The Relationship between the Therapeutic Alliance and Suicidal Experiences in People with Psychosis Receiving Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Intervention
2.3. Therapists
2.4. Measures
2.4.1. Working Alliance Inventory—Short Revised (WAI-SR)
2.4.2. Adult Suicide Ideation Questionnaire (ASIQ)
2.4.3. Suicide Plans and Attempts
2.4.4. Beck Hopelessness Scale (BHS)
2.4.5. Calgary Depression Scale for Schizophrenia (CDSS)
2.4.6. Dose of Therapy
2.4.7. Missing Data
2.5. Procedure
2.6. Statistical Analysis
3. Results
3.1. Is There a Relationship between Suicidal Experiences Prior to Starting Therapy and the Therapeutic Alliance (Session 4)?
3.1.1. Suicidal Ideation
3.1.2. Suicide Plans
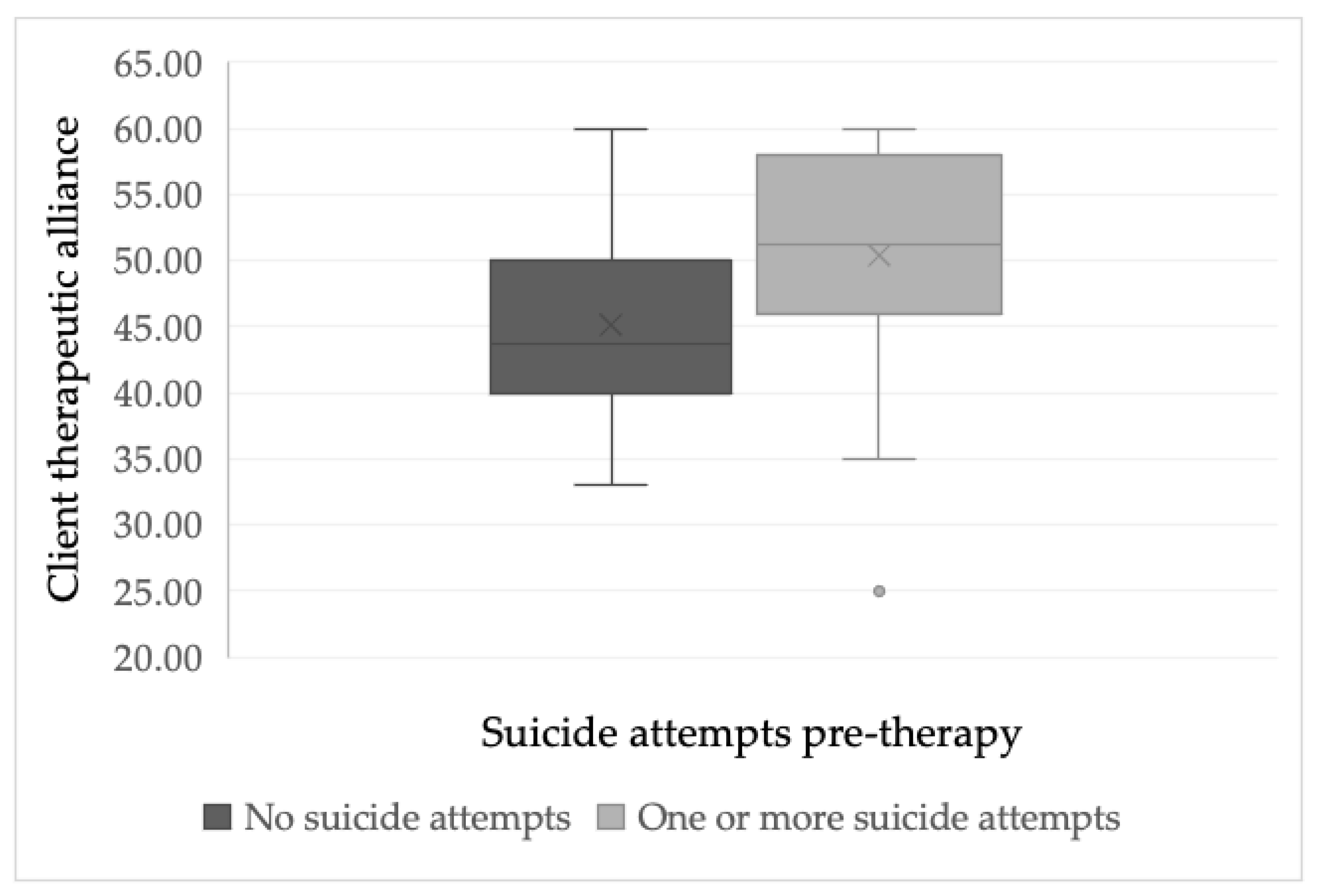
3.1.3. Suicide Attempts
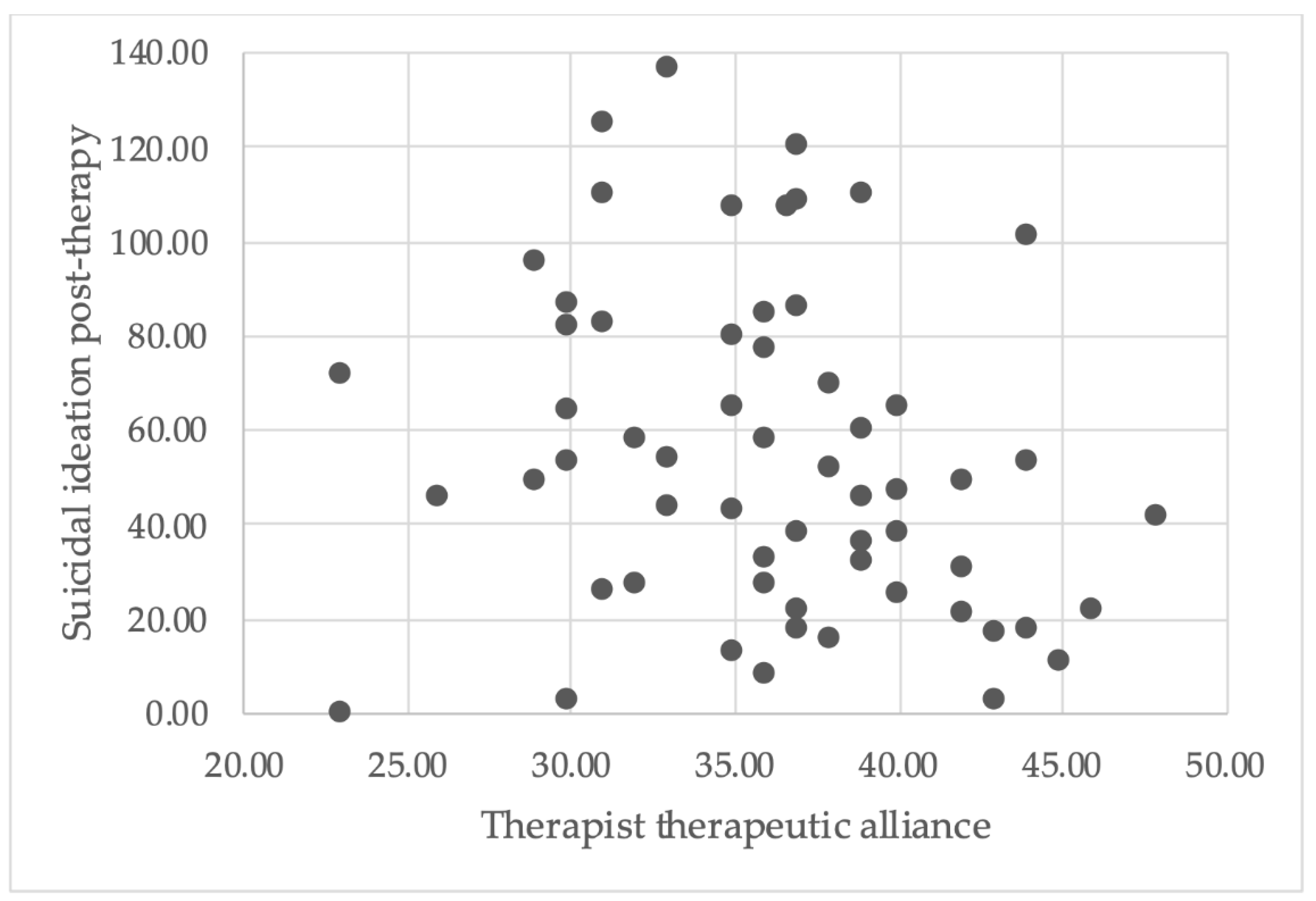
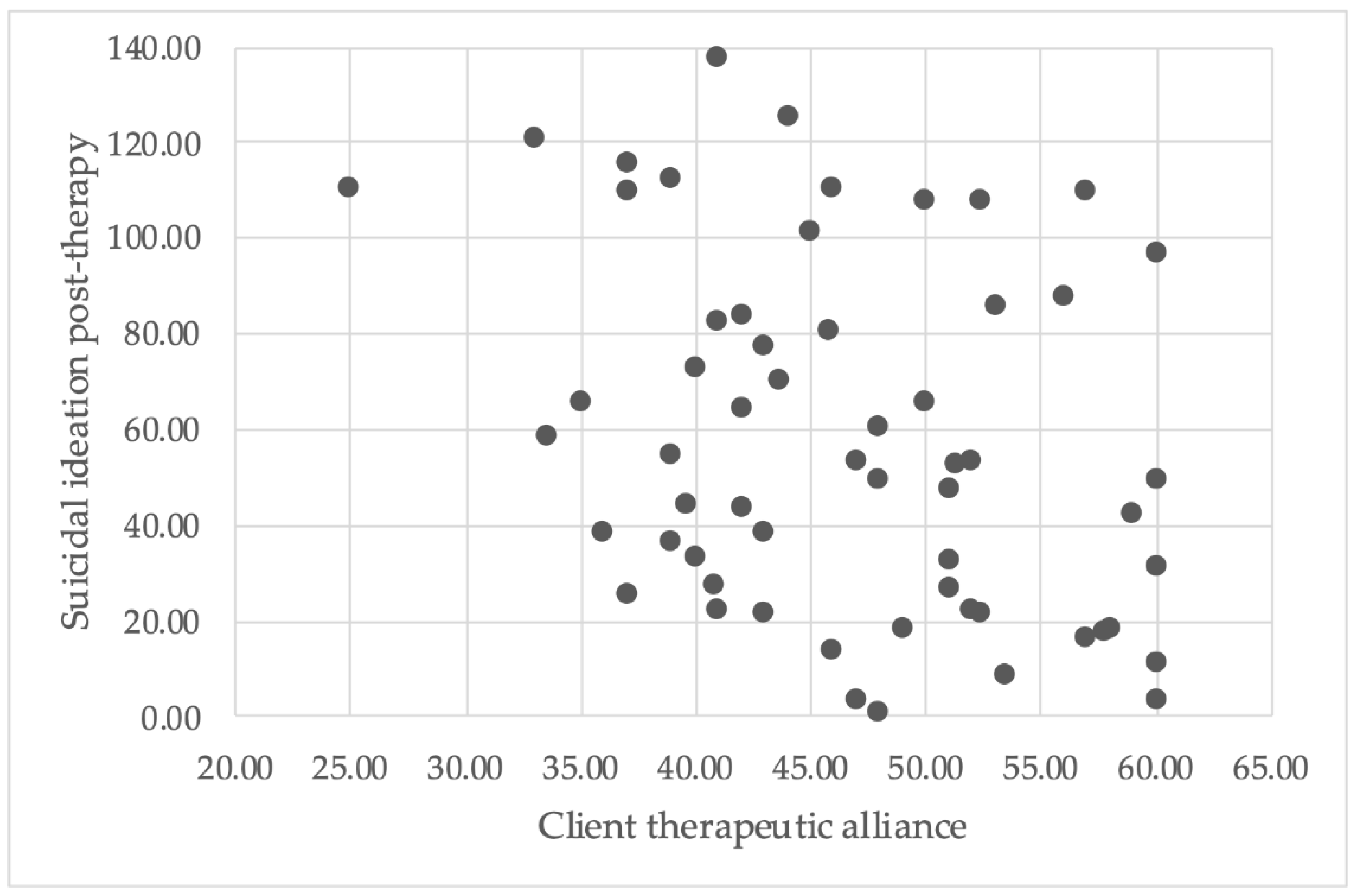
3.2. Does the Therapeutic Alliance Predict Suicidal Experiences Measured Post-Therapy?
3.2.1. Suicidal Ideation
3.2.2. Suicide Plans
3.2.3. Suicide Attempts
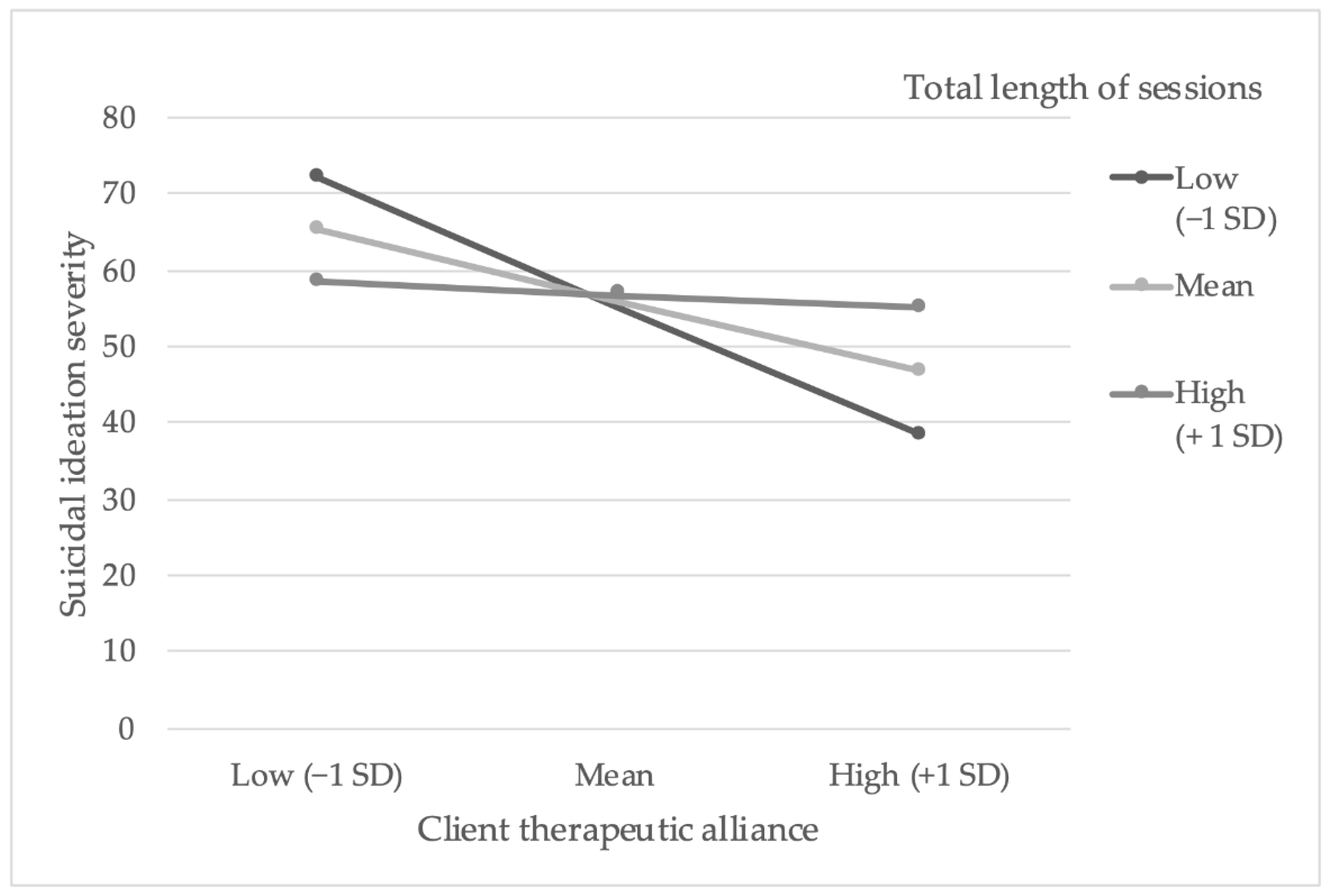
3.3. Does the Number of Minutes of CBSPp Therapy Session Attendance Amplify the Relationship between the Therapeutic Alliance and Suicidal Experiences Post-Therapy?
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bolton, C.; Gooding, P.; Kapur, N.; Barrowclough, C.; Tarrier, N. Developing Psychological Perspectives of Suicidal Behavior and Risk in People with a Diagnosis of Schizophrenia: We Know They Kill Themselves but Do We Understand Why? Clin. Psychol. Rev. 2007, 27, 511–536. [Google Scholar] [CrossRef]
- Ko, Y.S.; Tsai, H.C.; Chi, M.H.; Su, C.C.; Lee, I.H.; Chen, P.S.; Chen, K.C.; Yang, Y.K. Higher Mortality and Years of Potential Life Lost of Suicide in Patients with Schizophrenia. Psychiatry Res. 2018, 270, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Bornheimer, L.A.; Hong, V.; Li, J.; Fernandez, L.; King, C.A. Relationships between Hallucinations, Delusions, Depression, Suicide Ideation, and Plan among Adults Presenting with Psychosis in Psychiatric Emergency Care. Psychosis 2021. [Google Scholar] [CrossRef]
- Zaheer, J.; Jacob, B.; de Oliveira, C.; Rudoler, D.; Juda, A.; Kurdyak, P. Service Utilization and Suicide among People with Schizophrenia Spectrum Disorders. Schizophr. Res. 2018, 202, 347–353. [Google Scholar] [CrossRef]
- Sicotte, R.; Iyer, S.N.; Kiepura, B.; Abdel-Baki, A. A Systematic Review of Longitudinal Studies of Suicidal Thoughts and Behaviors in First-Episode Psychosis: Course and Associated Factors. Soc. Psych. Psychiatr. Epidemiol. 2021, 1, 1–38. [Google Scholar] [CrossRef]
- Clapham, E.; Bodén, R.; Brandt, L.; Jönsson, E.G.; Bahmanyar, S.; Ekbom, A.; Ösby, U.; Reutfors, J. Suicide Ideation and Behavior as Risk Factors for Subsequent Suicide in Schizophrenia: A Nested Case–Control Study. Suicide Life-Threat. Behav. 2019, 49, 996–1005. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, R.M.; Yang, F.; Kapczinski, F.; Passos, I.C. Risk Factors for Suicidality in Patients with Schizophrenia: A Systematic Review, Meta-Analysis, and Meta-Regression of 96 StuDies. Schizophr. Bull. 2018, 44, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Nah, G.; Choi, S.; Kim, H.; Lee, J.-Y.; Kim, J.-M.; Shin, I.-S.; Yoon, J.-S.; Kim, S.-W. Characteristics of Patients Who Died by Suicide in a Community Mental Health Center. Korean J. Schizophr. Res. 2017, 20, 55. [Google Scholar] [CrossRef][Green Version]
- Zaheer, J.; Olfson, M.; Mallia, E.; Lam, J.S.H.; de Oliveira, C.; Rudoler, D.; Carvalho, A.F.; Jacob, B.J.; Juda, A.; Kurdyak, P. Predictors of Suicide at Time of Diagnosis in Schizophrenia Spectrum Disorder: A 20-Year Total Population Study in Ontario, Canada. Schizophr. Res. 2020, 222, 382–388. [Google Scholar] [CrossRef]
- Bornheimer, L.A. Moderating Effects of Positive Symptoms of Psychosis in Suicidal Ideation among Adults Diagnosed with Schizophrenia. Schizophr. Res. 2016, 176, 364–370. [Google Scholar] [CrossRef]
- Berardelli, I.; Sarubbi, S.; Rogante, E.; Hawkins, M.; Cocco, G.; Erbuto, D.; Lester, D.; Pompili, M. The Role of Demoralization and Hopelessness in Suicide Risk in Schizophrenia: A Review of the Literature. Medicina 2019, 55, 200. [Google Scholar] [CrossRef]
- Johnson, J.; Gooding, P.A.; Wood, A.M.; Taylor, P.J.; Pratt, D.; Tarrier, N. Resilience to Suicidal Ideation in Psychosis: Positive Self-Appraisals Buffer the Impact of Hopelessness. Behav. Res. Ther. 2010, 48, 883–889. [Google Scholar] [CrossRef]
- Klonsky, D.E.; Kotov, R.; Bakst, S.; Rabinowitz, J.; Bromet, E.J. Hopelessness as a Predictor of Attempted Suicide among First Admission Patients with Psychosis: A 10-Year Cohort Study. Suicide Life-Threat. Behav. 2012, 42, 1–10. [Google Scholar] [CrossRef]
- Yates, K.; Lång, U.; Cederlöf, M.; Boland, F.; Taylor, P.; Cannon, M.; McNicholas, F.; Devylder, J.; Kelleher, I. Association of Psychotic Experiences with Subsequent Risk of Suicidal Ideation, Suicide Attempts, and Suicide Deaths: A Systematic Review and Meta-Analysis of Longitudinal Population Studies. JAMA Psychiatry 2019, 76, 180–189. [Google Scholar] [CrossRef]
- O’Connor, R.C.; Kirtley, O.J. The Integrated Motivational-Volitional Model of Suicidal Behavior. Philos. Trans. R. Soc. B 2018, 373, 20170268. [Google Scholar] [CrossRef]
- Tarrier, N.; Gooding, P.; Pratt, D.; Kelly, J.; Awenat, Y.; Maxwell, J. Cognitive Behavioral Prevention of Suicide in Psychosis; Routledge: London, UK, 2013. [Google Scholar] [CrossRef]
- Tarrier, N.; Taylor, K.; Gooding, P. Cognitive-Behavioral Interventions to Reduce Suicide Behavior: A Systematic Review and Meta-Analysis. Behav. Modif. 2008, 32, 77–108. [Google Scholar] [CrossRef]
- Joiner, T.E.; Silva, C. Why People Die by Suicide: Further Development and Tests of the Interpersonal-Psychological Theory of Suicidal Behavior. In Meaning, Mortality, and Choice: The Social Psychology of Existential Concerns; Shaver, P.R., Mikulincer, M., Eds.; American Psychological Association: Washington, DC, USA, 2012; pp. 325–336. [Google Scholar] [CrossRef]
- Johnson, J.; Gooding, P.; Tarrier, N. Suicide Risk in Schizophrenia: Explanatory Models and Clinical Implications, The Schematic Appraisal Model of Suicide (SAMS). Psychol. Psychother. 2008, 81, 55–77. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.M.G. Cry of Pain: Understanding Suicide and Self-Harm; Penguin Books: London, UK, 1997. [Google Scholar]
- Tarrier, N.; Kelly, J.; Maqsood, S.; Snelson, N.; Maxwell, J.; Law, H.; Dunn, G.; Gooding, P. The Cognitive Behavioral Prevention of Suicide in Psychosis: A Clinical Trial. Schizophr. Res. 2014, 156, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Haddock, G.; Pratt, D.; Gooding, P.A.; Peters, S.; Emsley, R.; Evans, E.; Kelly, J.; Huggett, C.; Munro, A.; Harris, K.; et al. Feasibility and Acceptability of Suicide Prevention Therapy on Acute Psychiatric Wards: Randomized Controlled Trial. BJPsych Open 2019, 5, e14. [Google Scholar] [CrossRef] [PubMed]
- Bordin, E.S. The Generalizability of the Psychoanalytic Concept of the Working Alliance. Psychol. Psychother. 1979, 16, 252–259. [Google Scholar] [CrossRef]
- Zilcha-Mano, S. Is the Alliance Really Therapeutic? Revisiting This Question in Light of Recent Methodological Advances. Am. Psychol. 2017, 72, 311–325. [Google Scholar] [CrossRef]
- Awenat, Y.F.; Peters, S.; Gooding, P.A.; Pratt, D.; Shaw-Núñez, E.; Harris, K.; Haddock, G. A Qualitative Analysis of Suicidal Psychiatric Inpatients Views and Expectations of Psychological Therapy to Counter Suicidal Thoughts, Acts and Deaths. BMC Psychiatry 2018, 18, 334. [Google Scholar] [CrossRef]
- Blanchard, M.; Farber, B.A. It Is Never Okay to Talk about Suicide: Patients’ Reasons for Concealing Suicidal Ideation in Psychotherapy. Psychother. Res. 2020, 30, 124–136. [Google Scholar] [CrossRef]
- Latalova, K.; Prasko, J.; Kamaradova, D.; Ociskova, M.; Cinculova, A.; Grambal, A.; Kubinek, R.; Mainerova, B.; Smoldasova, J.; Tichackova, A.; et al. Self-Stigma and Suicidality in Patients with Neurotic Spectrum Disorder—A Cross Sectional Study. Neuroendocr. Lett. 2014, 35, 474–480. [Google Scholar]
- Switzer, F.; Harper, S.F. A Narrative Review of the Barriers to the Implementation of Cognitive Behavioral Therapy for Psychosis. Psychosis 2019, 11, 151–161. [Google Scholar] [CrossRef]
- Browne, J.; Nagendra, A.; Kurtz, M.; Berry, K.; Penn, D.L. The Relationship between the Therapeutic Alliance and Client Variables in Individual Treatment for Schizophrenia Spectrum Disorders and Early Psychosis: Narrative Review. Clin. Psychol. Rev. 2019, 71, 51–62. [Google Scholar] [CrossRef]
- Shattock, L.; Berry, K.; Degnan, A.; Edge, D. Therapeutic Alliance in Psychological Therapy for People with Schizophrenia and Related Psychoses: A Systematic Review. Clin. Psychol. Psychother. 2018, 25, e60–e85. [Google Scholar] [CrossRef] [PubMed]
- Gysin-Maillart, A.C.; Soravia, L.M.; Gemperli, A.; Michel, K. Suicide Ideation Is Related to Therapeutic Alliance in a Brief Therapy for Attempted Suicide. Arch. Suicide Res. 2017, 21, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.L.; O’Connor, S.S.; Kaminer, B.; Gutierrez, P.M.; Carney, E.; Groh, B.; Jobes, D.A. Evaluation of Structured Assessment and Mediating Factors of Suicide-Focused Group Therapy for Veterans Recently Discharged from Inpatient Psychiatry. Arch. Suicide Res. 2019, 23, 15–33. [Google Scholar] [CrossRef]
- Flückiger, C.; Del, A.C.; Wampold, B.E.; Horvath, A.O. The Alliance in Adult Psychotherapy: A Meta-Analytic Synthesis. Psychother. 2018, 55, 316–340. [Google Scholar] [CrossRef]
- Turner, R.M. Naturalistic Evaluation of Dialectical Behavior Therapy-Oriented Treatment for Borderline Personality Disorder. Cogn. Behav. Pract. 2000, 7, 413–419. [Google Scholar] [CrossRef]
- Bedics, J.D.; Atkins, D.C.; Harned, M.S.; Linehan, M.M. The Therapeutic Alliance as a Predictor of Outcome in Dialectical Behavior Therapy Versus Nonbehavioral Psychotherapy by Experts for Borderline Personality Disorder. Psychother. 2015, 52, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Goldsmith, L.P.; Lewis, S.W.; Dunn, G.; Bentall, R.P. Psychological Treatments for Early Psychosis Can Be Beneficial or Harmful, Depending on the Therapeutic Alliance: An Instrumental Variable Analysis. Psychol. Med. 2015, 45, 2365–2373. [Google Scholar] [CrossRef] [PubMed]
- Howard, K.I.; Kopta, S.M.; Krause, M.S.; Orlinsky, D.E. The Dose-Effect Relationship in Psychotherapy. Am. Psychol. 1986, 41, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Parry, G.D.; Crawford, M.J.; Duggan, C. Iatrogenic Harm from Psychological Therapies-Time to Move On. Br. J. Psychiatry 2016, 208, 210–212. [Google Scholar] [CrossRef] [PubMed]
- Huggett, C.; Gooding, P.; Haddock, G.; Pratt, D. The Relationship between the Therapeutic Alliance in Psychotherapy and Suicidal Experiences: A Systematic Review. Division of Psychology and Mental Health; School of Health Sciences, University of Manchester, Manchester Academic Health Science Centre: Manchester, UK, 2020; manuscript submitted. [Google Scholar]
- Gooding, P.A.; Pratt, D.; Awenat, Y.; Drake, R.; Elliott, R.; Emsley, R.; Huggett, C.; Jones, S.; Kapur, N.; Lobban, F.; et al. A Psychological Intervention for Suicide Applied to Non-Affective Psychosis: The CARMS (Cognitive AppRoaches to CoMbatting Suicidality) Randomized Controlled Trial Protocol. BMC Psychiatry 2020, 20, 306. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Act 2020. Available online: https://www.legislation.gov.uk/ukpga/2020/7/contents/enacted (accessed on 20 August 2020).
- Pratt, D.; Gooding, P.A.; Kelly, J.A.; Johnson, J.; Tarrier, N. Case Formulation in Suicidal Behaviour. In Case Formulation in Cognitive Behaviour Therapy: The Treatment of Challenging and Complex Cases; Tarrier, N., Johnson, J., Eds.; Routledge: London, UK, 2016; pp. 265–283. [Google Scholar]
- Pratt, D.; Tarrier, N.; Dunn, G.; Awenat, Y.; Shaw, J.; Ulph, F.; Gooding, P. Cognitive-Behavioral Suicide Prevention for Male Prisoners: A Pilot Randomized Controlled Trial. Psychol. Med. 2015, 45, 3441–3451. [Google Scholar] [CrossRef]
- Haddock, G.; Devane, S.; Bradshaw, T.; McGovern, J.; Tarrier, N.; Kinderman, P.; Baguley, I.; Lancashire, S.; Harris, N. An Investigation into the Psychometric Properties of the Cognitive Therapy Scale for Psychosis (CTS-Psy). Behav. Cogn. Psychother. 2001, 29, 221–233. [Google Scholar] [CrossRef]
- Hatcher, R.L.; Gillaspy, J.A. Development and Validation of a Revised Short Version of the Working Alliance Inventory. Psychother. Res. 2006, 16, 12–25. [Google Scholar] [CrossRef]
- Horvath, A.O.; Greenberg, L.S. Development and Validation of the Working Alliance Inventory. J. Couns. Psychol. 1989, 36, 223–233. [Google Scholar] [CrossRef]
- Hatcher, R.L.; Lindqvist, K.; Falkenström, F. Psychometric Evaluation of the Working Alliance Inventory—Therapist Version: Current and New Short Forms. Psychother. Res. 2020, 30, 706–717. [Google Scholar] [CrossRef]
- Reynolds, W.M. ASIQ, Adult Suicidal Ideation Questionnaire: Professional Manual; Psychological Assessment Resources: Lutz, FL, USA, 1991. [Google Scholar]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The Measurement of Pessimism: The Hopelessness Scale. J. Consult. Clin. Psychol. 1974, 42, 861–865. [Google Scholar] [CrossRef]
- Addington, D.; Addington, J.; Schissel, B. A Depression Rating Scale for Schizophrenics. Schizophr. Res. 1990, 3, 247–251. [Google Scholar] [CrossRef]
- Hazell, C.M.; Hayward, M.; Cavanagh, K.; Strauss, C. A Systematic Review and Meta-Analysis of Low Intensity CBT for Psychosis. Clin. Psychol. Rev. 2016, 45, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Mazza, G.L.; Dueck, A.C. Statistical Analysis of Patient-Reported Outcomes in Clinical Trials. In Principles and Practice of Clinical Trials; Springer: Basel, Switzerland, 2020; pp. 1–20. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; SAGE Publications: London, UK, 2018. [Google Scholar]
- Kim, H.-Y. Statistical Notes for Clinical Researchers: Assessing Normal Distribution (2) Using Skewness and Kurtosis. Restor. Dent. Endod. 2013, 38, 52. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. PROCESS: A Versatile Computational Tool for Observed Variable Moderation, Mediation, and Conditional Process Modeling. 2012. Available online: http://www.afhayes.com/public/process2012.pdf (accessed on 5 April 2020).
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical Power Analyses Using G*Power 3.1: Tests for Correlation and Regression Analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Ibrahim, M.; Jin, B.; Russon, J.; Diamond, G.; Kobak, R. Predicting Alliance for Depressed and Suicidal Adolescents: The Role of Perceived Attachment to Mothers. Evidence-Based Pract. Child Adolesc. Ment. Health 2018, 3, 42–56. [Google Scholar] [CrossRef]
- Mirza, A.; Birtel, M.D.; Pyle, M.; Morrison, A.P. Cultural Differences in Psychosis: The Role of Causal Beliefs and Stigma in White British and South Asians. J. Cross. Cult. Psychol. 2019, 50, 441–459. [Google Scholar] [CrossRef]
- Koç, V.; Kafa, G. Cross-Cultural Research on Psychotherapy: The Need for a Change. J. Cross-Cult. Psychol. 2019, 50, 100–115. [Google Scholar] [CrossRef]
- Naeem, F.; Habib, N.; Gul, M.; Khalid, M.; Saeed, S.; Farooq, S.; Munshi, T.; Gobbi, M.; Husain, N.; Ayub, M.; et al. A Qualitative Study to Explore Patients’, Carers’ and Health Professionals’ Views to Culturally Adapt CBT for Psychosis (CBTp) in Pakistan. Behav. Cogn. Psychother. 2016, 44, 43–55. [Google Scholar] [CrossRef]
- Naeem, F. Cultural Adaptations of CBT: A Summary and Discussion of the Special Issue on Cultural Adaptation of CBT. Cogn. Behav. Ther. 2019, 12. [Google Scholar] [CrossRef]
- Horrell, S.C.V. Effectiveness of Cognitive-Behavioral Therapy with Adult Ethnic Minority Clients: A Review. Prof. Psychol. Res. Pract. 2008, 39, 160–168. [Google Scholar] [CrossRef]
- Behn, A.; Davanzo, A.; Errázuriz, P. Client and Therapist Match on Gender, Age, and Income: Does Match within the Therapeutic Dyad Predict Early Growth in the Therapeutic Alliance? J. Clin. Psychol. 2018, 74, 1403–1421. [Google Scholar] [CrossRef]
- Chang, D.F.; Yoon, P. Ethnic Minority Clients’ Perceptions of the Significance of Race in Cross-Racial Therapy Relationships. Psychother. Res. 2011, 21, 567–582. [Google Scholar] [CrossRef]
- Sharf, J.; Primavera, L.H.; Diener, M.J. Dropout and Therapeutic Alliance: A Meta-Analysis of Adult Individual Psychotherapy. Psychother. 2010, 47, 637–645. [Google Scholar] [CrossRef]
- Wnuk, S.; McMain, S.; Links, P.S.; Habinski, L.; Murray, J.; Guimond, T. Factors Related to Dropout from Treatment in Two Outpatient Treatments for Borderline Personality Disorder. J. Pers. Disord. 2013, 27, 716–726. [Google Scholar] [CrossRef] [PubMed]
- Samstag, L.W.; Batchelder, S.T.; Muran, J.C.; Safran, J.D.; Winston, A. Early identification of treatment failures in short-term psychotherapy. An assessment of therapeutic alliance and interpersonal behavior. J. Psychothe. Prac. Res. 1998, 7, 126–143. [Google Scholar]
| N | M (SD) | Range | |
|---|---|---|---|
| 1. Client therapeutic alliance | 59 | 46.62 (8.14) | 25–60 |
| 2. Therapist therapeutic alliance | 60 | 36.14 (5.41) | 23–48 |
| 3. Suicidal ideation (pre-therapy) | 64 | 78.44 (31.86) | 9–129 |
| 4. Suicidal ideation (post-therapy) | 64 | 56.78 (35.87) | 0–137 |
| 5. Depression (pre-therapy) | 64 | 12.47 (4.62) | 3–21 |
| 6. Hopelessness (pre-therapy) | 64 | 13.19 (5.55) | 1–20 |
| 7. Suicide plans (pre-therapy) | 62 | 19.35 (42.70) | 0–180 |
| No suicide plans | 24 | 0 | 0 |
| One or more suicide plans | 38 | 38.58 (51.08) a | 1–180 |
| 8. Suicide plans (post-therapy) | 61 | 10.59 (34.01) | 0–180 |
| No suicide plans | 33 | 0 | 0 |
| One or more suicide plans | 28 | 23.07 (47.66) a | 1–180 |
| 9. Suicide attempts (pre-therapy) | 63 | 1.41 (6.33) | 0–50 |
| No suicide attempts | 43 | 0 | 0 |
| One or more suicide attempts | 20 | 4.45 (10.79) a | 1–50 |
| 10. Suicide attempts (post-therapy) | 62 | 0.68 (2.89) | 0–21 |
| No suicide attempts | 53 | 0 | 0 |
| One or more suicide attempts | 9 | 4.67 (6.54) a | 1–21 |
| Continuous Variables | N | M (SD) | Range | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| 1. Client therapeutic alliance | 59 | 46.62 (8.14) | 25–60 | −0.12 | −0.33 * | −0.17 | −0.18 |
| 2. Suicidal ideation (pre-therapy) | 59 | 77.03 (32.07) | 9–129 | - | 0.48 * | 0.41 * | 0.61 * |
| 3. Suicidal ideation (post-therapy) | 59 | 57.14 (36.92) | 0–137 | - | 0.23 | 0.44 * | |
| 4. Depression (pre-therapy) | 59 | 12.29 (4.54) | 3–21 | - | 0.53 * | ||
| 5. Hopelessness (pre-therapy) | 59 | 12.80 (5.56) | 1–20 | - |
| Model | B (95% CI) | SE B | β | p | |
|---|---|---|---|---|---|
| Model 1 a: outcome of post-therapy suicidal ideation | Step 1 | ||||
| Constant | 127.42 (73.73, 181.11) | 26.81 | 0.000 | ||
| Client WAI-SR | −1.51 (−2.64, −0.37) | 0.57 | −0.33 | 0.010 | |
| Model 2 b: outcome of post-therapy suicidal ideation, whilst controlling for baseline suicidal ideation | Step 1 | ||||
| Constant | 14.53 (−7.79, 36.85) | 11.15 | 0.198 | ||
| ASIQ (pre-therapy) | 0.55 (0.29, 0.82) | 0.13 | 0.48 | 0.001 | |
| Step 2 | |||||
| Constant | 76.80 (22.73, 130.86) | 26.99 | 0.006 | ||
| ASIQ (pre-therapy) | 0.52 (0.29, 0.77) | 0.13 | 0.45 | 0.001 | |
| Client WAI-SR | −1.27 (−2.29, −0.26) | 0.51 | −0.28 | 0.015 | |
| Model 3 c: outcome of post-therapy suicidal ideation, whilst controlling for baseline suicidal ideation, depression, and hopelessness | Step 1 | ||||
| Constant | 14.53 (−7.79, 36.85) | 11.15 | 0.198 | ||
| ASIQ (pre-therapy) | 0.55 (0.29, 0.82) | 0.13 | 0.48 | 0.001 | |
| Step 2 | |||||
| Constant | 9.31 (−18.30, 36.92) | 13.78 | 0.502 | ||
| ASIQ (pre-therapy) | 0.40 (0.06, 0.73) | 0.17 | 0.34 | 0.023 | |
| CDSS (pre-therapy) | −0.35 (−2.59, 1.89) | 1.12 | −0.04 | 0.753 | |
| BHS (pre-therapy) | 1.70 (−0.40, 3.79) | 1.05 | 0.26 | 0.110 | |
| Step 3 | |||||
| Constant | 70.98 (11.96, 130.00) | 29.44 | 0.019 | ||
| ASIQ (pre-therapy) | 0.40 (0.07, 0.72) | 0.16 | 0.34 | 0.018 | |
| CDSS (pre-therapy) | −0.58 (−2.74, 1.58) | 1.08 | −0.07 | 0.591 | |
| BHS (pre-therapy) | 1.49 (−0.54, 3.51) | 1.01 | 0.22 | 0.148 | |
| Client WAI-SR | −1.21 (−2.23, −0.18) | 0.51 | −0.27 | 0.023 |
| Model | b (95% CI) | SE B | t | p | |
|---|---|---|---|---|---|
| Model 1 a: baseline suicidal ideation controlled for | Constant | 16.80 (−5.33, 38.93) | 11.04 | 1.52 | 0.198 |
| Client WAI-SR (centered) | −1.14 (−2.18, −0.10) | 0.52 | −2.20 | 0.032 | |
| Total number of minutes of therapy (centered) | 0.003 (−0.03, 0.03) | 0.02 | 0.12 | 0.861 | |
| Client WAI-SR x Total number of minutes of therapy | 0.003 (−0.0003, 0.007) | 0.01 | 1.85 | 0.07 | |
| ASIQ (pre-therapy) | 0.51 (0.24, 0.78) | 0.13 | 3.81 | 0.001 | |
| Model 2 b: baseline suicidal ideation, depression and hopelessness controlled for | Constant | 19.41 (−10.92, 47.74) | 14.62 | 1.26 | 0.214 |
| Client WAI-SR (centered) | −1.13 (−2.19, −0.07) | 0.53 | −2.13 | 0.038 | |
| Total number of minutes of therapy (centered) | 0.002 (−0.03, 0.04) | 0.02 | 0.13 | 0.896 | |
| Client therapeutic alliance x Total number of minutes of therapy | 0.003 (−0.0003, 0.007) | 0.01 | 1.57 | 0.123 | |
| ASIQ (pre-therapy) | 0.45 (0.12, 0.78) | 0.17 | 2.71 | 0.009 | |
| CDSS (pre-therapy) | −0.85 (−3.06, 1.37) | 1.10 | −0.77 | 0.446 | |
| BHS (pre-therapy) | 1.05 (−1.06, 3.16) | 1.05 | 1.00 | 0.322 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huggett, C.; Gooding, P.; Haddock, G.; Pratt, D. The Relationship between the Therapeutic Alliance and Suicidal Experiences in People with Psychosis Receiving Therapy. Int. J. Environ. Res. Public Health 2021, 18, 10706. https://doi.org/10.3390/ijerph182010706
Huggett C, Gooding P, Haddock G, Pratt D. The Relationship between the Therapeutic Alliance and Suicidal Experiences in People with Psychosis Receiving Therapy. International Journal of Environmental Research and Public Health. 2021; 18(20):10706. https://doi.org/10.3390/ijerph182010706
Chicago/Turabian StyleHuggett, Charlotte, Patricia Gooding, Gillian Haddock, and Daniel Pratt. 2021. "The Relationship between the Therapeutic Alliance and Suicidal Experiences in People with Psychosis Receiving Therapy" International Journal of Environmental Research and Public Health 18, no. 20: 10706. https://doi.org/10.3390/ijerph182010706
APA StyleHuggett, C., Gooding, P., Haddock, G., & Pratt, D. (2021). The Relationship between the Therapeutic Alliance and Suicidal Experiences in People with Psychosis Receiving Therapy. International Journal of Environmental Research and Public Health, 18(20), 10706. https://doi.org/10.3390/ijerph182010706







