The Combination of Modified Mitchell’s Osteotomy and Shortening Oblique Osteotomy for Patients with Rheumatoid Arthritis: An Analysis of Changes in Plantar Pressure Distribution
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Surgical Procedures
2.3. Patient Background Parameters
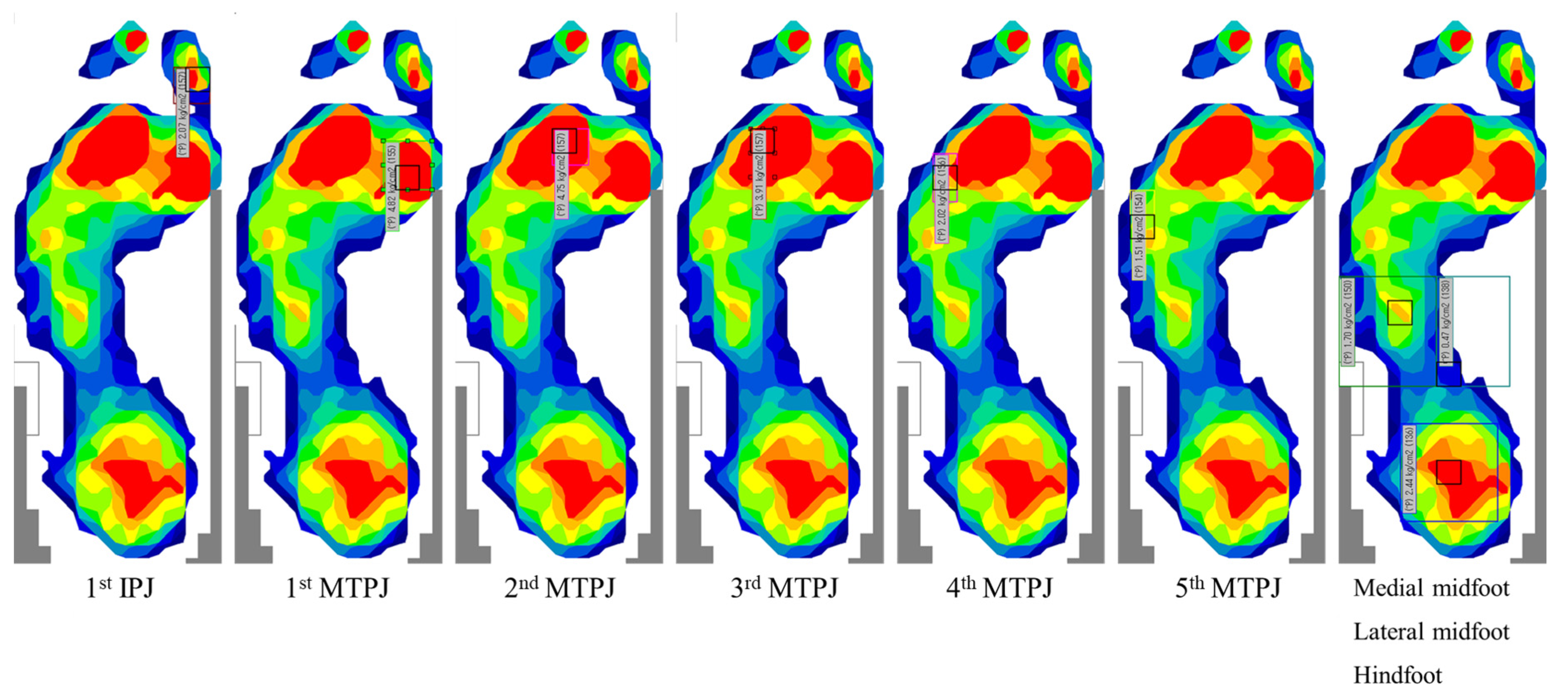
2.4. Plantar Pressure Measurement
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vainio, K. The rheumatoid foot; a clinical study with pathological and roentgenological comments. Ann. Chir. Gynaecol. Fenn. Suppl. 1956, 45, 1–107. [Google Scholar] [PubMed]
- Thould, A.K.; Simon, G. Assessment of radiological changes in the hands and feet in rheumatoid arthritis. Their correlation with prognosis. Ann. Rheum. Dis. 1966, 25, 220–228. [Google Scholar] [CrossRef] [Green Version]
- Sell, S.; Rehart, S.; Henniger, M.; Kurosch, B. The foot. In Surgery for Rheumatic Diseases; Sell, S., Rehart, S., Eds.; Thieme: Stuttgart, Germany, 2017; pp. 75–98. [Google Scholar]
- Williams, A.E.; Davies, S.; Graham, A.; Dagg, A.; Longrigg, K.; Lyons, C.; Bowen, C.; North West Clinical Effectiveness Group for the Foot in Rheumatic, D. Guidelines for the management of the foot health problems associated with rheumatoid arthritis. Musculoskeletal Care 2011, 9, 86–92. [Google Scholar] [CrossRef]
- Tenten-Diepenmaat, M.; Dekker, J.; Steenbergen, M.; Huybrechts, E.; Roorda, L.D.; van Schaardenburg, D.; Bus, S.A.; van der Leeden, M. In-shoe plantar pressure measurements for the evaluation and adaptation of foot orthoses in patients with rheumatoid arthritis: A proof of concept study. Gait Posture 2016, 45, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Siddle, H.J.; Redmond, A.C.; Waxman, R.; Dagg, A.R.; Alcacer-Pitarch, B.; Wilkins, R.A.; Helliwell, P.S. Debridement of painful forefoot plantar callosities in rheumatoid arthritis: The CARROT randomised controlled trial. Clin. Rheumatol. 2013, 32, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Helal, B.; Greiss, M. Telescoping osteotomy for pressure metatarsalgia. J. Bone Joint Surg. Br. 1984, 66, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Niki, H.; Hirano, T.; Okada, H.; Beppu, M. Combination joint-preserving surgery for forefoot deformity in patients with rheumatoid arthritis. J. Bone Joint Surg. Br. 2010, 92, 380–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanyu, T.; Yamazaki, H.; Ishikawa, H.; Arai, K.; Tohyama, C.T.; Nakazono, K.; Murasawa, A. Flexible hinge toe implant arthroplasty for rheumatoid arthritis of the first metatarsophalangeal joint: Long-term results. J. Orthop. Sci. 2001, 6, 141–147. [Google Scholar] [CrossRef]
- Shimoda, H.; Mochida, Y.; Oritsu, H.; Shimizu, Y.; Takahashi, Y.; Wakabayashi, H.; Watanabe, N. Effects of forefoot arthroplasty on plantar pressure, pain, gait and disability in rheumatoid arthritis. Mod. Rheumatol. 2020, 30, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Ishikawa, H.; Miyagawa, Y.; Takai, C.; Nomura, Y.; Nemoto, T.; Kobayashi, D.; Abe, A.; Otani, H.; Ito, S.; et al. Plantar pressure and surgical indication of toe arthroplasty for rheumatoid forefoot deformity. Mod. Rheumatol. 2017, 27, 990–994. [Google Scholar] [CrossRef]
- Konings-Pijnappels, A.P.M.; Tenten-Diepenmaat, M.; Dahmen, R.; Verberne, S.K.; Dekker, J.; Twisk, J.W.R.; Roorda, L.D.; van der Leeden, M. Forefoot pathology in relation to plantar pressure distribution in patients with rheumatoid arthritis: A cross-sectional study in the Amsterdam Foot cohort. Gait Posture 2019, 68, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Dhanendran, M.; Hutton, W.C.; Corbett, M. Changes in load bearing in the rheumatoid foot. Ann. Rheum. Dis. 1979, 38, 549–552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stewart, S.; Carroll, M.; Brenton-Rule, A.; Keys, M.; Bell, L.; Dalbeth, N.; Rome, K. Region-specific foot pain and plantar pressure in people with rheumatoid arthritis: A cross-sectional study. Clin. Biomech. (Bristol. Avon) 2018, 55, 14–17. [Google Scholar] [CrossRef]
- Betts, R.P.; Stockley, I.; Getty, C.J.; Rowley, D.I.; Duckworth, T.; Franks, C.I. Foot pressure studies in the assessment of forefoot arthroplasty in the rheumatoid foot. Foot Ankle 1988, 8, 315–326. [Google Scholar] [CrossRef] [PubMed]
- Ebina, K.; Hirao, M.; Takagi, K.; Ueno, S.; Morimoto, T.; Matsuoka, H.; Kitaguchi, K.; Iwahashi, T.; Hashimoto, J.; Yoshikawa, H. Comparison of the effects of forefoot joint-preserving arthroplasty and resection-replacement arthroplasty on walking plantar pressure distribution and patient-based outcomes in patients with rheumatoid arthritis. PLoS ONE 2017, 12, e0183805. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.; Ishikawa, H.; Shibuya, T.; Takai, C.; Nomura, Y.; Kobayashi, D.; Abe, A.; Otani, H.; Ito, S.; Nakazono, K.; et al. Changes in radiographic findings and plantar pressure distribution following forefoot reconstructive surgery for patients with rheumatoid arthritis. Mod. Rheumatol. 2020, 30, 967–974. [Google Scholar] [CrossRef]
- Yano, K.; Saito, H.; Ikari, K.; Okazaki, K. Impact of joint-preserving surgery on plantar pressure among patients with rheumatoid arthritis. Mod. Rheumatol. 2020, 30, 604–606. [Google Scholar] [CrossRef]
- Horita, M.; Nishida, K.; Hashizume, K.; Nasu, Y.; Saiga, K.; Nakahara, R.; Machida, T.; Ohashi, H.; Ozaki, T. Outcomes of Resection and Joint-Preserving Arthroplasty for Forefoot Deformities for Rheumatoid Arthritis. Foot Ankle Int. 2018, 39, 292–299. [Google Scholar] [CrossRef]
- Hanyu, T.; Yamazaki, H.; Murasawa, A.; Tohyama, C. Arthroplasty for rheumatoid forefoot deformities by a shortening oblique osteotomy. Clin. Orthop. Relat. Res. 1997, 131–138. [Google Scholar] [CrossRef]
- Mitchell, C.L.; Fleming, J.L.; Allen, R.; Glenney, C.; Sanford, G.A. Osteotomy-bunionectomy for hallux valgus. J. Bone Joint Surg. Am. 1958, 40, 41–58, discussion 59–60. [Google Scholar] [CrossRef]
- Yamamoto, K.; Imakiire, A.; Katori, Y.; Masaoka, T.; Koizumi, R. Clinical results of modified Mitchell’s osteotomy for hallux valgus augmented with oblique lesser metatarsal osteotomy. J. Orthop. Surg. 2005, 13, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Dhukaram, V.; Hullin, M.G.; Senthil Kumar, C. The Mitchell and Scarf osteotomies for hallux valgus correction: A retrospective, comparative analysis using plantar pressures. J. Foot Ankle Surg. 2006, 45, 400–409. [Google Scholar] [CrossRef] [PubMed]
- Kojima, T.; Ishikawa, H.; Tanaka, S.; Haga, N.; Nishida, K.; Yukioka, M.; Hashimoto, J.; Miyahara, H.; Niki, Y.; Kimura, T.; et al. Relationship between the physician-based clinical scale for foot and ankle surgery and patient-reported outcomes in patients with long-standing rheumatoid arthritis: Results from a multicenter prospective observational cohort study. Mod. Rheumatol. 2021, 31, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Abe, A.; Kojima, T.; Kojima, M.; Ishiguro, N.; Nomura, Y.; Otani, H.; Hasegawa, E.; Kobayashi, D.; Ito, S.; et al. Overall benefits provided by orthopedic surgical intervention in patients with rheumatoid arthritis. Mod. Rheumatol. 2019, 29, 335–343. [Google Scholar] [CrossRef]
- Niki, H.; Aoki, H.; Inokuchi, S.; Ozeki, S.; Kinoshita, M.; Kura, H.; Tanaka, Y.; Noguchi, M.; Nomura, S.; Hatori, M.; et al. Development and reliability of a standard rating system for outcome measurement of foot and ankle disorders I: Development of standard rating system. J. Orthop. Sci. 2005, 10, 457–465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niki, H.; Aoki, H.; Inokuchi, S.; Ozeki, S.; Kinoshita, M.; Kura, H.; Tanaka, Y.; Noguchi, M.; Nomura, S.; Hatori, M.; et al. Development and reliability of a standard rating system for outcome measurement of foot and ankle disorders II: Interclinician and intraclinician reliability and validity of the newly established standard rating scales and Japanese Orthopaedic Association rating scale. J. Orthop. Sci. 2005, 10, 466–474. [Google Scholar] [CrossRef] [Green Version]
- Bryant, A.; Singer, K.; Tinley, P. Comparison of the reliability of plantar pressure measurements using the two-step and midgait methods of data collection. Foot Ankle Int. 1999, 20, 646–650. [Google Scholar] [CrossRef]
- Putti, A.B.; Arnold, G.P.; Cochrane, L.A.; Abboud, R.J. Normal pressure values and repeatability of the Emed ST4 system. Gait Posture 2008, 27, 501–505. [Google Scholar] [CrossRef]
- Kuo, C.H.; Huang, P.J.; Cheng, Y.M.; Huang, K.Y.; Chen, T.B.; Chen, Y.W.; Lin, S.Y. Modified Mitchell osteotomy for hallux valgus. Foot Ankle Int. 1998, 19, 585–589. [Google Scholar] [CrossRef]
- Kennedy, J.G.; Deland, J.T. Resolution of metatarsalgia following oblique osteotomy. Clin. Orthop. Relat. Res. 2006, 453, 309–313. [Google Scholar] [CrossRef]
- Chen, S.J.; Cheng, Y.M.; Lin, S.Y.; Chen, C.H.; Huang, H.T.; Huang, P.J. Modified Mitchell osteotomy alone does not have higher rate of residual metatarsalgia than combined first and lesser metatarsal osteotomy. Kaohsiung J. Med. Sci. 2015, 31, 203–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merkel, K.D.; Katoh, Y.; Johnson, E.W., Jr.; Chao, E.Y. Mitchell osteotomy for hallux valgus: Long-term follow-up and gait analysis. Foot Ankle 1983, 3, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Brenton-Rule, A.; Dalbeth, N.; Menz, H.B.; Bassett, S.; Rome, K. Foot and ankle characteristics associated with falls in adults with established rheumatoid arthritis: A cross-sectional study. BMC Musculoskelet Disord. 2016, 17, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamanaka, H.; Seto, Y.; Tanaka, E.; Furuya, T.; Nakajima, A.; Ikari, K.; Taniguchi, A.; Momohara, S. Management of rheumatoid arthritis: The 2012 perspective. Mod. Rheumatol. 2013, 23, 1–7. [Google Scholar] [CrossRef]
- Bryant, A.R.; Tinley, P.; Cole, J.H. Plantar pressure and radiographic changes to the forefoot after the Austin bunionectomy. J. Am. Podiatr. Med. Assoc. 2005, 95, 357–365. [Google Scholar] [CrossRef]

| Number of patients | 23 |
| Number of female (%) | 21 (91.3) |
| Number of feet | 26 |
| Age, years | 60.0 (48.0–70.0) |
| Disease duration of RA, years | 11.0 (7.0–15.0) |
| Body mass index, kg/m2 | 21.5 (19.9–23.3) |
| Larsen grade for the first MTPJ (number) | II:16, III:10 |
| Preoperatively | One Year Potoperatively | |
|---|---|---|
| Methotrexate usage, number (%) | 17 (73.9) | 19 (82.6) |
| Biologics usage, number (%) | 9 (39.1) | 11 (47.8) |
| Prednisolone usage, number (%) | 13 (56.5) | 15 (65.2) |
| Pain visual analog scale, mm | 31.0 (10.0–50.3) | 20.0 (6.5–40.0) * |
| General visual analog scale, mm | 38.0 (19.0–60.3) | 26.0 (8.0–46.5) * |
| DAS28-ESR | 2.6 (2.2–3.4) | 2.7 (2.0–3.5) |
| SDAI | 9.2 (5.8–12.0) | 7.6 (2.5–10.0) |
| J-HAQ | 0.4 (0–0.6) | 0.4 (0–0.8) |
| JSSF RA scale | ||
| General pain, 0–30 points | 20.0 (20.0–30.0) | 30.0 (30.0–30.0) ** |
| Deformity, 0–25 points | 12.0 (10.0–17.5) | 21.5 (16.5–24.5) *** |
| Motion, 0–15 points | 13.0 (13.0–15.0) | 13.0 (13.0–13.0) |
| Walking ability, 0–20 points | 20.0 (20.0–20.0) | 20.0 (20.0–20.0) |
| Activities of daily living, 0–10 points | 5.0 (3.0–7.0) | 6.0 (4.0–7.0) |
| Total, 0–100 points | 70.0 (67.0–80.5) | 88.5 (85.0–91.0) *** |
| HVA, degree | 32.5 (27.3–42.1) | 15.8 (12.2–19.5) *** |
| M1/2, degree | 13.6 (11.6–15.9) | 9.7 (8.1–11.8) *** |
| M1/5, degree | 35.8 (33.3–39.5) | 25.7 (21.8–27.8) *** |
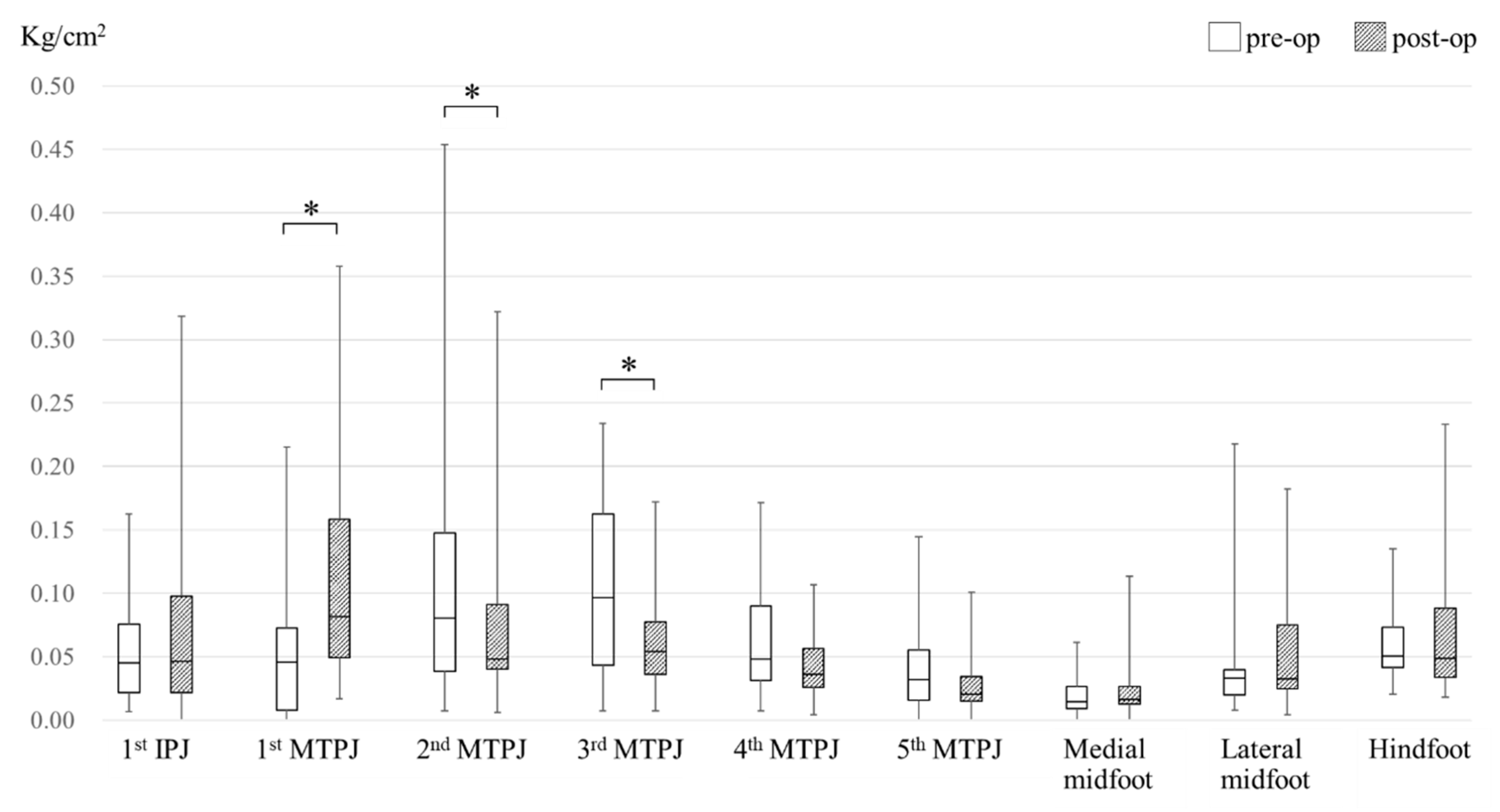
| (a). Maximum Peak Pressure | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| First IPJ | First MTPJ | Second MTPJ | Third MTPJ | Fourth MTPJ | Fifth MTPJ | Medial Midfoot | Lateral Midfoot | Hind-foot | ||
| Pre-op (n = 26) | % (n) | 7.7 (2) | 23.1 (6) | 19.2 (5) | 23.1 (6) | 3.8 (1) | 3.8 (1) | 0 (0) | 0 (0) | 19.2 (5) |
| Post-op (n = 26) | % (n) | 23.1 (6) | 34.6 (9) | 11.5 (3) | 11.5 (3) | 3.8 (1) | 0 (0) | 0 (0) | 7.7 (2) | 7.7 (2) |
| (b). Minimum Peak Pressure | ||||||||||
| First IPJ | First MTPJ | Second MTPJ | Third MTPJ | Fourth MTPJ | Fifth MTPJ | Medial Midfoot | Lateral Midfoot | Hind-foot | ||
| Pre-op (n = 26) | % (n) | 3.8 (1) | 30.8 (8) | 0 (0) | 0 (0) | 0 (0) | 30.8 (8) | 26.9 (7) | 7.7 (2) | 0 (0) |
| Post-op (n = 26) | % (n) | 11.5 (3) | 0 (0) | 0 (0) | 3.8 (1) | 0 (0) | 30.8 (8) | 46.2 (12) | 7.7 (2) | 0 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.; Ishikawa, H.; Shibuya, T.; Takai, C.; Nemoto, T.; Nomura, Y.; Abe, A.; Otani, H.; Ito, S.; Nakazono, K.; et al. The Combination of Modified Mitchell’s Osteotomy and Shortening Oblique Osteotomy for Patients with Rheumatoid Arthritis: An Analysis of Changes in Plantar Pressure Distribution. Int. J. Environ. Res. Public Health 2021, 18, 9948. https://doi.org/10.3390/ijerph18199948
Lee H, Ishikawa H, Shibuya T, Takai C, Nemoto T, Nomura Y, Abe A, Otani H, Ito S, Nakazono K, et al. The Combination of Modified Mitchell’s Osteotomy and Shortening Oblique Osteotomy for Patients with Rheumatoid Arthritis: An Analysis of Changes in Plantar Pressure Distribution. International Journal of Environmental Research and Public Health. 2021; 18(19):9948. https://doi.org/10.3390/ijerph18199948
Chicago/Turabian StyleLee, Hyunho, Hajime Ishikawa, Tatsuaki Shibuya, Chinatsu Takai, Tetsuya Nemoto, Yumi Nomura, Asami Abe, Hiroshi Otani, Satoshi Ito, Kiyoshi Nakazono, and et al. 2021. "The Combination of Modified Mitchell’s Osteotomy and Shortening Oblique Osteotomy for Patients with Rheumatoid Arthritis: An Analysis of Changes in Plantar Pressure Distribution" International Journal of Environmental Research and Public Health 18, no. 19: 9948. https://doi.org/10.3390/ijerph18199948






