Spatial Accessibility Assessment of Prehospital EMS with a Focus on the Elderly Population: A Case Study in Ningbo, China
Abstract
1. Introduction
2. Materials and Methods
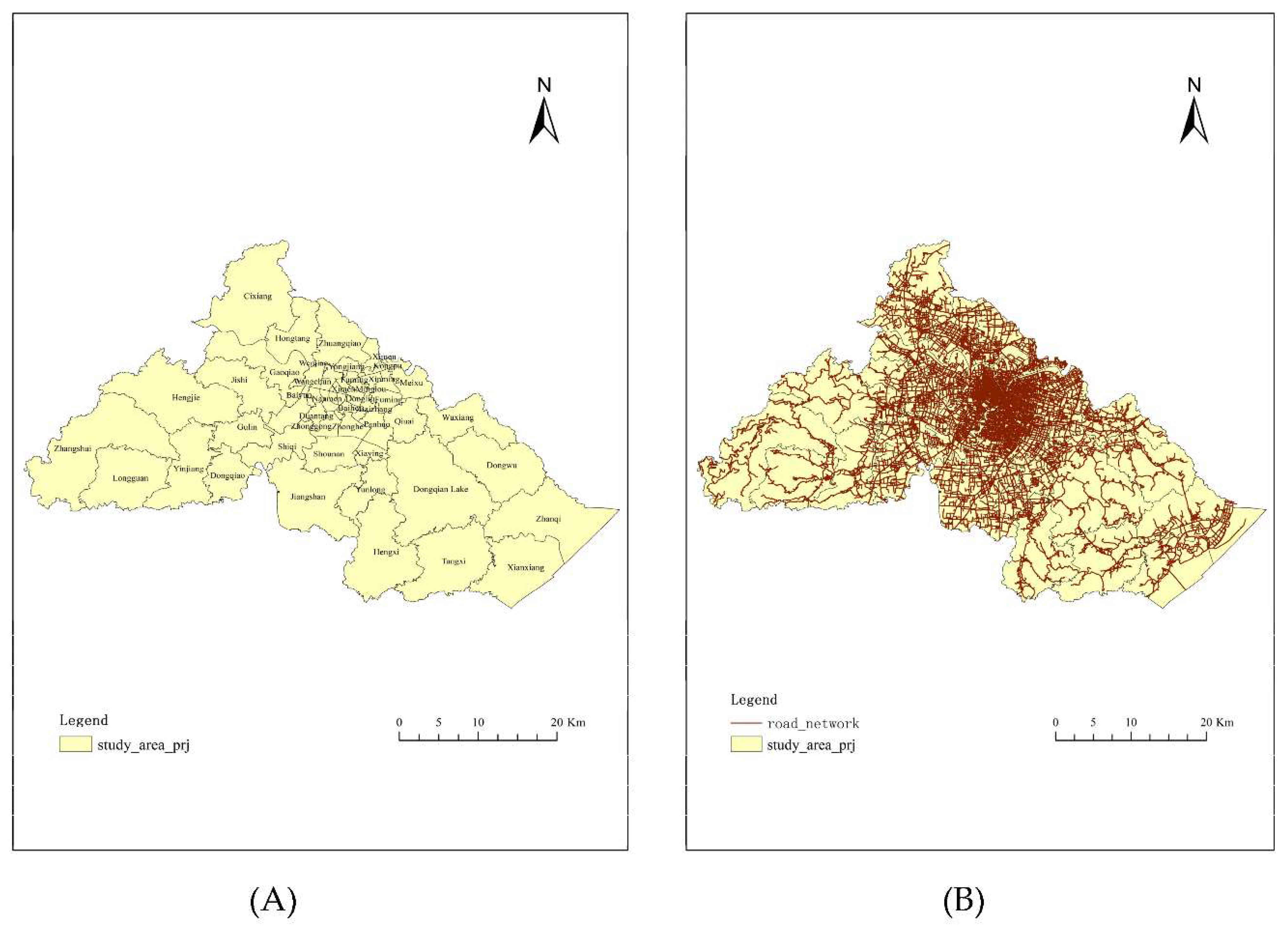
2.1. Study Area and Study Population
2.2. Data Collection and Sources
2.2.1. Elderly Population Data
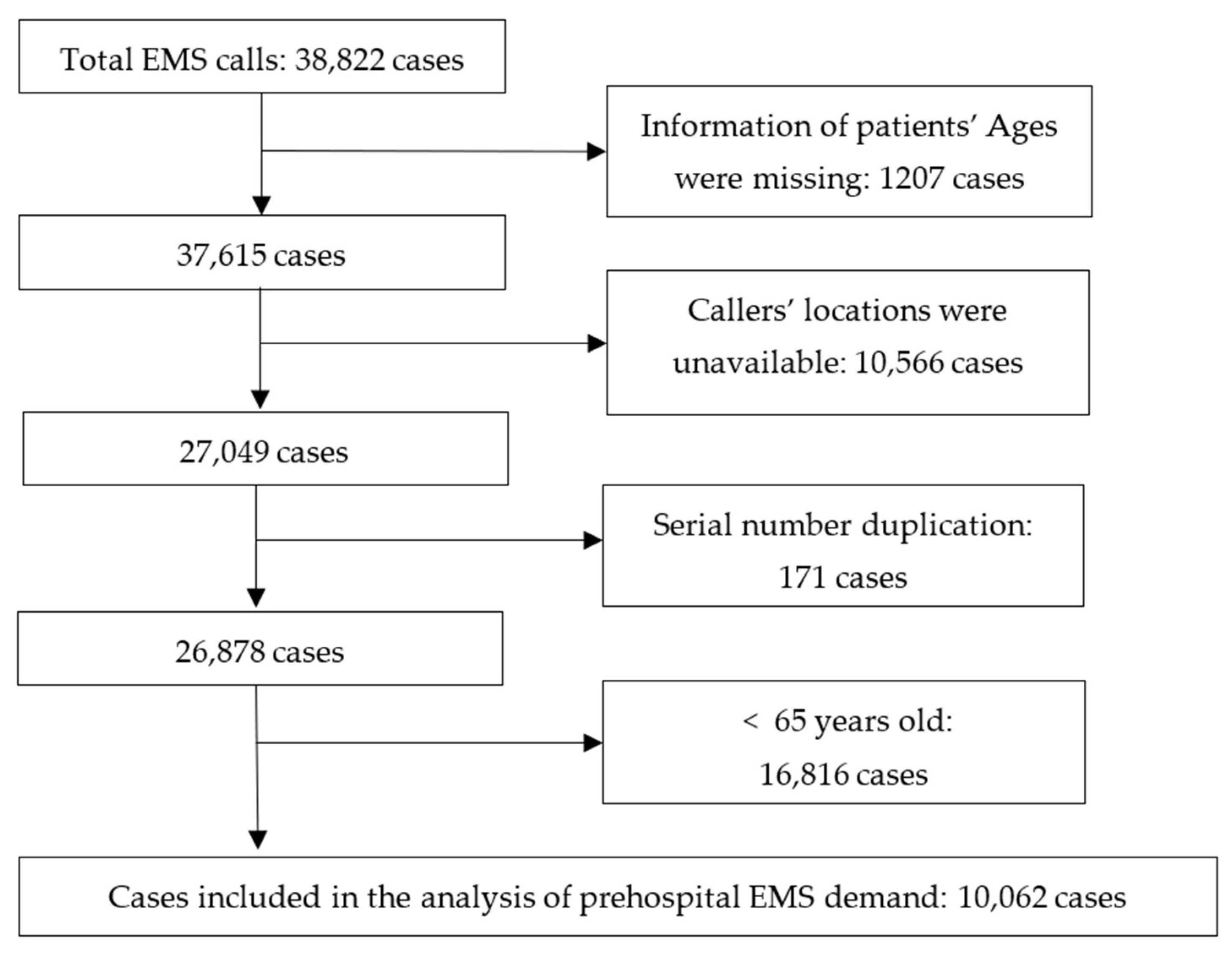
2.2.2. Elderly’s Emergency Call Data
2.2.3. Ambulance Bases Data
2.2.4. Administration Boundary Data
2.2.5. Road Network
2.3. Methodology
2.3.1. Stage 1: Data Process
2.3.2. Stage 2: Measuring Spatial Accessibility
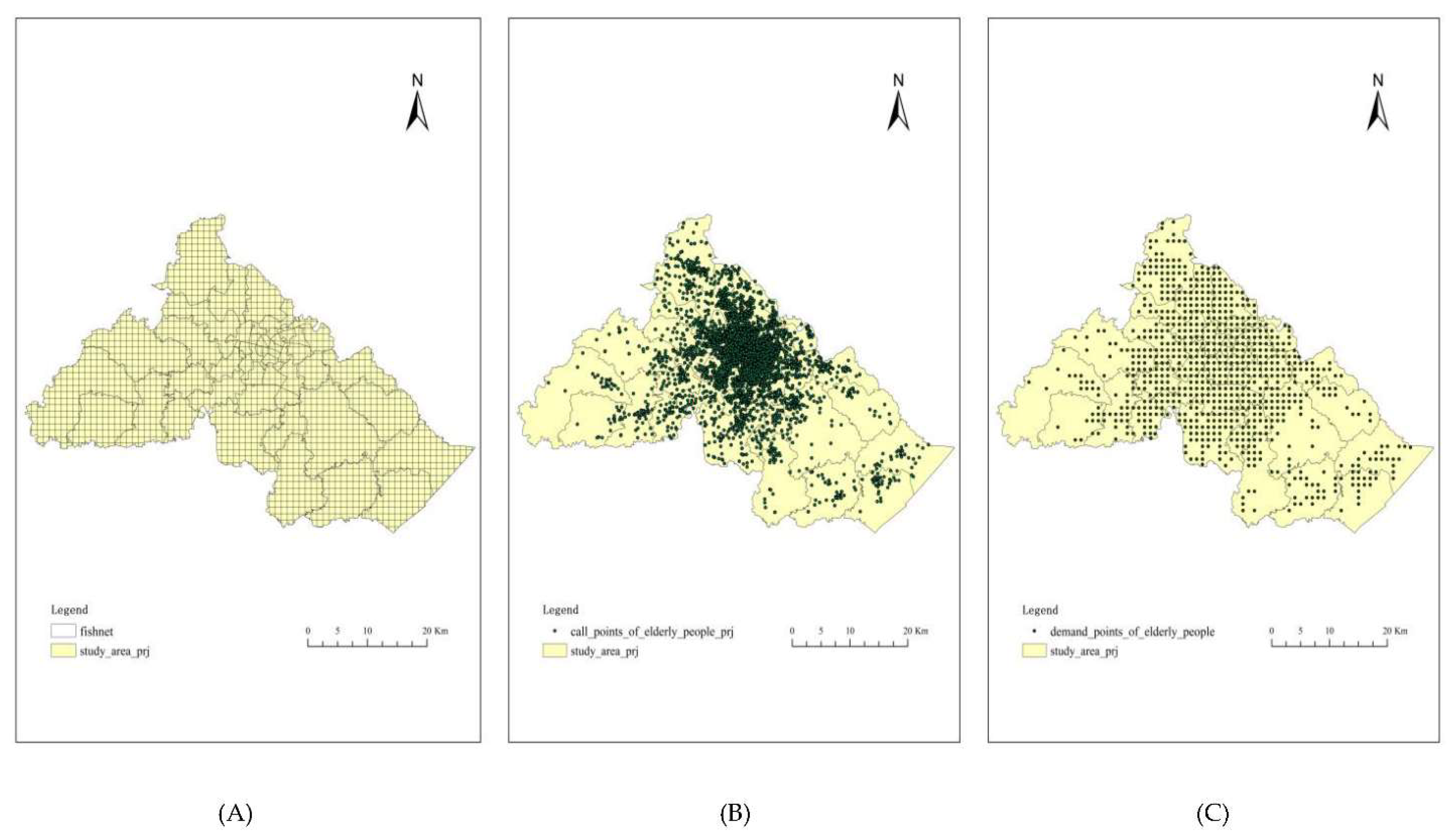
- Step 1: Definition of demand points
- Step 2: Locating the current ambulance bases
- Step 3: Evaluation of the spatial accessibility of demand points
2.3.3. Stage 3: Measuring Spatial Equilibrium of the Whole Study Area
3. Results
3.1. Basic Characteristics of the Study Elderly Population
3.2. Distribution Characteristics of the Elderly’s Demand for Prehospital EMS
3.2.1. Time Distribution
3.2.2. Disease Distribution
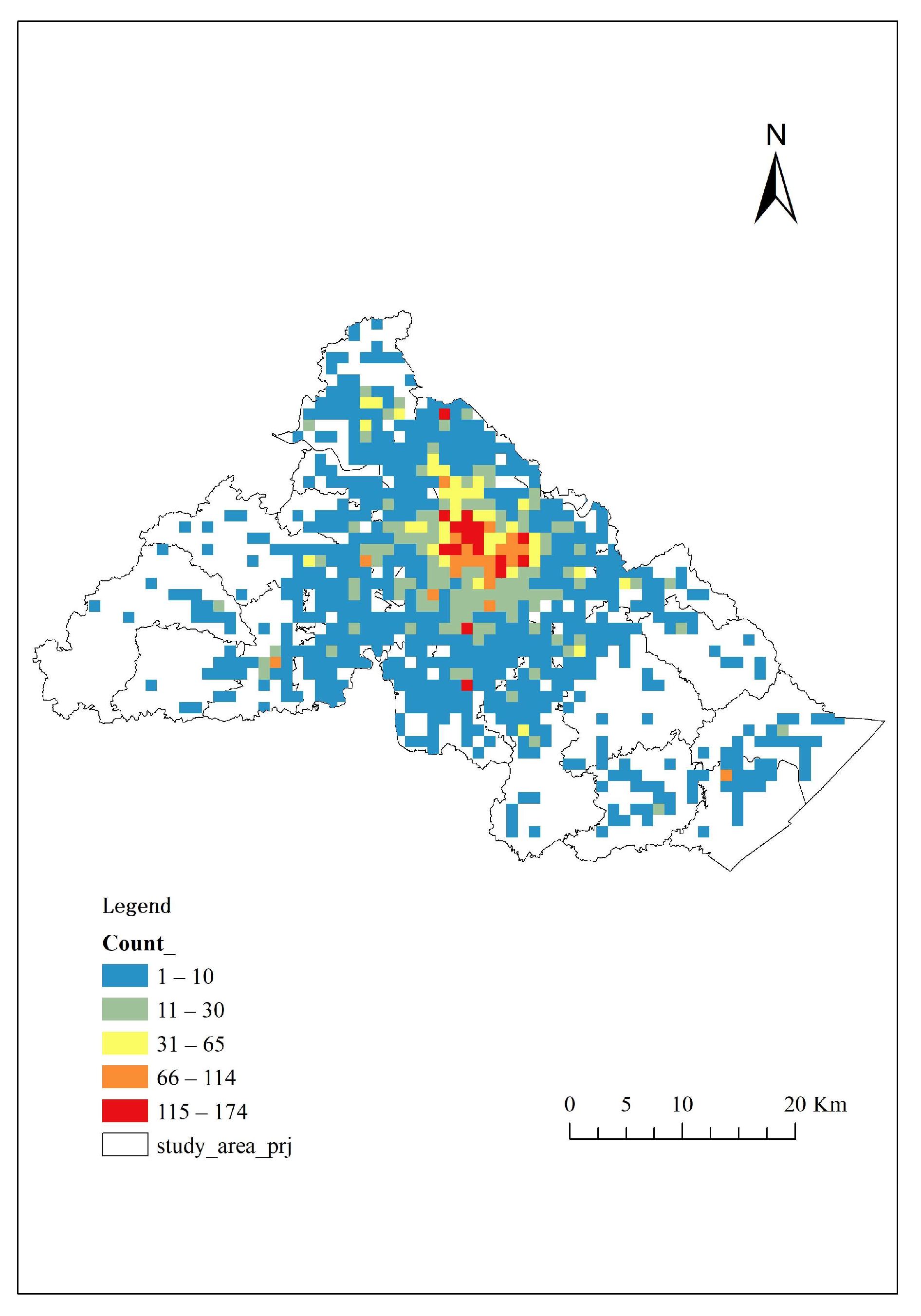
3.2.3. Calls’ Spatial Distribution
3.2.4. Demand Points’ Spatial Distribution
3.3. The Elderly’s Spatial Accessibility of Prehospital EMS
3.4. Spatial Equilibrium of the Elderly’s Spatial Accessibility to Prehospital EMS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mackenzie, R. Brief history of pre-hospital emergency medicine. Emerg. Med. J. 2018, 35, 146–148. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.H.; Habig, K.; Wright, C.; Hughes, A.; Davies, G.; Imray, C.H. Pre-hospital emergency medicine. Lancet 2015, 386, 2526–2534. [Google Scholar] [CrossRef]
- Lowthian, J.A.; Jolley, D.J.; Curtis, A.J.; Currell, A.; Cameron, P.A.; Stoelwinder, J.U.; McNeil, J.J. The challenges of population ageing: Accelerating demand for emergency ambulance services by older patients, 1995–2015. Med. J. Aust. 2011, 194, 574–578. [Google Scholar] [CrossRef] [PubMed]
- Dinh, M.M.; Muecke, S.; Berendsen Russell, S.; Chalkley, D.; Bein, K.J.; Muscatello, D.; Nagaraj, G.; Paoloni, R.; Ivers, R. Demand for emergency services trends in New South Wales years 2010–2014 (Destiny): Age and clinical factors associated with ambulance transportation to emergency departments. Prehospital Emerg. Care 2016, 20, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Lowthian, J.A.; Cameron, P.A.; Stoelwinder, J.U.; Curtis, A.; Currell, A.; Cooke, M.W.; McNeil, J.J. Increasing utilisation of emergency ambulances. Aust. Health Rev. 2011, 35, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Stathers, G.M.; Delpech, V.; Raftos, J.R. Factors influencing the presentation and care of elderly people in the emergency department. Med. J. Aust. 1992, 156, 197–200. [Google Scholar] [CrossRef]
- Strange, G.R.; Chen, E.H.; Sanders, A.B. Use of emergency departments by elderly patients: Projections from a multicenter data base. Ann. Emerg. Med. 1992, 21, 819–824. [Google Scholar] [CrossRef]
- Singal, B.M.; Hedges, J.R.; Rousseau, E.W.; Sanders, A.B.; Berstein, E.; McNamara, R.M.; Hogan, T.M. Geriatric patient emergency visits part I: Comparison of visits by geriatric and younger patients. Ann. Emerg. Med. 1992, 21, 802–807. [Google Scholar] [CrossRef]
- Keskinoglu, P.; Sofuoglu, T.; Ozmen, O.; Gunduz, M.; Ozkan, M. Older people’s use of pre-hospital emergency medical services in Izmir, Turkey. Arch. Gerontol. Geriatr. 2010, 50, 356–360. [Google Scholar] [CrossRef]
- Van Mechelen, M.F. The aging of the population; social & economic consequences & problems. Le Scalpel (Brux) 1957, 110, 591–599. [Google Scholar]
- Office for National Statistics Overview of the UK Population: January 2021. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/january2021 (accessed on 5 September 2021).
- National Institute of Statistics and Economics Demographic Balance Sheet 2020. Available online: https://www.insee.fr/en/accueil (accessed on 5 September 2021).
- The World Bank Population Ages 65 and Above (% of Total Population)—United States. Available online: https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?locations=US&view=chart (accessed on 5 September 2021).
- Statistics Bureau of Japan Population Census. Available online: http://www.stat.go.jp/english/index.html (accessed on 5 September 2021).
- Statistics Korea 2020 Population and Housing Census (Register-based Census). Available online: http://kostat.go.kr/portal/eng/pressReleases/8/7/index.board?bmode=read&bSeq=&aSeq=391585&pageNo=1&rowNum=10&navCount=10&currPg=&searchInfo=&sTarget=title&sTxt= (accessed on 5 September 2021).
- Australian Bureau of Statistics Disability, Ageing and Carers, Australia: Summary of Findings. Available online: https://www.abs.gov.au/statistics/health/disability/disability-ageing-and-carers-australia-summary-findings/2018 (accessed on 5 September 2021).
- Nogueira, L.C., Jr.; Pinto, L.R.; Silva, P.M.S. Reducing emergency medical service response time via the reallocation of ambulance bases. Health Care Manag. Sci. 2016, 19, 31–42. [Google Scholar] [CrossRef]
- National Bureau of Statistics Bulletin of the Seventh National Census (No. 5). Available online: http://www.stats.gov.cn/ztjc/zdtjgz/zgrkpc/dqcrkpc/ggl/202105/t20210519_1817698.html (accessed on 1 August 2021).
- Yang, G.; Wang, Y.; Zeng, Y.; Gao, G.F.; Liang, X.; Zhou, M.; Wan, X.; Yu, S.; Jiang, Y.; Naghavi, M.; et al. Rapid health transition in China, 1990–2010: Findings from the global burden of disease study 2010. Lancet 2013, 381, 1987–2015. [Google Scholar] [CrossRef]
- Zhao, S.; Cao, Y.; Lei, Y.; Liu, F.; Shao, S.; Liu, J.; Nie, D.; Yang, N.; Liu, M. Population ageing and injurious falls among one million elderly people who used emergency medical services from 2010 to 2017 in Beijing, China: A longitudinal observational study. BMJ Open 2019, 9, e028292. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Zhong, S.; Tu, W.; Zheng, J.; He, S.; Bao, J.; Huang, C. Assessing spatial accessibility to medical resources at the community level in Shenzhen, China. Int. J. Environ. Res. Public Health 2019, 16, 242. [Google Scholar] [CrossRef]
- Blanchard, I.E.; Doig, C.J.; Hagel, B.E.; Anton, A.R.; Zygun, D.A.; Kortbeek, J.B.; Powell, D.G.; Williamson, T.S.; Fick, G.H.; Innes, G.D. Emergency medical services response time and mortality in an urban setting. Prehospital Emerg. Care 2012, 16, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, M.S.; Bergner, L.; Hallstrom, A. Cardiac resuscitation in the community. Importance of rapid provision and implications for program planning. JAMA 1979, 241, 1905–1907. [Google Scholar] [CrossRef] [PubMed]
- Pons, P.T.; Markovchick, V.J. Eight minutes or less: Does the ambulance response time guideline impact trauma patient outcome? J. Emerg. Med. 2002, 23, 43–48. [Google Scholar] [CrossRef]
- Clarke, J.R.; Trooskin, S.Z.; Doshi, P.J.; Greenwald, L.; Mode, C.J. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. J. Trauma 2002, 52, 420–425. [Google Scholar] [CrossRef]
- Ghorbanzadeh, M.; Ozguven, E.E.; Tenney, C.S.; Leonarczyk, Z.; Jones, F.R.; Mardis, M.A. Natural disaster accessibility of small and rural libraries in Northwest Florida. Public Libr. Q. 2021, 40, 310–329. [Google Scholar] [CrossRef]
- Niedzielski, M.A.; Kucharski, R. Impact of commuting, time budgets, and activity durations on modal disparity in accessibility to supermarkets. Transp. Res. Part D Transp. Environ. 2019, 75, 106–120. [Google Scholar] [CrossRef]
- Chang, Z.; Chen, J.; Li, W.; Li, X. Public transportation and the spatial inequality of urban park accessibility: New evidence from Hong Kong. Transp. Res. Part D Transp. Environ. 2019, 76, 111–122. [Google Scholar] [CrossRef]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, F. Measures of spatial accessibility to healthcare in a GIS environment: Synthesis and a case study in Chicago Region. Environ. Plann B Plann Des. 2003, 30, 865–884. [Google Scholar] [CrossRef] [PubMed]
- Shugarman, L.R.; Campbell, D.E.; Bird, C.E.; Gabel, J.; Louis, T.A.; Lynn, J. Differences in medicare expenditures during the last 3 years of life. J. Gen. Intern. Med. 2004, 19, 127–135. [Google Scholar] [CrossRef][Green Version]
- Deng, Y.; Zhang, Y.; Pan, J. Optimization for locating emergency medical service facilities: A case study for health planning from China. Risk Manag. Healthc. Policy 2021, 14, 1791–1802. [Google Scholar] [CrossRef]
- Khan, A.A. An integrated approach to measuring potential spatial access to health care services. Socio-Econ. Plan. Sci. 1992, 26, 275–287. [Google Scholar] [CrossRef]
- Joseph, A.E.; Bantock, P.R. Measuring potential physical accessibility to general practitioners in rural areas: A method and case study. Soc. Sci. Med. 1982, 16, 85–90. [Google Scholar] [CrossRef]
- Wang, K.; Bai, J.; Dang, X. Spatial difference and equity analysis for accessibility to three-level medical services based on actual medical behavior in Shaanxi, China. Int. J. Environ. Res. Public Health 2020, 18, 112. [Google Scholar] [CrossRef]
- Ghorbanzadeh, M.; Kim, K.; Ozguven, E.E.; Horner, M.W. Spatial accessibility assessment of COVID-19 patients to healthcare facilities: A case study of Florida. Travel Behav. Soc. 2021, 24, 95–101. [Google Scholar] [CrossRef]
- Liu, S.; Qin, Y.; Xu, Y. Inequality and influencing factors of spatial accessibility of medical facilities in Rural Areas of China: A case study of Henan Province. Int. J. Environ. Res. Public Health 2019, 16, 1833. [Google Scholar] [CrossRef]
- Mirzaei, R.; Sakizadeh, M. Comparison of interpolation methods for the estimation of groundwater contamination in Andimeshk-Shush Plain, Southwest of Iran. Environ. Sci. Pollut. Res. 2016, 23, 2758–2769. [Google Scholar] [CrossRef] [PubMed]
- Ningbo Municipal Statistics Bureau Main Data Bulletin of the Seventh National Census of Ningbo. Available online: http://tjj.ningbo.gov.cn/art/2021/5/17/art_1229042825_58913572.html (accessed on 28 July 2021).
- Ningbo Jiangbei District People’s Government Bulletin of the Seventh National Census in Jiangbei District, Ningbo. Available online: http://www.nbjb.gov.cn/art/2021/5/19/art_1229105125_58930664.html (accessed on 3 August 2021).
- Ningbo Yinzhou District People’s Government Bulletin of the Seventh National Census in Yinzhou District, Ningbo. Available online: http://www.nbyz.gov.cn/art/2021/5/18/art_1229117002_3730626.html (accessed on 3 August 2021).
- Ningbo Haishu District People’s Government Bulletin of the Seventh National Census in Haishu District, Ningbo. Available online: http://www.haishu.gov.cn/art/2021/7/29/art_1229116354_3757013.html (accessed on 3 August 2021).
- National Health Commission of the People’s Republlic of China Tranfer Plan for Pneumonia Cases Infected by COVID-19 (Trial). Available online: http://www.gov.cn/zhengce/zhengceku/2020-01/29/content_5472894.htm (accessed on 7 September 2021).
- Wang, F. Measurement, optimization, and impact of health care accessibility: A methodological review. Ann. Assoc. Am. Geogr. 2012, 102, 1104–1112. [Google Scholar] [CrossRef]
- Tao, Z.; Cheng, Y.; Dai, T.; Rosenberg, M.W. Spatial optimization of residential care facility locations in Beijing, China: Maximum equity in accessibility. Int. J. Health Geogr. 2014, 13, 33. [Google Scholar] [CrossRef] [PubMed]
- Peeters, D.; Thomas, I. Distance predicting functions and applied location-allocation models. J. Geogr. Syst. 2000, 2, 167–184. [Google Scholar] [CrossRef]
- Vale, D.S.; Pereira, M. The influence of the impedance function on gravity-based pedestrian accessibility measures: A comparative analysis. Environ. Plan. B Urban Anal. City Sci. 2016, 44, 740–763. [Google Scholar] [CrossRef]
- Gribov, A.; Krivoruchko, K. Empirical bayesian kriging implementation and usage. Sci. Total. Environ. 2020, 722, 137290. [Google Scholar] [CrossRef]
- Brown, V.; Barr, A.; Scheurer, J.; Magnus, A.; Zapata-Diomedi, B.; Bentley, R. Better transport accessibility, better health: A health economic impact assessment study for Melbourne, Australia. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 89. [Google Scholar] [CrossRef]
- Yang, Y.T.; Iqbal, U.; Ko, H.L.; Wu, C.R.; Chiu, H.T.; Lin, Y.C.; Lin, W.; Hsu, Y.H.E. The relationship between accessibility of healthcare facilities and medical care utilization among the middle-aged and elderly population in Taiwan. Int. J. Qual. Health Care 2015, 27, 222–231. [Google Scholar] [CrossRef]
- CDC National Hospital Ambulatory Medical Care Survey: 2015 Emergency Department Summary Tables. Available online: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2015_ed_web_tables.pdf (accessed on 8 August 2021).
- Tacken, M.; Rosenboom, H. Mobility of elderly persons in time and space in The Netherlands: Flexible public transport for the elderly. Stud. Health Technol. Inform. 1998, 48, 195–203. [Google Scholar]
- Schnittker, J. Chronic illness and depressive symptoms in late life. Soc. Sci. Med. 2005, 60, 13–23. [Google Scholar] [CrossRef]
- Beilun District People’s Government of Ningbo Guidance on Novel Coronavirus Pneumonia Prevention and Control in Public Places. Available online: http://www.bl.gov.cn/art/2020/2/10/art_1229056774_184093.html (accessed on 7 September 2021).
- Pakdemirli, A.; Bayram, B.; Guvenc, E.; Ellidokuz, H. Evaluation of ambulance calls for patients over 65 years of age in Izmir, Turkey: A two-year retrospective analysis. Turk. J. Med. Sci. 2021, 51, 1253–1260. [Google Scholar] [CrossRef] [PubMed]
- Close, J.; Ellis, M.; Hooper, R.; Glucksman, E.; Jackson, S.; Swift, C. Prevention of falls in the elderly trial (PROFET): A randomised controlled trial. Lancet 1999, 353, 93–97. [Google Scholar] [CrossRef]
- Caplan, G.A.; Williams, A.J.; Daly, B.; Abraham, K. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department—the DEED II study. J. Am. Geriatr. Soc. 2004, 52, 1417–1423. [Google Scholar] [CrossRef]
- Valenzuela, T.D.; Criss, E.A.; Spaite, D.W.; Meislin, H.W. Evaluation of EMS management training offered during emergency medicine residency training. Ann. Emerg. Med. 1989, 18, 812–814. [Google Scholar] [CrossRef]
- Pan, J.; Liu, H.; Wang, X.; Xie, H.; Delamater, P.L. Assessing the spatial accessibility of hospital care in Sichuan Province, China. Geospat. Health 2015, 10, 384. [Google Scholar] [CrossRef] [PubMed]
- Tansley, G.; Stewart, B.; Zakariah, A.; Boateng, E.; Achena, C.; Lewis, D.; Mock, C. Population-level Spatial Access to Prehospital Care by the National Ambulance Service in Ghana. Prehospital Emerg. Care 2016, 20, 768–775. [Google Scholar] [CrossRef]
- Ningbo Municipal People’s Government the 14th Five-Year Plan for Health development in Ningbo. Available online: http://zjjcmspublic.oss-cn-hangzhou-zwynet-d01-a.internet.cloud.zj.gov.cn/jcms_files/jcms1/web2984/site/attach/0/996018484e6c4096a6a3d864851fdc22.pdf (accessed on 28 July 2021).




| Districts | Permanent Residents (n) | Aged 65 and Above (n) | Percentage of the Elderly (%) |
|---|---|---|---|
| Haishu District | 1,041,285 | 131,201 | 12.60 |
| Jiangbei District | 488,885 | 57,383 | 11.74 |
| Yinzhou District | 1,609,555 | 178,762 | 11.11 |
| Study area | 3,139,725 | 367,346 | 11.70 |
| Characteristics | All Patients (n = 10,062) |
|---|---|
| Sex (%) | |
| Male | 5399 (53.66) |
| Female | 4663 (46.34) |
| Age (%) | |
| 65–74 | 3724 (37.01) |
| 75–84 | 3187 (31.67) |
| 85–94 | 2851 (28.33) |
| 95–104 | 297 (2.96) |
| 105 and above | 3 (0.03) |
| Mean age | 78.79 |
| Disease Diagnosis | n | % |
|---|---|---|
| Trauma and intoxication | 2385 | 23.70 |
| Unclassified diseases | 1969 | 19.57 |
| Neurologic diseases | 1499 | 14.90 |
| Cardiovascular diseases | 1119 | 11.12 |
| Respiratory diseases | 1029 | 10.23 |
| Gastrointestinal diseases | 852 | 8.47 |
| Muscle, skeletal and connective tissue diseases | 341 | 3.39 |
| Others | 263 | 2.61 |
| Urogenital diseases | 217 | 2.16 |
| Tumor and blood-related diseases | 154 | 1.53 |
| Endocrine nutritional metabolic diseases | 135 | 1.34 |
| Skin and subcutaneous tissue diseases | 41 | 0.41 |
| ENT diseases | 35 | 0.35 |
| Psychiatric illness | 15 | 0.15 |
| Infectious and parasitic disease | 8 | 0.08 |
| Districts | Permanent Residents | Aged 65 and Above | Ambulance Utilization by the Elderly | Number of Ambulances Utilization per 1000 Elderly Residents |
|---|---|---|---|---|
| Haishu District | 1,041,285 | 131,201 | 3960 | 10.78 |
| Jiangbei District | 488,885 | 57,383 | 1856 | 5.05 |
| Yinzhou District | 1,609,555 | 178,762 | 4246 | 11.56 |
| Study area | 3,139,725 | 367,346 | 10,062 | 27.39 |
| Accessibility Score | 0~1 | 1~10 | 10~20 | 20 and Over |
|---|---|---|---|---|
| Number of demand points | 538 | 239 | 12 | 4 |
| Proportion (%) | 67.84 | 30.14 | 1.51 | 0.51 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, H.; Pan, L.; Li, Y.; Jin, H.; Wang, Q.; Liu, X.; Wang, C.; Liao, P.; Jiang, X.; Li, L. Spatial Accessibility Assessment of Prehospital EMS with a Focus on the Elderly Population: A Case Study in Ningbo, China. Int. J. Environ. Res. Public Health 2021, 18, 9964. https://doi.org/10.3390/ijerph18199964
Zhu H, Pan L, Li Y, Jin H, Wang Q, Liu X, Wang C, Liao P, Jiang X, Li L. Spatial Accessibility Assessment of Prehospital EMS with a Focus on the Elderly Population: A Case Study in Ningbo, China. International Journal of Environmental Research and Public Health. 2021; 18(19):9964. https://doi.org/10.3390/ijerph18199964
Chicago/Turabian StyleZhu, Huanhuan, Lin Pan, Yiji Li, Huiming Jin, Qian Wang, Xin Liu, Cong Wang, Peng Liao, Xinyang Jiang, and Luo Li. 2021. "Spatial Accessibility Assessment of Prehospital EMS with a Focus on the Elderly Population: A Case Study in Ningbo, China" International Journal of Environmental Research and Public Health 18, no. 19: 9964. https://doi.org/10.3390/ijerph18199964
APA StyleZhu, H., Pan, L., Li, Y., Jin, H., Wang, Q., Liu, X., Wang, C., Liao, P., Jiang, X., & Li, L. (2021). Spatial Accessibility Assessment of Prehospital EMS with a Focus on the Elderly Population: A Case Study in Ningbo, China. International Journal of Environmental Research and Public Health, 18(19), 9964. https://doi.org/10.3390/ijerph18199964






