Caregivers’ Knowledge and Food Accessibility Contributes to Childhood Malnutrition: A Case Study of Dora Nginza Hospital, South Africa
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Study Setting
2.3. Sample Size Calculation and Sampling Technique
2.4. Data Collection Procedure and Variables Measured
2.5. Ethical Clearance
2.6. Data Analysis
3. Results
3.1. Socio-Demographic Characteristics
3.2. Caregivers’ Nutrition Knowledge
3.3. Household Food Insecurity Measured Using Food Availability and Accessibility
3.4. Anthropometry
3.5. Relationship between Socio-Demographic Characteristics, Food Security, Caregivers’ Nutrition Knowledge, and Anthropometry
4. Discussion
5. Limitation of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. The Double Burden of Malnutrition. Policy Brief; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Oenema, S.; Campeau, C.; Delmuè, D. (Eds.) A Spotlight on the Nutrition Decade, 42nd ed.; UNSCN: Rome, Italy, 2017; pp. 9–15. Available online: https://www.unscn.org/uploads/web/news/UNSCN-News42-with-Programme-News.pdf (accessed on 5 January 2018).
- Anon. Double Burden of Malnutrition. 2018. Available online: http://www.who.int/nutrition/double-burden-malnutrition/en/ (accessed on 5 January 2018).
- UNICEF. Statistical Data on the Status of Children Aged 0–4 Years in South Africa. 2007. Available online: https://www.unicef.org/southafrica/SAF_resources_younglives.pdf (accessed on 5 January 2018).
- Tzioumis, E.; Adair, L.S. Childhood dual burden of under-and overnutrition in low-and middle-income countries: A critical review. Food Nutr. Bull. 2014, 35, 230–243. [Google Scholar] [CrossRef] [Green Version]
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P.; et al. The South African National Health and Nutrition Examination Survey, 2012: SANHANES-1: The Health and Nutritional Status of the Nation. 2014. Available online: https://repository.hsrc.ac.za/handle/20.500.11910/2864 (accessed on 6 January 2018).
- De Valença, A.W.; Bake, A.; Brouwer, I.D.; Giller, K.E. Agronomic biofortification of crops to fight hidden hunger in sub-Saharan Africa. Glob. Food Sec. 2017, 12, 8–14. [Google Scholar] [CrossRef]
- Zuma, M.K.; Kolanisi, U.; Modi, A.T. The potential of integrating provitamin A-biofortified maize in smallholder farming systems to reduce malnourishment in South Africa. Int. J. Environ. Res. Public Health 2018, 15, 805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Devereux, S.; Waidler, J. Why Does Malnutrition Persist in South Africa Despite Social Grants? Food Security SA Working Paper Series No.001. DST-NRF; Centre of Excellence in Food Security: Cape Town, South Africa, 2017. [Google Scholar]
- Misselhorn, A.; Hendriks, S. A systematic review of sub-national food insecurity research in South Africa: Missed opportunities for policy insights. PLoS ONE 2017, 12, e0182399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chakona, G.; Shackleton, C. Food insecurity in South Africa: To what extent can social grants and consumption of wild foods eradicate hunger? World Dev. Perspect. 2019, 1, 87–94. [Google Scholar] [CrossRef]
- Mbhenyane, X.G. Indigenous foods and their contribution to nutrient requirements. South Afr. J. Clin. Nutr. 2017, 30, 5–7. [Google Scholar]
- UNICEF. The State of the World’s Children. 2012. Available online: https://www.unicef.org/sowc2012/pdfs/SOWC-2012-Main-Report_EN_21Dec2011.pdf (accessed on 6 January 2018).
- Gundersen, C.; Kreider, B.; Pepper, J. Partially Identifying the Impact of the Supplemental Nutrition Assistance Program on food Insecurity Among Children: Addressing Endogeneity and Misreporting Using the SIPP; Working Paper; National Poverty Center: Ann Arbor, MI, USA, 27 January 2011. [Google Scholar]
- Wight, V.; Kaushal, N.; Waldfogel, J.; Garfinkel, I. Understanding the link between poverty and food insecurity among children: Does the definition of poverty matter? J. Child. Poverty 2014, 20, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Pickett, W.; Michaelson, V.; Davison, C. Beyond nutrition: Hunger and its impact on the health of young Canadians. Int. J. Public Health 2015, 60, 527–538. [Google Scholar] [CrossRef] [Green Version]
- Arthur, S.; Nyide, B.; Soura, A.; Kahn, K.; Weston, M.; Sankoh, O. Tackling malnutrition: A systematic review of 15-year research evidence from INDEPTH health and demographic surveillance systems. Glob. Health Action 2015, 8, 28298. [Google Scholar] [CrossRef] [Green Version]
- Kavosi, E.; Hassanzadeh Rostami, Z.; Nasihatkon, A.; Moghadami, M.; Heidari, M. Prevalence and Determinants of Under-Nutrition Among Children Under Six: A Cross-Sectional Survey in Fars Province, Iran. Int. J. Health Policy Manag. 2014, 3, 71–76. [Google Scholar] [CrossRef]
- UNICEF. UNICEF Programme Guidance for Early Childhood Development. Programme Division. 2016. Available online: https://www.unicef.org/earlychildhood/files/FINAL_ECD_Programme_Guidance._September._2017.pdf (accessed on 5 March 2018).
- Branca, F.; Lartey, A. Ending malnutrition in all its forms? A Decade of Opportunity. World Health Organisation. 2016. Available online: http://www.who.int/mediacentre/commentaries/ending-malnutrition-opportunity/en/ (accessed on 8 January 2018).
- Rahman, M.; Howlader, T.; Masud, M.; Rahman, M. Association of Low-Birth Weight with Malnutrition in Children under Five Years in Bangladesh: Do Mother’s Education, Socio-Economic Status, and Birth Interval Matter? PLoS ONE 2016, 11, e0157814. [Google Scholar] [CrossRef] [Green Version]
- Christian, P.; Lee, S.E.; Donahue Angel, M.; Adair, L.S.; Arifeen, S.E.; Ashorn, P.; Barros, F.C.; Fall, C.H.; Fawzi, W.W.; Hao, W.; et al. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low-and middle-income countries. Int. J. Epidemiol. 2013, 42, 1340–1355. [Google Scholar] [CrossRef]
- Prendergast, A.; Humphrey, J. The stunting syndrome in developing countries. Paediatr. Int. Child Health 2014, 34, 250–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, A.I.; Kabir, I.; Ekström, E.C.; Åsling-Monemi, K.; Alam, D.S.; Frongillo, E.A.; Yunus, M.; Arifeen, S.; Persson, L.Å. Effects of prenatal food and micronutrient supplementation on child growth from birth to 54 months of age: A randomized trial in Bangladesh. Nutr. J. 2011, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tette, E.; Sifah, E.; Nartey, E. Factors affecting malnutrition in children and the uptake of interventions to prevent the condition. BMC Pediatrics 2015, 15, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mkhize, M.; Sibanda, M. A review of selected studies on the factors associated with the nutrition status of children under the age of five years in South Africa. J. Environ. Res. Public Health 2020, 17, 7973. [Google Scholar] [CrossRef] [PubMed]
- SADHS. Key Indicator Report, Statistics South Africa; Statistics South Africa: Pretoria, South Africa, 2017.
- StatsSA. Census 2011 Municipal Fact Sheet. 2012. Available online:http://www.hst.org.za/publications/District%20Health%20Barometers/16%20(Section%20B)%20Eastern%20Cape%20Province.pdf (accessed on 13 February 2018).
- McLaren, S.; Steenkamp, L.; Feeley, A.; Nyarko, J.; Venter, D. Food insecurity, social welfare and low birth weight: Implications for childhood malnutrition in an urban Eastern Cape Province township. South Afr. J. Child Health 2018, 12, 95–99. [Google Scholar]
- Deitchler, M.; Swindale, A.; Coates, J.; Ballard, T. Household Hunger Scale: Indicator Definition and Measurement Guide; Food and Nutrition Technical Assistance II Project, FHI 360: Washington, DC, USA, 2011. [Google Scholar]
- ADSA. Anthropometry Guideline Paediatrics. Cape Town Metropole Paediatric Interest Group. 2009. Available online: http://www.adsa.org.za/Portals/14/Documents/Clinical20Guideline20Anthropometry.pdf (accessed on 10 January 2018).
- Stewart, A.; Marfell-Jones, M. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Lower Hutt, New Zealand, 2011. [Google Scholar]
- Cashin, K.; Oot, L. Guide to Anthropometry: A Practical Tool for Program Planners, Managers, and Implementers; Food and Nutrition Technical Assistance III Project (FANTA)/FHI 360: Washington, DC, USA, 2018. [Google Scholar]
- WHO. Training Course on Child Growth Assessment; Geneva. 2008. Available online: http://www.who.int/childgrowth/training/module_b_measuringgrowth.pdf (accessed on 7 April 2018).
- Owoaje, E.; Onifade, O.; Desmennu, A. Family and socio-economic risk factors for undernutrition among children aged 6 to 23 Months in Ibadan, Nigeria. Pan Afr. Med. J. 2014, 17, 161. [Google Scholar] [CrossRef] [PubMed]
- Daelmans, B.; Mangasaryan, N.; Martines, J.; Saadeh, R.; Casanovas, C.; Arabi, M. Strengthening Actions to Improve Feeding of Infants and Young Children 6 to 23 Months of Age: Summary of a Recent World Health Organization/UNICEF Technical Meeting, Geneva, 6–9 October 2008. Food Nutr. Bull. 2009, 30 (Suppl. 2), S236–S238. [Google Scholar] [CrossRef] [Green Version]
- Vorster, H. The link between poverty and malnutrition: A South African perspective. Health SA Gesondheid 2010, 15. [Google Scholar] [CrossRef]
- Piniel, A. Factors contributing to severe acute malnutrition among the under five children in Francistown-Botswana. Master’s Thesis, University of the Western Cape, Cape Town, South Africa, 2016; pp. 16–32. [Google Scholar]
- Barnes, H.; Hall, K.; Sambu, W.; Wright, G.; Zembe- Mkabile, W. Review of Research Evidence on Child Poverty in South Africa: Policy Brief Series; PSPPD. Barometer 2007/08; Health Systems Trust: Durban, South Africa, 2017. [Google Scholar]
- StatsSA. National poverty lines. 2018. Available online: www.statssa.gov.za (accessed on 8 May 2019).
- Farzana, F.; Rahman, A.; Sultana, S.; Raihan, M.; Haque, M.; Waid, J.; Choudhury, N.; Ahmed, T. Coping strategies related to food insecurity at the household level in Bangladesh. PLoS ONE 2017, 12, e0171411. [Google Scholar] [CrossRef] [PubMed]
- Belaynew, W.B. Assessment of Factors Associated with Malnutrition among Under Five Years Age Children at Machakel Woreda, Northwest Ethiopia: A Case Control Study. J. Nutr. Food Sci. 2014. [Google Scholar] [CrossRef] [Green Version]
- StatsSA. Provincial Profile: Eastern Cape, Census 2011. 2011. Available online: http://www.statssa.gov.za/publications/Report-03-01-71/Report-03-01-712011.pdf (accessed on 8 January 2018).
- Labadarios, D.; Mchiza, Z.; Steyn, N.; Gericke, G.; Maunder, E.; Davids, Y.; Parker, W. Food security in South Africa: A review of national surveys. Bull. World Health Organ. 2011, 89, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Dubois, L.; Ohm Kyvik, K.; Girard, M.; Tatone-Tokuda, F.; Pérusse, D.; Hjelmborg, J.; Skytthe, A.; Rasmussen, F.; Wright, M.; Lichtenstein, P.; et al. Genetic and Environmental Contributions to Weight, Height, and BMI from Birth to 19 Years of Age: An International Study of Over 12,000 Twin Pairs. PLoS ONE 2012, 7, e30153. [Google Scholar] [CrossRef] [PubMed]
- Duggal, P.; William, A.; Petri, J. Does malnutrition have a genetic component? Annu. Rev. Genom. Hum. Genet. 2018, 19, 247–262. [Google Scholar] [CrossRef] [PubMed]
- Psaki. Household Food Insecurity Access Scale (HFIAS): Guiding Framework. 2012. Available online: https://pdfs.semanticscholar.org/72e4/5f0fa7e142c1a55aa65d8ebb7056a77aaac2.pdf (accessed on 22 May 2019).
- Roba, K.; O’Connor, T.; O’Brien, N.; Aweke, C. Seasonal variations in household food insecurity and dietary diversity and their association with maternal and child nutritional status in rural Ethiopia. Food Sec. 2019, 11, 651–664. [Google Scholar] [CrossRef]
- Gavhi, F.; Kuonza, L.; Musekiwa, A.; Motaze, N.V. Factors associated with mortality in children under five years old hospitalized for Severe Acute Malnutrition in Limpopo province, South Africa, 2014–2018: A cross-sectional analytic study. PLoS ONE 2020, 15, e0232838. [Google Scholar] [CrossRef]
- Budree, S.; Goddard, E.; Brittain, K.; Cader, S.; Myer, L.; Zar, H.J. Infant feeding practices in a South African birth cohort—A longitudinal study. Matern. Child Nutr. 2017, 13, e12371. [Google Scholar] [CrossRef]


| Province | % Stunting |
|---|---|
| Gauteng | 34 |
| Free state | 34 |
| KwaZulu-Natal | 29 |
| Northwest | 27 |
| Eastern Cape | 25 |
| Western Cape | 23 |
| Limpopo | 22 |
| Mpumalanga | 22 |
| Northern Cape | 21 |
| Characteristics of Caregivers | Caregivers (%) | Children (%) |
|---|---|---|
| Participants Gender | ||
| Male | 6 (3.3) | 97 (52.7) |
| Female | 178 (96.7) | 87 (47.3) |
| Ethnicity | ||
| African | 107 (58.2) | 108 (58.7) |
| Coloured | 69 (37.5) | 68 (37) |
| Caucasian | 6 (3.3) | 6 (3.3) |
| Indian | 1 (0.5) | 1 (0.5) |
| Other (prefer not to be classified) | 1 (0.5) | 1 (0.5) |
| Level of School Completed | ||
| Grade 3 or less | 3 (1.6) | - |
| Grade 6 | 9 (4.9) | - |
| Grade 9 | 51 (27.8) | - |
| Grade 12 | 97 (52.7) | - |
| Any tertiary education | 24 (13) | - |
| Age Categories (years) | ||
| 16–25 | 52 (28.3) | |
| 26–35 | 85 (46.2) | |
| 36–40 | 18 (9.8) | |
| >40 | 29 (15.7) | |
| Employment | ||
| Unemployed | 129 (70.1) | - |
| Employed (part- or full-time) | 48 (26.1) | - |
| Studying | 7 (3.8) | - |
| Number of Children in the Household | ||
| 2 | 130 (70.6) | - |
| 4 | 51 (27.8) | - |
| 5–6 | 3 (1.6) | - |
| Nutrition Knowledge of Caregiver | Frequency (n) | Percentage (%) |
|---|---|---|
| Which food is the best for a baby younger than 6 months? | ||
| Breastmilk (correct answer) | 159 | 87.8 |
| Infant formula | 3 | 1.7 |
| Breast- and formula milk | 12 | 6.6 |
| Soft porridge | 6 | 3.3 |
| Do not know | 1 | 0.6 |
| Ideal duration of breastfeeding | ||
| 24 months + (correct answer) | 58 | 32 |
| < 6 months | 21 | 11.7 |
| 6 to 12 months | 34 | 18.8 |
| 12 to 18 months | 33 | 18.2 |
| 19 to 23 months | 31 | 17.1 |
| Do not know | 4 | 2.2 |
| Suitable substitute for porridge | ||
| Rice or bread (correct answer) | 44 | 24.3 |
| Meat or milk | 17 | 9.4 |
| Banana or mango | 30 | 16.6 |
| Cabbage or pumpkin | 85 | 47 |
| Do not know | 5 | 2.7 |
| Suitable meat alternative | ||
| Legumes (correct answer) | 17 | 9.2 |
| Spinach | 60 | 32.6 |
| Potatoes | 101 | 54.9 |
| Do not know | 3 | 1.6 |
| Amount of dairy needed/day for children 2 to 5 years | ||
| 1.5 to > 2.5 cups (correct answer) | 124 | 68.5 |
| 0.5 to 1 cup | 29 | 16 |
| Do not know | 28 | 15.5 |
| Suitable milk alternative | ||
| Cheese (correct answer) | 50 | 27.7 |
| Coffee creamer | 18 | 9.9 |
| Peanut butter | 94 | 51.9 |
| Do not know | 19 | 10.5 |
| Number of times a child of 2 to 5 years old should eat per day | ||
| Three or more (correct answer) | 166 | 91.7 |
| Once | 1 | 0.6 |
| Twice | 10 | 5.5 |
| Do not know | 4 | 2.2 |
| Sources of nutrition information (more than one option was allowed | ||
| Clinic/community health centre | 86 | 47.5 |
| Friends/family | 52 | 28.7 |
| Television, radio, newspaper, magazine | 42 | 23.2 |
| Own experience | 29 | 16 |
| Internet | 9 | 5 |
| Household Food Insecurity Scale Questions | Frequency (n) (‘yes’ answers) | Percentage (%) |
|---|---|---|
| During the past 30 days: | ||
| Did you worry that your household would not have enough food? | 113 | 61.4 |
| Were you or a household member unable to eat the types of food you like more? | 86 | 46.7 |
| Did you or a household member have to eat a small variety of food? | 90 | 48.9 |
| Did you or a household member have to eat foods that you really did not want to eat? | 76 | 41.3 |
| Did you or a household member have to eat a smaller meal than you needed? | 77 | 41.8 |
| Did you or a household member have to eat fewer meals in a day? | 67 | 36.4 |
| Was there ever no food to eat due to lack of resources? | 29 | 15.8 |
| Did you or a household member sleep hungry because of lack of food? | 23 | 12.5 |
| Did you or a household member go a whole day and night without eating anything because there was no food? | 19 | 10.3 |
| Anthropometry as per Z-Scores | Frequency (n) | Percentage (%) |
|---|---|---|
| Weight for age (WAZ) | ||
| Severely underweight for age, < −3 | 13 | 7.1 |
| Moderate underweight for age, −3 to < −2 | 12 | 6.5 |
| Normal, ≥ −2 | 159 | 86.4 |
| Height for age (HAZ) | ||
| Severely stunted, < −3 | 23 | 12.5 |
| Moderately stunted, −3 to < −2 | 24 | 13.1 |
| Normal, ≥ −2 | 137 | 74.4 |
| Weight for height (WHZ) * (n = 181) | ||
| SAM, < −3 | 5 | 2.8 |
| MAM, −3 to < −2 | 7 | 3.9 |
| At risk of wasting, −2 to ˂ −1 | 24 | 13.3 |
| Normal, −1 to ˂ 1 | 104 | 57.4 |
| At risk of overweight, 1 to ˂ 2 | 28 | 15.4 |
| Overweight, 2 to < 3 | 10 | 5.5 |
| Obese, > 3 | 3 | 1.7 |
| MUAC (n = 106) | ||
| MAM, (11 to 12.5 cm) | 4 | 4 |
| At risk of malnutrition, (12.5 to 13.5 cm) | 11 | 10 |
| Normal, (> 13.5 cm) | 91 | 86 |
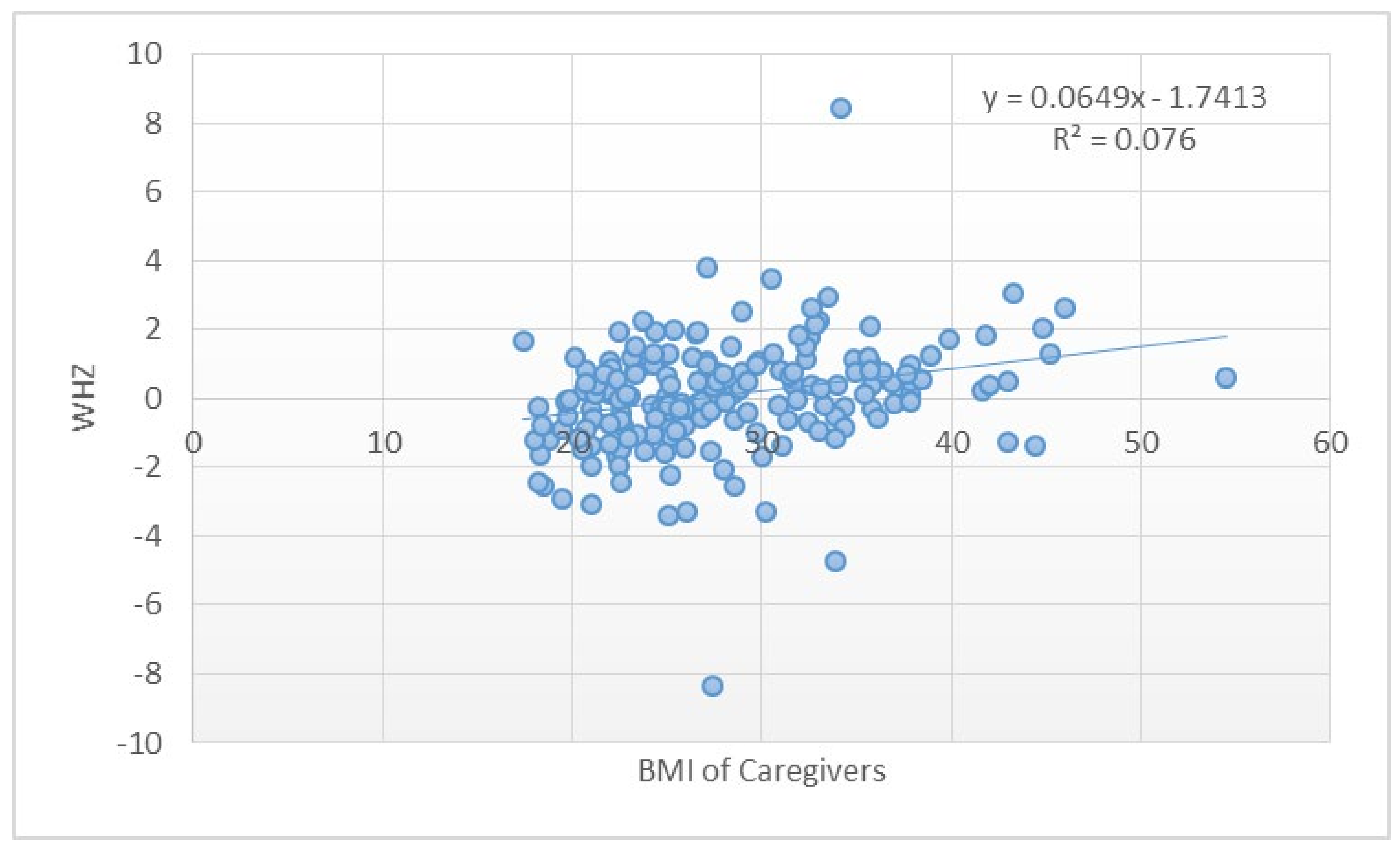
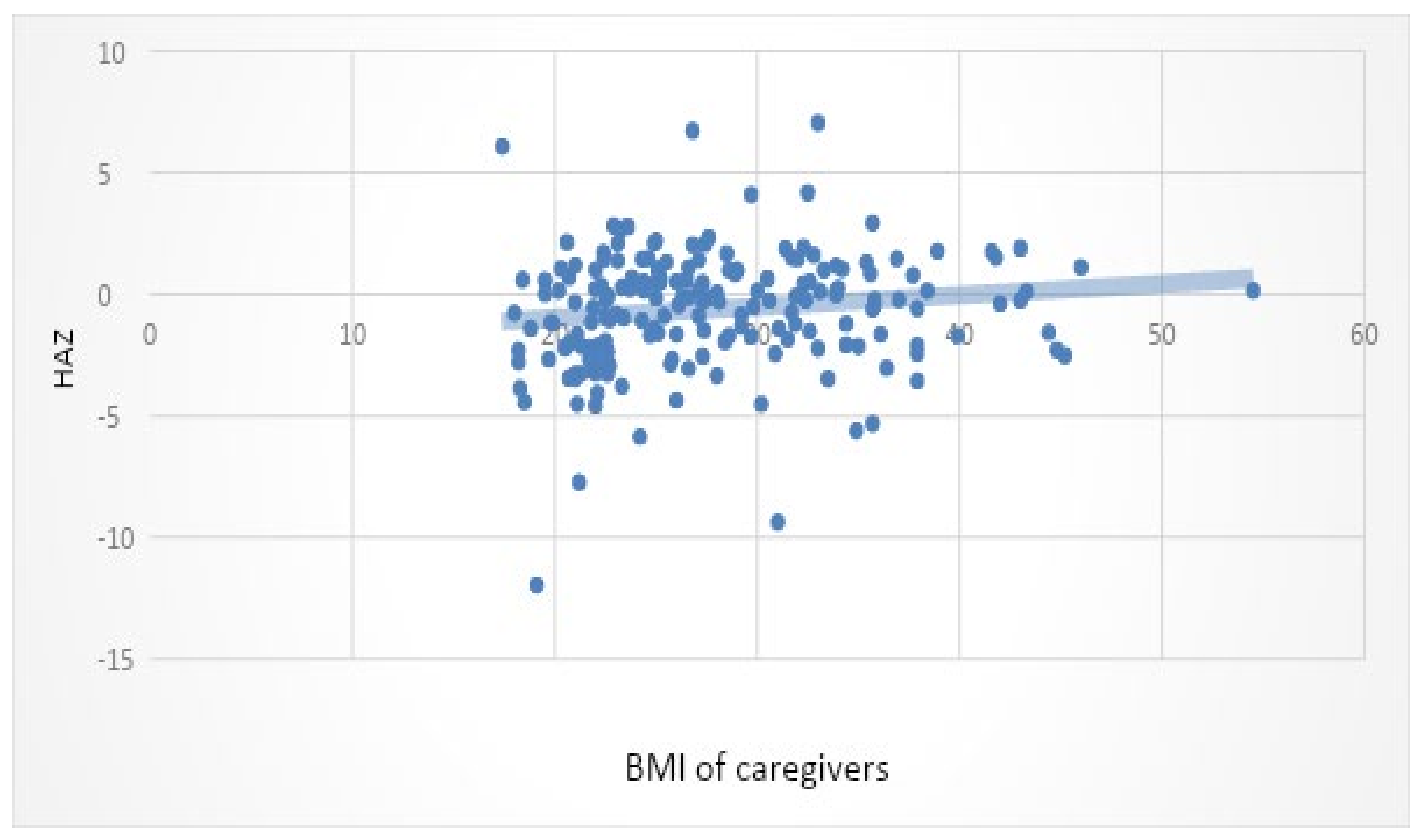
| Variables | Pearson-r | p-Value | |
|---|---|---|---|
| HAZ | MUAC | 0.14 | 0.0001 *** |
| BMI of caregivers | 0.018 | 0.009 ** | |
| WHZ | MUAC | 0.23 | 0.000 *** |
| BMI of caregivers | 0.08 | 0.0001 *** | |
| WAZ | MUAC | 0.30 | 0.0001 *** |
| Gestational age | 0.02 | 0.038 * | |
| MUAC | Child’s appetite | 0.01 | 0.000 *** |
| Receiving grant | 0.01 | 0.000 *** | |
| Household income | 0.004 | 0.000 *** | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clarke, P.; Zuma, M.K.; Tambe, A.B.; Steenkamp, L.; Mbhenyane, X.G. Caregivers’ Knowledge and Food Accessibility Contributes to Childhood Malnutrition: A Case Study of Dora Nginza Hospital, South Africa. Int. J. Environ. Res. Public Health 2021, 18, 10691. https://doi.org/10.3390/ijerph182010691
Clarke P, Zuma MK, Tambe AB, Steenkamp L, Mbhenyane XG. Caregivers’ Knowledge and Food Accessibility Contributes to Childhood Malnutrition: A Case Study of Dora Nginza Hospital, South Africa. International Journal of Environmental Research and Public Health. 2021; 18(20):10691. https://doi.org/10.3390/ijerph182010691
Chicago/Turabian StyleClarke, Pamela, Mthokozisi Kwazi Zuma, Ayuk Betrand Tambe, Liana Steenkamp, and Xikombiso Gertrude Mbhenyane. 2021. "Caregivers’ Knowledge and Food Accessibility Contributes to Childhood Malnutrition: A Case Study of Dora Nginza Hospital, South Africa" International Journal of Environmental Research and Public Health 18, no. 20: 10691. https://doi.org/10.3390/ijerph182010691
APA StyleClarke, P., Zuma, M. K., Tambe, A. B., Steenkamp, L., & Mbhenyane, X. G. (2021). Caregivers’ Knowledge and Food Accessibility Contributes to Childhood Malnutrition: A Case Study of Dora Nginza Hospital, South Africa. International Journal of Environmental Research and Public Health, 18(20), 10691. https://doi.org/10.3390/ijerph182010691






