Association between Dietary Patterns and Frailty Prevalence in Shanghai Suburban Elders: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Questionnaire and Anthropometric Measurements
2.3. Frailty Assessment
2.4. Dietary Assessment
2.5. A Priori Dietary Pattern Scores
2.6. A Posteriori Dietary Pattern Scores
2.7. Statistical Analysis
3. Results
3.1. General Information of the Participants
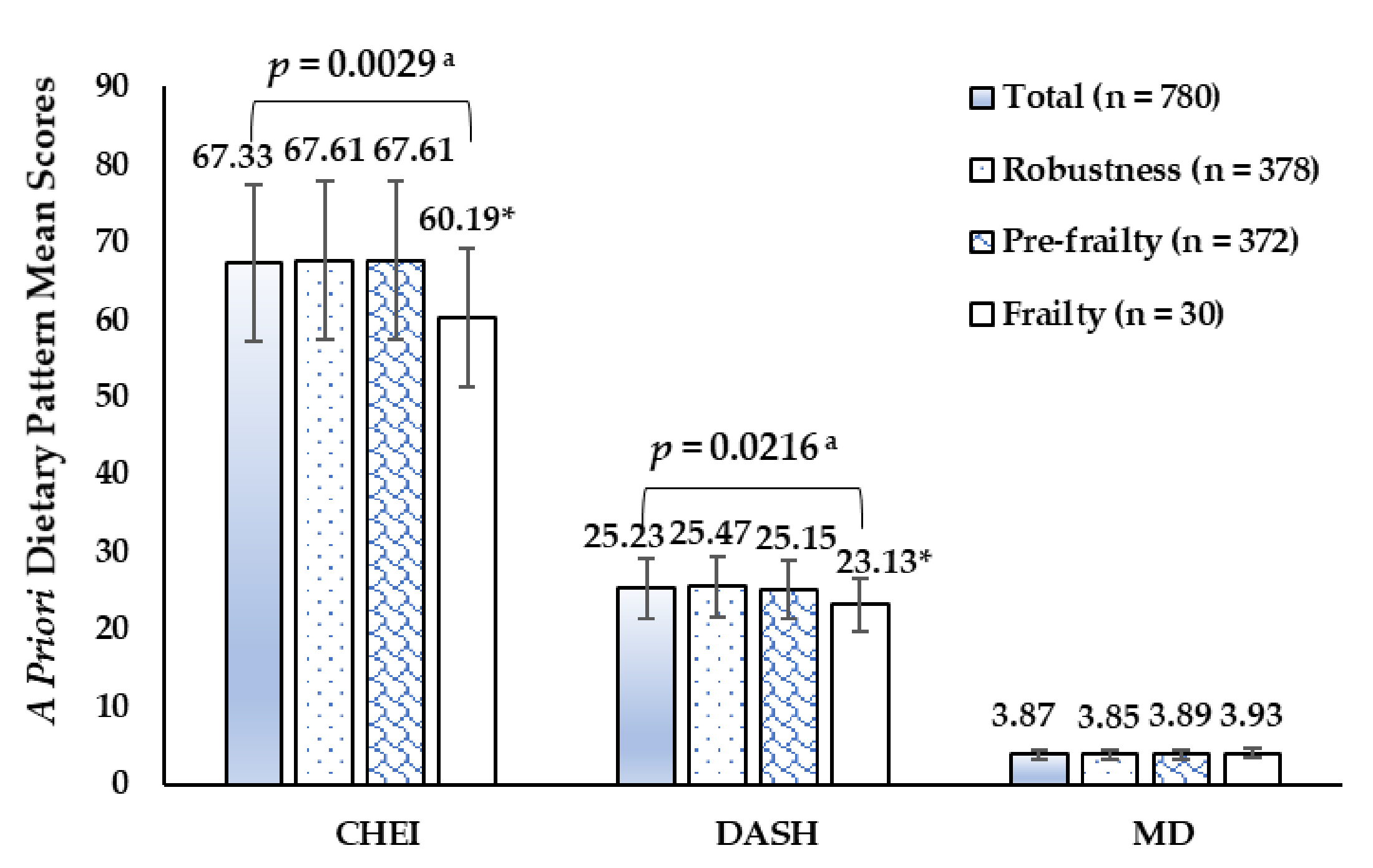
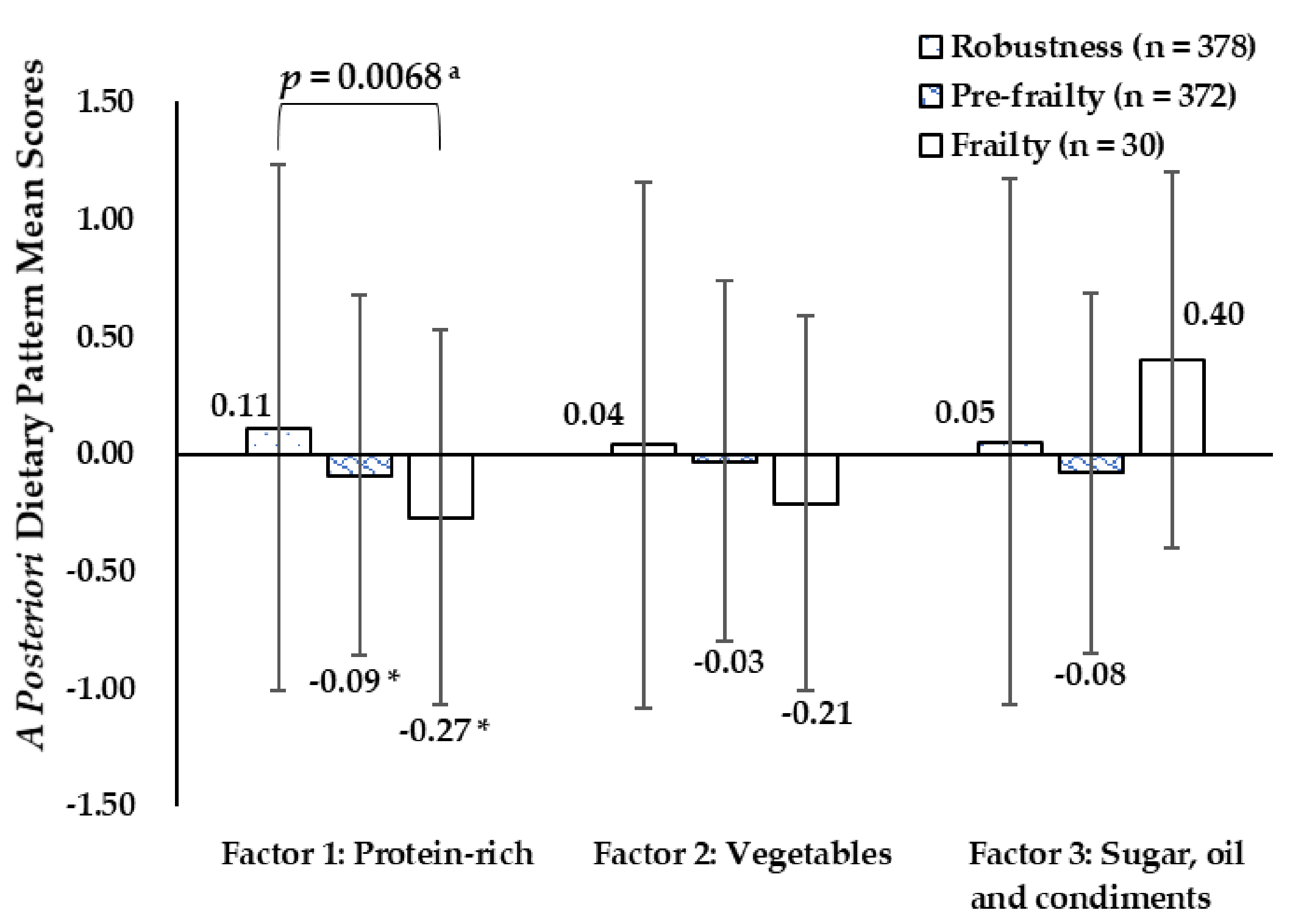
3.2. Dietary Pattern Scores of the Participants
| Characteristics a | Total | Robustness | Pre-Frailty | Frailty | p Value b |
|---|---|---|---|---|---|
| Age (Years) | 68.85 (2.64) | 68.57 (2.60) | 69.14 (2.66) | 68.87 (2.66) | 0.011 |
| BMI (kg/m2) | 25.35 (3.29) | 25.04 (2.98) | 25.63 (3.53) | 25.80 (3.75) | 0.041 |
| Energy intake (kcal/day) | 1408.39 (579.45) | 1438.06 (586.89) | 1388.88 (579.01) | 1276.43 (467.06) | 0.227 |
| Total, N (%) | 780 (100) | 378 (48.46) | 372 (47.69) | 30 (3.85) | |
| Sex | |||||
| Male | 335 (42.95) | 191 (57.01) | 136 (40.60) | 8 (2.39) | <0.001 |
| Female | 445 (57.05) | 187 (42.02) | 236 (53.03) | 22 (4.94) | |
| Age | |||||
| 65–69 years | 472 (60.51) | 247 (52.33) | 208 (44.07) | 17 (3.60) | 0.010 |
| 70–74 years | 308 (39.49) | 131 (42.53) | 164 (53.25) | 13 (4.22) | |
| Education Level | |||||
| Primary school or below | 613 (78.59) | 279 (45.51) | 307 (50.08) | 27 (4.40) | 0.004 |
| Secondary school or above | 167 (21.41) | 99(59.28) | 65 (38.92) | 3 (1.80) | |
| Marital status | |||||
| Married | 672 (86.15) | 339 (50.45) | 307 (45.68) | 26 (3.87) | 0.018 |
| Others c | 108 (13.85) | 39 (36.11) | 65 (60.19) | 4 (3.70) | |
| Annual per capita household income | |||||
| <¥10,000 | 58(7.44) | 19 (32.76) | 35 (60.34) | 4 (6.90) | <0.001 |
| ¥10,000~30,000 | 495 (63.46) | 223 (45.05) | 252 (50.91) | 20 (4.04) | |
| ≥¥30,000 | 227 (29.10) | 136 (59.91) | 85 (37.44) | 6 (2.64) | |
| Behavioral variables | |||||
| Current smoker d | 111 (14.23) | 63 (56.76) | 42 (37.84) | 6 (5.41) | 0.006 |
| Not current smoker | 669 (85.77) | 315 (47.09) | 330 (42.31) | 24 (0.04) | |
| Current alcohol use e | 50 (6.41) | 17 (34.00) | 29 (58.00) | 4 (8.00) | <0.001 |
| Not current alcohol user | 730 (93.59) | 361 (49.45) | 343 (46.99) | 26 (3.56) | |
| Doing housework everyday | 672 (86.15) | 329 (48.96) | 324 (48.21) | 19 (2.83) | 0.001 |
| Not doing housework everyday | 108 (13.85) | 49 (45.37) | 48 (44.44) | 11 (10.19) | |
| Being sedentary > 6 h/day | 94 (12.05) | 45 (47.87) | 43 (45.74) | 6 (6.38) | 0.390 |
| Not being sedentary > 6 h/day | 686 (87.95) | 333 (48.54) | 329 (47.96) | 24 (3.50) | |
| Self-reported diseases | |||||
| Hypertension | 405 (51.92) | 198 (48.89) | 189 (46.67) | 18 (4.44) | 0.606 |
| Without hypertension | 375 (48.08) | 180 (48.00) | 183 (48.80) | 12 (3.20) | |
| Diabetes | 129 (16.54) | 52 (40.31) | 62 (48.06) | 15 (11.63) | <0.001 |
| Without diabetes | 651 (93.46) | 326 (50.08) | 310 (47.62) | 15 (2.30) | |
| Chronic lung disease | 50 (6.41) | 20 (40.00) | 25 (50.00) | 5 (10.00) | 0.067 |
| Without chronic lung disease | 730 (93.59) | 358 (49.04) | 347 (47.53) | 25 (3.42) | |
| Myocardial infarction | 17 (2.18) | 6 (35.29) | 10 (58.82) | 1 (5.88) | 0.465 |
| Without myocardial infarction | 763 (97.92) | 372 (48.75) | 362 (47.44) | 29 (3.80) | |
| Angina | 33 (4.23) | 14 (42.42) | 17 (51.52) | 2 (6.06) | 0.669 |
| Without angina | 747 (95.77) | 364 (48.73) | 355 (47.52) | 28 (3.75) | |
| Asthma | 26 (3.33) | 8 (30.77) | 13 (50.00) | 5 (19.23) | <0.001 |
| Without asthma | 754 (96.67) | 370 (49.07) | 359 (47.61) | 25 (3.32) | |
| Arthritis | 286 (36.67) | 132 (46.15) | 139 (48.60) | 15 (5.24) | 0.238 |
| Without arthritis | 494 (63.33) | 246 (49.80) | 233 (47.17) | 15 (3.04) | |
| Stroke | 102 (13.08) | 37 (36.27) | 56 (54.90) | 9 (8.82) | 0.002 |
| Without stroke | 678 (86.92) | 341 (50.29) | 316 (46.61) | 21 (3.10) | |
| Kidney disease | 164 (21.03) | 80 (48.78) | 78 (47.56) | 6 (3.66) | 0.988 |
| Without kidney disease | 616 (79.97) | 298 (48.38) | 294 (47.73) | 24 (3.90) | |
| Cancer | 27 (3.46) | 8 (29.63) | 17 (62.96) | 2 (7.41) | 0.114 |
| Without cancer | 753 (96.54) | 370 (49.14) | 355 (47.14) | 28 (3.72) | |
3.3. Associations between Each Dietary Pattern Score and Frailty Prevalence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DGC | Dietary Guidelines for Chinese; |
| SSAC | Shanghai Suburban Adult Cohort; |
| FFQ | food frequency questionnaire; |
| BMI | body mass index; |
| Cm | Centimeters; |
| Kg | Kilograms; |
| CES-D | Centers for Epidemiologic Studies Depression Scale; |
| CHEI | Chinese Healthy Eating Index; |
| DASH | Dietary Approaches to Stop Hypertension; |
| MD | Mediterranean Diet; |
| OR | odds ratio; |
| CI | 95% confidence interval. |
References
- Dent, E.; Martin, F.C.; Bergman, H.; Woo, J.; Romero-Ortuno, R.; Walston, J.D. Management of frailty: Opportunities, challenges, and future directions. Lancet 2019, 394, 1376–1386. [Google Scholar] [CrossRef]
- Mousa, A.; Savva, G.M.; Mitnitski, A.; Rockwood, K.; Jagger, C.; Brayne, C.; Matthews, F.E. Is frailty a stable predictor of mortality across time? Evidence from the Cognitive Function and Ageing Studies. Age Ageing 2018, 47, 721–727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ilinca, S.; Calciolari, S. The patterns of health care utilization by elderly Europeans: Frailty and its implications for health systems. Health Serv. Res. 2015, 50, 305–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sodergren, M. Lifestyle predictors of healthy ageing in men. Maturitas 2013, 75, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Yannakoulia, M.; Ntanasi, E.; Anastasiou, C.A.; Scarmeas, N. Frailty and nutrition: From epidemiological and clinical evidence to potential mechanisms. Metabolism 2017, 68, 64–76. [Google Scholar] [CrossRef] [PubMed]
- Woo, J. Nutrition and Frailty. J. Nutr. Health Aging 2018, 22, 1025–1027. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goisser, S.; Guyonnet, S.; Volkert, D. The Role of Nutrition in Frailty: An Overview. J. Frailty Aging 2016, 5, 74–77. [Google Scholar] [PubMed]
- Rashidi, P.F.N.; Amirabdollahian, F.; Haghighatdoost, F. Dietary patterns and frailty: A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 498–513. [Google Scholar] [CrossRef]
- Schulze, M.B.; Hoffmann, K. Methodological approaches to study dietary patterns in relation to risk of coronary heart disease and stroke. Br. J. Nutr. 2006, 95, 860–869. [Google Scholar] [CrossRef]
- Schulze, M.B.; Hu, F.B. Dietary patterns and risk of hypertension, type 2 diabetes mellitus, and coronary heart disease. Curr. Atheroscler. Rep. 2002, 4, 462–467. [Google Scholar] [CrossRef]
- Kojima, G.; Avgerinou, C.; Iliffe, S.; Walters, K. Adherence to Mediterranean Diet Reduces Incident Frailty Risk: Systematic Review and Meta-Analysis. J. Am. Geriatr. Soc. 2018, 66, 783–788. [Google Scholar] [CrossRef]
- Wang, Y.; Hao, Q.; Su, L.; Liu, Y.; Liu, S.; Dong, B. Adherence to the Mediterranean Diet and the Risk of Frailty in Old People: A Systematic Review and Meta-Analysis. J. Nutr. Health Aging 2018, 22, 613–618. [Google Scholar] [CrossRef]
- Chan, R.; Leung, J.; Woo, J. Dietary Patterns and Risk of Frailty in Chinese Community-Dwelling Older People in Hong Kong: A Prospective Cohort Study. Nutrients 2015, 7, 7070–7084. [Google Scholar] [CrossRef] [Green Version]
- Phillips, C.M.; Harrington, J.M.; Perry, I.J. Relationship between dietary quality, determined by DASH score, and cardiometabolic health biomarkers: A cross-sectional analysis in adults. Clin. Nutr. 2019, 38, 1620–1628. [Google Scholar] [CrossRef]
- Djousse, L.; Ho, Y.L.; Nguyen, X.T.; Gagnon, D.R.; Wilson, P.; Cho, K.; Gaziano, J.M. DASH Score and Subsequent Risk of Coronary Artery Disease: The Findings from Million Veteran Program. J. Am. Heart Assoc. 2018, 7, e8089. [Google Scholar] [CrossRef]
- Mozaffari, H.; Ajabshir, S.; Alizadeh, S. Dietary Approaches to Stop Hypertension and risk of chronic kidney disease: A systematic review and meta-analysis of observational studies. Clin. Nutr. 2020, 39, 2035–2044. [Google Scholar] [CrossRef]
- Akhlaghi, M. Dietary Approaches to Stop Hypertension (DASH): Potential mechanisms of action against risk factors of the metabolic syndrome. Nutr. Res. Rev. 2019, 33, 1–18. [Google Scholar] [CrossRef]
- Chiavaroli, L.; Viguiliouk, E.; Nishi, S.K.; Blanco, M.S.; Rahelic, D.; Kahleova, H.; Salas-Salvado, J.; Kendall, C.W.; Sievenpiper, J.L. DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients 2019, 11, 338. [Google Scholar] [CrossRef] [Green Version]
- De Haas, S.; de Jonge, E.; Voortman, T.; Graaff, J.S.; Franco, O.H.; Ikram, M.A.; Rivadeneira, F.; Kiefte-de Jone, J.C.; Schoufour, J.D. Dietary patterns and changes in frailty status: The Rotterdam study. Eur. J. Nutr. 2018, 57, 2365–2375. [Google Scholar] [CrossRef] [Green Version]
- Leon-Munoz, L.M.; Garcia-Esquinas, E.; Lopez-Garcia, E.; Banegas, J.R.; Rodriguez-Artalejo, F. Major dietary patterns and risk of frailty in older adults: A prospective cohort study. BMC Med. 2015, 13, 11. [Google Scholar] [CrossRef] [Green Version]
- Pilleron, S.; Ajana, S.; Jutand, M.A.; Helmer, C.; Dartigues, J.F.; Samieri, C.; Feart, C. Dietary Patterns and 12-Year Risk of Frailty: Results From the Three-City Bordeaux Study. J. Am. Med. Dir. Assoc. 2017, 18, 169–175. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.H.; Martins, B.A.; Okada, K.; Matsushita, E.; Uno, C.; Satake, S.; Kuzuya, M. A 3-year prospective cohort study of dietary patterns and frailty risk among community-dwelling older adults. Clin. Nutr. 2020, 40, 229–236. [Google Scholar] [CrossRef]
- Lo, Y.L.; Hsieh, Y.T.; Hsu, L.L.; Chuang, S.Y.; Chang, H.Y.; Hsu, C.C.; Chen, C.Y.; Pan, W.H. Dietary Pattern Associated with Frailty: Results from Nutrition and Health Survey in Taiwan. J. Am. Geriatr. Soc. 2017, 65, 2009–2015. [Google Scholar] [CrossRef]
- Zhao, Q.; Chen, B.; Wang, R.; Zhu, M.; Shao, Y.; Wang, N.; Liu, X.; Zhang, T.; Jiang, F.; Wang, W.; et al. Cohort profile: Protocol and baseline survey for the Shanghai Suburban Adult Cohort and Biobank (SSACB) study. BMJ Open 2020, 10, e35430. [Google Scholar] [CrossRef]
- Zhang, Y.; Gu, Y.; Wang, N.; Zhao, Q.; Ng, N.; Wang, R.; Zhou, X.; Jiang, Y.; Wang, W.; Zhao, G. Association between anthropometric indicators of obesity and cardiovascular risk factors among adults in Shanghai, China. BMC Public Health 2019, 19, 1035. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Gao, J.; Fei, J.Q.; Jiang, L.J.; Yao, W.Q.; Lin, B.; Guo, H.W. Assessment of the Reproducibility and Validity of a Simple Food-Frequency Questionnaire Used in Dietary Patterns Studies. Acta Nutr. Sin. 2011, 33, 452–456. [Google Scholar]
- Yang, Y.; Wang, G.; Pan, X. China Food Composition Tables Standard Edition; Peking University Medical Press: Beijing, China, 2019. [Google Scholar]
- Yuan, Y.Q.; Li, F.; Wu, H.; Wang, Y.C.; Chen, J.S.; He, G.S.; Li, S.G.; Chen, B. Evaluation of the Validity and Reliability of the Chinese Healthy Eating Index. Nutrients 2018, 10, 114. [Google Scholar] [CrossRef] [Green Version]
- Yuan, Y.Q.; Li, F.; Dong, R.H.; Chen, J.S.; He, G.S.; Li, S.G.; Chen, B. The Development of a Chinese Healthy Eating Index and Its Application in the General Population. Nutrients 2017, 9, 977. [Google Scholar] [CrossRef] [Green Version]
- Fung, T.T.; Chiuve, S.E.; McCullough, M.L.; Rexrode, K.M.; Logroscino, G.; Hu, F.B. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef] [Green Version]
- Talegawkar, S.A.; Bandinelli, S.; Bandeen-Roche, K.; Chen, P.; Milaneschi, Y.; Tanaka, T.; Semba, R.D.; Guralnik, J.M.; Ferrucci, L. A higher adherence to a Mediterranean-style diet is inversely associated with the development of frailty in community-dwelling elderly men and women. J. Nutr. 2012, 142, 2161–2166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, B.; Ma, Y.; Wang, C.; Jiang, M.; Geng, C.; Chang, X.; Ma, B.; Han, L. Prevalence and Risk Factors for Frailty among Community-Dwelling Older People in China: A Systematic Review and Meta-Analysis. J. Nutr. Health Aging 2019, 23, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Liese, A.D.; Krebs-Smith, S.M.; Subar, A.F.; George, S.M.; Harmon, B.E.; Neuhouser, M.L.; Boushey, C.J.; Schap, T.E.; Reedy, J. The Dietary Patterns Methods Project: Synthesis of findings across cohorts and relevance to dietary guidance. J. Nutr. 2015, 145, 393–402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Struijk, E.A.; Hagan, K.A.; Fung, T.T.; Hu, F.B.; Rodriguez-Artalejo, F.; Lopez-Garcia, E. Diet quality and risk of frailty among older women in the Nurses’ Health Study. Am. J. Clin. Nutr. 2020, 111, 877–883. [Google Scholar] [CrossRef] [PubMed]
- Ward, R.E.; Orkaby, A.R.; Chen, J.; Hshieh, T.T.; Driver, J.A.; Gaziano, J.M.; Djousse, L. Association between Diet Quality and Frailty Prevalence in the Physicians’ Health Study. J. Am. Geriatr. Soc. 2020, 68, 770–776. [Google Scholar] [CrossRef]
- Afilalo, J.; Alexander, K.P.; Mack, M.J.; Maurer, M.S.; Green, P.; Allen, L.A.; Popma, J.J.; Ferrucci, L.; Forman, D.E. Frailty assessment in the cardiovascular care of older adults. J. Am. Coll. Cardiol. 2014, 63, 747–762. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.K.; Lyass, A.; Larson, M.G.; Massaro, J.M.; Wang, N.; D’Agostino, R.S.; Benjamin, E.J.; Murabito, J.M. Biomarkers of oxidative stress are associated with frailty: The Framingham Offspring Study. Age 2016, 38, 1. [Google Scholar] [CrossRef] [Green Version]
- Laclaustra, M.; Rodriguez-Artalejo, F.; Guallar-Castillon, P.; Banegas, J.R.; Graciani, A.; Garcia-Esquinas, E.; Ordovas, J.; Lopez-Garcia, E. Prospective association between added sugars and frailty in older adults. Am. J. Clin. Nutr. 2018, 107, 772–779. [Google Scholar] [CrossRef]
- Ntanasi, E.; Yannakoulia, M.; Kosmidis, M.H.; Anastasiou, C.A.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; Scarmeas, N. Adherence to Mediterranean Diet and Frailty. J. Am. Med. Dir. Assoc. 2018, 19, 315–322. [Google Scholar] [CrossRef]
- Veronese, N.; Stubbs, B.; Noale, M.; Solmi, M.; Rizzoli, R.; Vaona, A.; Demurtas, J.; Crepaldi, G.; Maggi, S. Adherence to a Mediterranean diet is associated with lower incidence of frailty: A longitudinal cohort study. Clin. Nutr. 2018, 37, 1492–1497. [Google Scholar] [CrossRef]
- Capurso, C.; Bellanti, F.; Lo, B.A.; Vendemiale, G. The Mediterranean Diet Slows Down the Progression of Aging and Helps to Prevent the Onset of Frailty: A Narrative Review. Nutrients 2019, 12, 35. [Google Scholar] [CrossRef] [Green Version]
- Nanri, H.; Yamada, Y.; Yoshida, T.; Okabe, Y.; Nozawa, Y.; Itoi, A.; Yoshimura, E.; Watanabe, Y.; Yamaguchi, M.; Yokoyama, K.; et al. Sex Difference in the Association Between Protein Intake and Frailty: Assessed Using the Kihon Checklist Indexes Among Older Adults. J. Am. Med. Dir. Assoc. 2018, 19, 801–805. [Google Scholar] [CrossRef]
- O’Connell, M.L.; Coppinger, T.; McCarthy, A.L. The role of nutrition and physical activity in frailty: A review. Clin. Nutr. ESPEN 2020, 35, 1–11. [Google Scholar] [CrossRef]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the PROT-AGE Study Group. J. Am. Med. Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef]
- Coelho-Junior, H.J.; Calvani, R.; Picca, A.; Goncalves, I.O.; Landi, F.; Bernabei, R.; Cesari, M.; Uchida, M.C.; Marzetti, E. Protein-Related Dietary Parameters and Frailty Status in Older Community-Dwellers across Different Frailty Instruments. Nutrients 2020, 12, 508. [Google Scholar] [CrossRef] [Green Version]
- Katsanos, C.S.; Kobayashi, H.; Sheffield-Moore, M.; Aarsland, A.; Wolfe, R.R. Aging is associated with diminished accretion of muscle proteins after the ingestion of a small bolus of essential amino acids. Am. J. Clin. Nutr. 2005, 82, 1065–1073. [Google Scholar] [CrossRef] [Green Version]
- Rahi, B.; Colombet, Z.; Gonzalez-Colaco, H.M.; Dartigues, J.F.; Boirie, Y.; Letenneur, L.; Feart, C. Higher Protein but Not Energy Intake Is Associated With a Lower Prevalence of Frailty Among Community-Dwelling Older Adults in the French Three-City Cohort. J. Am. Med. Dir. Assoc. 2016, 17, 672–677. [Google Scholar] [CrossRef]
- Sandoval-Insausti, H.; Perez-Tasigchana, R.F.; Lopez-Garcia, E.; Garcia-Esquinas, E.; Rodriguez-Artalejo, F.; Guallar-Castillon, P. Macronutrients Intake and Incident Frailty in Older Adults: A Prospective Cohort Study. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2016, 71, 1329–1334. [Google Scholar] [CrossRef]
- Coelho-Junior, H.J.; Rodrigues, B.; Uchida, M.; Marzetti, E. Low Protein Intake Is Associated with Frailty in Older Adults: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2018, 10, 1334. [Google Scholar] [CrossRef] [Green Version]
- Bollwein, J.; Diekmann, R.; Kaiser, M.J.; Bauer, J.M.; Uter, W.; Sieber, C.C.; Volkert, D. Distribution but not amount of protein intake is associated with frailty: A cross-sectional investigation in the region of Nurnberg. Nutr. J. 2013, 12, 109. [Google Scholar] [CrossRef] [Green Version]
- Shikany, J.M.; Barrett-Connor, E.; Ensrud, K.E.; Cawthon, P.M.; Lewis, C.E.; Dam, T.T.; Shannon, J.; Redden, D.T. Macronutrients, diet quality, and frailty in older men. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 695–701. [Google Scholar] [CrossRef]
- Coelho-Junior, H.J.; Marzetti, E.; Picca, A.; Cesari, M.; Uchida, M.C.; Calvani, R. Protein Intake and Frailty: A Matter of Quantity, Quality, and Timing. Nutrients 2020, 12, 2915. [Google Scholar] [CrossRef]
- Checa-Lopez, M.; Oviedo-Briones, M.; Pardo-Gomez, A.; Gonzales-Turin, J.; Guevara-Guevara, T.; Carnicero, J.A.; Alamo-Ascencio, S.; Landi, F.; Cesari, M.; Grodzicki, T.; et al. FRAILTOOLS study protocol: A comprehensive validation of frailty assessment tools to screen and diagnose frailty in different clinical and social settings and to provide instruments for integrated care in older adults. BMC Geriatr. 2019, 19, 86. [Google Scholar] [CrossRef] [Green Version]
- Gill, T.M.; Gahbauer, E.A.; Allore, H.G.; Han, L. Transitions between frailty states among community-living older persons. Arch. Intern. Med. 2006, 166, 418–423. [Google Scholar] [CrossRef]
- Xu, J.W.; Chen, X.R.; Li, Y.C.; Wang, L.M.; Ma, J.X. Analysis of the Eating behavior of Chinese adults in 2010. Chin. J. Prev. Control Chronic Dis. 2015, 23, 684–686. [Google Scholar]
- Pan, H.Y.; Su, Y.P.; Zhao, L.; Liu, X.T.; Tao, L.X.; Ping, Z.; Guo, C. Study on the relationship between eating behavior and cardiovascular disease prevalence in adults. Chin. J. Prev. Control Chronic Dis. 2021, 29, 122–126. [Google Scholar]
- Cohen-Mansfield, J. Skornick-Bouchbinder M, Brill S. Trajectories of end of life: A systematic review. J. Gerontol. Ser. B 2018, 73, 564–572. [Google Scholar] [CrossRef] [Green Version]
| Food Items | Dietary Patterns b | ||
|---|---|---|---|
| Factor 1: “Protein-Rich” | Factor 2: “Vegetables” | Factor 3: “Sugar, Oil, and Condiments” | |
| Soybean and soybean products | 0.66 | 0.26 | 0.10 |
| Red meat | 0.58 | 0.04 | −0.04 |
| Poultry | 0.39 | 0.17 | −0.08 |
| Freshwater fish | 0.63 | 0.15 | 0.04 |
| Ocean fish | 0.44 | 0.40 | −0.06 |
| Shellfish, Shrimp, and Crab | 0.74 | 0.05 | −0.07 |
| Dark vegetables | 0.01 | 0.88 | 0.02 |
| Light colored vegetables | 0.38 | 0.74 | 0.04 |
| Added sugars | −0.03 | 0.02 | 0.58 |
| Cooking oil | 0.06 | −0.01 | 0.75 |
| Condiments | −0.05 | 0.05 | 0.79 |
| Fruits | 0.19 | −0.02 | 0.17 |
| Juice | 0.00 | −0.02 | −0.02 |
| Eggs | 0.04 | 0.17 | −0.03 |
| Dairy and dairy products | 0.02 | 0.19 | 0.09 |
| Processed meat | 0.07 | 0.01 | 0.00 |
| Animal innards | 0.11 | −0.03 | −0.01 |
| Rice and rice products | −0.05 | 0.22 | −0.01 |
| Wheat and wheat products | 0.07 | 0.05 | −0.02 |
| Fried dough foods and potato chips | 0.01 | −0.04 | 0.02 |
| Whole Grains and Mixed Beans | −0.06 | 0.14 | −0.09 |
| Tubers | 0.12 | 0.00 | −0.01 |
| Nuts and Seeds | 0.08 | −0.05 | 0.07 |
| Sweets and desserts | 0.00 | 0.01 | 0.08 |
| Cakes, cookies, pies, and biscuits | 0.02 | −0.02 | −0.02 |
| Beverages | −0.02 | 0.02 | 0.05 |
| Alcoholic beverages | 0.08 | −0.08 | 0.23 |
| Dietary Pattern Score, Mean (SD) | Sex | Age | ||||
|---|---|---|---|---|---|---|
| Male (n = 335) | Female (n = 445) | p value a | 65–59 (n = 472) | 70–74 (n = 308) | p Value a | |
| CHEI | 66.10 (11.58) | 68.25 (11.70) | 0.011 | 68.18 (11.55) | 66.02 (11.80) | 0.012 |
| DASH | 24.79 (4.57) | 25.55 (4.43) | 0.020 | 25.52 (4.56) | 24.77 (4.39) | 0.023 |
| MD | 3.54 (1.37) | 4.13 (1.42) | <0.001 | 3.94 (1.45) | 3.77 (1.38) | 0.108 |
| Factor 1: Protein-rich | 0.12 (1.16) | −0.09 (0.85) | 0.005 | 0.09 (1.12) | −0.13 (0.75) | 0.003 |
| Factor 2: Vegetables | 0.02 (0.70) | −0.02 (1.18) | 0.605 | 0.02 (1.13) | −0.02 (0.76) | 0.686 |
| Factor 3: Sugar, oil and condiments | 0.07 (1.14) | −0.05 (0.88) | 0.104 | −0.04 (1.07) | 0.06 (0.88) | 0.160 |
| Dietary Pattern Score | Model 1 | Model 2 a | Model 3 b | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | p Value | OR | 95%CI | p Value | OR | 95%CI | p Value | |
| All 780 subjects | |||||||||
| DASH | 0.97 | 0.94–1.00 | 0.060 | 0.97 | 0.94–0.99 | 0.033 | 0.98 | 0.95–1.01 | 0.219 |
| CHEI | 0.99 | 0.98–1.00 | 0.193 | 0.99 | 0.98–1.00 | 0.125 | 0.99 | 0.98–1.01 | 0.388 |
| MD | 1.02 | 0.93–1.12 | 0.688 | 0.98 | 0.89–1.09 | 0.719 | 1.01 | 0.91–1.12 | 0.885 |
| Factor 1: Protein-rich | 0.76 | 0.64–0.91 | 0.002 | 0.81 | 0.68–0.96 | 0.015 | 0.82 | 0.69–0.98 | 0.033 |
| Factor 2: Vegetables | 0.90 | 0.77–1.06 | 0.200 | 0.90 | 0.77–1.06 | 0.211 | 0.90 | 0.76–1.06 | 0.219 |
| Factor 3: Sugar, oil and condiments | 0.94 | 0.81–1.08 | 0.391 | 0.95 | 0.82–1.09 | 0.451 | 0.96 | 0.82–1.13 | 0.639 |
| 555 subjects without Diabetes, Stroke, and Asthma | |||||||||
| DASH | 0.95 | 0.92–0.99 | 0.013 | 0.95 | 0.91–0.99 | 0.007 | 0.96 | 0.92–1.00 | 0.032 |
| CHEI | 0.99 | 0.98–1.00 | 0.136 | 0.99 | 0.97–1.00 | 0.115 | 0.99 | 0.98–1.01 | 0.272 |
| MD | 0.97 | 0.86–1.08 | 0.548 | 0.94 | 0.83–1.05 | 0.271 | 0.95 | 0.84–1.08 | 0.450 |
| Factor 1: Protein-rich | 0.80 | 0.66–0.97 | 0.022 | 0.84 | 0.69–1.00 | 0.049 | 0.84 | 0.68–1.03 | 0.085 |
| Factor 2: Vegetables | 0.86 | 0.70–1.06 | 0.148 | 0.87 | 0.71–1.06 | 0.176 | 0.84 | 0.67–1.06 | 0.139 |
| Factor 3: Sugar, oil and condiments | 0.89 | 0.75–1.06 | 0.182 | 0.90 | 0.75–1.08 | 0.248 | 0.91 | 0.74–1.12 | 0.389 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Huang, Y.; Wu, H.; He, G.; Li, S.; Chen, B. Association between Dietary Patterns and Frailty Prevalence in Shanghai Suburban Elders: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 10852. https://doi.org/10.3390/ijerph182010852
Wang Y, Huang Y, Wu H, He G, Li S, Chen B. Association between Dietary Patterns and Frailty Prevalence in Shanghai Suburban Elders: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(20):10852. https://doi.org/10.3390/ijerph182010852
Chicago/Turabian StyleWang, Yingchuan, Yue Huang, Han Wu, Gengsheng He, Shuguang Li, and Bo Chen. 2021. "Association between Dietary Patterns and Frailty Prevalence in Shanghai Suburban Elders: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 20: 10852. https://doi.org/10.3390/ijerph182010852
APA StyleWang, Y., Huang, Y., Wu, H., He, G., Li, S., & Chen, B. (2021). Association between Dietary Patterns and Frailty Prevalence in Shanghai Suburban Elders: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(20), 10852. https://doi.org/10.3390/ijerph182010852







