Equity of Health Services Utilisation and Expenditure among Urban and Rural Residents under Universal Health Coverage
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sites and Participants
2.2. Data Collection
2.3. Indicator Calculation
2.4. Statistical Methods
3. Results
3.1. Urban and Rural Residents’ Demand for and Utilisation of Health Services
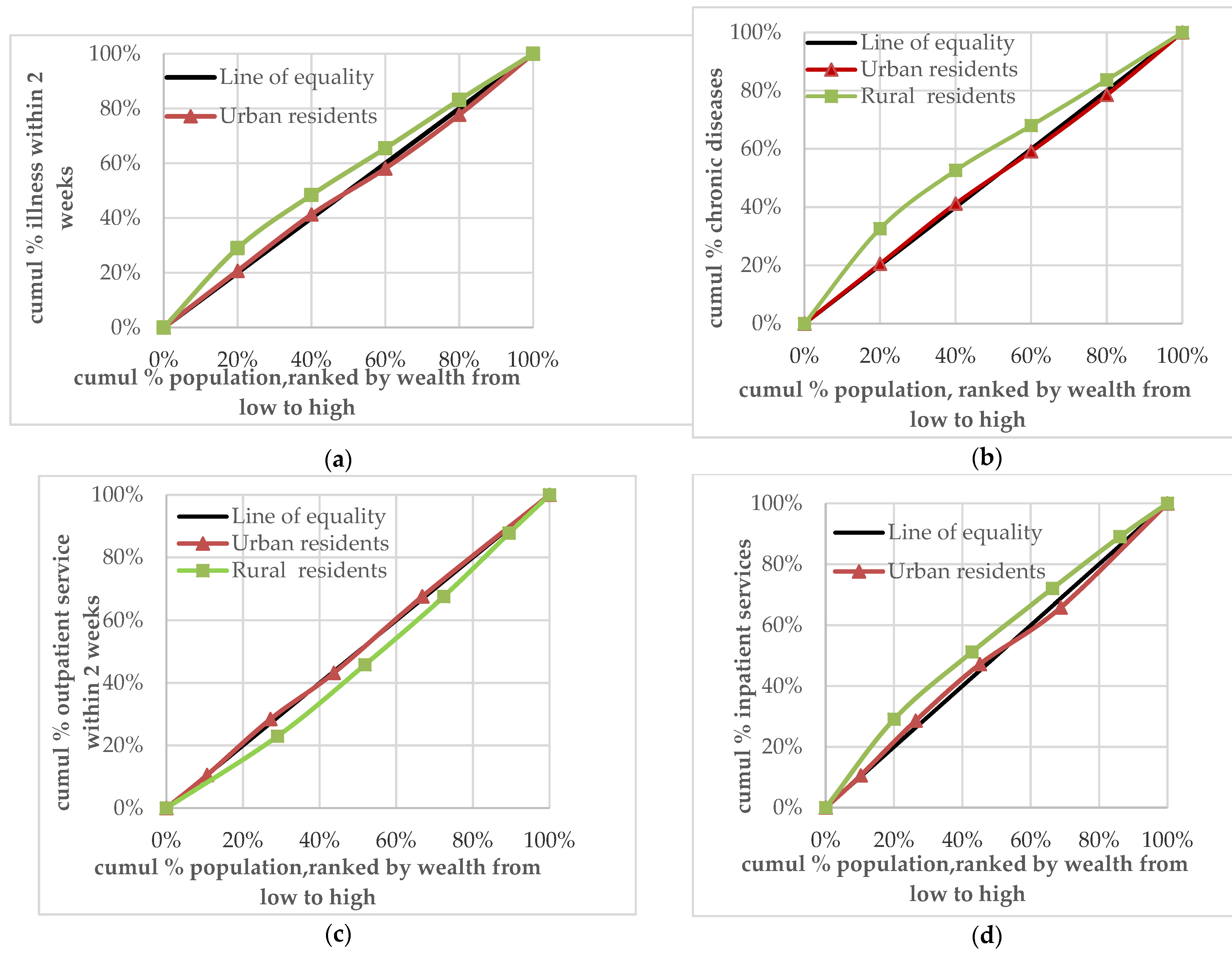
3.2. Analysis of the Equity Difference of Demand for, and Utilisation of, Health Services between Urban and Rural Residents
3.3. Health Expenditure of Urban and Rural Residents
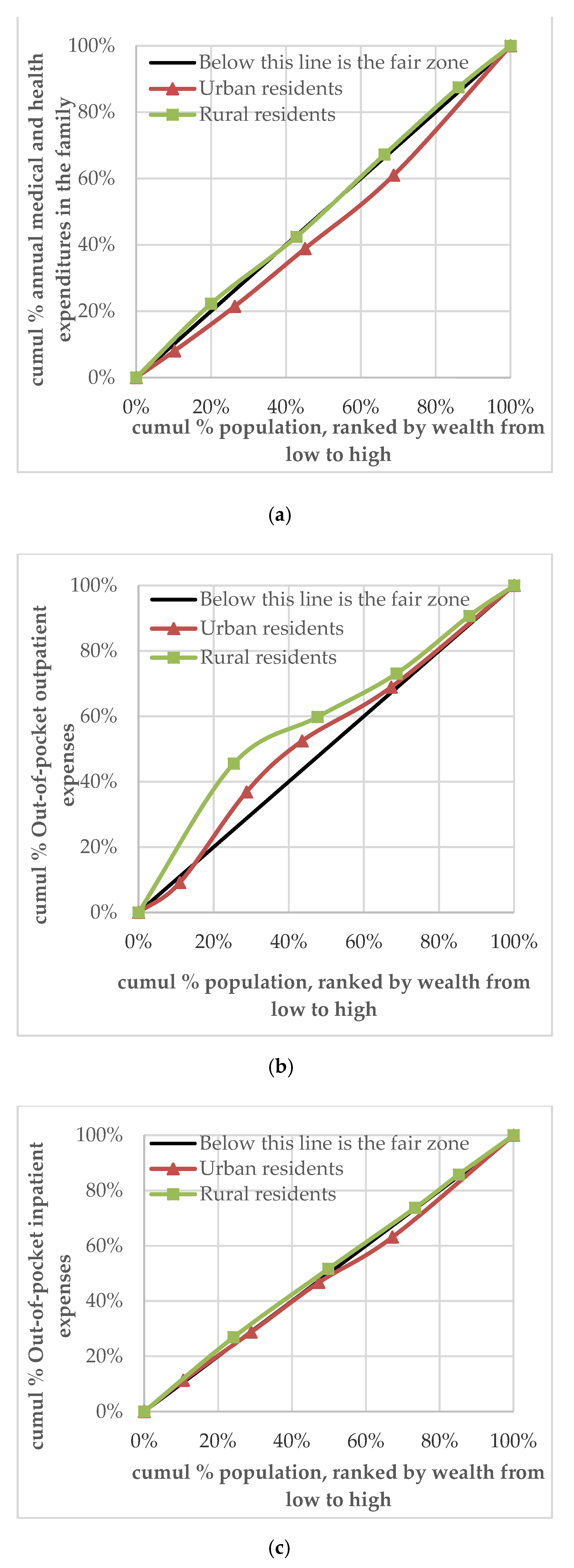
3.4. Analysis of the Equity Difference between Urban and Rural Health Expenditure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Bank Group. Monitoring Frameworks, Indicators and Targets for Universal Health Coverage Progress at the National and Global Levels; World Health Organization: Geneva, Switzerland, 2014; pp. 1–10. [Google Scholar]
- The World Health. Universal Health Coverage Study; Chapter 1; World Health Organization: Geneva, Switzerland, 2013; pp. 1–15. [Google Scholar]
- McKee, M.; Balabanova, D.; Basu, S.; Ricciardi, W.; Stuckler, D. Universal health coverage: A quest for all countries but under threat in some. Value Health 2013, 16, S39–S45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurakbayev, K.K.; Issayev, D.S.; Koshimbekov, M.K.; Kumar, A.B. Assessment of technical equipment supply in healthcare institutions: Example of Almaty. J. Res. Med. Sci. 2014, 9, 819–822. [Google Scholar]
- World Health Organization. Resolution WHA 58.33: Sustainable health financing, universal coverage and social health insurance. World Health Assem. Resolut. 2005, 14, 139–140. [Google Scholar]
- The World Health Report. Health Systems Financing: The Path to Universal Coverage; Chapter 1; World Health Organization: Geneva, Switzerland, 2010; pp. 13. [Google Scholar]
- Low, S.; Tun, K.T.; Mhote, N.P. Human resources for health: Task shifting to promote basic health service delivery among internally displaced people in ethnic health program service areas in eastern Burma/Myanmar. Glob. Health Action. 2014, 7, 24937. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The, L. Ensuring and measuring universality in UHC. Lancet 2019, 10166, 1. [Google Scholar]
- Reid, M.; Roberts, G.; Goosby, E.; Wesson, P. Monitoring Universal Health Coverage (UHC) in high Tuberculosis burden countries: Tuberculosis mortality an important tracer of UHC service coverage. PLoS ONE 2019, 110, e0223559. [Google Scholar]
- Macintyre, S. The Black Report and beyond: What are the issues? Soc. Sci. Med. 1997, 6, 723–745. [Google Scholar] [CrossRef]
- Annear, P.L.; Bigdeli, M.; Jacobs, B. A functional model for monitoring equity and effectiveness in purchasing health insurance premiums for the poor: Evidence from Cambodia and the Lao PDR. Health Policy 2011, 102, 295–303. [Google Scholar] [CrossRef]
- Wagstaff, A. Poverty and health sector inequalities. Bull. World Health Organ. 2002, 2, 97–105. [Google Scholar]
- A New global partnership: Eradicate poverty and transform economies through sustainable development. Report of the High-level Panel of Eminent Persons on the Post-2015 Development Agenda; United Nations: New York, NY, USA, 2013. [Google Scholar]
- Zhao, P.; Diao, Y.; You, L.; Wu, S.; Yang, L.; Liu, Y. The influence of basic public health service project on maternal health services: An interrupted time series study. BMC Public Health 2019, 1, 824. [Google Scholar]
- Li, C.; Tang, C.; Wang, H. Effects of health insurance integration on health care utilization and its equity among the mid-aged and elderly: Evidence from China. Int. J. Equity Health 2019, 1, 166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, X.; Zhang, Y.; Shao, H. Healthy China 2030: A breakthrough for improving health. Glob. Health Promot. 2019, 4, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Sun, N.; Xu, F. Influencing factors of inequity in health services utilization among the elderly in China. Int. J. Equity Health 2018, 1, 144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Layton, N.; Bell, D.; Borg, J. Assistive technology as a pillar of universal health coverage: Qualitative analysis of stakeholder responses to the world health assembly resolution on assistive technology. Disabil. Rehabil. Assist. Technol. 2020, 7, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Yao, X.; Jian, W. Improving health equity: Changes in self-assessed health across income groups in China. Int. J. Equity Health 2018, 1, 94. [Google Scholar] [CrossRef] [Green Version]
- Liu, G.G.; Vortherms, S.A.; Hong, X. China’s Health Reform Update. Annu. Rev. Public Health. 2017, 38, 431–448. [Google Scholar] [CrossRef] [Green Version]
- Song, P.; Jin, C.; Tang, W. New medical education reform in China: Towards healthy China 2030. Biosci. Trends 2017, 4, 366–369. [Google Scholar]
- Yip, W.; Fu, H.; Chen, A.T. 10 years of health-care reform in China: Progress and gaps in Universal Health Coverage. Lancet 2019, 10204, 1192–1204. [Google Scholar]
- Jing, L.; Chen, R.; Jing, L.; Qiao, Y.; Lou, J.; Xu, J.; Wang, J.; Chen, W.; Sun, X. Development and enrolee satisfaction with basic medical insurance in China: A systematic review and stratified cluster sampling survey. Int. J. Health Plan. Manag. 2017, 3, 285–298. [Google Scholar]
- Chen, R.; Li, N.X.; Liu, X. Study on the equity of medical services utilization for elderly enrolled in different basic social medical insurance systems in an underdeveloped city of Southwest China. Int. J. Equity Health 2018, 1, 54. [Google Scholar]
- Bragg, F.; Holmes, M.V.; Iona, A. Association between Diabetes and Cause-Specific Mortality in Rural and Urban Areas of China. JAMA 2017, 3, 280–289. [Google Scholar] [CrossRef] [PubMed]
- Weinhold, I.; Gurtner, S. Rural-urban differences in determinants of patient satisfaction with primary care. Soc. Sci. Med. 2018, 212, 76–85. [Google Scholar] [PubMed]
- Zhu, K.; Zhang, L.; Yuan, S.; Zhang, X.; Zhang, Z. Health financing and integration of urban and rural residents’ basic medical insurance systems in China. Int. J. Equity Health 2017, 1, 194. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.S.; Chen, C. Analysis on the equity of health care utilization among the elderly in Jiangsu Province. Chin. Health Resour. 2017, 6, 520–524. (In Chinese) [Google Scholar]
- He, L.P.; Li, X.M.; Luo, J.H. Study on the evaluation methods of health equity. Soft Sci. Health 2010, 2, 100–103. (In Chinese) [Google Scholar]
- Ma, W.S. Equity evaluation on the basic medical insurance system in Tianjin. Chin. J. Health Policy 2016, 7, 41–45. (In Chinese) [Google Scholar]
- Yao, Z.B.; Zhang, F.; Sun, Y.F. Studying on the equity of residents’ healthcare utilization. Chin. Health Serv. Manag. 2016, 7, 517–519, 546. (In Chinese) [Google Scholar]
- Cui, K.C.; Xu, L.Z. A review of research on equity in health service utilization and its influencing factors. Soft Sci. Health 2011, 5, 388–391. (In Chinese) [Google Scholar]
- Liang, W.P.; Zheng, J.Z.; Han, Y.; He, L. Equity of health care and the evaluation of different ways of assessment. Chin. Rural Health Serv. Adm. 2007, 10, 742–744. (In Chinese) [Google Scholar]
- Shi, Y.Y.; Fu, X.Z.; Guo, H.W.; Yang, J.Y.; Sun, C.Q. Evaluation of equity in utilization of outpatient health services for the elderly in China and its main influencing factors. J. Zhengzhou Univ. (Med Sci.) 2020, 4, 468–471. (In Chinese) [Google Scholar]
- He, L.P.; Li, X.M.; Bai, Y.L.; Wang, J. Analysis on equity of health service utilization of Bai nationality in Yunnan. Soft Sci. Health 2017, 4, 16–20. (In Chinese) [Google Scholar]
- Cao, Y.Y.; Yan, M.Q.; Niu, Y.N.; Wang, L.; Sun, C.Q. Equity of health service utilization among residents in Henan province. Chin. J. Public Health 2017, 6, 894–900. (In Chinese) [Google Scholar]
- Chen, M.; Palmer, A.J.; Si, L. Improving equity in health care financing in China during the progression towards Universal Health Coverage. BMC Health Serv. Res. 2017, 1, 852. [Google Scholar]
- Kim, S.; Kwon, S. Impact of the policy of expanding benefit coverage for cancer patients on catastrophic health expenditure across different income groups in South Korea. Soc. Sci. Med. 2015, 138, 241–247. [Google Scholar] [PubMed]
- Witthayapipopsakul, W.; Cetthakrikul, N.; Suphanchaimat, R.; Noree, T.; Sawaengdee, K. Equity of health workforce distribution in Thailand: An implication of concentration index. Risk Manag. Healthc. Policy 2019, 12, 13–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, X.; Zhang, H.; Hu, X. Measurement and analysis of equity in health: A case study conducted in Zhejiang Province, China. Int. J. Equity Health 2018, 1, 36. [Google Scholar]
- Wang, X.; Yang, H.; Duan, Z.; Pan, J. Spatial accessibility of primary health care in China: A case study in Sichuan Province. Soc. Sci. Med. 2018, 209, 14–24. [Google Scholar]
- Lee, W.Y.; Shaw, I. The impact of out-of-pocket payments on health care inequity: The case of national health insurance in South Korea. Int. J. Environ. Res. Public Health 2014, 7, 7304–7318. [Google Scholar] [CrossRef] [Green Version]
- Ekman, B. Catastrophic health payments and health insurance: Some counterintuitive evidence from one low-income country. Health Policy 2007, 83, 304–313. [Google Scholar]
- Kien, V.D.; Van Minh, H.; Giang, K.B.; Dao, A.; Tuan, L.T.; Ng, N. Socioeconomic inequalities in catastrophic health expenditure and impoverishment associated with non-communicable diseases in urban Hanoi, Vietnam. Int. J. Equity Health 2016, 1, 169. [Google Scholar] [CrossRef] [Green Version]
- Waters, H.R.; Anderson, G.F.; Mays, J. Measuring financial protection in health in the United States. Health Policy 2004, 69, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Kavosi, Z.; Keshtkaran, A.; Hayati, R.; Ravangard, R.; Khammarnia, M. Household financial contribution to the health System in Shiraz, Iran in 2012. Int. J. Health Policy Manag. 2014, 3, 243–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shang, X.; Huang, Y.; Li, B. Residents’ Awareness of Family Doctor Contract Services, Status of Contract with a Family Doctor, and Contract Service Needs in Zhejiang Province, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 18, 3312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.; Chen, S.; Zhu, J.; Li, W. China’s new 4 + 4 medical education programme. Lancet 2019, 10204, 1121–1123. [Google Scholar] [CrossRef]
- Tian, M.; Wang, H.; Tong, X.; Zhu, K.; Zhang, X.; Chen, X. Essential Public Health Services’ Accessibility and its Determinants among Adults with Chronic Diseases in China. PLoS ONE 2015, 4, e0125262. [Google Scholar] [CrossRef] [Green Version]
- Meessen, B. The Role of Digital Strategies in Financing Health Care for Universal Health Coverage in Low- and Middle-Income Countries. Glob. Health Sci. Pract. 2018, 6 (Suppl. S1), S29–S40. [Google Scholar] [CrossRef]
- Myint, C.Y.; Pavlova, M.; Thein, K.N.; Groot, W. A systematic review of the health-financing mechanisms in the Association of Southeast Asian Nations countries and the People’s Republic of China: Lessons for the move towards universal health coverage. PLoS ONE 2019, 6, e0217278. [Google Scholar] [CrossRef]
- Wagstaff, A.; Neelsen, S. A comprehensive assessment of universal health coverage in 111 countries: A retrospective observational study. Lancet Glob. Health 2020, 8, e39–e49. [Google Scholar]
- Uzochukwu, B.S.; Ughasoro, M.D.; Etiaba, E.; Okwuosa, C.; Envuladu, E.; Onwujekwe, O.E. Health care financing in Nigeria: Implications for achieving universal health coverage. Niger. J. Clin. Pract. 2015, 4, 437–444. [Google Scholar] [CrossRef] [Green Version]
- Islam, M.R.; Rahman, M.S.; Islam, Z.; Nurs, C.Z.; Sultana, P.; Rahman, M.M. Inequalities in financial risk protection in Bangladesh: An assessment of universal health coverage. Int. J. Equity Health 2017, 1, 59. [Google Scholar]
| Variable | Survey Questions and Description |
|---|---|
| Variable of basic characteristics of the population | |
| Urban and rural categories | What is the nature of your registered residence? 1 = Agriculture; 2 = Non-agriculture |
| Income | How much was your household’s total income in the previous year? (Disposable income for urban households and net income for rural households) |
| Classification into 5 groups by income | Customised variables: Using the method of five levels of income classification, researchers divided urban and rural households into 5 levels according to their income. (Low-income group, lower middle-income group, middle-income group, upper middle-income group, and high-income group) |
| Measurement variables of residents’ demand for and utilisation of health services | |
| Getting sick in two weeks | Did you have any illness or injury in the two weeks before the investigation? 1 = Yes; 2 = No |
| Annual chronic disease | Have you been diagnosed with chronic diseases (hypertension, diabetes, cancer, and other chronic diseases) in the past year? 1 = Yes; 2 = No |
| Medical treatment in two weeks | Have you seen a doctor for a disease or injury in the last two weeks? 1 = Yes; 2 = No |
| Hospitalised | In the past 12 months, have you been diagnosed by a doctor as requiring hospitalisation but you have not been hospitalised? 1 = Yes; 2 = No |
| Measurement variables of medical and health expenditure | |
| Personal cash health expenditure on outpatient services | How much did you pay for your illness in the last two weeks? (Excluding reimbursement and expenses paid by personal medical accounts) |
| Personal cash health expenditure on hospitalisation | How much did you pay for your hospitalisation expenses in the last year? (Excluding reimbursement and expenses paid by personal medical accounts) |
| Urban or Rural/Income Group | No. | Getting Sick in Two Weeks (n %) | Annual Chronic Disease (n %) | Medical Treatment in Two Weeks (n %) a | Hospitalised (n %) |
|---|---|---|---|---|---|
| Urban and rural areas | |||||
| Rural areas | 22,669 | 5096 (22.48) | 4972 (21.93) | 1813 (8.00) | 172 (7.60) |
| Urban areas | 10,391 | 2656 (25.56) | 2741 (26.38) | 643 (6.20) | 801 (7.70) |
| χ2 | 37.780 | 78.722 | 32.501 | 0.090 | |
| p-Value | 0.000 | 0.000 | 0.000 | 0.773 | |
| Rural households | |||||
| Low-income group | 4535 | 1478 (32.59) | 1621 (35.74) | 417 (9.20) | 503 (11.10) |
| Lower middle-income group | 5170 | 1162 (22.48) | 1178 (22.79) | 414 (8.00) | 383 (7.40) |
| Middle-income group | 5333 | 1048 (19.65) | 940 (17.63) | 395 (7.40) | 357 (6.70) |
| Upper middle-income group | 4477 | 870 (19.43) | 739 (16.51) | 367 (8.20) | 295 (6.60) |
| High-income group | 3154 | 537 (17.03) | 494 (15.66) | 221 (7.00) | 189 (6.00) |
| χ2b | 281.059 | 548.474 | 8.728 | 72.491 | |
| p-Value | 0.000 | 0.000 | 0.003 | 0.000 | |
| Urban households | |||||
| Low-income group | 1064 | 282 (26.50) | 288 (27.07) | 68 (6.40) | 85 (8.00) |
| Lower middle-income group | 1669 | 439 (26.30) | 454 (27.20) | 115 (6.90) | 144 (8.60) |
| Middle-income group | 1953 | 439 (22.48) | 476 (24.37) | 95 (4.90) | 148 (7.60) |
| Upper middle-income group | 2459 | 614 (24.97) | 632 (25.70) | 157 (6.40) | 150 (6.10) |
| High-income group | 3246 | 882 (27.17) | 891 (27.45) | 209 (6.40) | 273 (8.40) |
| χ2c | 0.927 | 0.164 | 0.019 | 0.153 | |
| p-Value | 0.336 | 0.686 | 0.890 | 0.696 | |
| Income Groups | Households’ Annual Medical and Health Expenditure | Outpatient Expenditure | Hospitalisation Expenditure | |||
|---|---|---|---|---|---|---|
| No. | M (Q) | No. | M (Q) | No. | M (Q) | |
| Urban and rural areas | ||||||
| Rural areas | 6000 | 1000 (2000) | 1126 | 50 (180) | 1232 | 2500 (3789.25) |
| Urban areas | 6006 | 1300 (2500) | 1336 | 40 (137) | 1296 | 2000 (4000) |
| U | 118,197,131.5 | 673,924.5 | 709,269.5 | |||
| p-Value | 0.000 | 0.000 | 0.000 | |||
| Rural households | ||||||
| Low-income group | 1200 | 1000 (2700) | 219 | 60 (180) | 282 | 2000 (3141) |
| Lower middle-income group | 1200 | 1000 (1600) | 230 | 60 (180) | 252 | 2850 (3600) |
| Middle-income group | 1200 | 1000 (1725) | 220 | 50 (180) | 236 | 2550 (3500) |
| Upper middle-income group | 1200 | 1000 (2000) | 255 | 45 (183) | 218 | 2300 (1900) |
| High-income group | 1200 | 1000 (2000) | 202 | 45 (185) | 244 | 2800 (4100) |
| χ2 | 4.151 | 5.036 | 14.411 | |||
| p-Value | 0.386 | 0.284 | 0.006 | |||
| Urban households | ||||||
| Low-income group | 1201 | 1000 (2140) | 270 | 35 (107) | 305 | 1800 (4700) |
| Lower middle-income group | 1201 | 1000 (2500) | 298 | 33 (108) | 275 | 1580 (3500) |
| Middle-income group | 1201 | 1000 (2500) | 269 | 50 (185) | 272 | 2000 (4075) |
| Upper middle-income group | 1201 | 1700 (3000) | 269 | 40 (135) | 225 | 2000 (3450) |
| High-income group | 1202 | 2000 (4000) | 230 | 50 (198) | 219 | 2400 (4000) |
| χ2 | 172.689 | 2.778 | 16.72 | |||
| p-Value | 0.000 | 0.596 | 0.002 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, J.; Zheng, J.; Xu, L.; Wu, H. Equity of Health Services Utilisation and Expenditure among Urban and Rural Residents under Universal Health Coverage. Int. J. Environ. Res. Public Health 2021, 18, 593. https://doi.org/10.3390/ijerph18020593
Xu J, Zheng J, Xu L, Wu H. Equity of Health Services Utilisation and Expenditure among Urban and Rural Residents under Universal Health Coverage. International Journal of Environmental Research and Public Health. 2021; 18(2):593. https://doi.org/10.3390/ijerph18020593
Chicago/Turabian StyleXu, Jianqiang, Juan Zheng, Lingzhong Xu, and Hongtao Wu. 2021. "Equity of Health Services Utilisation and Expenditure among Urban and Rural Residents under Universal Health Coverage" International Journal of Environmental Research and Public Health 18, no. 2: 593. https://doi.org/10.3390/ijerph18020593
APA StyleXu, J., Zheng, J., Xu, L., & Wu, H. (2021). Equity of Health Services Utilisation and Expenditure among Urban and Rural Residents under Universal Health Coverage. International Journal of Environmental Research and Public Health, 18(2), 593. https://doi.org/10.3390/ijerph18020593




