Gender and Socioeconomic Inequality in the Prescription of Direct Oral Anticoagulants in Patients with Non-Valvular Atrial Fibrillation in Primary Care in Catalonia (Fantas-TIC Study)
Abstract
:1. Introduction
Gender-Based and Socioeconomic Differences in Health Care and Drug Prescription
2. Materials and Methods
2.1. Study Design and Population
2.2. Inclusion and Exclusion Criteria
2.3. Study Variables
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; E Dilaveris, P.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2020, 42, 373–498. [Google Scholar] [CrossRef]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration with the Society of Thoracic Surgeons. Circulation 2019, 140, e125–e151. [Google Scholar] [CrossRef]
- Sholzberg, M.; Gomes, T.; Juurlink, D.N.; Yao, Z.; Mamdani, M.M.; Laupacis, A. The Influence of Socioeconomic Status on Selection of Anticoagulation for Atrial Fibrillation. PLoS ONE 2016, 11, e0149142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Townsend, P.; Corrigan, P.; Kowarzik, U. Poverty and Labour in London: Interim Report of a Centenary Survey; Low Pay Unit: London, UK, 1987. [Google Scholar]
- Borrell, C.; Marí-Dell’Olmo, M.; Serral, G.; Martínez-Beneito, M.; Gotsens, M. Inequalities in mortality in small areas of eleven Spanish cities (the multicenter MEDEA project). Health Place 2010, 16, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Nathan, A.S.; Geng, Z.; Dayoub, E.J.; Khatana, S.A.M.; Eberly, L.A.; Kobayashi, T.; Pugliese, S.C.; Adusumalli, S.; Giri, J.; Groeneveld, P.W. Racial, Ethnic, and Socioeconomic Inequities in the Prescription of Direct Oral Anticoagulants in Patients with Venous Thromboembolism in the United States. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005600. [Google Scholar] [CrossRef] [PubMed]
- Cabezas-Rodríguez, A.; Bacigalupe, A.; Martín, U. Diagnosis and Treatment of Depression in Spain: Are There Gender Inequalities? Int. J. Environ. Res. Public Health 2020, 17, 9232. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Berjón, M.F.; Borrell, C.; Cano-Serral, G.; Esnaola, S.; Nolasco, A.; Pasarín, M.I.; Ramis, R.; Saurina, C.; Escolar-Pujolar, A. Construcción de un índice de privación a partir de datos censales en grandes ciudades españolas (Proyecto MEDEA). Gac. Sanit. 2008, 22, 179–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mooney, J.; Yau, R.; Moiz, H.; Kidy, F.; Evans, A.; Hillman, S.; Todkill, D.; Shantikumar, S. Associations between socioeconomic deprivation and pharmaceutical prescribing in primary care in England. Postgrad. Med. J. 2020. [Google Scholar] [CrossRef]
- Hyun, K.K.; Brieger, D.; Woodward, M.; Richtering, S.; Redfern, J. The effect of socioeconomic disadvantage on prescription of guideline-recommended medications for patients with acute coronary syndrome: Systematic review and meta-analysis. Int. J. Equity Health 2017, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Lunde, E.D.; Joensen, A.M.; Fonager, K.; Lundbye-Christensen, S.; Johnsen, S.P.; Larsen, M.L.; Lip, G.Y.; Riahi, S. Socioeconomic inequality in oral anticoagulation therapy initiation in patients with atrial fibrillation with high risk of stroke: A register-based observational study. BMJ Open 2021, 11, e048839. [Google Scholar] [CrossRef]
- Sjölander, M.; Eriksson, M.; Asplund, K.; Norrving, B.; Glader, E.-L. Socioeconomic Inequalities in the Prescription of Oral Anticoagulants in Stroke Patients with Atrial Fibrillation. Stroke 2015, 46, 2220–2225. [Google Scholar] [CrossRef]
- Essien, U.R.; Magnani, J.W.; Chen, N.; Gellad, W.F.; Fine, M.J.; Hernandez, I. Race/Ethnicity and Sex-Related Differences in Direct Oral Anticoagulant Initiation in Newly Diagnosed Atrial Fibrillation: A Retrospective Study of Medicare Data. J. Natl. Med. Assoc. 2020, 112, 103–108. [Google Scholar] [CrossRef]
- Morgan, R.; Klein, S.L. The intersection of sex and gender in the treatment of influenza. Curr. Opin. Virol. 2019, 35, 35–41. [Google Scholar] [CrossRef]
- Li, Y.-M.; Jiang, C.; He, L.; Li, X.-X.; Hou, X.-X.; Chang, S.-S.; Lip, G.Y.; Du, X.; Dong, J.-Z.; Ma, C.-S. Sex Differences in Presentation, Quality of Life, and Treatment in Chinese Atrial Fibrillation Patients: Insights from the China Atrial Fibrillation Registry Study. Med. Sci. Monit. 2019, 25, 8011–8018. [Google Scholar] [CrossRef]
- Thompson, L.E.; Maddox, T.M.; Lei, L.; Grunwald, G.K.; Bradley, S.M.; Peterson, P.N.; Masoudi, F.A.; Turchin, A.; Song, Y.; Doros, G.; et al. Sex Differences in the Use of Oral Anticoagulants for Atrial Fibrillation: A Report from the National Cardiovascular Data Registry (NCDR ®) PINNACLE Registry. J. Am. Heart Assoc. 2017, 6, e005801. [Google Scholar] [CrossRef]
- WHO (World Health Organization). Classification of Diseases (ICD). Available online: https://www.who.int/classifications/classification-of-diseases (accessed on 26 November 2020).
- World Health Organization. WHOCC-ATC/DDD Index. Available online: https://www.whocc.no/atc_ddd_index/ (accessed on 28 November 2020).
- Caro-Mendivelso, J.; Elorza-Ricart, J.M.; Hermosilla, E.; Méndez-Boo, L.; García-Gil, M.; Prieto-Alhambra, D. Associations between socioeconomic index and mortality in rural and urban small geographic areas of Catalonia, Spain: Ecological study. J. Epidemiol. Res. 2015, 2, 80. [Google Scholar] [CrossRef] [Green Version]
- OMS Health Inequities and Their Causes. Available online: https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes (accessed on 26 November 2020).
- Llorca, M.D.; Martín, C.A.; Carrasco-Querol, N.; Rojas, Z.H.; Drago, E.F.; Cumplido, D.R.; Blanco, E.C.; Gonçalves, A.; Fernández-Sáez, J. Anticoagulation Control with Acenocoumarol or Warfarin in Non-Valvular Atrial Fibrillation in Primary Care (Fantas-TIC Study). Int. J. Environ. Res. Public Health 2021, 18, 5700. [Google Scholar] [CrossRef] [PubMed]
- Chilet-Rosell, E.; Ruiz-Cantero, M.T.; Sáez, J.F.; Álvarez-Dardet, C. Inequality in analgesic prescription in Spain. A gender development issue. Gac. Sanit. 2013, 27, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Dalmau Llorca, M.R.; Aguilar Martín, C.; Carrasco-Querol, N.; Hernández Rojas, Z.; Forcadell Drago, E.; Rodríguez Cumplido, D.; Pepió Vilaubí, J.M.; Castro Blanco, E.; Gonçalves, A.Q.; Fernández-Sáez, J. Oral Anticoagulant Adequacy in Non-Valvular Atrial Fibrillation in Primary Care: A Cross-Sectional Study Using Real-World Data (Fantas-TIC Study). Int. J. Environ. Res. Public Health 2021, 18, 2244. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad, Servicios Sociales E Igualdad. Criterios y Recomendaciones Generales Para el Uso de los Anticoagulantes Orales Directos (ACOD) en la Prevención del Ictus y la Embolia sistéMica en Pacientes con Fibrilación Auricular no Valvular; UT-ACOD/V5/21112016; Informe de Posicionamento Terapéutico, Agencia Española de Medicamentos y Productos Sanitarios, Madrid, Spain; 2016. Available online: https://www.aemps.gob.es/medicamentosUsoHumano/informesPublicos/docs/criterios-anticoagulantes-orales.pdf (accessed on 26 November 2020).
- Gurusamy, V.K.; Brobert, G.; Vora, P.; Friberg, L. Sociodemographic factors and choice of oral anticoagulant in patients with non-valvular atrial fibrillation in Sweden: A population-based cross-sectional study using data from national registers. BMC Cardiovasc. Disord. 2019, 19, 43. [Google Scholar] [CrossRef]
- Jain, R.; Fu, A.-C.; Lim, J.; Wang, C.; Elder, J.; Sander, S.D.; Tan, H. Health Care Resource Utilization and Costs Among Newly Diagnosed and Oral Anticoagulant-Naive Nonvalvular Atrial Fibrillation Patients Treated with Dabigatran or Warfarin in the United States. J. Manag. Care Spéc. Pharm. 2018, 24, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Rojas, Z.H.; Llorca, M.R.D.; Martín, C.A.; Gonçalves, A.Q.; Casajuana, M.; Fernández-Sáez, J.; Cumplido, D.R.; Drago, E.F.; Querol, N.C.; Vilaubí, J.M.P.; et al. Cost-effectiveness of direct oral anticoagulants versus vitamin K antagonist in atrial fibrillation. Medicine 2020, 99, e22054. [Google Scholar] [CrossRef] [PubMed]

| Variables | Vitamin K Antagonists | Direct Oral Anticoagulants | p Value | ||
|---|---|---|---|---|---|
| n * | % | n * | % | ||
| Primary care center characteristics | |||||
| Classification by rurality and socioeconomic deprivation (urban settings) | |||||
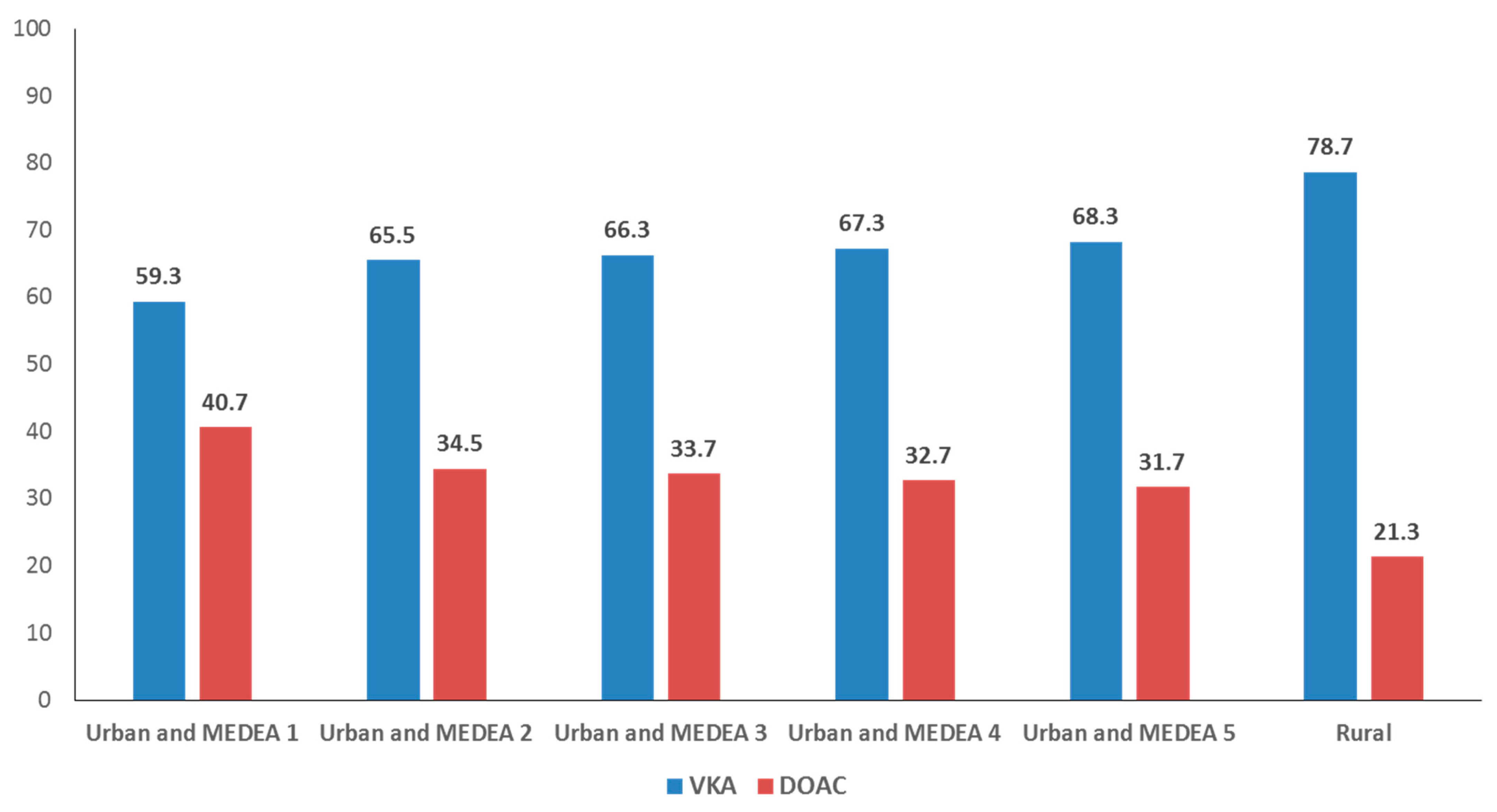
| MEDEA 1 | 5296 | 12.8 | 3630 | 18.6 | <0.001 |
| MEDEA 2 | 6142 | 14.8 | 3230 | 16.5 | <0.001 |
| MEDEA 3 | 6457 | 15.6 | 3285 | 16.8 | <0.001 |
| MEDEA 4 | 6636 | 16.0 | 3224 | 16.5 | 0.14 |
| MEDEA 5 | 5909 | 14.3 | 2747 | 14.1 | 0.49 |
| Rural | 9350 | 22.6 | 2532 | 13.0 | <0.001 |
| Missing | 1640 | 4.0 | 900 | 4.6 | <0.001 |
| Prescription in Primary Care | 33,263 | 80.3 | 9009 | 46.1 | <0.001 |
| Care setting outside PCC | |||||
| Home care | 4926 | 11.9 | 2906 | 14.9 | <0.001 |
| Institutional care | 1646 | 4.0 | 1016 | 5.2 | <0.001 |
| Teaching center | |||||
| Yes | 11,305 | 27.3 | 5117 | 26.2 | 0.004 |
| Missing | 176 | 0.4 | 124 | 0.6 | 0.001 |
| Patient characteristics | |||||
| Total | 41,430 | 67.9 | 19,548 | 32.1 | <0.001 |
| Women | 20,285 | 49.0 | 9800 | 50.1 | 0.007 |
| Men | 21,145 | 51.0 | 9748 | 49.9 | 0.007 |
| Age group | |||||
| <60 years | 935 | 2.3 | 1031 | 5.3 | <0.001 |
| 60–69 years | 4682 | 11.3 | 2893 | 14.8 | <0.001 |
| 70–79 years | 13,654 | 33.0 | 6061 | 31.0 | <0.001 |
| ≥80 years | 22,159 | 53.5 | 9563 | 48.9 | <0.001 |
| Age in years (median, IQR) | 80.0 | 11.0 | 79.0 | 14.0 | <0.001 |
| Years since diagnosis of atrial fibrillation (median, IQR) | 4.0 | 6.0 | 3.0 | 5.0 | <0.001 |
| History of cardiovascular disease | |||||
| Peripheral artery disease | 2704 | 6.5 | 1489 | 7.6 | <0.001 |
| Ischemic cardiopathy | 7514 | 18.1 | 4108 | 21.0 | <0.001 |
| Aortic atheromatosis | 400 | 1.0 | 234 | 1.2 | 0.009 |
| Cerebrovascular event | |||||
| Ischemic stroke | 6436 | 15.5 | 4693 | 24.0 | <0.001 |
| Unspecified cardiovascular accident | 559 | 1.3 | 392 | 2.0 | <0.001 |
| Intracranial bleeding | 364 | 0.9 | 462 | 2.4 | <0.001 |
| Comorbidities | |||||
| Diabetes mellitus | 13,587 | 32.8 | 6474 | 33.1 | 0.43 |
| Hypertension | 33,360 | 80.5 | 15187 | 77.7 | <0.001 |
| Heart failure | 10,846 | 26.2 | 5253 | 26.9 | 0.070 |
| Renal insufficiency | 12,340 | 29.8 | 5281 | 27.0 | <0.001 |
| Bleeding risk factors | |||||
| Alcohol consumption | 1727 | 4.2 | 843 | 4.3 | 0.41 |
| Brain aneurism | 28 | 0.1 | 35 | 0.2 | <0.001 |
| Portal hypertension | 80 | 0.2 | 24 | 0.1 | 0.050 |
| Hepatic insufficiency | 263 | 0.6 | 118 | 0.6 | 0.65 |
| Hereditary hemorrhagic telangiectasia | 2 | 0.0 | 2 | 0.0 | 0.44 |
| Aneurism and aortic dissection | 614 | 1.5 | 322 | 1.6 | 0.12 |
| Intestinal angiodysplasia | 92 | 0.2 | 85 | 0.4 | <0.001 |
| Gastrointestinal bleeding | 3286 | 7.9 | 1852 | 9.5 | <0.001 |
| Bleeding other than gastrointestinal or intracranial | 569 | 1.4 | 269 | 1.4 | 0.98 |
| Stroke risk (CHA2DS2-VASC) | |||||
| 0 | 404 | 1.0 | 499 | 2.6 | <0.001 |
| 1 | 2107 | 5.1 | 1613 | 8.3 | <0.001 |
| 2 | 7251 | 17.5 | 3472 | 17.8 | 0.43 |
| 3 | 14,681 | 35.4 | 5820 | 29.8 | <0.001 |
| ≥4 | 16,987 | 41.0 | 8144 | 41.7 | 0.12 |
| Bleeding risk (HAS-BLED) | |||||
| 0 | 953 | 2.3 | 1063 | 5.4 | <0.001 |
| 1 | 14,563 | 35.2 | 7582 | 38.8 | <0.001 |
| 2 | 15,112 | 36.5 | 6528 | 33.4 | <0.001 |
| 3 | 7783 | 18.8 | 3164 | 16.2 | <0.001 |
| ≥4 | 3019 | 7.3 | 1211 | 6.2 | <0.001 |
| ORadj | 95% CI | p | |
|---|---|---|---|
| Primary care center characteristics | |||
| Classification by rurality and socioeconomic deprivation (urban settings) | |||
| MEDEA 1 | 1 | ||
| MEDEA 2 | 0.69 | (0.65–0.74) | <0.001 |
| MEDEA 3 | 0.64 | (0.60–0.68) | <0.001 |
| MEDEA 4 | 0.61 | (0.57–0.65) | <0.001 |
| MEDEA 5 | 0.58 | (0.54–0.62) | <0.001 |
| Rural | 0.34 | (0.32–0.36) | <0.001 |
| Care setting outside PCC | |||
| Home care | 1.30 | (1.22–1.37) | <0.001 |
| Institutional care | 1.20 | (1.09–1.32) | <0.001 |
| Prescription in Primary Care | |||
| No | 1 | ||
| Yes | 0.22 | (0.21–0.23) | <0.001 |
| Teaching center | |||
| No | 1 | ||
| Yes | 0.88 | (0.85–0.93) | <0.001 |
| Patient characteristics | |||
| Gender | |||
| Men | 1 | ||
| Women | 1.12 | (1.08–1.16) | <0.001 |
| Age group | |||
| <60 | 1 | ||
| 60–69 | 0.59 | (0.52–0.66) | <0.001 |
| 70–79 | 0.43 | (0.38–0.47) | <0.001 |
| ≥80 | 0.41 | (0.37–0.45) | <0.001 |
| Years since diagnosis of atrial fibrillation | 0.98 | (0.97–0.98) | <0.001 |
| History of cardiovascular disease | |||
| Peripheral artery disease | 1.14 | (1.05–1.22) | <0.001 |
| Ischemic cardiopathy | 1.15 | (1.09–1.20) | <0.001 |
| Aortic atheromatosis | 1.11 | (0.93–1.33) | 0.26 |
| Cerebrovascular event | |||
| Ischemic stroke | 1.64 | (1.56–1.72) | <0.001 |
| Unspecified cardiovascular accident | 1.23 | (1.06–1.43) | 0.005 |
| Intracranial bleeding | 2.70 | (2.33–3.13) | <0.001 |
| Comorbidities | |||
| Diabetes mellitus | 1.01 | (0.97–1.05) | 0.62 |
| Hypertension | 0.88 | (0.83–0.92) | <0.001 |
| Heart failure | 1.06 | (1.02–1.11) | 0.004 |
| Renal insufficiency | 0.88 | (0.85–0.93) | <0.001 |
| Bleeding risk factors | |||
| Alcohol consumption | 0.92 | (0.83–1.01) | 0.094 |
| Brain aneurism | 1.18 | (0.65–2.13) | 0.59 |
| Portal hypertension | 0.61 | (0.37–1.02) | 0.059 |
| Hepatic insufficiency | 0.88 | (0.68–1.12) | 0.29 |
| Hereditary hemorrhagic telangiectasia | 1.27 | (0.14–11.11) | 0.83 |
| Aneurism and aortic dissection | 1.10 | (0.94–1.30) | 0.21 |
| Intestinal angiodysplasia | 1.79 | (1.30–2.50) | <0.001 |
| Gastrointestinal bleeding | 1.22 | (1.15–1.32) | <0.001 |
| Bleeding other than gastrointestinal or intracranial | 0.92 | (0.78–1.09) | 0.30 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dalmau Llorca, M.R.; Aguilar Martín, C.; Carrasco-Querol, N.; Hernández Rojas, Z.; Forcadell Drago, E.; Rodríguez Cumplido, D.; Castro Blanco, E.; Pepió Vilaubí, J.M.; Gonçalves, A.Q.; Fernández-Sáez, J. Gender and Socioeconomic Inequality in the Prescription of Direct Oral Anticoagulants in Patients with Non-Valvular Atrial Fibrillation in Primary Care in Catalonia (Fantas-TIC Study). Int. J. Environ. Res. Public Health 2021, 18, 10993. https://doi.org/10.3390/ijerph182010993
Dalmau Llorca MR, Aguilar Martín C, Carrasco-Querol N, Hernández Rojas Z, Forcadell Drago E, Rodríguez Cumplido D, Castro Blanco E, Pepió Vilaubí JM, Gonçalves AQ, Fernández-Sáez J. Gender and Socioeconomic Inequality in the Prescription of Direct Oral Anticoagulants in Patients with Non-Valvular Atrial Fibrillation in Primary Care in Catalonia (Fantas-TIC Study). International Journal of Environmental Research and Public Health. 2021; 18(20):10993. https://doi.org/10.3390/ijerph182010993
Chicago/Turabian StyleDalmau Llorca, Mª Rosa, Carina Aguilar Martín, Noèlia Carrasco-Querol, Zojaina Hernández Rojas, Emma Forcadell Drago, Dolores Rodríguez Cumplido, Elisabet Castro Blanco, Josep Mª Pepió Vilaubí, Alessandra Queiroga Gonçalves, and José Fernández-Sáez. 2021. "Gender and Socioeconomic Inequality in the Prescription of Direct Oral Anticoagulants in Patients with Non-Valvular Atrial Fibrillation in Primary Care in Catalonia (Fantas-TIC Study)" International Journal of Environmental Research and Public Health 18, no. 20: 10993. https://doi.org/10.3390/ijerph182010993
APA StyleDalmau Llorca, M. R., Aguilar Martín, C., Carrasco-Querol, N., Hernández Rojas, Z., Forcadell Drago, E., Rodríguez Cumplido, D., Castro Blanco, E., Pepió Vilaubí, J. M., Gonçalves, A. Q., & Fernández-Sáez, J. (2021). Gender and Socioeconomic Inequality in the Prescription of Direct Oral Anticoagulants in Patients with Non-Valvular Atrial Fibrillation in Primary Care in Catalonia (Fantas-TIC Study). International Journal of Environmental Research and Public Health, 18(20), 10993. https://doi.org/10.3390/ijerph182010993








