 2003, 20, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Kain, V.J. Pilot study of an instrument to measure attitudes to palliative care practice in neonatal intensive care nursing. Collegian 2007, 14, 16–20. [Google Scholar] [CrossRef]
- Ascencio Huertas, L. Adaptación en español de la escala de actitudes ante cuidados paliativos: Confiabilidad y análisis factorial. Psicooncologia 2016, 12, 367. [Google Scholar] [CrossRef]
- Mason, S.; Ellershaw, J. Assessing undergraduate palliative care education: Validity and reliability of two scales examining perceived efficacy and outcome expectancies in palliative care. Med. Educ. 2004, 38, 1103–1110. [Google Scholar] [CrossRef]
- Herrero-Hahn, R.; Montoya-Juárez, R.; Hueso-Montoro, C.; Martí-García, C.; Salazar-Blandón, D.A.; García-Caro, M.P. Cultural adaptation, validation, and analysis of the self-efficacy in Palliative Care Scale for use with Spanish nurses. Int. J. Environ. Res. Public Health. 2019, 16, 4840. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.H.; Yang, S.K.; Park, M.H.; Choe, S.O. Assessment for the needs to develop hospice training program for nurses. Korean J. Hosp. Palliat Care. 2008, 11, 147–155. [Google Scholar]
- Nakazawa, Y.; Miyashita, M.; Morita, T.; Ueda, M.; Oyagi, Y.; Ogasawara, T. The palliative care knowledge test: Reliability and validity of an instrument to measure palliative care knowledge among health professionals. Palliat Med. 2009, 23, 754–766. [Google Scholar] [CrossRef]
- Guevara-Valtier, M.C.; Santos-Flores, J.M.; Santos-Flores, I.; Valdez-Ramírez, F.J.; Garza-Dimas, I.Y.; Paz-Morales, M.A.; Gutiérrez-Valver, J.M. Conocimiento de enfermería sobre cuidados paliativos en centros de primer y segundo nivel de atención para la salud. Rev. CONAMED. 2017, 22, 170–173. [Google Scholar]
- Al-Ansari, A.M.; Suroor, S.N.; AboSerea, S.M.; Abd-El-Gawad, W.M. Development of palliative care attitude and knowledge (PCAK) questionnaire for physicians in Kuwait. BMC Palliat Care. 2019, 18, 49. [Google Scholar] [CrossRef]
- Karacsony, S.; Good, A.; Chang, E.; Johnson, A.; Edenborough, M. An instrument to assess the education needs of nursing assistants within a palliative approach in residential aged care facilities. BMC Palliat Care. 2019, 18, 61. [Google Scholar] [CrossRef]
- Chover-Sierra, E.; Martínez-Sabater, A.; Lapeña-Moñux, Y.R. An instrument to measure nurses’ knowledge in palliative care: Validation of the Spanish version of Palliative Care Quiz for Nurses. PLoS ONE 2017, 12, e0177000. [Google Scholar]
- Franco Pujante, L. Adaptación Transcultural Y Validación De La Versión Española De La Escala Rotterdam MOVE2PC Para Enfermeras. Master’s Final Project. Universitat de Valencia, Valencia, Spain. 2017. Available online: http://www.cuidarypaliar.es/wp-content/uploads/2016/12/TFM-con-portada.pdf (accessed on 13 January 2020).
- Batista-Foguet, J.M.; Coenders, G.; Alonso, J. Análisis factorial confirmatorio. Su utilidad en la validación de cuestionarios relacionados con la salud. Med. Clin. 2004, 122, 21–27. [Google Scholar] [CrossRef]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales, 5th ed; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Álvarez, R.R. Elaboración Y Validación De Un Cuestionario Multimedia Y Multilingüe De Evaluación De La Autoestima; Granada Editorial Universidad de Granada: Granada, Spain, 2008. [Google Scholar]
- Escobar-Pérez, J.; Martínez, A. Validez de contenido y juicio de expertos: Una aproximación a su utilización. Avances en Medición 2008, 6, 27–36. [Google Scholar]
- García Salvador, I.; Vallés Martínez, P.; Guanter Peris, L.; Utor Ponce, L.; Pérez Yuste, P.; López-Casero Beltrán, N.; Alonso, V.R.; Monfort, P.C.; Sierra, E.C.; Plaza, T.E.; et al. Recommendations About Training in Palliative Care in Nursing Degree Of The Spanish Palliative Care Nurses Association, 1st ed.; Inspira Network: Madrid, Spain, 2019; Volume 1, pp. 273–280. [Google Scholar]
- Bakieva, M. Diseño Y Validación De Un Instrumento Para Evaluar La Colegialidad Docente. Ph.D., Universitat de Valencia. Available online: https://www.uv.es/gem/gemeduco/publicaciones/Disenyo_y_validacion_de_un_instrumento_para_evaluar_la_colegialidad_docente_Tesis_doctoral.pdf (accessed on 3 March 2020).
- Nunnally, J.C. McGraw-Hill Series in Psychology. In Psychometric Theory, 2nd ed.; Mcgraw-Hill College: New York, NY, USA, 1978; pp. 9–17. [Google Scholar]
- Revelle, W.R. Psych: Procedures for Personality and Psychological Research. Available online: https://www.scholars.northwestern.edu/en/publications/psych-procedures-for-personality-and-psychological-research (accessed on 18 April 2021).
- Rosseel, Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. Available online: https://www.jstatsoft.org/article/view/v048i02 (accessed on 6 March 2020). [CrossRef]
- Barbero García, M.I.; Vila Abad, E.; Suárez Falcón, J.C. Psicometria, 2nd ed.; Universidad Nacional de Educación a Distancia: Madrid, Spain, 2006. [Google Scholar]
- Bartlett, M.S. Tests of significance in factor analysis. Br. J. Stat. Psychol. 1950, 3, 77–85. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Martínez-Arias, R. Psicometría: Teoría De Los Test Psicológicos Y Educativos; Síntesis: Madrid, Spain, 1995. [Google Scholar]
- Comrey, A.L.; Lee, H.B. A First Course in Factor Analysis, 2nd ed.; Lawrence Erlbaum: Hillsdale, NJ, USA, 1992. [Google Scholar]
- Snook, S.C.Y.; Gorsuch, R.L. Component analysis versus common factor analysis: A Monte Carlo study. Psychol. Bull. 1989, 106, 148–154. [Google Scholar] [CrossRef]
- Stevens, J. Applied Multivariate Statistics for The Social Sciences; Lawrence Erlbaum: Hillsdale, NJ, USA, 1992. [Google Scholar]
- DeVon, H.A.; Block, M.E.; Moyle-Wright, P.; Ernst, D.M.; Hayden, S.J.; Lazzara, D.J.; Kostas-Polston, E. A psychometric toolbox for testing validity and reliability. J. Nurs. Scholarsh. 2007, 39, 55–164. [Google Scholar] [CrossRef] [PubMed]
- De la Rica Escuín, M.; García-Navarro, E.B.; García Salvador, I.; De la Ossa Sendra, M.J.; Chisbert-Alapont, E. Acompañamiento a los pacientes al final de la vida durante la pandemia COVID-19. Med. Pal. 2020, 27, 181–191. Available online: https://www.medicinapaliativa.es/Acompanamiento-a-los-pacientes-al-final-de-la-vida-durante-la-pandemia-por-COVID-19534 (accessed on 14 November 2020).
- Rojas-Ocaña, M.J.; Araujo-Hernández, M.; Romero-Castillo, R.; Román-Mata, S.S.; García-Navarro, E.B. Nursing as a Sustainability Factor of the Health System during the COVID-19 Pandemic: A Qualitative Study. Sustainability 2020, 12, 8099. [Google Scholar] [CrossRef]
- Yu, H.; Huang, C.; Chin, Y.; Shen, Y.; Chiang, Y.; Chang, C.; Lou, J. The Mediating Effects of Nursing Professional Commitment on the Relationship between Social Support, Resilience, and Intention to Stay among Newly Graduated Male Nurses: A Cross-Sectional Questionnaire Survey. Int. J. Environ. Res. Public Health 2021, 18, 7546. [Google Scholar] [CrossRef]
- Lynn, M.R. Determination and quantification of content validity. Nurs. Res. 1986, 35, 382–385. [Google Scholar] [CrossRef]
- Hyrkäs, K.; Appelqvist-Schmidlechner, K.; Oksa, L. Validating an instrument for clinical super-vision using an expert panel. Int. J. Nurs. Stud. 2003, 40, 619–625. [Google Scholar] [CrossRef]
| Areas | Part 1: Theoretical Knowledge Theoretical Block (n = 35) | Part 2: Practical Application Practical Block (n = 32) | ||
|---|---|---|---|---|
| Number of Items | Response Type | Number of Items | Response Type | |
| 1. Principles of PC | 7 | Yes | 6 | Never |
| 2. Symptom management and specific care plans | 7 | 6 | Rarely | |
| 3. Coping with loss and death | 8 | No | 6 | Sometimes |
| 4. Communication skills | 7 | 6 | Often | |
| 5. Ethical and legal aspects | 6 | Do not know/no answer | 8 | Always |
| Variable | Expert Panel 1 (n = 8) | Expert Panel 2 (n = 10) | Pilot Phase (n = 31) | Validation Phase (n = 339) |
|---|---|---|---|---|
| Age (years), M ± SD | 49.6 ± 1.3 | 45.7 ± 12 | 41.8 ± 12 | 45.5 ± 11.2 |
| Gender, n (%) | ||||
| Female | 7 (75) | 9 (90) | 27 (87.1) | 280 (82.6) |
| Male | 1 (25) | 1 (10) | 4 (12.9) | 59 (17.4) |
| Maximum level of professional qualification | ||||
| Doctorate | 2 (25) | 2 (20) | 1 (3.2) | 17 (5) |
| Nursing Specialization | 0 (0) | 0 (0) | 2 (6.5) | 53 (15.6) |
| Master degree | 6 (75) | 8 (80) | 5 (16.1) | 88 (26) |
| Diploma/Graduate | 0 (0) | 0 (0) | 23 (74.2) | 181 (53.4) |
| Current position | ||||
| Reference Nurse in Palliative Care | 0 (0) | 10 (100) | 1 (3.2) | 45 (13.3) |
| Nurse and Center Coordinator | 0 (0) | 0 (0) | 2 (6.5) | 0 (0) |
| Nurse | 8 (100) | 0 (0) | 27 (87.1) | 208 (61.4) |
| Center Coordinator | 0 (0) | 0 (0) | 1 (3.2) | 33 (9.7) |
| Community case manager | 0 (0) | 0 (0) | 0 (0) | 53 (15.6) |
| Professional experience (years), M ± SD | 29.2 ± 2.2 | 20.7 ± 6.5 | 13.7 ± 9.18 | 21 ± 11.7 |
| Palliative-care training | ||||
| Yes | 8 (100) | 10 (100) | 25 (80.6) | 292 (86.1) |
| No | 0 (0) | 0 (0) | 6 (19.4) | 47 (13.9) |
| Level of training in PC | ||||
| Advanced (Master or PhD) | 8 (100) | 10 (100) | 0 (0) | 51 (15.0) |
| Intermediate (80–150 h) | 0 (0) | 0 (0) | 10 (32.2) | 92 (27.2) |
| Basic (25–80 h) | 0 (0) | 0 (0) | 15 (48.4) | 154 (45.4) |
| Don’t know/No answer | 0 (0) | 0 (0) | 6 (19.4) | 42 (12.4) |
| Theoretical Block (without the Questions 3, 6, 7, 11, 14, 16, 19, 22, 27 and 28) | Practical Block (without Question 62) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Item | Factor Weight | Item-Total Correlation | KR20 on Omitting the Question | KR20 Index | Item | Factor Weight | Item-Total Correlation | Cronbach’s Alpha on Omitting the Question | Cronbach’s Alpha |
| 1 | 0.56 | 0.109 | 0.700 | 0.700 | 34 | 0.69 | 0.415 | 0.941 | 0.941 |
| 2 | 0.64 | 0.242 | 0.693 | 35 | 0.76 | 0.758 | 0.938 | ||
| 4 | 0.43 | 0.263 | 0.690 | 36 | 0.80 | 0.706 | 0.939 | ||
| 5 | 0.52 | 0.255 | 0.692 | 37 | 0.71 | 0.635 | 0.939 | ||
| 8 | 0.75 | 0.432 | 0.677 | 38 | 0.69 | 0.650 | 0.939 | ||
| 9 | 0.37 | 0.206 | 0.695 | 39 | 0.68 | 0.547 | 0.940 | ||
| 10 | 0.24 | 0.119 | 0.705 | 40 | 0.74 | 0.689 | 0.938 | ||
| 12 | 0.55 | 0.348 | 0.681 | 41 | 0.61 | 0.653 | 0.939 | ||
| 13 | 0.57 | 0.290 | 0.688 | 42 | 0.60 | 0.695 | 0.938 | ||
| 15 | 0.75 | 0.171 | 0.698 | 43 | 0.49 | 0.395 | 0.942 | ||
| 17 | 0.44 | 0.304 | 0.686 | 44 | 0.81 | 0.681 | 0.938 | ||
| 18 | 0.68 | 0.339 | 0.686 | 45 | 0.65 | 0.701 | 0.938 | ||
| 20 | 0.39 | 0.148 | 0.703 | 46 | 0.83 | 0.776 | 0.937 | ||
| 21 | 0.77 | 0.357 | 0.680 | 47 | 0.84 | 0.660 | 0.939 | ||
| 23 | 0.46 | 0.162 | 0.697 | 48 | 0.66 | 0.649 | 0.939 | ||
| 24 | 0.2 | 0.212 | 0.697 | 49 | 0.73 | 0.658 | 0.939 | ||
| 25 | 0.54 | 0.272 | 0.689 | 50 | 0.64 | 0.672 | 0.938 | ||
| 26 | 0.48 | 0.384 | 0.678 | 51 | 0.52 | 0.579 | 0.940 | ||
| 29 | 0.62 | 0.213 | 0.695 | 52 | 0.36 | 0.568 | 0.940 | ||
| 30 | 0.46 | 0.223 | 0.694 | 53 | 0.68 | 0.460 | 0.942 | ||
| 31 | 0.45 | 0.218 | 0.694 | 54 | 0.69 | 0.680 | 0.939 | ||
| 32 | 0.47 | 0.339 | 0.683 | 55 | 0.76 | 0.577 | 0.940 | ||
| 33 | 0.45 | 0.351 | 0.681 | 56 | 0.80 | 0.740 | 0.938 | ||
| 57 | 0.71 | 0.782 | 0.938 | ||||||
| 58 | 0.69 | 0.557 | 0.940 | ||||||
| 59 | 0.68 | 0.663 | 0.939 | ||||||
| 60 | 0.74 | 0.629 | 0.939 | ||||||
| 61 | 0.61 | 0.429 | 0.941 | ||||||
| 63 | 0.60 | 0.356 | 0.942 | ||||||
| 64 | 0.49 | 0.605 | 0.940 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Salvador, I.; Chisbert-Alapont, E.; Antonaya Campos, A.; Casaña Mohedo, J.; Hurtado Navarro, C.; Fernández Peris, S.; Bonías López, J.; De la Rica Escuín, M.L. Design and Validation of the INCUE Questionnaire: Assessment of Primary Healthcare Nurses’ Basic Training Needs in Palliative Care. Int. J. Environ. Res. Public Health 2021, 18, 10995. https://doi.org/10.3390/ijerph182010995
García-Salvador I, Chisbert-Alapont E, Antonaya Campos A, Casaña Mohedo J, Hurtado Navarro C, Fernández Peris S, Bonías López J, De la Rica Escuín ML. Design and Validation of the INCUE Questionnaire: Assessment of Primary Healthcare Nurses’ Basic Training Needs in Palliative Care. International Journal of Environmental Research and Public Health. 2021; 18(20):10995. https://doi.org/10.3390/ijerph182010995
Chicago/Turabian StyleGarcía-Salvador, Isidro, Encarna Chisbert-Alapont, Amparo Antonaya Campos, Jorge Casaña Mohedo, Clara Hurtado Navarro, Silvia Fernández Peris, José Bonías López, and Maria Luisa De la Rica Escuín. 2021. "Design and Validation of the INCUE Questionnaire: Assessment of Primary Healthcare Nurses’ Basic Training Needs in Palliative Care" International Journal of Environmental Research and Public Health 18, no. 20: 10995. https://doi.org/10.3390/ijerph182010995
APA StyleGarcía-Salvador, I., Chisbert-Alapont, E., Antonaya Campos, A., Casaña Mohedo, J., Hurtado Navarro, C., Fernández Peris, S., Bonías López, J., & De la Rica Escuín, M. L. (2021). Design and Validation of the INCUE Questionnaire: Assessment of Primary Healthcare Nurses’ Basic Training Needs in Palliative Care. International Journal of Environmental Research and Public Health, 18(20), 10995. https://doi.org/10.3390/ijerph182010995







