Development of a Community-Based Integrated Service Model of Health and Social Care for Older Adults Living Alone
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
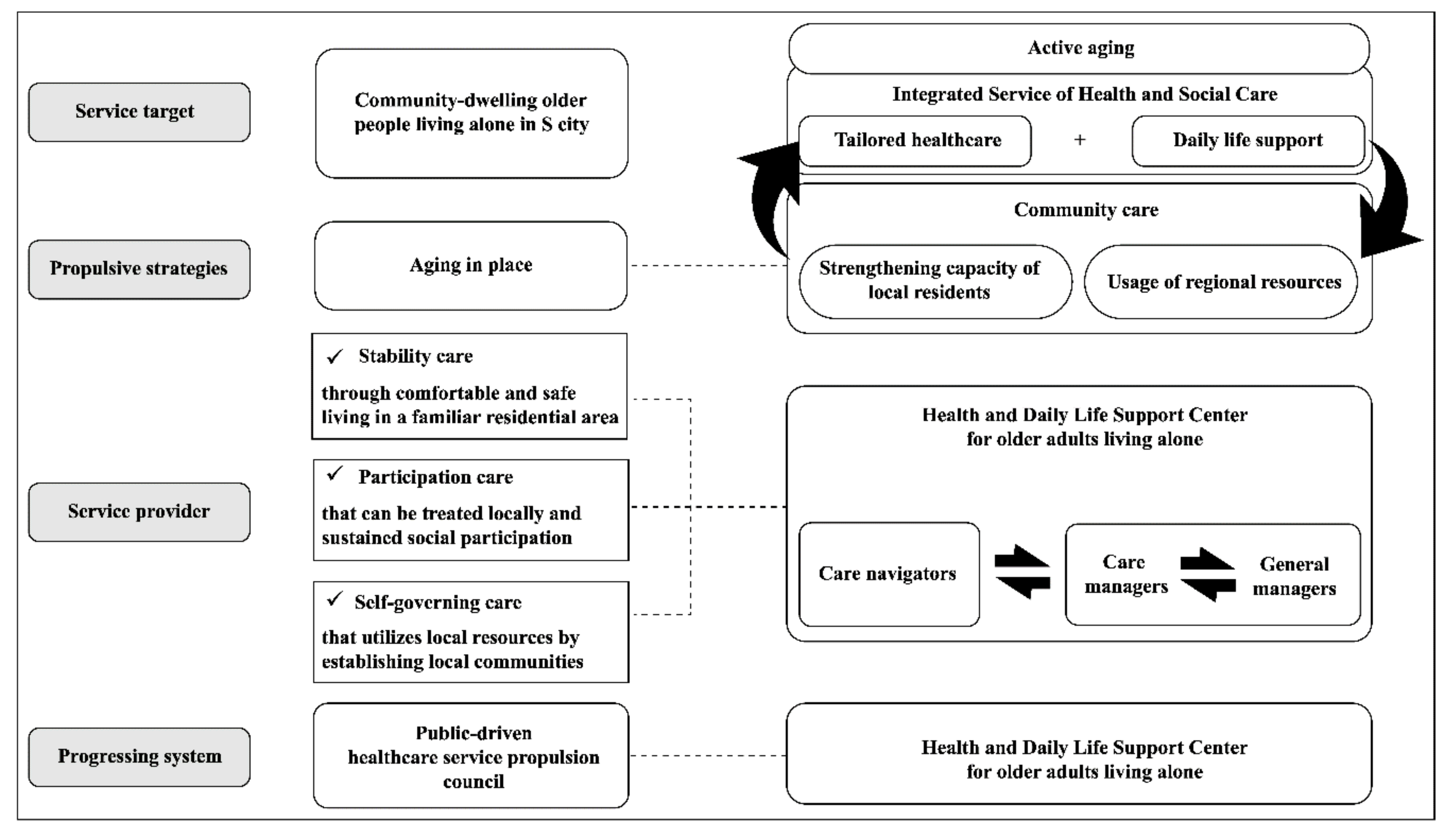
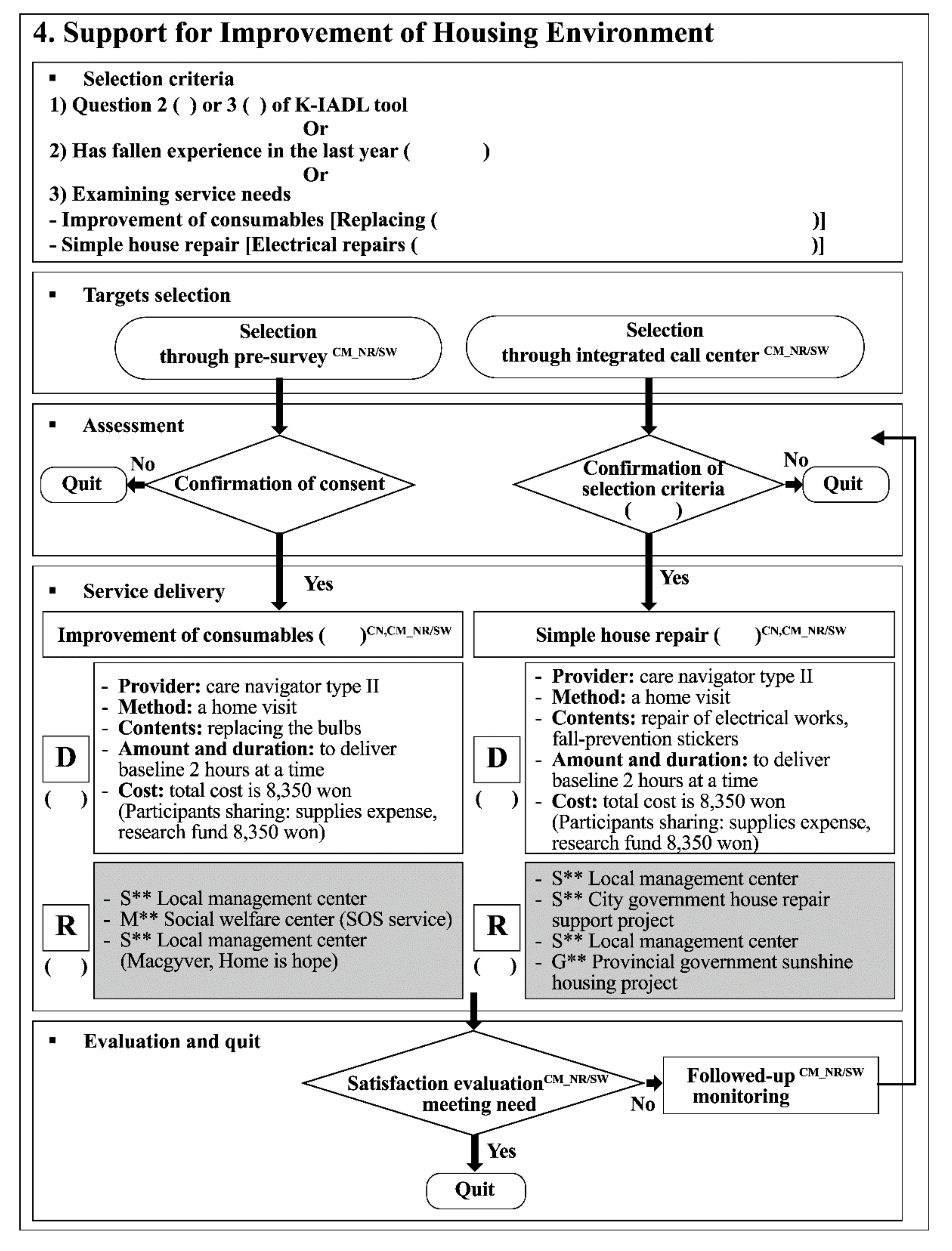
2.2. Development of the CBIS Model
2.3. Pilot Testing of CBIS
2.3.1. Participants
2.3.2. Procedure
2.3.3. Ethics Statement
3. Results
3.1. Participant’s Characteristics
3.2. Service Feasibility
3.3. Service Sustainability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Banerjee, S. Multimorbidity—Older adults need health care that can count past one. Lancet 2015, 385, 587–589. [Google Scholar] [CrossRef]
- Czaja, S.J. Long-term care services and support systems for older adults: The role of technology. Am. Psychol. 2016, 71, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Cutchin, M.P.; Coppola, S.; Talley, V.; Svihula, J.; Catellier, D.J.; Shank, K.H. Feasibility and effects of preventive home visits for at-risk older people: Design of a randomized controlled trial. BMC Geriatr. 2009, 9, 54. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.M.; Jeong, L.S. A study on the influential factors of the effectiveness of welfare service delivery system for elders. Korean Political Sci. Rev. 2011, 15, 53–81. [Google Scholar]
- McDonough, K.E.; Davitt, J.K. It Takes a Village: Community Practice, Social Work, and Aging-in-Place. J. Gerontol. Soc. Work 2011, 54, 528–541. [Google Scholar] [CrossRef]
- Lynch, M.; Hernandez, M.; Estes, C. PACE: Has It Changed the Chronic Care Paradigm? Soc. Work Public Health 2008, 23, 3–24. [Google Scholar] [CrossRef]
- Fänge, A.; Ivanoff, S.D. The home is the hub of health in very old age: Findings from the ENABLE-AGE Project. Arch. Gerontol. Geriatr. 2009, 48, 340–345. [Google Scholar] [CrossRef]
- Kim, H.; Jeong, J.A. A study on linkage between local welfare hub service and elderly care service. Korean Gerontol. Soc. Conf. Paper 2017, 234–238. [Google Scholar]
- Haksil, K. A study of service co-production based on community: Focused on Chnungbuk’s ‘9988 Happiness Protector Business’. Korean Pol. Stud. Rev. 2017, 26, 79–106. [Google Scholar]
- Jeongmi, L. The current state of community care in Japan: With special reference to community care centers. Glob. Soc. Secur. Rev. 2018, 5, 67–77. [Google Scholar]
- Lee, H.K.; Lee, J.S. A study on the factors affecting in successful aging through the participatory characteristics on the National Senior Public Work (NSPW) program—Focusing on mediating effects of participation satisfaction in the elderly work program. Soc. Work Pract. Res. 2018, 15, 5–33. [Google Scholar]
- Ministry of Health and Welfare. Health and Welfare Program for the Elderly South Korea: Jinhan M&B. Available online: http://www.mohw.go.kr/eng/upload/content_data/2018/2018%20Welfare%20Services%20Guidelines.pdf (accessed on 13 September 2020).
- Xiu-Ying, H.; Qian, C.; Xiao-Dong, P.; Xue-Mei, Z.; Chang-Quan, H. Living arrangements and risk for late life depression: A meta-analysis of published literature. Int. J. Psychiatry Med. 2012, 43, 19–34. [Google Scholar] [CrossRef] [PubMed]
- Zali, M.; Farhadi, A.; Soleimanifar, M.; Allameh, H.; Janani, L. Loneliness, fear of falling, and quality of life in community-dwelling older women who live alone and live with others. Educ. Gerontol. 2017, 43, 582–588. [Google Scholar] [CrossRef]
- Pantell, M.; Rehkopf, D.; Jutte, D.; Syme, S.L.; Balmes, J.; Adler, N. Social isolation: A predictor of mortality comparable to traditional clinical risk factors. Am. J. Public Health 2013, 103, 2056–2062. [Google Scholar] [CrossRef]
- Jae-Chul, N.; Zoon-Ki, K. Current status and problems of support polices and legal improvement devices for the aged living alone. J. Korea Contents Assoc. 2013, 13, 257–268. [Google Scholar]
- Pastalan, L.A. Aging in Place: The role of Housing and Social Supports; The Haworth Press: New York, NY, USA, 2013. [Google Scholar]
- Bienkowska-Gibbs, T. Integrated care programmes in Canada. Eurohealth 2013, 19, 13–14. [Google Scholar]
- Hébert, R.; Durand, P.J.; Dubuc, N.; Tourigny, A.; The PRISMA Group. PRISMA: A new model of integrated service delivery for the frail older people in Canada. Int. J. Integr. Care 2003, 3, e08. [Google Scholar]
- Sunwoo, D. Policy issues in elderly health and long-term care policy. In paper presented at the Health and Welfare Policy Forum; Korean Institute for Health and Social Affairs. 2016. Available online: https://www.kihasa.re.kr/english/publications/eng_research/view.do?pageIndex=2&keyField=&key=&menuId=73&tid=34&bid=39&division=&ano=946 (accessed on 13 September 2020).
- Lee, Y.J. Determinants of welfare service utilization among the single and the married couple’s elderly. Korean Gerontol. Soc. 2012, 32, 1119–1135. [Google Scholar]
- Yeom, J. Implementation process and prospects of the elderly-the elderly care program. J. Korean Gerontol. Soc. 2013, 33, 221–238. [Google Scholar]
- Soonduck, Y.; Hyesun, C. Case study on the problems of elderly care by community elderly in rural Korea. Korean J. Gerontol. Soc. Welf. 2008, 40, 31–54. [Google Scholar] [CrossRef]
- Ko, H.; Park, Y.-H.; Cho, B.; Lim, K.-C.; Chang, S.J.; Yi, Y.M.; Noh, E.Y.; Ryu, S.I. Gender differences in health status, quality of life, and community service needs of older adults living alone. Arch. Gerontol. Geriatr. 2019, 83, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Lim, K.C.; Cho, B.L.; Ko, H.N.; Yi, Y.M.; Noh, E.Y.; Ryu, S.I.; Chang, S.J. Experiences of healthcare and daily life support services in community-dwelling elders living alone: A thematic analysis using focus-group interviewing. J. Korean Gerontol. Nurs. 2019, 21, 200–210. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Survey of Elderly State. 2020. Available online: http://kosis.kr/eng/statisticsList/statisticsListIndex.do?menuId=M_01_01 (accessed on 13 September 2020).
- Beckman, A.G.K.; Parker, M.G.; Thorslund, M. Can elderly people take their medicine? Patient Educ. Couns. 2005, 59, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.M.; Nam, E.S.; Bae, S.S.; Shin, D.S.; Choi, Y.J. Effects of peer support home visiting for older adults living alone in a rural area. Ment. Health Soc. Work 2016, 44, 35–63. [Google Scholar]
- Stark, C.R.; Riordan, V.; O’Connor, R. A conceptual model of suicide in rural areas. Rural Remote Health 2011, 11, 1622. [Google Scholar]
- Kim, S.H. Effects of a volunteer-run peer support program on health and satisfaction with social support of older adults living alone. J. Korean Acad. Nurs. 2012, 42, 525–536. [Google Scholar] [CrossRef]
- Cantegreil-Kallen, I.; Pin, S. Fear of Alzheimer’s disease in the French population: Impact of age and proximity to the disease. Int. Psychogeriatr. 2012, 24, 108–116. [Google Scholar] [CrossRef]
- Lee, Y.J.; Kwon, M.K.; Baek, H.J.; Lee, S.S. Comparative analysis of food intake according to the family type of elderly women in Seoul area. J. Nutr. Health Aging 2015, 48, 277–288. [Google Scholar] [CrossRef]
- Kyoung-Poon, H.; Min-Kyoung, J.; Sun-Hee, S. Relationship of participation satisfaction, living satisfaction and life satisfaction among elderly participants in the job creation project for the elderly. J. Korea Contents Assoc. 2014, 14, 160–170. [Google Scholar]
| Service Manual ITEMS | Mean ± SD | Individual CVIs | |
|---|---|---|---|
| Service overview | Service purpose | 4.6 ± 0.5 | 0.85 |
| Service rationale | 4.8 ± 0.4 | 0.75 | |
| HDLS Center | HDLS Center management | 4.8 ± 0.4 | 0.9 |
| HDLS Center guideline | 4.8 ± 0.4 | 0.9 | |
| HDLS Center administration | 4.4 ± 0.5 | 0.85 | |
| service target | selection criteria | 4.2 ± 0.8 | 0.85 |
| selection procedures | 4.6 ± 0.5 | 0.9 | |
| target management | 4.6 ± 0.5 | 0.9 | |
| Quit management | 4.6 ± 0.5 | 0.85 | |
| service content | Algorithms | 4.6 ± 0.5 | 0.9 |
| detailed contents | 4.4 ± 0.5 | 0.9 | |
| service delivery personnel | General manager task | 4.6 ± 0.5 | 0.95 |
| Care manager task | 4.6 ± 0.5 | 0.8 | |
| care navigator task | 4.8 ± 0.4 | 0.85 | |
| Others (co-operative physician, care-navigator managers) | 4.6 ± 0.5 | 0.85 | |
| Total means 4.62 | Scale CVI 0.87 | ||
| Service Type | Service Satisfaction Level | Service Delivery Times | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adequacy of Content | Time | Immediacy | Convenience | Kindness | Overall Satisfactionwith Center | Minutes | ||||||||||||||||
| Sex | Sex | Sex | Sex | Sex | Sex | |||||||||||||||||
| W | M | T | W | M | T | W | M | T | W | M | T | W | M | T | W | M | T | Mean | Min. | Max. | ||
| S2 | 9.3 | 8.3 | 9.1 | 8.8 | 8 | 8.6 | 9 | 7.5 | 8.6 | 8.6 | 8 | 8.4 | 9.6 | 9.5 | 9.6 | 9.1 | 8.5 | 8.9 | 8.8 | 7 | 10 | |
| S3 | 9.3 | 10 | 9.4 | 9.3 | 10 | 9.4 | 9 | 10 | 9.1 | 8.9 | 10 | 9 | 9.6 | 10 | 9.6 | 8.4 | 10 | 8.6 | 125 | 90 | 180 | |
| S5 | 10 | - | 10 | 10 | - | 10 | 10 | - | 10 | 10 | - | 10 | 10 | - | 10 | 10 | - | 10 | 15 | 15 | 15 | |
| S6 | 8.8 | - | 8.8 | 9.8 | - | 9.8 | - | 9.8 | 9.8 | - | 9.8 | 9.8 | - | 9.8 | 8.8 | - | 8.8 | 30 | 30 | 60 | ||
| S7 | 7.5 | - | 7.5 | 8 | - | 8 | 9 | - | 9 | 7.5 | - | 7.5 | 10 | - | 10 | 9 | - | 9 | 70 | 60 | 90 | |
| S10 | 7.7 | 8.3 | 7.8 | 7.5 | 7.7 | 7.5 | 6.5 | 7.5 | 7.2 | 7.5 | 7.5 | 7.5 | 8.3 | 7.7 | 8.2 | 8.7 | 8 | 8.6 | 3.9 | 1.2 | 18.4 | |
| S11 | V | 9.5 | 8.3 | 9.2 | 9.5 | 8.3 | 9.2 | 8.9 | 8.7 | 8.8 | 9.4 | 8.3 | 9.1 | 9.5 | 8 | 9.1 | 9.3 | 8.7 | 9.1 | 50 | 30 | 60 |
| P | 5.3 | 1.1 | 10 | |||||||||||||||||||
| S12 | 8.4 | - | 8.4 | 8 | - | 8 | 8.6 | - | 8.6 | 8.5 | - | 8.5 | 9.2 | - | 9.2 | 9 | - | 9 | 38.7 | 26 | 58 | |
| S13 | 9.4 | 5 | 9.1 | 9.8 | 7 | 9.6 | 9.8 | 5 | 9.5 | 9.8 | 5 | 9.5 | 9.8 | 7 | 9.6 | 10 | 6 | 9.7 | 60 | 60 | 60 | |
| Total | 8.9 | 8.0 | 8.8 | 9 | 8.2 | 8.9 | 9 | 7.7 | 9.0 | 8.9 | 7.8 | 8.8 | 9.5 | 8.4 | 9.5 | 9.1 | 8.2 | 9 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yi, Y.M.; Park, Y.-H.; Cho, B.; Lim, K.-C.; Jang, S.-N.; Chang, S.J.; Ko, H.; Noh, E.-Y.; Ryu, S.I. Development of a Community-Based Integrated Service Model of Health and Social Care for Older Adults Living Alone. Int. J. Environ. Res. Public Health 2021, 18, 825. https://doi.org/10.3390/ijerph18020825
Yi YM, Park Y-H, Cho B, Lim K-C, Jang S-N, Chang SJ, Ko H, Noh E-Y, Ryu SI. Development of a Community-Based Integrated Service Model of Health and Social Care for Older Adults Living Alone. International Journal of Environmental Research and Public Health. 2021; 18(2):825. https://doi.org/10.3390/ijerph18020825
Chicago/Turabian StyleYi, Yu Mi, Yeon-Hwan Park, BeLong Cho, Kyung-Choon Lim, Soong-Nang Jang, Sun Ju Chang, Hana Ko, Eun-Young Noh, and So Im Ryu. 2021. "Development of a Community-Based Integrated Service Model of Health and Social Care for Older Adults Living Alone" International Journal of Environmental Research and Public Health 18, no. 2: 825. https://doi.org/10.3390/ijerph18020825
APA StyleYi, Y. M., Park, Y.-H., Cho, B., Lim, K.-C., Jang, S.-N., Chang, S. J., Ko, H., Noh, E.-Y., & Ryu, S. I. (2021). Development of a Community-Based Integrated Service Model of Health and Social Care for Older Adults Living Alone. International Journal of Environmental Research and Public Health, 18(2), 825. https://doi.org/10.3390/ijerph18020825





