Telehealth-Based Family Conferences with Implementation of Shared Decision Making Concepts and Humanistic Communication Approach: A Mixed-Methods Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
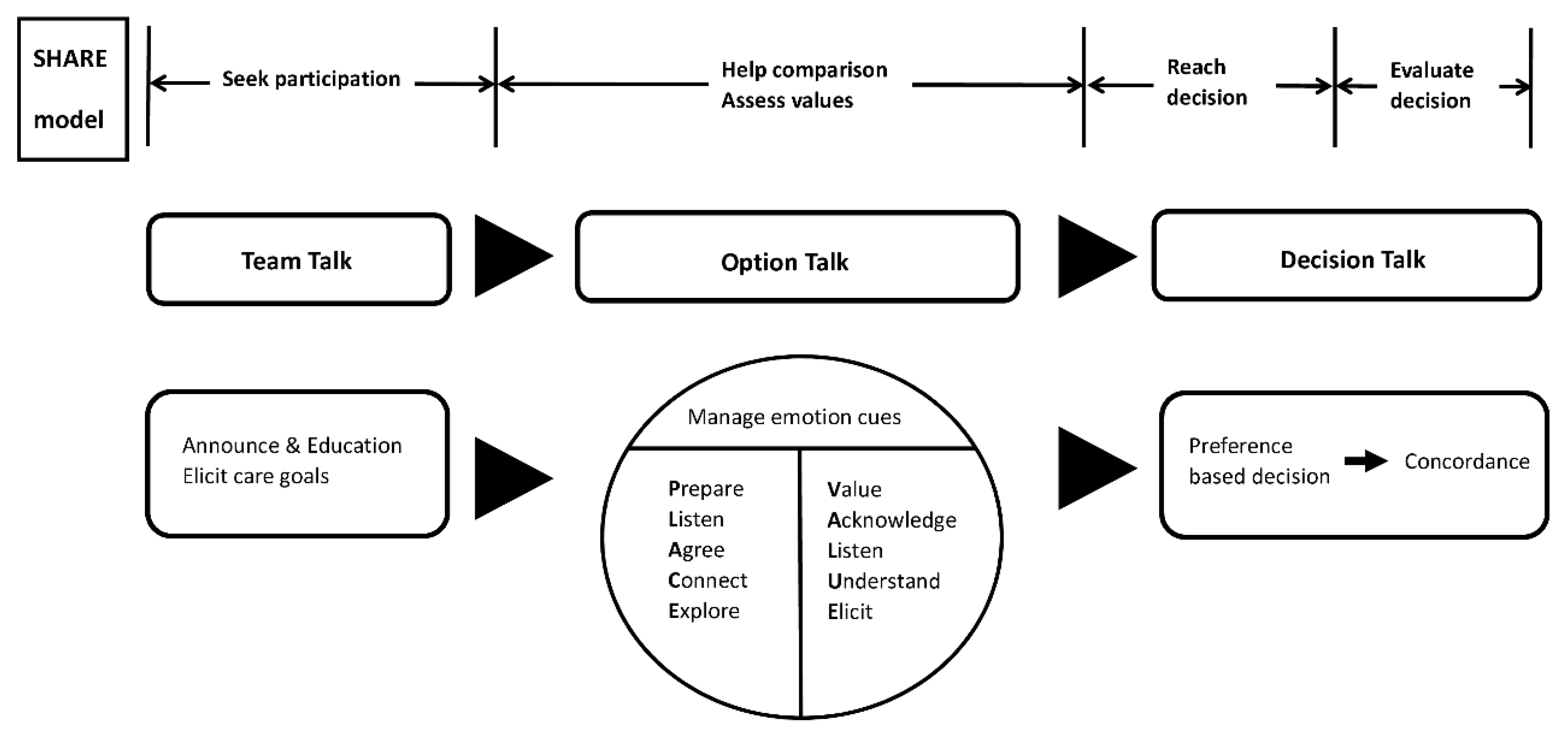
2.1. Framework of Telehealth-Based Family Conference Model with Integration of Shared Decision Making Concepts
2.2. Study Design and Setting
2.3. Collection of Family Conference Information and Statistical Analysis
2.4. Patient and Family-Reported Outcome toward the Smartphone-Enabled Telehealth Family Conference
2.5. Patient Consent Statement and Ethical Approval
3. Results
3.1. Demographic Characteristics
3.2. Patient and Family’s Emotional Cues (Verbal and Nonverbal)
3.3. Medical Team’s Emotional Work and VALUE Approach
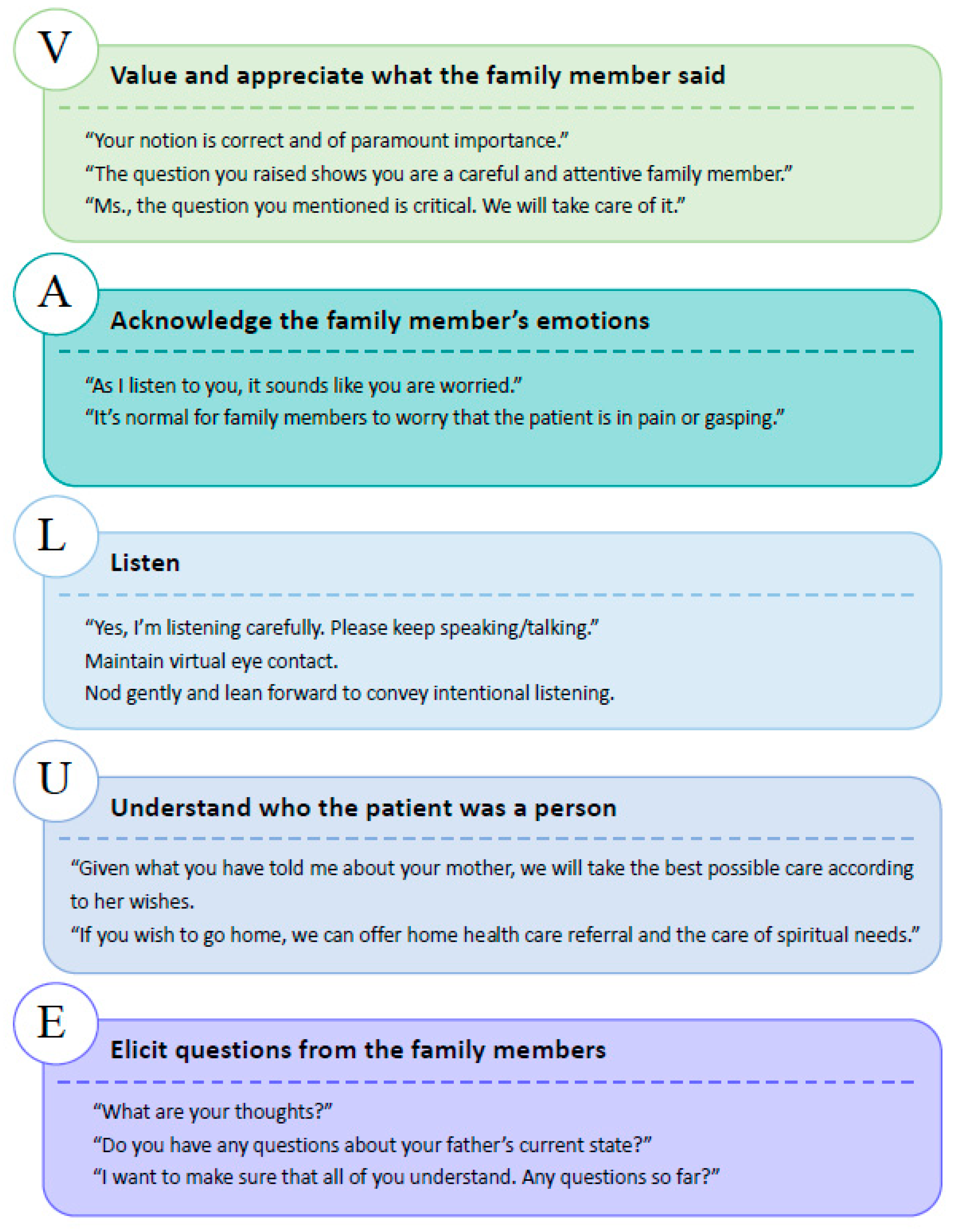
3.4. Patients’ and Family’s Reported Outcomes toward the Telehealth Family Conference
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Powazki, R.D.; Walsh, D. The family conference in palliative medicine: A practical approach. Am. J. Hosp. Palliat. Care 2014, 31, 678–684. [Google Scholar] [CrossRef]
- Fineberg, I.C.; Kawashima, M.; Asch, S.M. Communication with families facing life-threatening illness: A research-based model for family conferences. J. Palliat. Med. 2011, 14, 421–427. [Google Scholar] [CrossRef] [Green Version]
- Budd, J.; Miller, B.S.; Manning, E.M.; Lampos, V.; Zhuang, M.; Edelstein, M.; Rees, G.; Emery, V.C.; Stevens, M.M.; Keegan, N.; et al. Digital technologies in the public-health response to COVID-19. Nat. Med. 2020, 26, 1183–1192. [Google Scholar] [CrossRef]
- Barnes, M.; Sax, P.E. Challenges of "Return to Work" in an ongoing pandemic. N. Engl. J. Med. 2020, 383, 779–786. [Google Scholar] [CrossRef]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schunemann, H.J.; El-Harakek, A.; Bognanni, A.; Lotfi, T.; Loeb, M.; et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Will, C.M. ′And breathe…′? The sociology of health and illness in COVID-19 time. Sociol. Health Illn. 2020, 42, 967–971. [Google Scholar] [CrossRef]
- Mehta, A.K.; Smith, T.J. Palliative care for patients with cancer in the COVID-19 Era. JAMA Oncol. 2020, 6, 1527–1528. [Google Scholar] [CrossRef]
- Curtis, J.R.; Kross, E.K.; Stapleton, R.D. The importance of addressing advance care planning and decisions about do-not-resuscitate orders during novel coronavirus 2019 (COVID-19). JAMA 2020, 323, 1771–1772. [Google Scholar] [CrossRef] [Green Version]
- Kuntz, J.G.; Kavalieratos, D.; Esper, G.J.; Ogbu, N., Jr.; Mitchell, J.; Ellis, C.M.; Quest, T. Feasibility and acceptability of inpatient palliative care e-family meetings during COVID-19 pandemic. J. Pain Symptom Manag. 2020, 60, e28–e32. [Google Scholar] [CrossRef]
- Abrams, E.M.; Shaker, M.; Oppenheimer, J.; Davis, R.S.; Bukstein, D.A.; Greenhawt, M. The challenges and opportunities for shared decision making highlighted by COVID-19. J. Allergy Clin. Immunol. Pract. 2020, 8, 2474–2480 e1. [Google Scholar] [CrossRef]
- Elwyn, G.; Frosch, D.; Thomson, R.; Joseph-Williams, N.; Lloyd, A.; Kinnersley, P.; Cording, E.; Tomson, D.; Dodd, C.; Rollnick, S.; et al. Shared decision making: A model for clinical practice. J. Gen. Intern. Med. 2012, 27, 1361–1367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elwyn, G.; Durand, M.A.; Song, J.; Aarts, J.; Barr, P.J.; Berger, Z.; Cochran, N.; Frosch, D.; Galasinski, D.; Gulbrandsen, P.; et al. A three-talk model for shared decision making: Multistage consultation process. BMJ 2017, 359, j4891. [Google Scholar] [CrossRef] [Green Version]
- Hardman, D.; Geraghty, A.W.A.; Lown, M.; Bishop, F.L. Subjunctive medicine: Enacting efficacy in general practice. Soc. Sci. Med. 2020, 245, 112693. [Google Scholar] [CrossRef] [PubMed]
- Carson, S.S.; Cox, C.E.; Wallenstein, S.; Hanson, L.C.; Danis, M.; Tulsky, J.A.; Chai, E.; Nelson, J.E. Effect of palliative care-led meetings for families of patients with chronic critical illness: A randomized clinical trial. JAMA 2016, 316, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Powazki, R.; Walsh, D.; Hauser, K.; Davis, M.P. Communication in palliative medicine: A clinical review of family conferences. J. Palliat. Med. 2014, 17, 1167–1177. [Google Scholar] [CrossRef] [PubMed]
- Lautrette, A.; Darmon, M.; Megarbane, B.; Joly, L.M.; Chevret, S.; Adrie, C.; Barnoud, D.; Bleichner, G.; Bruel, C.; Choukroun, G.; et al. A communication strategy and brochure for relatives of patients dying in the ICU. N. Engl. J. Med. 2007, 356, 469–478. [Google Scholar] [CrossRef] [Green Version]
- Zulman, D.M.; Haverfield, M.C.; Shaw, J.G.; Brown-Johnson, C.G.; Schwartz, R.; Tierney, A.A.; Zionts, D.L.; Safaeinili, N.; Fischer, M.; Israni, S.T. Practices to foster physician presence and connection with patients in the clinical encounter. JAMA 2020, 323, 70–81. [Google Scholar] [CrossRef]
- Henry, B.W.; Block, D.E.; Ciesla, J.R.; McGowan, B.A.; Vozenilek, J.A. Clinician behaviors in telehealth care delivery: A systematic review. Adv. Health Sci. Educ. Theory Pract. 2017, 22, 869–888. [Google Scholar] [CrossRef]
- Sabesan, S.; Allen, D.; Caldwell, P.; Loh, P.K.; Mozer, R.; Komesaroff, P.A.; Talman, P.; Williams, M.; Shaheen, N.; Grabinski, O. Practical aspects of telehealth: Doctor-patient relationship and communication. Intern. Med. J. 2014, 44, 101–103. [Google Scholar] [CrossRef]
- Fischer, S.H.; Ray, K.N.; Mehrotra, A.; Bloom, E.L.; Uscher-Pines, L. Prevalence and characteristics of telehealth utilization in the United States. JAMA Netw. Open 2020, 3, e2022302. [Google Scholar] [CrossRef]
- Humphreys, J.; Schoenherr, L.; Elia, G.; Saks, N.T.; Brown, C.; Barbour, S.; Pantilat, S.Z. Rapid implementation of inpatient telepalliative medicine consultations during COVID-19 pandemic. J. Pain Symptom Manag. 2020, 60, e54–e59. [Google Scholar] [CrossRef] [PubMed]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef] [PubMed]
- US Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. Available online: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html (accessed on 10 July 2020).
- Taiwan Taiwan Can Help-National Health Insurance’s Contribution in Combating COVID-19. Available online: https://www.nhi.gov.tw/english/Content_List.aspx?n=0B98DCEC6E834809 (accessed on 10 July 2020).
- Greenhalgh, T.; Koh, G.C.H.; Car, J. Covid-19: A remote assessment in primary care. BMJ 2020, 368, m1182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neville, C.W. Telehealth: A balanced look at incorporating this technology into practice. SAGE Open Nurs 2018, 4. [Google Scholar] [CrossRef] [Green Version]
- Wootton, R.; Darkins, A. Telemedicine and the doctor-patient relationship. J. R. Coll. Physicians Lond. 1997, 31, 598–599. [Google Scholar]
- Gordon, H.S.; Solanki, P.; Bokhour, B.G.; Gopal, R.K. “I′m not feeling like i′m part of the conversation” patients′ perspectives on communicating in clinical video telehealth visits. J. Gen. Intern. Med. 2020, 35, 1751–1758. [Google Scholar] [CrossRef]
- Wu, Y.R.; Chou, T.J.; Wang, Y.J.; Tsai, J.S.; Cheng, S.Y.; Yao, C.A.; Peng, J.K.; Hu, W.Y.; Chiu, T.Y.; Huang, H.L. Smartphone-Enabled, telehealth-based family conferences in palliative care during the COVID-19 pandemic: Pilot observational study. JMIR Mhealth Uhealth 2020, 8, e22069. [Google Scholar] [CrossRef]
- Hancock, S.; Preston, N.; Jones, H.; Gadoud, A. Telehealth in palliative care is being described but not evaluated: A systematic review. BMC Palliat. Care 2019, 18, 114. [Google Scholar] [CrossRef] [Green Version]
- Hollander, J.E.; Carr, B.G. Virtually perfect? telemedicine for Covid-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Belanger, E. Shared decision-making in palliative care: Research priorities to align care with patients′ values. Palliat. Med. 2017, 31, 585–586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waterloo, S.F.; Baumgartner, S.E.; Peter, J.; Valkenburg, P.M. Norms of online expressions of emotion: Comparing Facebook, Twitter, Instagram, and WhatsApp. New Media Soc. 2018, 20, 1813–1831. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curtis, J.R.; White, D.B. Practical guidance for evidence-based ICU family conferences. Chest 2008, 134, 835–843. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown-Johnson, C.; Schwartz, R.; Maitra, A.; Haverfield, M.C.; Tierney, A.; Shaw, J.G.; Zionts, D.L.; Safaeinili, N.; Thadaney Israni, S.; Verghese, A.; et al. What is clinician presence? A qualitative interview study comparing physician and non-physician insights about practices of human connection. BMJ Open 2019, 9, e030831. [Google Scholar] [CrossRef] [Green Version]
- Chua, I.S.; Jackson, V.; Kamdar, M. Webside manner during the COVID-19 pandemic: Maintaining human connection during virtual visits. J. Palliat. Med. 2020, 23, 1507–1509. [Google Scholar] [CrossRef]
- Hudson, P.; Quinn, K.; O′Hanlon, B.; Aranda, S. Family meetings in palliative care: Multidisciplinary clinical practice guidelines. BMC Palliat. Care 2008, 7, 12. [Google Scholar] [CrossRef] [Green Version]
- Dev, R.; Coulson, L.; Del Fabbro, E.; Palla, S.L.; Yennurajalingam, S.; Rhondali, W.; Bruera, E. A prospective study of family conferences: Effects of patient presence on emotional expression and end-of-life discussions. J. Pain Symptom Manag. 2013, 46, 536–545. [Google Scholar] [CrossRef]
- Curtis, J.R.; Engelberg, R.A.; Wenrich, M.D.; Shannon, S.E.; Treece, P.D.; Rubenfeld, G.D. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am. J. Respir. Crit. Care Med. 2005, 171, 844–849. [Google Scholar] [CrossRef] [PubMed]
- Curtis, J.R.; Patrick, D.L.; Engelberg, R.A.; Norris, K.; Asp, C.; Byock, I. A measure of the quality of dying and death. Initial validation using after-death interviews with family members. J. Pain Symptom Manag. 2002, 24, 17–31. [Google Scholar] [CrossRef]
- Abbott, K.H.; Sago, J.G.; Breen, C.M.; Abernethy, A.P.; Tulsky, J.A. Families looking back: One year after discussion of withdrawal or withholding of life-sustaining support. Crit. Care Med. 2001, 29, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Wall, R.J.; Engelberg, R.A.; Downey, L.; Heyland, D.K.; Curtis, J.R. Refinement, scoring, and validation of the Family Satisfaction in the Intensive Care Unit (FS-ICU) survey. Crit. Care Med. 2007, 35, 271–279. [Google Scholar] [CrossRef]
- October, T.W.; Dizon, Z.B.; Arnold, R.M.; Rosenberg, A.R. Characteristics of physician empathetic statements during pediatric intensive care conferences with family members: A qualitative study. JAMA Netw. Open 2018, 1, e180351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brock, C.D.; Salinsky, J.V. Empathy: An essential skill for understanding the physician-patient relationship in clinical practice. Fam. Med. 1993, 25, 245–248. [Google Scholar] [PubMed]
- Kelly, M.A.; Gormley, G.J. In, but out of touch: Connecting with patients during the virtual visit. Ann. Fam. Med. 2020, 18, 461–462. [Google Scholar] [CrossRef] [PubMed]
- Gifford, V.; Niles, B.; Rivkin, I.; Koverola, C.; Polaha, J. Continuing education training focused on the development of behavioral telehealth competencies in behavioral healthcare providers. Rural Remote Health 2012, 12, 2108. [Google Scholar]
- Liu, X.; Sawada, Y.; Takizawa, T.; Sato, H.; Sato, M.; Sakamoto, H.; Utsugi, T.; Sato, K.; Sumino, H.; Okamura, S.; et al. Doctor-patient communication: A comparison between telemedicine consultation and face-to-face consultation. Intern. Med. 2007, 46, 227–232. [Google Scholar] [CrossRef] [Green Version]
- Shorofi, S.A.; Jannati, Y.; Moghaddam, H.R.; Yazdani-Charati, J. Psychosocial needs of families of intensive care patients: Perceptions of nurses and families. Niger. Med. J. 2016, 57, 10–18. [Google Scholar] [PubMed]
- Kraft-Todd, G.T.; Reinero, D.A.; Kelley, J.M.; Heberlein, A.S.; Baer, L.; Riess, H. Empathic nonverbal behavior increases ratings of both warmth and competence in a medical context. PLoS ONE 2017, 12, e0177758. [Google Scholar] [CrossRef]
- Holtz, B.E. Patients perceptions of telemedicine visits before and after the coronavirus disease 2019 pandemic. Telemed. J. e-Health 2021, 27, 107–112. [Google Scholar] [CrossRef]
- Ramaswamy, A.; Yu, M.; Drangsholt, S.; Ng, E.; Culligan, P.J.; Schlegel, P.N.; Hu, J.C. Patient satisfaction with telemedicine during the COVID-19 pandemic: Retrospective cohort study. J. Med. Internet Res. 2020, 22, e20786. [Google Scholar] [CrossRef]
- Isautier, J.M.; Copp, T.; Ayre, J.; Cvejic, E.; Meyerowitz-Katz, G.; Batcup, C.; Bonner, C.; Dodd, R.; Nickel, B.; Pickles, K.; et al. People′s experiences and satisfaction with telehealth during the COVID-19 pandemic in australia: Cross-sectional survey study. J. Med. Internet Res. 2020, 22, e24531. [Google Scholar] [CrossRef]
- October, T.W.; Hinds, P.S.; Wang, J.; Dizon, Z.B.; Cheng, Y.I.; Roter, D.L. Parent satisfaction with communication is associated with physician′s patient-centered communication patterns during family conferences. Pediatr. Crit. Care Med. 2016, 17, 490–497. [Google Scholar] [CrossRef] [Green Version]
- West, H.F.; Engelberg, R.A.; Wenrich, M.D.; Curtis, J.R. Expressions of nonabandonment during the intensive care unit family conference. J. Palliat. Med. 2005, 8, 797–807. [Google Scholar] [CrossRef]
- Polinski, J.M.; Barker, T.; Gagliano, N.; Sussman, A.; Brennan, T.A.; Shrank, W.H. Patients′ satisfaction with and preference for telehealth visits. J. Gen. Intern. Med. 2016, 31, 269–275. [Google Scholar] [CrossRef] [Green Version]
- Demiris, G.; Edison, K.; Vijaykumar, S. A comparison of communication models of traditional and video-mediated health care delivery. Int. J. Med. Inform. 2005, 74, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Ohannessian, R.; Duong, T.A.; Odone, A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: A call to action. JMIR Public Health Surveill. 2020, 6, e18810. [Google Scholar] [CrossRef] [PubMed]
- Mazor, K.M.; Clauser, B.E.; Field, T.; Yood, R.A.; Gurwitz, J.H. A demonstration of the impact of response bias on the results of patient satisfaction surveys. Health Serv. Res. 2002, 37, 1403–1417. [Google Scholar] [CrossRef] [Green Version]
- Diamond-Brown, L. The doctor-patient relationship as a toolkit for uncertain clinical decisions. Soc. Sci. Med. 2016, 159, 108–115. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | No. (%) |
|---|---|
| Patient’s baseline characteristics | |
| Age, (mean ± SD) | 72.9 ± 14.3 |
| Marital status | |
| Married | 19 (76%) |
| Single | 4 (16%) |
| Widowed | 2 (8%) |
| Education | |
| Illiterate | 2 (8%) |
| Elementary school | 7 (28%) |
| Junior high school | 5 (20%) |
| High school | 4 (16%) |
| Bachelor | 6 (24%) |
| Master or PhD | 1 (4%) |
| ECOG | |
| 1 | 0 (0%) |
| 2 | 1 (4%) |
| 3 | 9 (36%) |
| 4 | 15 (60%) |
| Whether the patient participates in family conference | |
| Yes | 16 (64%) |
| No | 9 (36%) |
| Family participants’ characteristics | |
| The number of participants (mean ± SD) | 3.52 ± 1.42 |
| The representative primary family caregiver’s relationship to the patient | |
| Parents | 1 (4%) |
| Spouse | 7 (28%) |
| Daughter/Son | 11 (44%) |
| Sibling | 3 (12%) |
| Others | 3 (12%) |
| Category of Emotional Cue | Patient | Family Members |
|---|---|---|
| Nonverbal emotional distress Observed, N (%) Sample behaviors | 6 (24%) Frowning Crying Shaking voices | 7 (28%) Sobbing Fidgeting |
| Verbal emotional distress Observed, N (%) Sample quotes | 5 (20%) Worried about being a burden to his wife. Do not want to receive any treatment (including hospice treatment). Do not want to go back home. | 5 (20%) Worried about withdrawal of treatment. Ask questions about withdraw of treatment repeatedly. Can we deal with unexpected situations? |
| Positive emotion expression Observed, N (%) Sample behaviors | 2 (8%) Smiling | 2 (8%) Smiling Happily waving towards the camera |
| Evaluation Questions | Mean (SD) |
|---|---|
| 1. How well did the medical team answer your questions about your loved one’s illness and treatment? | 8.7 (0.9) |
| 2. How well did the medical team listen to what you had to say? | 8.7 (0.9) |
| 3. How well did the medical team ask about the kinds of treatments your loved one would want if s/he could speak for him/herself? | 8.9 (0.9) |
| 4. How well did the medical team help your family decide about the treatments your loved one would want? | 8.9 (1.1) |
| 5. Overall, how would you rate the medical team’s communication with you during the conference? | 8.7 (1.5) |
| 6. How well did this conference help you understand the choices and decisions that may need to be made? | 9.0 (0.9) |
| 7. Overall, how well did this conference meet your needs? | 9.0 (1.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chou, T.-J.; Wu, Y.-R.; Tsai, J.-S.; Cheng, S.-Y.; Yao, C.-A.; Peng, J.-K.; Chiu, T.-Y.; Huang, H.-L. Telehealth-Based Family Conferences with Implementation of Shared Decision Making Concepts and Humanistic Communication Approach: A Mixed-Methods Prospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 10801. https://doi.org/10.3390/ijerph182010801
Chou T-J, Wu Y-R, Tsai J-S, Cheng S-Y, Yao C-A, Peng J-K, Chiu T-Y, Huang H-L. Telehealth-Based Family Conferences with Implementation of Shared Decision Making Concepts and Humanistic Communication Approach: A Mixed-Methods Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(20):10801. https://doi.org/10.3390/ijerph182010801
Chicago/Turabian StyleChou, Tzu-Jung, Yu-Rui Wu, Jaw-Shiun Tsai, Shao-Yi Cheng, Chien-An Yao, Jen-Kuei Peng, Tai-Yuan Chiu, and Hsien-Liang Huang. 2021. "Telehealth-Based Family Conferences with Implementation of Shared Decision Making Concepts and Humanistic Communication Approach: A Mixed-Methods Prospective Cohort Study" International Journal of Environmental Research and Public Health 18, no. 20: 10801. https://doi.org/10.3390/ijerph182010801
APA StyleChou, T.-J., Wu, Y.-R., Tsai, J.-S., Cheng, S.-Y., Yao, C.-A., Peng, J.-K., Chiu, T.-Y., & Huang, H.-L. (2021). Telehealth-Based Family Conferences with Implementation of Shared Decision Making Concepts and Humanistic Communication Approach: A Mixed-Methods Prospective Cohort Study. International Journal of Environmental Research and Public Health, 18(20), 10801. https://doi.org/10.3390/ijerph182010801






