Outcomes of Scarf and Akin Osteotomy with Intra-Articular Stepwise Lateral Soft Tissue Release for Correcting Hallux Valgus Deformity in Rheumatoid Arthritis
Abstract
:1. Introduction
2. Patients and Methods
2.1. Patients
2.2. Radiographic and Clinical Assessments
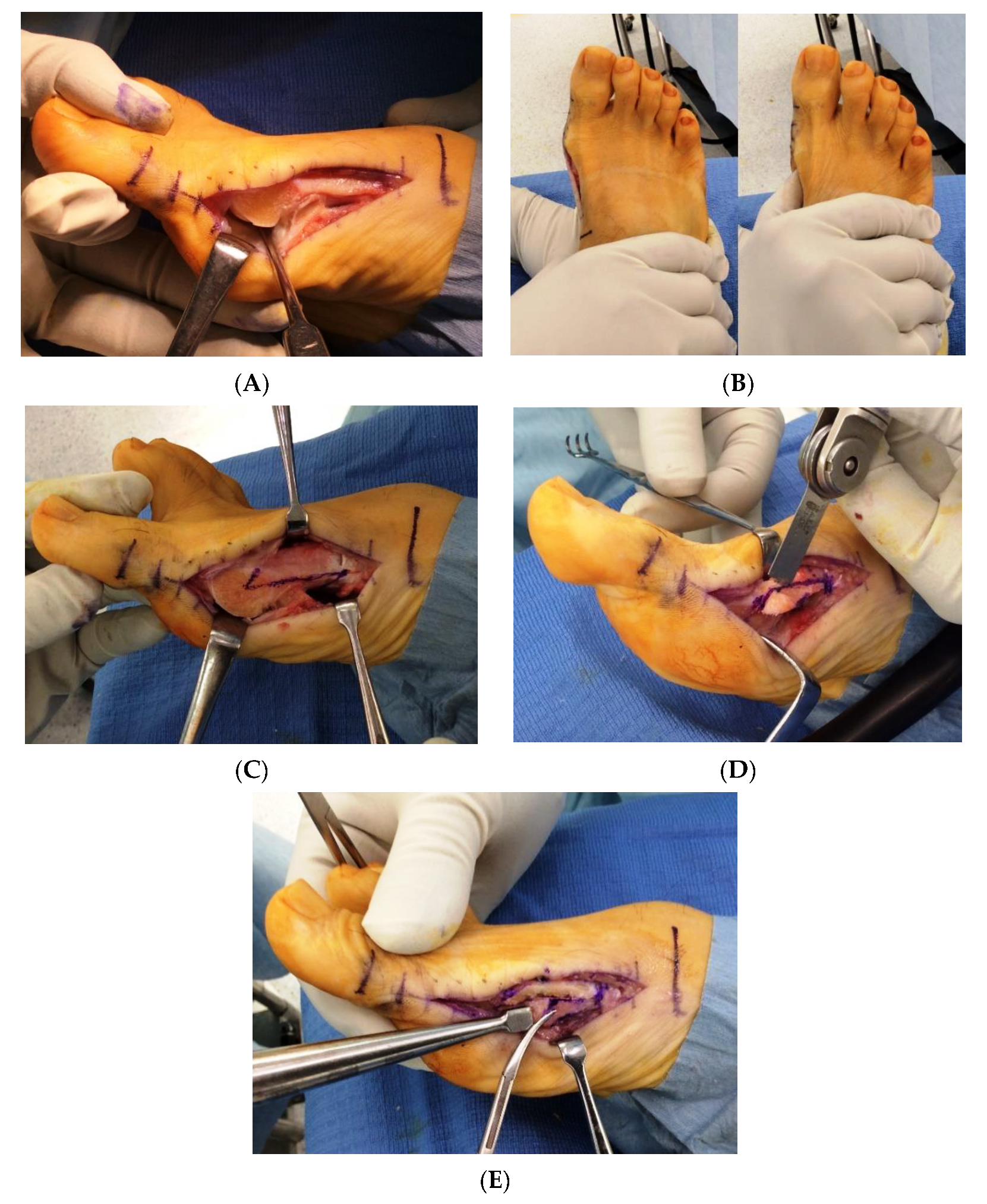
2.3. Surgical Technique
2.4. Postoperative Care
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- López-López, D.; Pérez-Ríos, M.; Ruano-Ravina, A.; Losa-Iglesias, M.E.; Becerro-de-Bengoa-Vallejo, R.; Romero-Morales, C.; Calvo-Lobo, C.; Navarro-Flores, E. Impact of quality of life related to foot problems: A case-control study. Sci. Rep. 2021, 11, 14515. [Google Scholar] [CrossRef]
- Rojas-Villarraga, A.; Bayona, J.; Zuluaga, N.; Mejia, S.; Hincapie, M.E.; Anaya, J.M. The impact of rheumatoid foot on disability in Colombian patients with rheumatoid arthritis. BMC Musculoskelet. Disord. 2009, 10, 67. [Google Scholar] [CrossRef] [Green Version]
- Momohara, S.; Inoue, E.; Ikari, K.; Ochi, K.; Ishida, O.; Yano, K.; Sakuma, Y.; Yoshida, S.; Koyama, T.; Koenuma, N.; et al. Recent trends in orthopedic surgery aiming to improve quality of life for those with rheumatoid arthritis: Data from a large observational cohort. J. Rheumatol. 2014, 41, 862–866. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Nishino, J.; Izawa, N.; Naito, M.; Hirose, J.; Tanaka, S.; Yasui, T.; Saisho, K.; Tohma, S. Trends in Treatment, Outcomes, and Incidence of Orthopedic Surgery in Patients with Rheumatoid Arthritis: An Observational Cohort Study Using the Japanese National Database of Rheumatic Diseases. J. Rheumatol. 2017, 44, 1575–1582. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, P. An operation for severe grades of contracted or clawed toes. Am. J. Orthop. Surg. 1912, 9, 441–449. [Google Scholar] [CrossRef]
- Matsumoto, T.; Kadono, Y.; Nishino, J.; Nakamura, K.; Tanaka, S.; Yasui, T. Midterm results of resection arthroplasty for forefoot deformities in patients with rheumatoid arthritis and the risk factors associated with patient dissatisfaction. J. Foot Ankle Surg. 2014, 53, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Ebina, K.; Hirao, M.; Takagi, K.; Ueno, S.; Morimoto, T.; Matsuoka, H.; Kitaguchi, K.; Iwahashi, T.; Hashimoto, J.; Yoshikawa, H. Comparison of the effects of forefoot joint-preserving arthroplasty and resection-replacement arthroplasty on walking plantar pressure distribution and patient-based outcomes in patients with rheumatoid arthritis. PLoS ONE 2017, 12, e0183805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yano, K.; Ikari, K.; Tobimatsu, H.; Tominaga, A.; Okazaki, K. Joint-Preserving Surgery for Forefoot Deformities in Patients with Rheumatoid Arthritis: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 4093. [Google Scholar] [CrossRef] [PubMed]
- Yano, K.; Saito, H.; Ikari, K.; Okazaki, K. Impact of joint-preserving surgery on plantar pressure among patients with rheumatoid arthritis. Mod. Rheumatol. 2020, 30, 604–606. [Google Scholar] [CrossRef] [PubMed]
- Iselin, L.D.; Munt, J.; Symeonidis, P.D.; Klammer, G.; Chehade, M.; Stavrou, P. Operative management of common forefoot deformities: A representative survey of Australian orthopaedic surgeons. Foot Ankle Spec. 2012, 5, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Berg, R.; Kelder, W.; Olsthoorn, R.; Poll, R. Scarf and Weil osteotomies for correction of rheumatoid forefoot deformities: A review of 20 cases. Foot Ankle Surg. 2007, 13, 35–40. [Google Scholar] [CrossRef]
- Barouk, L.S.; Barouk, P. Joint-preserving surgery in rheumatoid forefoot: Preliminary study with more-than-two-year follow-up. Foot Ankle Clin. 2007, 12, 435–454. [Google Scholar] [CrossRef] [PubMed]
- Bhavikatti, M.; Sewell, M.D.; Al-Hadithy, N.; Awan, S.; Bawarish, M.A. Joint preserving surgery for rheumatoid forefoot deformities improves pain and corrects deformity at midterm follow-up. Foot 2012, 22, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Chao, J.C.; Charlick, D.; Tocci, S.; Brodsky, J.W. Radiographic and clinical outcomes of joint-preserving procedures for hallux valgus in rheumatoid arthritis. Foot Ankle Int. 2013, 34, 1638–1644. [Google Scholar] [CrossRef] [PubMed]
- Kushioka, J.; Hirao, M.; Tsuboi, H.; Ebina, K.; Noguchi, T.; Nampei, A.; Tsuji, S.; Akita, S.; Hashimoto, J.; Yoshikawa, H. Modified Scarf Osteotomy with Medial Capsule Interposition for Hallux Valgus in Rheumatoid Arthritis: A Study of Cases Including Severe First Metatarsophalangeal Joint Destruction. J. Bone Jt. Surg. Am. 2018, 100, 765–776. [Google Scholar] [CrossRef]
- Yano, K.; Ikari, K.; Tobimatsu, H.; Okazaki, K. Patient-Reported and Radiographic Outcomes of Joint-Preserving Surgery for Rheumatoid Forefoot Deformities: A Retrospective Case Series with Mean Follow-up of 6 Years. J. Bone Jt. Surg. Am. 2021, 103, 506–516. [Google Scholar] [CrossRef]
- Smith, R.W.; Reynolds, J.C.; Stewart, M.J. Hallux valgus assessment: Report of research committee of American Orthopaedic Foot and Ankle Society. Foot Ankle 1984, 5, 92–103. [Google Scholar] [CrossRef]
- Niki, H.; Aoki, H.; Inokuchi, S.; Ozeki, S.; Kinoshita, M.; Kura, H.; Tanaka, Y.; Noguchi, M.; Nomura, S.; Hatori, M.; et al. Development and reliability of a standard rating system for outcome measurement of foot and ankle disorders I: Development of standard rating system. J. Orthop. Sci. 2005, 10, 457–465. [Google Scholar] [CrossRef] [Green Version]
- Niki, H.; Aoki, H.; Inokuchi, S.; Ozeki, S.; Kinoshita, M.; Kura, H.; Tanaka, Y.; Noguchi, M.; Nomura, S.; Hatori, M.; et al. Development and reliability of a standard rating system for outcome measurement of foot and ankle disorders II: Interclinician and intraclinician reliability and validity of the newly established standard rating scales and Japanese Orthopaedic Association rating scale. J. Orthop. Sci. 2005, 10, 466–474. [Google Scholar] [PubMed] [Green Version]
- Niki, H.; Tatsunami, S.; Haraguchi, N.; Aoki, T.; Okuda, R.; Suda, Y.; Takao, M.; Tanaka, Y. Validity and reliability of a self-administered foot evaluation questionnaire (SAFE-Q). J. Orthop. Sci. 2013, 18, 298–320. [Google Scholar] [CrossRef] [Green Version]
- Prevoo, M.L.; van’t Hof, M.A.; Kuper, H.H.; van Leeuwen, M.A.; van de Putte, L.B.; van Riel, P.L. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995, 38, 44–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leemrijse, T.; Maestro, M.; Tribak, K.; Gombault, V.; Devos Bevernage, B.; Deleu, P.A. Scarf osteotomy without internal fixation to correct hallux valgus. Orthop. Traumatol. Surg. Res. 2012, 98, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Takeda, R.; Maenohara, Y.; Chang, S.H.; Omata, Y.; Takuo, J.; Tanaka, S. Comparison between suture and staple fixations as internal fixation techniques for Akin osteotomy. Foot Ankle Surg. 2021. [Google Scholar] [CrossRef]
- Ebina, K.; Hirao, M.; Hashimoto, J.; Nampei, A.; Shi, K.; Tomita, T.; Futai, K.; Kunugiza, Y.; Noguchi, T.; Yoshikawa, H. Comparison of a self-administered foot evaluation questionnaire (SAFE-Q) between joint-preserving arthroplasty and resection-replacement arthroplasty in forefoot surgery for patients with rheumatoid arthritis. Mod. Rheumatol. 2017, 27, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, C.L.; Aper, R.L.; Brown, T.D. Anatomic determinants of first metatarsophalangeal flexion moments in hallux valgus. Clin. Orthop. Relat. Res. 1997, 339, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Peterson, D.A.; Zilberfarb, J.L.; Greene, M.A.; Colgrove, R.C. Avascular necrosis of the first metatarsal head: Incidence in distal osteotomy combined with lateral soft tissue release. Foot Ankle Int. 1994, 15, 59–63. [Google Scholar] [CrossRef]
- Park, Y.B.; Lee, K.B.; Kim, S.K.; Seon, J.K.; Lee, J.Y. Comparison of distal soft-tissue procedures combined with a distal chevron osteotomy for moderate to severe hallux valgus: First web-space versus transarticular approach. J. Bone Jt. Surg. Am. 2013, 95, e158. [Google Scholar] [CrossRef] [Green Version]
- Lee, W.C.; Kim, Y.M. Correction of hallux valgus using lateral soft-tissue release and proximal Chevron osteotomy through a medial incision. J. Bone Jt. Surg. Am. 2007, 89 (Suppl. 3), 82–89. [Google Scholar] [CrossRef]
- Simons, P.; Klos, K.; Loracher, C.; Skulev, H.K.; Gras, F.; Hofmann, G.O.; Fröber, R. Lateral soft-tissue release through a medial incision: Anatomic comparison of two techniques. Foot Ankle Surg. 2015, 21, 113–118. [Google Scholar] [CrossRef]
- Stamatis, E.D.; Huber, M.H.; Myerson, M.S. Transarticular distal soft-tissue release with an arthroscopic blade for hallux valgus correction. Foot Ankle Int. 2004, 25, 13–18. [Google Scholar] [CrossRef]
- Kennedy, J.; Berg, A.; Welsh, L.; Mehta, J. Single incision lateral release for hallux valgus using a cervical biopsy blade: A cadaveric study. Foot 2018, 36, 35–38. [Google Scholar] [CrossRef] [Green Version]
- Choi, Y.R.; Lee, H.S.; Jeong, J.J.; Kim, S.W.; Jeon, I.H.; Lee, D.H.; Lee, W.C. Hallux valgus correction using transarticular lateral release with distal chevron osteotomy. Foot Ankle Int. 2012, 33, 838–843. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.Y.; Lee, H.S.; Chun, H.; Kim, J.S.; Seo, D.K.; Choi, Y.R.; Kim, S.W. Comparison of open lateral release and transarticular lateral release in distal chevron metatarsal osteotomy for hallux valgus correction. Int. Orthop. 2013, 37, 1781–1787. [Google Scholar] [CrossRef] [Green Version]
- Silver, D. The operative treatment of hallux valgus. J. Bone Jt. Surg. Am. 1923, 5, 225–232. [Google Scholar]
- Schneider, W. Influence of different anatomical structures on distal soft tissue procedure in hallux valgus surgery. Foot Ankle Int. 2012, 33, 991–996. [Google Scholar] [CrossRef]
- Augoyard, R.; Largey, A.; Munoz, M.A.; Canovas, F. Efficacy of first metatarsophalangeal joint lateral release in hallux valgus surgery. Orthop. Traumatol. Surg. Res. 2013, 99, 425–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niki, H.; Hirano, T.; Okada, H.; Beppu, M. Combination joint-preserving surgery for forefoot deformity in patients with rheumatoid arthritis. J. Bone Jt. Surg. Br. 2010, 92, 380–386. [Google Scholar] [CrossRef] [Green Version]
- Takakubo, Y.; Takagi, M.; Tamaki, Y.; Sasaki, A.; Nakano, H.; Orui, H.; Ogino, T. Mid-term results of joint-preserving procedures by a modified Mann method for big toe deformities in rheumatoid patients undergoing forefoot surgeries. Mod. Rheumatol. 2010, 20, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Shi, K.; Hayashida, K.; Tomita, T.; Tanabe, M.; Ochi, T. Surgical treatment of hallux valgus deformity in rheumatoid arthritis: Clinical and radiographic evaluation of modified Lapidus technique. J. Foot Ankle Surg. 2000, 39, 376–382. [Google Scholar] [CrossRef]
- Hirao, M.; Ebina, K.; Tsuboi, H.; Noguchi, T.; Hashimoto, J.; Yoshikawa, H. Appearance of hindfoot valgus deformity and recurrence of hallux valgus in the very early period after hallux valgus surgery in a poorly controlled rheumatoid arthritis case: A case report. Mod. Rheumatol. 2019, 29, 367–369. [Google Scholar] [CrossRef]
- Perez Boal, E.; Becerro de Bengoa Vallejo, R.; Fuentes Rodriguez, M.; Lopez Lopez, D.; Losa Iglesias, M.E. Geometry of the Proximal Phalanx of Hallux and First Metatarsal Bone to Predict Hallux Abducto Valgus: A Radiological Study. PLoS ONE 2016, 11, e0166197. [Google Scholar] [CrossRef] [PubMed]
- Grande-Del-Arco, J.; Becerro-de-Bengoa-Vallejo, R.; Palomo-López, P.; López-López, D.; Calvo-Lobo, C.; Pérez-Boal, E.; Losa-Iglesias, M.E.; Martin-Villa, C.; Rodriguez-Sanz, D. Radiographic Analysis on the Distortion of the Anatomy of First Metatarsal Head in Dorsoplantar Projection. Diagnostics 2020, 10, 552. [Google Scholar] [CrossRef] [PubMed]
- Devos Bevernage, B.; Leemrijse, T. Hallux varus: Classification and treatment. Foot Ankle Clin. 2009, 14, 51–65. [Google Scholar] [CrossRef] [PubMed]
| Procedures | Second Toe | Third Toe | Fourth Toe | Fifth Toe |
|---|---|---|---|---|
| Oblique osteotomy for shortening of the metatarsal | 32 | 27 | 23 | 11 |
| PIP joint arthrodesis * | 12 | 6 | 6 | 0 |
| Shortening osteotomy of the proximal phalanx | 3 | 1 | 0 | 0 |
| Abduction osteotomy of the metatarsal | 1 | 1 | 0 | 0 |
| Weil osteotomy | 0 | 4 | 0 | 0 |
| Medial translation of the metatarsal head | 0 | 0 | 0 | 13 |
| Items | Total (n = 36) | Recurrent Deformity (n = 5) | No Recurrent Deformity (n = 31) | p Value | |
|---|---|---|---|---|---|
| Age, years | 64.8 ± 9.2 | 64.2 ± 8.2 | 64.9 ± 0.5 | 0.8712 | |
| Duration of disease, years | 18.5 ± 12.0 | 10.8 ± 5.2 | 19.7 ± 12.4 | 0.1266 | |
| Follow-up period, months | 30.9 ± 16.2 | 36.2 ± 22.0 | 30.1 ± 15.4 | 0.4420 | |
| Methotrexate, mg/week | 5.1 ± 4.5 | 9.0 ± 6.0 | 4.5 ± 4.0 | 0.0344 * | |
| Prednisolone, mg/day | 1.4 ± 2.0 | 2.6 ± 2.5 | 1.2 ± 1.9 | 0.1595 | |
| Use of bDMARDs, n (%) | 12 (33) | 2 (40) | 10 (32) | 0.8053 | |
| DAS28-ESR | 2.8 ± 0.9 | 3.2 ± 1.2 | 2.7 ± 0.9 | 0.2930 | |
| Body mass index, kg/m2 | 20.8 ± 2.7 | 22.0 ± 2.5 | 20.7 ± 2.7 | 0.2956 | |
| Radiographic parameters | |||||
| Preoperative | HVA, ° | 45.5 ± 9.6 | 54.2 ± 7.2 | 44.0 ± 9.2 | 0.0257 * |
| IMA, ° | 17.5 ±3.7 | 18.8 ± 3.3 | 17.3 ± 3.8 | 0.4000 | |
| Sesamoid position | 0:1:35:0 | 0:0:0:5 | 0:0:1:30 | >0.999 | |
| 1 month postoperative | HVA, ° | 7.9 ±6.8 | 19.6 ± 6.0 | 6.0 ± 4.7 | <0.0001 * |
| IMA, ° | 6.5 ± 4.3 | 10.1 ± 4.4 | 5.9 ± 4.0 | 0.0383 * | |
| Sesamoid position | 16:13:7:0 | 0:4:1:0 | 16:9:6:0 | 0.0585 | |
| 3 months postoperative | HVA, ° | 10.2 ± 6.8 | 21.0 ± 6.0 | 8.4 ± 5.1 | <0.0001 * |
| IMA, ° | 7.9 ± 3.9 | 10.1 ± 6.4 | 7.6 ± 3.4 | 0.0886 | |
| Sesamoid position | 11:17:5:3 | 0:3:1:1 | 10:14:4:2 | 0.4160 | |
| 6 months postoperative | HVA, ° | 9.7 ± 7.7 | 20.1 ± 6.3 | 8.0 ± 6.6 | 0.0005 * |
| IMA, ° | 7.1 ± 4.2 | 9.8 ± 5.2 | 6.7 ± 3.9 | 0.1331 | |
| Sesamoid position | 11:13:10:2 | 0:1:4:0 | 11:12:6:2 | 0.0418 * | |
| Latest follow-up | HVA, ° | 10.3 ± 11.2 | 29.2 ±7.6 | 7.2 ± 8.4 | <0.0001 * |
| IMA, ° | 7.0 ± 4.1 | 10.0 ±5.2 | 6.5 ± 3.8 | 0.0801 | |
| Sesamoid position | 11:8:10:7 | 0:1:2:2 | 11:7:8:5 | 0.2036 | |
| Scores | Preoperative | Latest Follow-Up | p Value |
|---|---|---|---|
| JSSF hallux scale score | |||
| Pain (40 points) | 22.3 ± 9.1 | 37.9 ± 4.2 | <0.0001 * |
| Function (45 points) | 22.7 ± 7.9 | 38.9 ± 6.7 | <0.0001 * |
| Alignment (15 points) | 0.7 ± 2.8 | 14.0 ± 2.6 | <0.0001 * |
| Total (100 points) | 45.1 ± 14.6 | 90.7 ± 10.8 | <0.0001 * |
| SAFE-Q score | |||
| Pain and pain-related | 67.1 ± 18.8 | 84.6 ± 15.7 | <0.0001 * |
| Physical functioning and daily living | 67.6 ± 22.3 | 79.1 ± 19.3 | 0.0053 * |
| Social functioning | 66.8 ± 26.9 | 84.0 ± 22.7 | 0.0019 * |
| Shoe-related | 39.7 ± 19.5 | 61.6 ± 18.0 | <0.0001 * |
| General health and well-being | 62.0 ± 27.8 | 85.5 ± 17.8 | <0.0001 * |
| Study | Procedures for Correcting HV | Addition of Akin Osteotomy | No. of Feet | Mean FU Period, Months | Approach for Lateral Release | Extent of Lateral Release | Preoperative HVA, ° | HVA at the Latest FU, ° | Cases with Recurrent HV, % | Cases with Iatrogenic Hallux Varus, % | Clinical Outcomes |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Berg et al. [9] | scarf osteotomy | if necessary, 30% | 20 | 65 | dorsal | NR | 41 | 28 | 40% (no definition of recurrent HV) | 0% | Patient satisfaction rate: 79% |
| Barouk et al. [10] | scarf osteotomy | routine, 100% | 55 | 75 | NR | NR | NR | NR | 5% (no definition of recurrent HV) | some | none |
| Bhavikatti et al. [11] | scarf osteotomy | 0% | 66 | 51 | dorsal | NR | 32 | 14 | 5% (HVA >18° and IMA >11°) | NR | AOFAS score: 39.8 ⇒ 88.7, Subjective report: excellent 74%, good 13.5%, fair 10.5%; poor 1% |
| Kushioka et al. [13] | scarf osteotomy with medial capsule interposition | if necessary, 4% | 76 | 35 | dorsal | routine fashion: adductor tendon insertion into the PP, DTML, and capsule between the first metatarsal and the lateral sesamoid | 50.8 | 12.8 | 16% (HVA >20°) | 9% | JSSF RA foot and ankle scale score: 52.2 ⇒ 76.9, JSSF hallux scale score: 38.2 ⇒ 74.5, SAFE-Q score: no preoperative data ⇒ 78.8/71.3/70.2/83.1/60.4 |
| Our study | scarf osteotomy | if necessary, 100% | 36 | 32 | intra- articular | stepwise fashion: suspensory ligament, lateral capsule, and adductor tendon insertion into the PP | 45.5 | 10.3 | 14% (HVA >20°) | 11% | JSSF hallux scale score: 45.1 ⇒ 90.7, SAFE-Q score: 67.1/67.6/66.8/39.7/62.0 ⇒ 84.6/79.1/84.0/61.6/85.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsumoto, T.; Maenohara, Y.; Chang, S.H.; Ono, K.; Omata, Y.; Hirose, J.; Tanaka, S. Outcomes of Scarf and Akin Osteotomy with Intra-Articular Stepwise Lateral Soft Tissue Release for Correcting Hallux Valgus Deformity in Rheumatoid Arthritis. Int. J. Environ. Res. Public Health 2021, 18, 10667. https://doi.org/10.3390/ijerph182010667
Matsumoto T, Maenohara Y, Chang SH, Ono K, Omata Y, Hirose J, Tanaka S. Outcomes of Scarf and Akin Osteotomy with Intra-Articular Stepwise Lateral Soft Tissue Release for Correcting Hallux Valgus Deformity in Rheumatoid Arthritis. International Journal of Environmental Research and Public Health. 2021; 18(20):10667. https://doi.org/10.3390/ijerph182010667
Chicago/Turabian StyleMatsumoto, Takumi, Yuji Maenohara, Song Ho Chang, Kumiko Ono, Yasunori Omata, Jun Hirose, and Sakae Tanaka. 2021. "Outcomes of Scarf and Akin Osteotomy with Intra-Articular Stepwise Lateral Soft Tissue Release for Correcting Hallux Valgus Deformity in Rheumatoid Arthritis" International Journal of Environmental Research and Public Health 18, no. 20: 10667. https://doi.org/10.3390/ijerph182010667
APA StyleMatsumoto, T., Maenohara, Y., Chang, S. H., Ono, K., Omata, Y., Hirose, J., & Tanaka, S. (2021). Outcomes of Scarf and Akin Osteotomy with Intra-Articular Stepwise Lateral Soft Tissue Release for Correcting Hallux Valgus Deformity in Rheumatoid Arthritis. International Journal of Environmental Research and Public Health, 18(20), 10667. https://doi.org/10.3390/ijerph182010667






