The Economic Impact of Rectal Cancer: A Population-Based Study in Italy
Abstract
1. Introduction
2. Materials
2.1. Data Sources
2.2. Study Cohort
3. Methods
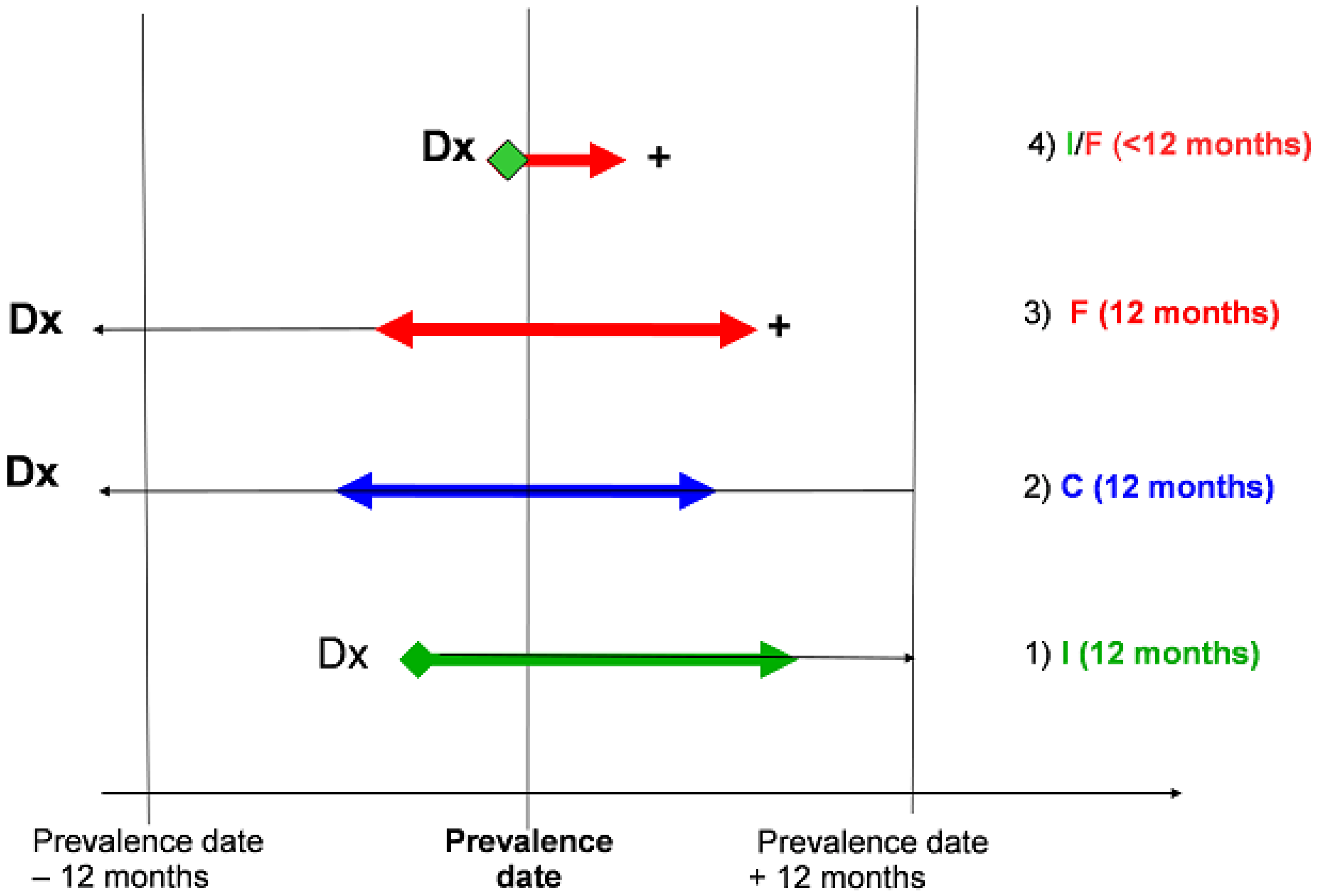
3.1. Phase of Care Prevalence
3.2. Definition and Calculation of Costs by Phase of Care
3.3. Care Patterns by Phase of Disease
3.4. Statistics
4. Results
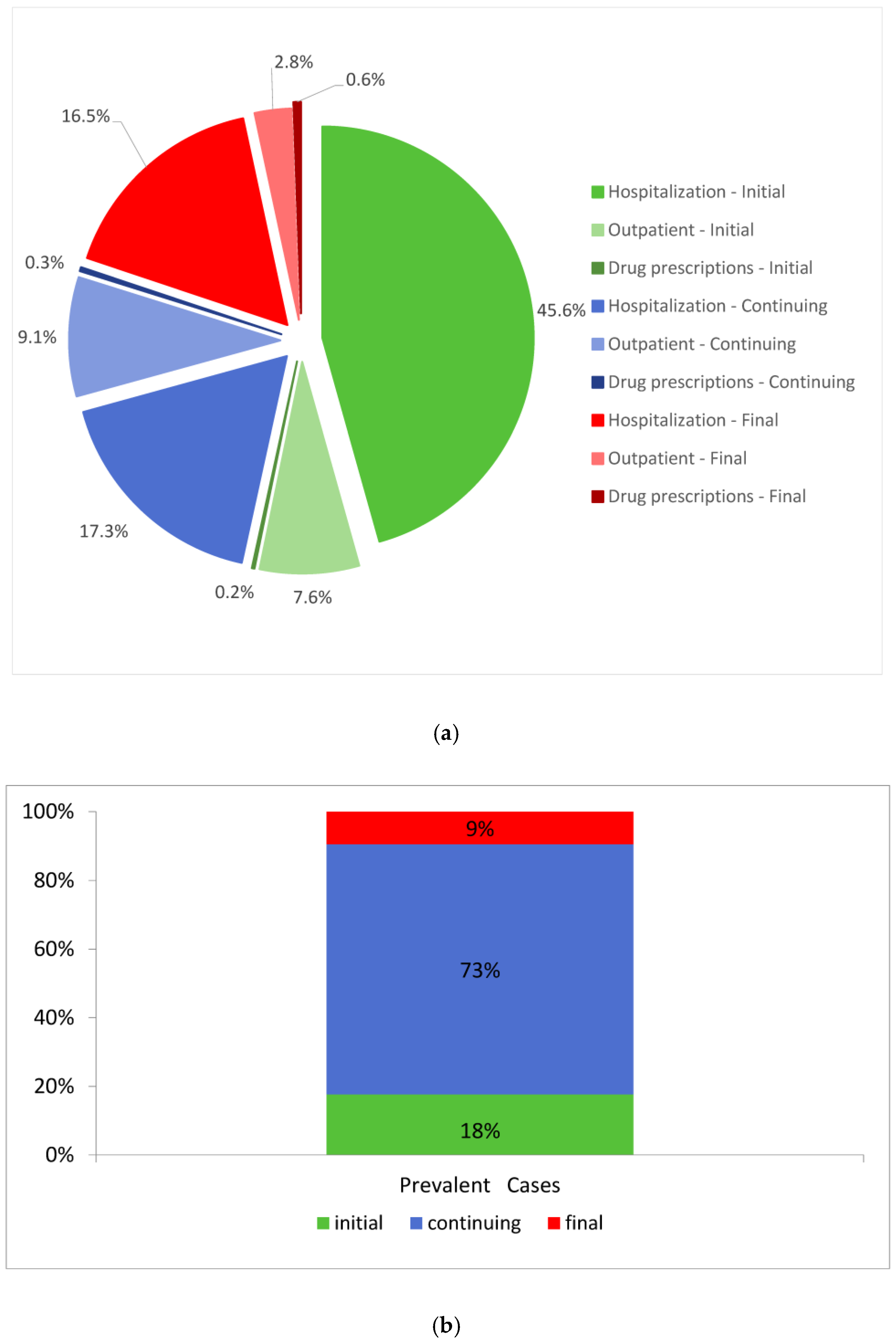
4.1. Overall Costs
4.2. Costs by Cancer Registry
4.3. Focus on Initial Phase of Care
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ATC | Anatomical Therapeutic Chemical |
| CR | Cancer Registry |
| CRs | Cancer Registries |
| DP | Drug Prescriptions database |
| DRG | Diagnosis-related Group |
| ER | Emergency Room |
| ICD9-CM | International Classification of Diseases, 9th Revision-Clinical Modification |
| ICD-10 | International Classification of Diseases-Tenth Revision |
| HD | Hospital Discharge database |
| NHS | National Health Service |
| OPS | Outpatient Services database |
| VG | Venezia Giulia |
Appendix A
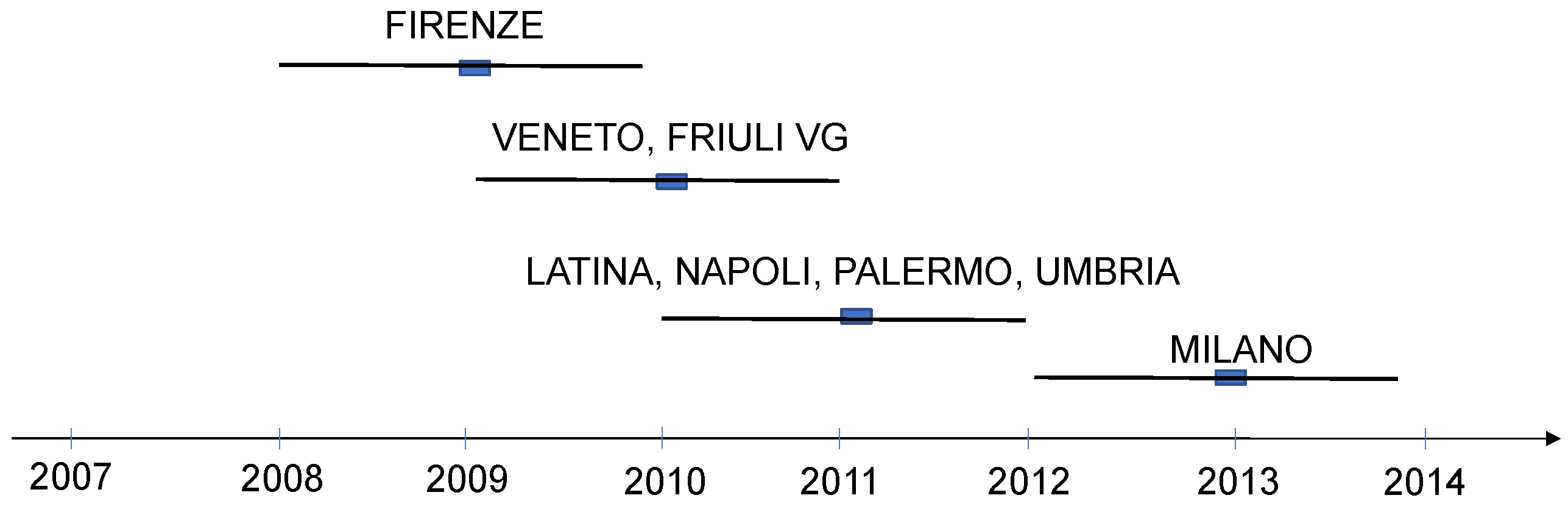
- period of incidence in Firenze CR is 2001–2008; prevalence date is 1 January 2009; data for cost analysis is in period 1 January 2008 to 31 December 2009;
- period of incidence in Veneto and Friuli VG CRs is 2002–2009; prevalence date is 1 January 2010; data for cost analysis is in period 1 January 2009 to 31 December 2010;
- period of incidence in Latina, Napoli, Palermo and Umbria CRs is 2003–2010; prevalence date is 1 January 2011; data for cost analysis is in period 1 January 2010 to 31 December 2011;
- period of incidence in Milano CR is 2005–2012; prevalence date is 1 January 2013; data for cost analysis is in period 1 January 2012 to 31 December 2013.
References
- Goldstein, D.A.; Clark, J.; Tu, Y.; Zhang, J.; Fang, F.; Goldstein, R.; Stemmer, S.M.; Rosenbaum, E. A global comparison of the cost of patented cancer drugs in relation to global differences in wealth. Oncotarget 2017, 8, 71548–71555. [Google Scholar] [CrossRef]
- Sullivan, R.; Peppercorn, J.; Sikora, K.; Zalcberg, J.; Meropol, N.J.; Amir, E.; Khayat, D.; Boyle, P.; Autier, P.; Tannock, I.F.; et al. Delivering affordable cancer in high -income countries. Lancet Oncol. 2011, 12, 933–980. [Google Scholar] [CrossRef]
- Sartorius, K.; Sartorius, B.; Govender, P.S.; Sharma, V.; Sheriff, A. The future cost of cancer in South Africa: An interdisciplinary cost management strategy. S. Afr. Med. J. 2016, 106, 949–950. [Google Scholar] [CrossRef] [PubMed]
- Kimman, M.; Jan, S.; Kingston, D.; Monaghan, H.; Sokha, E.; Thabrany, H.; Bounxouei, B.; Bhoo-Pathy, N.; Khin, M.; Cristal-Luna, G.; et al. Socioeconomic Impact of Cancer in Member Countries of the Association of Southeast Asian Nations (ASEAN): The ACTION Study Protocol. Asian Pac. J. Cancer Prev. 2012, 13, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, R.; Strasser-Weippl, K.; Touya, D.; Vincent, C.H.; Hernandez-Blanquisett, A.; Louis, J.S.; Bukowski, A.; Goss, P.E. Improving Access to High-Cost Cancer Drugs in Latin America: Much to Be Done. Cancer 2017, 123, 1313–1323. [Google Scholar] [CrossRef]
- Ades, F.; Senterre, C.; de Azambuja1, E.; Sullivan, R.; Popescu, R.; Parent, F.; Piccart, M. Discrepancies in cancer incidence and mortality and its relationship to health expenditure in the 27 European Union member states. Ann. Oncol. 2013, 24, 2897–2902. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, B.; Hofmarcher, T.; Lindgren, P.; Wilking, N. The cost and burden of cancer in the European Union 1995–2014. Eur. J. Cancer 2016, 66, 162–170. [Google Scholar] [CrossRef]
- Luengo-Fernandez, R.; Leal, J.; Gray, A.; Sullivan, R. Economic burden of cancer across the European Union: A population-based cost analysis. Lancet Oncol. 2013, 14, 1165–1174. [Google Scholar] [CrossRef]
- de Oliveira, C.; Weir, S.; Rangrej, J.; Krahn, M.D.; Mittmann, N.; Hoch, J.S.; Chan, K.K.W.; Peacock, S. The economic burden of cancer care in Canada: A population-based cost study. CMAJ Open 2018, 6, E1–E10. [Google Scholar] [CrossRef]
- Scalo, J.F.; Rascati, K.L. Trends and issues in oncology costs. Expert Rev. Pharmacoecon. Outcomes Res. 2014, 14, 35–44. [Google Scholar] [CrossRef]
- Blakely, T.; Atkinson, J.; NZC Statistics; Kvizhinadze, G.; Wilson, N.; Davies, A.; Clarke, P. Patterns of Cancer Care Costs in a Country with Detailed Individual Data. Med. Care 2015, 53, 302–309. [Google Scholar] [CrossRef]
- Torkki, P.; Leskelä, R.-L.; Linna, M.; Mäklin, S.; Mecklin, J.-P.; Bono, P.; Kataja, V.; Karjalainen, S. Cancer costs and outcomes for common cancer sites in the Finnish population between 2009–2014. Acta Oncol. 2018, 57, 983–988. [Google Scholar] [CrossRef] [PubMed]
- Banegas, M.P.; Yabroff, K.R.; O’Keeffe-Rosetti, M.C.; Ritzwoller, D.P.; Fishman, P.A.; Salloum, R.G.; Lafata, J.E.; Hornbrook, M.C. Medical care costs associated with cancer in integrated delivery system. J. Natl. Compr. Cancer Netw. 2018, 16, 402–410. [Google Scholar] [CrossRef] [PubMed]
- de Moor, J.S.; Mariotto, A.B.; Parry, C.; Alfano, C.M.; Padgett, L.; Kent, E.E.; Forsythe, L.; Scoppa, S.; Hachey, M.; Rowland, J.H. Cancer Survivors in the United States: Prevalence across the Survivorship Trajectory and Implications for Care. Cancer Epidemiol. Biomark. Prev. 2013, 22, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Mariotto, A.B.; Yabroff, K.R.; Shao, Y.; Feuer, E.J.; Brown, M.L. Projections of the cost of cancer care in the United States: 2010–2020. J. Natl. Cancer Inst. 2011, 103, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Laudicella, M.; Walsh, B.; Burns, E.; Smith, P.C. Cost of care for cancer patients in England: Evidence from population-based patient-level data. Br. J. Cancer 2016, 114, 1286–1292. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, C.; Pataky, R.; Bremner, K.E.; Rangrej, J.; Chan, K.K.W.; Cheung, W.Y.; Hoch, J.S.; Peacock, S.; Krahn, M.D. Phase-specific and lifetime costs of cancer care in Ontario, Canada. BMC Cancer 2016, 16, 809. [Google Scholar] [CrossRef]
- Giuliani, J.; Bonetti, A. The Pharmacological Costs of First-Line Therapies in Unselected Patients with Advanced Colorectal Cancer: A Review of Published Phase III Trials. Clin. Colorectal Cancer 2016, 15, 277–284. [Google Scholar] [CrossRef]
- Francisci, S.; Guzzinati, S.; Mezzetti, M.; Crocetti, E.; Giusti, F.; Miccinesi, G.; Paci, E.; Angiolini, C.; Gigli, A. Cost profiles of colorectal cancer patients in Italy based on individual patterns of care. BMC Cancer 2013, 13, 329. [Google Scholar] [CrossRef][Green Version]
- Capri, S.; Russo, A. Cost of breast cancer based on real-world data: A cancer registry study in Italy. BMC Health Serv. Res 2017, 17, 84. [Google Scholar] [CrossRef]
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 66, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Guzzinati, S.; Virdone, S.; De Angelis, R.; Panato, C.; Buzzoni, C.; Capocaccia, R.; Francisci, S.; Gigli, A.; Zorzi, M.; Tagliabue, G.; et al. Characteristics of people living in Italy after a cancer diagnosis in 2010 and projections to 2020. BMC Cancer 2018, 18, 169. [Google Scholar] [CrossRef]
- Associazione Italiana Registri Tumori (AIRTUM). I Numeri del Cancro 2016; Il Pensiero Scientifico Editore: Roma, Italy, 2016. [Google Scholar]
- Kobayashi, S.T.; Diz, M.D.P.E.; Campolina, A.G.; De Soárez, P.C.; Ribeiro, U., Jr.; Nahas, S.C.; Vasconcelos, K.G.M.C.; Capareli, F.; Cecconello, I.; Hoff, P.M. Integrated care pathway for rectal cancer treatment: Health care resource utilization, costs, and outcomes. Int. J. Evid. Based Healthc. 2017, 15, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Gigli, A.; Warren, J.L.; Yabroff, K.R.; Francisci, S.; Stedman, M.; Guzzinati, S.; Giusti, F.; Miccinesi, G.; Crocetti, E.; Angiolini, C.; et al. Initial Treatment for Newly Diagnosed Elderly Colorectal Cancer Patients: Patterns of Care in Italy and the United States. J. Natl. Cancer Inst. Monogr. 2013, 2013, 88–98. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yabroff, K.R.; Lamont, E.B.; Mariotto, A.; Warren, J.L.; Topor, M.; Meekins, A.; Brown, M.L. Cost of Care for Elderly Cancer Patients in the United States. J. Natl. Cancer Inst. 2008, 100, 630–641. [Google Scholar] [CrossRef] [PubMed]
- Färkkilä, N.; Torvinen, S.; Sintonen, H.; Saarto, T.; Järvinen, H.; Hänninen, J.; Taari, K.; Roine, R.P. Costs of colorectal cancer in different states of the disease. Acta Oncol. 2015, 54, 454–462. [Google Scholar] [CrossRef]
- Yabroff, K.R.; Borowski, L.; Lipscomb, J. Economic Studies in Colorectal Cancer: Challenges in Measuring and Comparing Costs. J. Natl. Cancer Inst. Monogr. 2013, 2013, 62–78. [Google Scholar] [CrossRef]
- The EPICOST Project. Available online: http://www.epicost.it (accessed on 18 September 2020).
- World Health Organization. International Classification of Diseases 9th Revision, Clinical Modification; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- WHO Collaborating Centre for Drug Statistics Methodology. ATC Classification Index with DDDs, 2019; World Health Organization: Oslo, Norway, 2018. [Google Scholar]
- Yabroff, K.R.; Lund, J.; Kepka, D.; Mariotto, A. Economic Burden of Cancer in the United States: Estimates, Projections, and Future Research. Cancer Epidemiol. Biomark. Prev. 2011, 20, 2006–2014. [Google Scholar] [CrossRef]
- Altini, M.; Solinas, L.; Bucchi, L.; Gentili, N.; Gallegati, D.; Balzi, W.; Falcini, F.; Massa, I. Assessment of Cancer Care Costs in Disease-Specific Cancer Care Pathways. Int. J. Environ. Res. Public Health 2020, 17, 4765. [Google Scholar] [CrossRef]
- Dal Maso, L.; Guzzinati, S.; Buzzoni, C.; Capocaccia, R.; Serraino, D.; Caldarella, A.; Dei Tos, A.P.; Falcini, F.; Auteliano, M.; Masanotti, G.; et al. Long-term survival, prevalence, and cure of cancer: A population-based estimation for 818,902 Italian patients and 26 cancer types. Ann. Oncol. 2014, 25, 2251–2260. [Google Scholar] [CrossRef] [PubMed]
- Zorzi, M.; Fedato, C.; Grazzini, G.; de’ Bianchi, P.S.; Naldoni, C.; Pendenza, M.; Sassatelli, R.; Senore, C.; Visioli, C.B.; Zappa, M. Screening for colorectal cancer in Italy, 2010 survey. Epidemiol. Prev. 2012, 36, 55–77. [Google Scholar] [PubMed]
- Corti, M.C.; Avossa, F.; Schievano, E.; Gallina, P.; Ferroni, E.; Alba, N.; Dotto, M.; Basso, C.; Netti, S.T.; Fedeli, U.; et al. A case-mix classification system for explaining healthcare costs using administrative data in Italy. Eur. J. Int. Med. 2018, 54, 13–16. [Google Scholar] [CrossRef] [PubMed]
- The iPAAC Project. Available online: https://www.ipaac.eu (accessed on 30 November 2020).


| Cancer Registry | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Firenze | Friuli VG | Latina | Milano | Napoli | Palermo | Umbria | Veneto | PooL | ||
| Population coverage | Counts | 1,211,074 | 1,219,493 | 537,590 | 3,300,881 | 1,163,644 | 1,240,830 | 879,993 | 629,993 | 10,183,498 |
| % Males | 47.9 | 48.3 | 48.8 | 48.1 | 48.5 | 48.2 | 48.1 | 49.3 | 48.3 | |
| Regional Coverage | 33.3% | 100% | 9.8% | 33.7% | 20.2% | 24.8% | 100% | 13.0% | 27.8% | |
| Prevalence | Date (January 1st) | 2009 | 2010 | 2011 | 2013 | 2011 | 2011 | 2011 | 2010 | |
| 8-year Incidence | 2001–2008 | 2002–2009 | 2003–2010 | 2005–2012 | 2003–2010 | 2003–2010 | 2003–2010 | 2002–2009 | ||
| Cases | 1495 | 1407 | 477 | 2671 | 540 | 1006 | 1166 | 596 | 9358 | |
| % Males | 56.5 | 57.2 | 59.7 | 57.9 | 52.8 | 55.9 | 59 | 58.2 | 57.3 | |
| Cases within 1 year | 227 | 270 | 78 | 409 | 128 | 176 | 211 | 105 | 1604 | |
| Unstaged | 21.6% | 33.0% | 25.4% | 11.3% | 10.9% | 24.4% | 11.4% | 6.7% | ||
| Average events in a year | Hospital Admissions | 0.7 | 0.7 | 0.7 | 0.6 | 2.1 | 0.9 | 0.7 | 0.5 | 0.8 |
| Outpatient Services | 35.3 | 43.8 | 45 | 38.8 | 51.5 | 38.1 | 35.2 | 32.1 | 39.1 | |
| Drug Prescriptions | 1.7 | 1.7 | 1.8 | 1.1 | 2.5 | 1.8 | 2 | 1.6 | 1.6 | |
| Initial Phase | |||||
| Age | Prevalent Cases a | Hospitalization b | Outpatient b | Drug Prescription b | Total Costs c |
| 15–49 | 99 | 14,425 | 2787 | 67 | 17,279 |
| 50–69 | 739 | 12,379 | 2590 | 58 | 15,027 |
| 70–79 | 529 | 12,209 | 2169 | 88 | 14,466 |
| 80+ | 255 | 10,372 | 966 | 27 | 11,365 |
| Continuing Phase | |||||
| Age | Prevalent Cases a | Hospitalization b | Outpatient b | Drug Prescription b | Total Costs c |
| 15–49 | 281 | 1446 | 857 | 11 | 2314 |
| 50–69 | 2714 | 1301 | 731 | 21 | 2053 |
| 70–79 | 2239 | 912 | 594 | 19 | 1525 |
| 80+ | 1443 | 641 | 348 | 22 | 1011 |
| Final Phase | |||||
| Age | Prevalent Cases a | Hospitalization b | Outpatient b | Drug Prescription b | Total Costs c |
| 15–49 | 30 | 16,180 | 2398 | 989 | 19,567 |
| 50–69 | 227 | 12,497 | 2786 | 597 | 15,880 |
| 70–79 | 233 | 9598 | 1621 | 223 | 11,442 |
| 80+ | 378 | 3933 | 517 | 112 | 4562 |
| Cancer Registry | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Phase of Care | Firenze | Friuli VG | Latina | Milano | Napoli | Palermo | Umbria | Veneto | PooL a | |
| Initial | Prevalent Cases b | 229 | 274 | 79 | 413 | 130 | 178 | 213 | 106 | 1622 |
| Hospitalization c | 13,418 | 14,353 | 10,854 | 9311 | 13,345 | 11,362 | 14,987 | 9638 | 12,159 | |
| Outpatient c | 841 | 2807 | 1686 | 3509 | 1785 | 1041 | 1349 | 3150 | 2021 | |
| Drug Prescription c | 13 | 27 | 80 | 154 | 57 | 46 | 24 | 23 | 53 | |
| Total costs c | 14,271 | 17,187 | 12,620 | 12,973 | 15,186 | 12,448 | 16,360 | 12,810 | 14,232 | |
| Continuing | Prevalent Cases b | 1075 | 983 | 350 | 1989 | 337 | 706 | 812 | 425 | 6677 |
| Hospitalization c | 1195 | 1164 | 1133 | 754 | 2059 | 777 | 1394 | 480 | 1120 | |
| Outpatient c | 398 | 733 | 550 | 745 | 638 | 495 | 465 | 687 | 589 | |
| Drug Prescription c | 20 | 21 | 18 | 22 | 21 | 17 | 15 | 23 | 20 | |
| Total costs c | 1612 | 1919 | 1701 | 1522 | 2717 | 1289 | 1874 | 1190 | 1728 | |
| Final | Prevalent Cases b | 168 | 118 | 40 | 219 | 56 | 98 | 119 | 52 | 868 |
| Hospitalization c | 7595 | 12,680 | 6730 | 6236 | 11,231 | 7494 | 8592 | 5143 | 8213 | |
| Outpatient c | 627 | 2148 | 608 | 2365 | 1640 | 861 | 805 | 2059 | 1389 | |
| Drug Prescription c | 261 | 342 | 186 | 353 | 348 | 401 | 180 | 211 | 285 | |
| Total costs c | 8483 | 15,170 | 7524 | 8954 | 13,219 | 8756 | 9578 | 7412 | 9887 | |
| Grand Total costs d | 6,423,658 | 8,385,964 | 1,886,562 | 10,345,333 | 3,630,197 | 3,975,765 | 6,145,767 | 2,252,122 | 43,206,310 | |
| Cancer Registry | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Stage | Firenze | Friuli VG | Latina | Milano | Napoli | Palermo | Umbria | Veneto | Pool a | |
| Prevalent cases b | I | 30 | 80 | 7 | 46 | 14 | 11 | 87 | 44 | 319 |
| II | 83 | 36 | 26 | 136 | 50 | 57 | 35 | 16 | 439 | |
| III | 49 | 51 | 19 | 149 | 33 | 45 | 45 | 27 | 418 | |
| IV | 16 | 14 | 6 | 32 | 17 | 20 | 20 | 11 | 136 | |
| NA | 49 | 89 | 20 | 45 | 14 | 43 | 24 | 7 | 291 | |
| Hospitalization c | I | 10,912 | 9086 | 13,204 | 7393 | 9062 | 6616 | 11,584 | 8141 | 9500 |
| II | 13,543 | 15,806 | 8413 | 10,284 | 12,027 | 9798 | 16,996 | 8900 | 11,971 | |
| III | 17,528 | 15,176 | 14,086 | 9130 | 13,545 | 12,171 | 18,602 | 12,367 | 14,076 | |
| IV | 20,752 | 21,171 | 14,005 | 8892 | 17,547 | 16,416 | 18,381 | 11,207 | 16,046 | |
| NA | 6624 | 15,728 | 8506 | 5327 | 12,610 | 10,606 | 11,584 | 5241 | 9528 | |
| Outpatient c | I | 790 | 951 | 2896 | 993 | 972 | 540 | 1013 | 876 | 1129 |
| II | 781 | 2769 | 1267 | 3357 | 1847 | 731 | 1236 | 3392 | 1922 | |
| III | 969 | 5081 | 1789 | 4146 | 1967 | 1269 | 1845 | 5693 | 2845 | |
| IV | 1224 | 5178 | 3504 | 4936 | 1904 | 1810 | 1437 | 5696 | 3211 | |
| NA | 701 | 2872 | 1233 | 3220 | 1955 | 1003 | 1722 | 3080 | 1973 | |
| Drug Prescription c | I | 8 | 8 | 35 | 14 | 27 | 6 | 13 | 5 | 15 |
| II | 15 | 13 | 16 | 81 | 20 | 8 | 55 | 47 | 32 | |
| III | 4 | 26 | 204 | 264 | 89 | 66 | 17 | 24 | 87 | |
| IV | 21 | 32 | 168 | 246 | 123 | 141 | 34 | 6 | 96 | |
| NA | 14 | 49 | 36 | 47 | 23 | 42 | 17 | 105 | 42 | |
| Total Costs c | I | 11,710 | 10,045 | 16,136 | 8400 | 10,061 | 7163 | 12,610 | 9022 | 10,643 |
| II | 14,338 | 18,588 | 9696 | 13,722 | 13,893 | 10,537 | 18,287 | 12,340 | 13,925 | |
| III | 18,501 | 20,283 | 16,080 | 13,540 | 15,601 | 13,506 | 20,465 | 18,084 | 17,007 | |
| IV | 21,997 | 26,381 | 17,677 | 14,074 | 19,573 | 18,367 | 19,852 | 16,909 | 19,354 | |
| NA | 7339 | 18,648 | 9776 | 8593 | 14,588 | 11,652 | 13,323 | 8426 | 11,543 | |
| Treatment Regimen | Age at Prevalence | Stage at Diagnosis | Total | ||||
|---|---|---|---|---|---|---|---|
| I | II | III | IV | X | |||
| Prevalent cases a | 15–49 | 10 | 22 | 33 | 19 | 14 | 98 |
| 50–69 | 163 | 180 | 204 | 65 | 124 | 736 | |
| 70–79 | 100 | 164 | 118 | 41 | 100 | 523 | |
| 80+ | 46 | 73 | 63 | 11 | 54 | 247 | |
| Patients (%) receiving surgery treatment b | 15–49 | 90 | 91 | 94 | 84 | 86 | 90 |
| 50–69 | 88 | 92 | 96 | 85 | 73 | 88 | |
| 70–79 | 79 | 96 | 97 | 80 | 72 | 87 | |
| 80+ | 80 | 96 | 98 | 91 | 54 | 84 | |
| Patients (%) receiving chemo-therapy b | 15–49 | 10 | 55 | 64 | 68 | 43 | 56 |
| 50–69 | 11 | 29 | 66 | 82 | 43 | 43 | |
| 70–79 | 7 | 21 | 47 | 54 | 33 | 30 | |
| 80+ | 2 | 4 | 13 | 9 | 6 | 6 | |
| Patients (%) receiving neoadjuvant chemo-therapy c | 15–49 | 10 | 32 | 18 | 16 | 57 | 26 |
| 50–69 | 7 | 18 | 12 | 22 | 26 | 15 | |
| 70–79 | 5 | 4 | 8 | 12 | 17 | 8 | |
| 80+ | 0 | 0 | 0 | 0 | 1.9 | 0.4 | |
| Patients (%) receiving radio-therapy b | 15–49 | 10 | 41 | 42 | 32 | 57 | 40 |
| 50–69 | 15 | 35 | 40 | 22 | 37 | 31 | |
| 70–79 | 12 | 26 | 33 | 24 | 38 | 27 | |
| 80+ | 22 | 16 | 13 | 0 | 19 | 14 | |
| Patients (%) receiving neoadjuvant radio-therapy c | 15–49 | 10 | 14 | 15 | 11 | 50 | 18 |
| 50–69 | 10 | 18 | 11 | 11 | 21 | 14 | |
| 70–79 | 8 | 10 | 13 | 7 | 13 | 11 | |
| 80+ | 11 | 7 | 2 | 0 | 9 | 6 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gigli, A.; Francisci, S.; Capodaglio, G.; Pierannunzio, D.; Mallone, S.; Tavilla, A.; Lopez, T.; Zorzi, M.; Stracci, F.; Busco, S.; et al. The Economic Impact of Rectal Cancer: A Population-Based Study in Italy. Int. J. Environ. Res. Public Health 2021, 18, 474. https://doi.org/10.3390/ijerph18020474
Gigli A, Francisci S, Capodaglio G, Pierannunzio D, Mallone S, Tavilla A, Lopez T, Zorzi M, Stracci F, Busco S, et al. The Economic Impact of Rectal Cancer: A Population-Based Study in Italy. International Journal of Environmental Research and Public Health. 2021; 18(2):474. https://doi.org/10.3390/ijerph18020474
Chicago/Turabian StyleGigli, Anna, Silvia Francisci, Giulia Capodaglio, Daniela Pierannunzio, Sandra Mallone, Andrea Tavilla, Tania Lopez, Manuel Zorzi, Fabrizio Stracci, Susanna Busco, and et al. 2021. "The Economic Impact of Rectal Cancer: A Population-Based Study in Italy" International Journal of Environmental Research and Public Health 18, no. 2: 474. https://doi.org/10.3390/ijerph18020474
APA StyleGigli, A., Francisci, S., Capodaglio, G., Pierannunzio, D., Mallone, S., Tavilla, A., Lopez, T., Zorzi, M., Stracci, F., Busco, S., Mazzucco, W., Lonardi, S., Bianconi, F., Russo, A. G., Iacovacci, S., Serraino, D., Manneschi, G., Fusco, M., Cusimano, R., ... Guzzinati, S. (2021). The Economic Impact of Rectal Cancer: A Population-Based Study in Italy. International Journal of Environmental Research and Public Health, 18(2), 474. https://doi.org/10.3390/ijerph18020474







