Foot Position Measurement during Assistive Motion for Sit-to-Stand Using a Single Inertial Sensor and Shoe-Type Force Sensors
Abstract
1. Introduction
1.1. Lower Back Pain due to Assistive Motion for Sit-to-Stand
1.2. Related Works to Prevent LBP due to Assistive Motion for Sit-to-Stand
1.3. Related Studies for Foot Position Measurement
1.4. Potential of Inertial Sensor and Shoe-Type Force Sensors
1.5. Potential of Machine Learning-Based Regression
1.6. Objective of This Paper
1.7. Contribution of This Paper
2. Materials and Methods
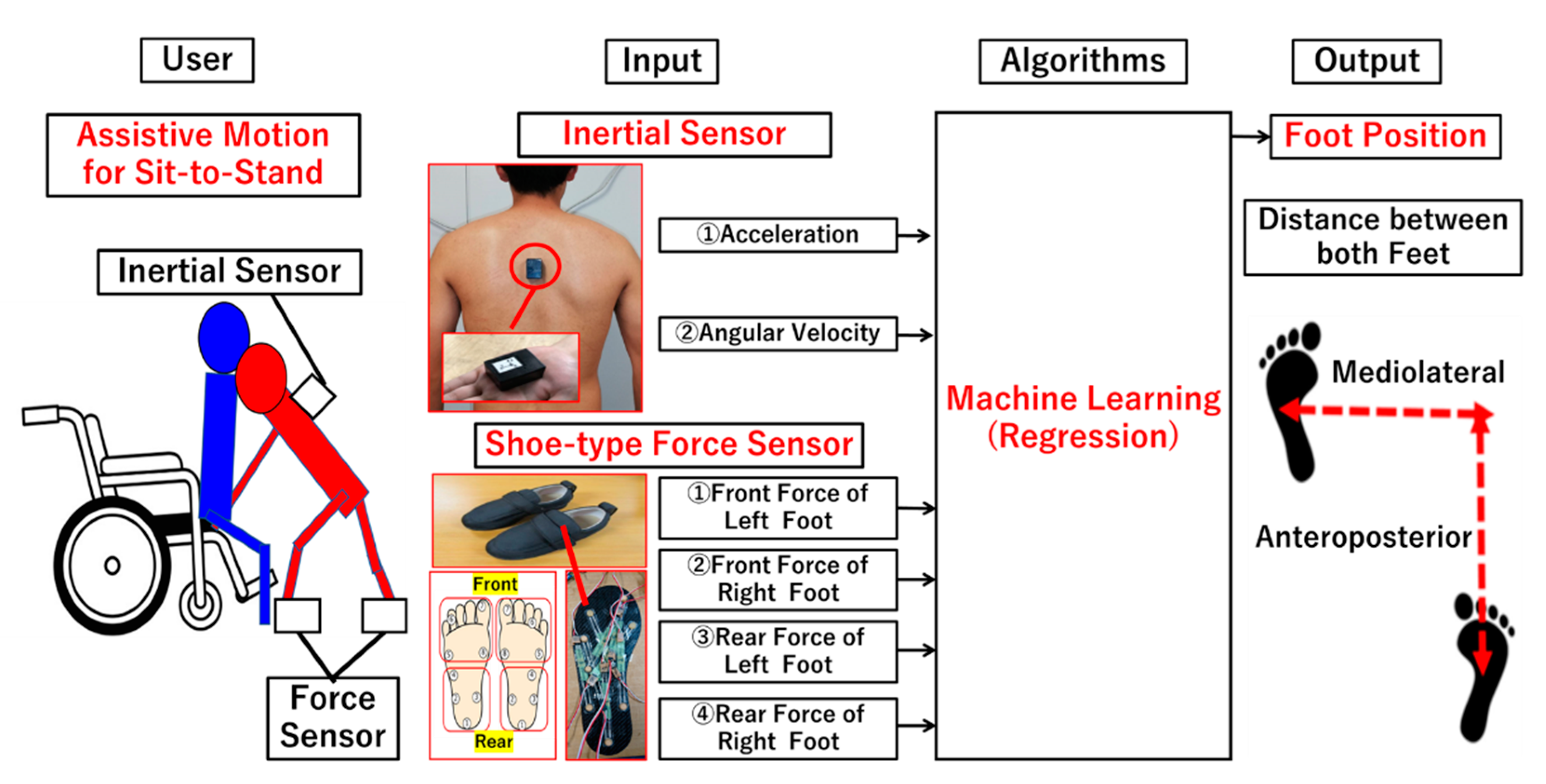
2.1. Proposed Method for Foot Position Measurement
2.1.1. Architecture
2.1.2. Wearable Sensors
2.1.3. Machine Learning-Based Regression Algorithm
2.1.4. Foot Position
2.1.5. Expected Intervention
2.2. Experiment for Evaluation of the Proposed Method
2.2.1. Participants
2.2.2. Experimental Procedure
2.2.3. Data Analysis
3. Results
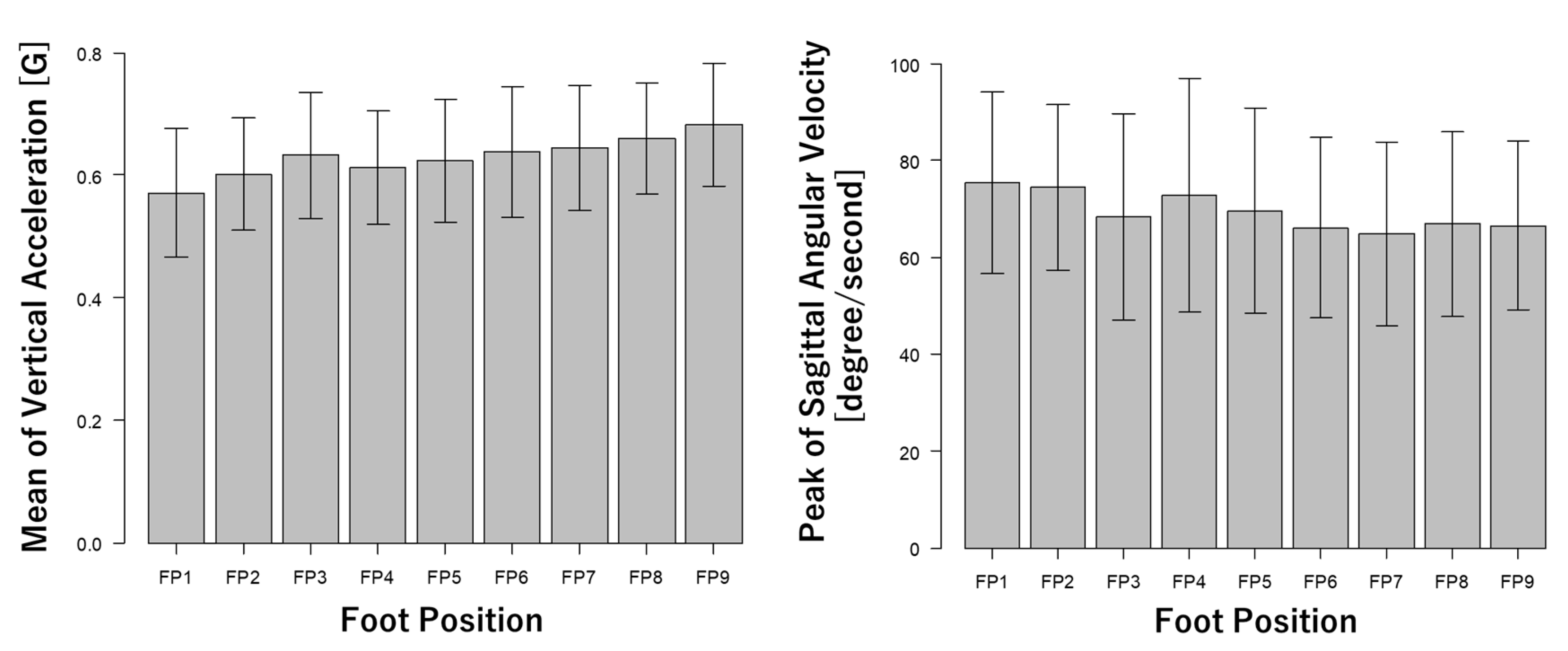
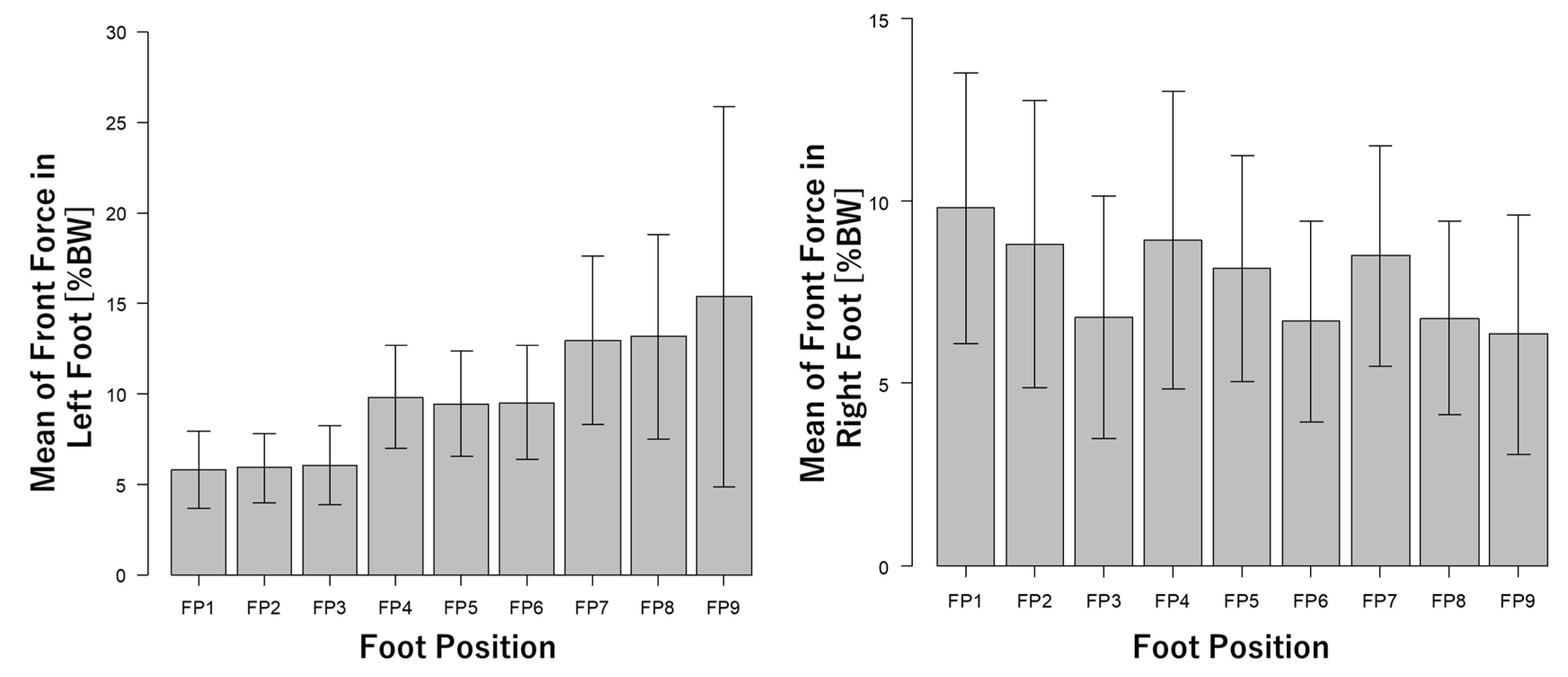
3.1. Data Specification
3.2. RMSE Values
3.3. Statistical Results
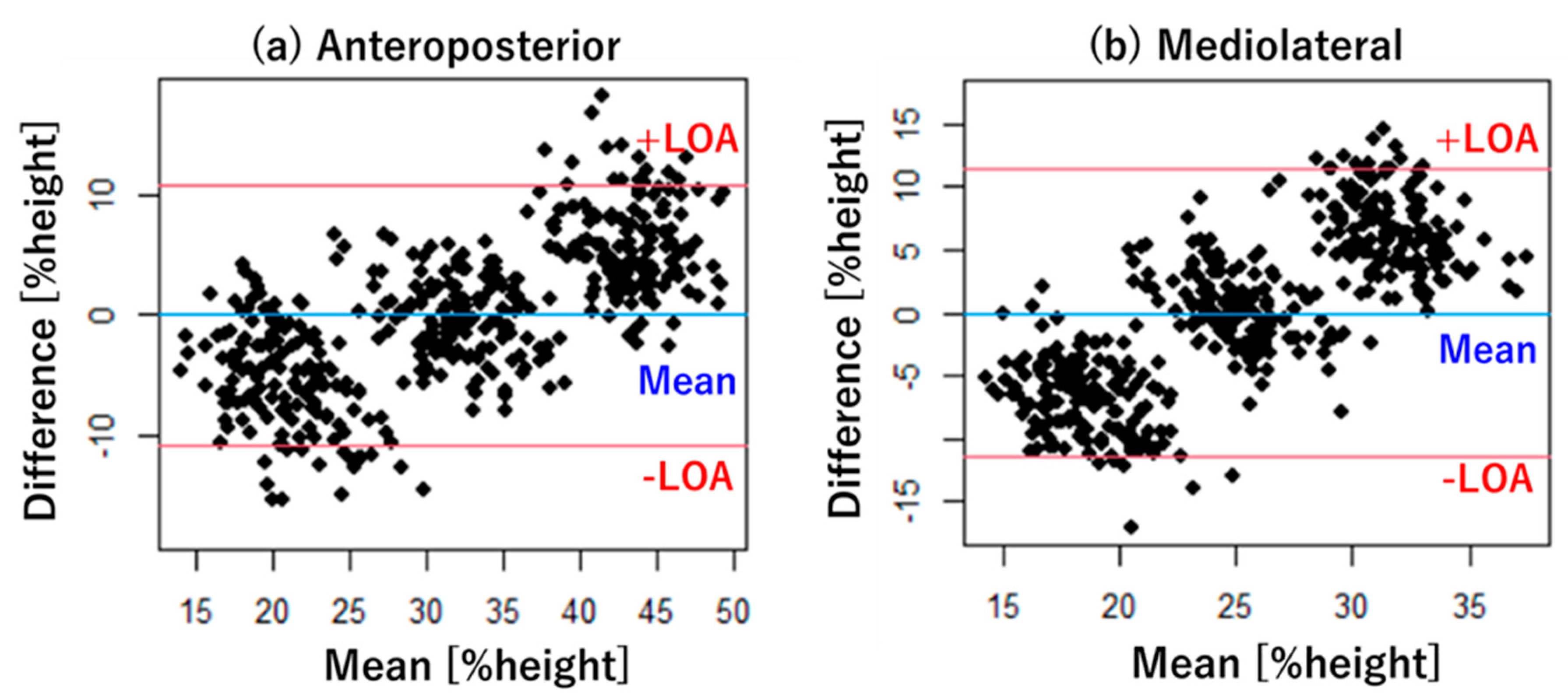
3.4. Bland–Altman Plot
4. Discussion
4.1. Validity of the Proposed Method
4.2. Wearable Sensors
4.3. Machine Learning Algorithms
4.4. Limitation and Future Works
5. Conclusions
- The proposed method can measure quantitative foot positions using a single inertial sensor, shoe-type force sensors, and a machine learning algorithm.
- The proposed method was evaluated using RMSE values, statistical analysis, and Bland–Altman plots.
- Optimal combinations of wearable sensors and machine learning algorithm were explored for the proposed method.
- The experimental results showed that a combination of both inertial and shoe-type force sensors and Gaussian process is the optimal combination for the proposed method.
- The RMSE values and statistical results indicated that the proposed method could measure foot position during assistive motion for sit-to-stand.
- Bland–Altman plots showed that the proportional error should be improved in the proposed method.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smedley, J.; Egger, P.; Cooper, C.; Coggon, D. Manual handling activities and risk of low back pain in nurses. Occup. Environ. Med. 1995, 52, 160–163. [Google Scholar] [CrossRef]
- Kitagawa, K.; Nagasaki, T.; Nakano, S.; Hida, M.; Okamatsu, S.; Wada, C. Analysis of Occupational Injury Reports Related to Patient Care Activities Using Text Mining Technique. In Proceedings of the 11th Asian-Pacific Conference on Medical and Biological Engineering: Online Conference APCMBE 2020; Springer Nature: London, UK, 2021; Volume 82, pp. 153–158. [Google Scholar]
- Robielos, R.A.C.; Sambua, K.C.A.; Fernandez, J.G. Ergonomic intervention for healthcare workers and patients: A development of patient handling device. In Proceedings of the Congress of the International Ergonomics Association, Florence, Italy, 26–30 August 2018; Springer: Berlin/Heidelberg, Germany, 2018; pp. 615–638. [Google Scholar]
- Aljohani, W.A.; Pascua, G.P. Impacts of Manual Handling Training and Lifting Devices on Risks of Back Pain among Nurses: An Integrative Literature Review. Nurse Media J. Nurs. 2019, 9, 210–230. [Google Scholar] [CrossRef]
- Hoogendoorn, W.E.; Bongers, P.M.; De Vet, H.C.; Douwes, M.; Koes, B.W.; Miedema, M.C.; Ariëns, G.A.; Bouter, L.M. Flexion and rotation of the trunk and lifting at work are risk factors for low back pain: Results of a prospective cohort study. Spine 2000, 25, 3087–3092. [Google Scholar] [CrossRef]
- Delise, A.; Gagnon, M.; Desjardins, P. Load acceleration and footstep strategies in asymmetrical lifting and lowering. Int. J. Occup. Saf. Ergon. 1996, 2, 185–195. [Google Scholar] [CrossRef][Green Version]
- Delisle, A.; Gagnon, M.; Desjardins, P. Kinematic analysis of footstep strategies in asymmetrical lifting and lowering tasks. Int. J. Ind. Ergon. 1999, 23, 451–460. [Google Scholar] [CrossRef]
- Kitagawa, K.; Nagasaki, T.; Nakano, S.; Hida, M.; Okamatsu, S.; Wada, C. Optimal foot-position of caregiver based on muscle activity of lower back and lower limb while providing sit-to-stand support. J. Phys. Ther. Sci. 2020, 32, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, K.; Nishisako, Y.; Nagasaki, T.; Nakano, S.; Wada, C. Musculoskeletal simulation of the relationship between foot position and stress of the L4–L5 joint in supporting standing-up motion to prevent low back pain among caregivers. J. Mech. Med. Biol. 2019, 19, 1940016. [Google Scholar] [CrossRef]
- Owlia, M.; Ng, C.; Ledda, K.; Kamachi, M.; Longfield, A.; Dutta, T. Preventing back injury in caregivers using real-time posture-based feedback. In Proceedings of the Congress of the International Ergonomics Association, Florence, Italy, 26–30 August 2018; Springer: Berlin/Heidelberg, Germany, 2018; pp. 750–758. [Google Scholar]
- Owlia, M.; Kamachi, M.; Dutta, T. Reducing lumbar spine flexion using real-time biofeedback during patient handling tasks. Work 2020, 66, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Cerqueira, S.M.; Da Silva, A.F.; Santos, C.P. Smart Vest for Real-Time Postural Biofeedback and Ergonomic Risk Assessment. IEEE Access 2020, 8, 107583–107592. [Google Scholar] [CrossRef]
- Doss, R.; Robathan, J.; Abdel-Malek, D.; Holmes, M.W. Posture coaching and feedback during patient handling in a student nurse population. IISE Trans. Occup. Ergon. Hum. Factors 2018, 6, 116–127. [Google Scholar] [CrossRef]
- Wagner, D.W.; Reed, M.P.; Chaffin, D.B. Predicting foot positions for manual materials handling tasks. SAE Trans. 2005, 114, 2872–2876. [Google Scholar]
- Muller, A.; Vallée-Marcotte, J.; Robert-Lachaine, X.; Mecheri, H.; Larue, C.; Corbeil, P.; Plamondon, A. A machine-learning method for classifying and analyzing foot placement: Application to manual material handling. J. Biomech. 2019, 97, 109410. [Google Scholar] [CrossRef]
- Marcotte, J.V.; Muller, A.; Robert-Lachaine, X.; Fecteau, V.; Denis, D.; Plamondon, A.; Corbeil, P. New taxonomy for assessing manual material handlers’ footstep patterns. Appl. Ergon. 2021, 94, 103424. [Google Scholar] [CrossRef]
- Panebianco, G.P.; Bisi, M.C.; Stagni, R.; Fantozzi, S. Analysis of the performance of 17 algorithms from a systematic review: Influence of sensor position, analysed variable and computational approach in gait timing estimation from IMU measurements. Gait Posture 2018, 66, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Widodo, R.B.; Wada, C. Artificial neural network based step-length prediction using ultrasonic sensors from simulation to implementation in shoe-type measurement device. J. Adv. Comput. Intell. Intell. Inform. 2017, 21, 321–329. [Google Scholar] [CrossRef]
- Kitagawa, K.; Matsumoto, K.; Iwanaga, K.; Ahmad, S.A.; Nagasaki, T.; Nakano, S.; Hida, M.; Okamatsu, S.; Wada, C. Posture Recognition Method for Caregivers during Postural Change of a Patient on a Bedusing Wearable Sensors. Adv. Sci. Technol. Eng. Syst. J. 2020, 5, 1093–1098. [Google Scholar] [CrossRef]
- Wagner, D.W.; Reed, M.P.; Chaffin, D.B. The development of a model to predict the effects of worker and task factors on foot placements in manual material handling tasks. Ergonomics 2010, 53, 1368–1384. [Google Scholar] [CrossRef]
- Kingma, I.; Faber, G.S.; Van Dieën, J.H. How to lift a box that is too large to fit between the knees. Ergonomics 2010, 53, 1228–1238. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.; Yamada, K.; Kido, M.; Okada, S.; Nomura, T.; Ohno, Y. Analysis of difference in center-of-pressure positions between experts and novices during asymmetric lifting. IEEE J. Transl. Eng. Health Med. 2016, 4, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-J.; Aruin, A.S. Effects of asymmetrical stance and movement on body rotation in pushing. J. Biomech. 2015, 48, 283–289. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Antwi-Afari, M.F.; Li, H. Fall risk assessment of construction workers based on biomechanical gait stability parameters using wearable insole pressure system. Adv. Eng. Inform. 2018, 38, 683–694. [Google Scholar] [CrossRef]
- Antwi-Afari, M.F.; Li, H.; Yu, Y.; Kong, L. Wearable insole pressure system for automated detection and classification of awkward working postures in construction workers. Autom. Constr. 2018, 96, 433–441. [Google Scholar] [CrossRef]
- Matijevich, E.S.; Volgyesi, P.; Zelik, K.E. A Promising Wearable Solution for the Practical and Accurate Monitoring of Low Back Loading in Manual Material Handling. Sensors 2021, 21, 340. [Google Scholar] [CrossRef]
- Kitagawa, K.; Nishisako, Y.; Nagasaki, T.; Nakano, S.; Hida, M.; Okamatsu, S.; Wada, C. Regression Equation between Required Force and Lumbar Load of Caregiver in Supporting Standing-up Motion via Computational Musculoskeletal Simulation. Pertanika J. Sci. Technol. 2020, 28, 59–70. [Google Scholar] [CrossRef]
- Gurchiek, R.D.; Cheney, N.; McGinnis, R.S. Estimating biomechanical time-series with wearable sensors: A systematic review of machine learning techniques. Sensors 2019, 19, 5227. [Google Scholar] [CrossRef]
- Choffin, Z.; Jeong, N.; Callihan, M.; Olmstead, S.; Sazonov, E.; Thakral, S.; Getchell, C.; Lombardi, V. Ankle Angle Prediction Using a Footwear Pressure Sensor and a Machine Learning Technique. Sensors 2021, 21, 3790. [Google Scholar] [CrossRef] [PubMed]
- Almassri, A.M.; Wan Hasan, W.Z.; Ahmad, S.A.; Ishak, A.J.; Ghazali, A.M.; Talib, D.N.; Wada, C. Pressure sensor: State of the art, design, and application for robotic hand. J. Sens. 2015, 2015, 846487. [Google Scholar] [CrossRef]
- Almassri, A.M.; Hasan, W.Z.W.; Wada, C.; Horio, K. Evaluation of a commercial force sensor for real time applications. ICIC Express Lett. Part. B Appl. Int. J. Res. Surv. 2020, 11, 421–426. [Google Scholar]
- Setiawan, J.D.; Ariyanto, M.; Munadi, M.; Mutoha, M.; Glowacz, A.; Caesarendra, W. Grasp posture control of wearable extra robotic fingers with flex sensors based on neural network. Electronics 2020, 9, 905. [Google Scholar] [CrossRef]
- Monoli, C.; Fuentez-Pérez, J.F.; Cau, N.; Capodaglio, P.; Galli, M.; Tuhtan, J.A. Land and Underwater Gait Analysis Using Wearable IMU. IEEE Sens. J. 2021, 21, 11192–11202. [Google Scholar] [CrossRef]
- Shi, W.; Wang, W.; Hou, Z.-G.; Liang, X.; Wang, J.; Ren, S.; Peng, L. SEMG and KNN Based Human Motion Intention Recognition for Active and Safe Neurorehabilitation. Aust. J. Intell. Inf. Process Syst. 2019, 15, 43–52. [Google Scholar]
- Hester, T.; Hughes, R.; Sherrill, D.M.; Knorr, B.; Akay, M.; Stein, J.; Bonato, P. Using wearable sensors to measure motor abilities following stroke. In Proceedings of the International Workshop on Wearable and Implantable Body Sensor Networks (BSN’06), Cambridge, MA, USA, 3–5 April 2006; IEEE: Manhattan, NY, USA, 2006; pp. 4–8. [Google Scholar]
- Zago, M.; Sforza, C.; Dolci, C.; Tarabini, M.; Galli, M. Use of machine learning and wearable sensors to predict energetics and kinematics of cutting maneuvers. Sensors 2019, 19, 3094. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, C.E. Gaussian processes in machine learning. In Proceedings of the Summer School on Machine Learning, Canberra, Australia; Springer: Berlin/Heidelberg, Germany, 2003; pp. 63–71. [Google Scholar]
- Specht, D.F. A general regression neural network. IEEE Trans. Neural Netw. 1991, 2, 568–576. [Google Scholar] [CrossRef]
- Balabin, R.M.; Lomakina, E.I. Support vector machine regression (SVR/LS-SVM)—An alternative to neural networks (ANN) for analytical chemistry? Comparison of nonlinear methods on near infrared (NIR) spectroscopy data. Analyst 2011, 136, 1703–1712. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; Singh, H.; Pudi, V. Gear: Generic, efficient, accurate kNN-based regression. In Proceedings of the International Conference on Knowledge Discovery and Information Retrieval, Valencia, Spain, 25–28 October 2010; pp. 1–13. [Google Scholar]
- Huang, Z.; Nagata, A.; Kanai-Pak, M.; Maeda, J.; Kitajima, Y.; Nakamura, M.; Aida, K.; Kuwahara, N.; Ogata, T.; Ota, J. Self-help training system for nursing students to learn patient transfer skills. IEEE Trans. Learn. Technol. 2014, 7, 319–332. [Google Scholar] [CrossRef]
- Ibrahim, R.; Elsaay, O. The effect of body mechanics training program for intensive care nurses in reducing low back pain. IOSR J. Nurs. Health Sci. 2015, 4, 81–96. [Google Scholar]
- Hall, M.; Frank, E.; Holmes, G.; Pfahringer, B.; Reutemann, P.; Witten, I.H. The WEKA data mining software: An update. ACM SIGKDD Explor. Newsl. 2009, 11, 10–18. [Google Scholar] [CrossRef]
- Le, T.Q.; Cheng, C.; Sangasoongsong, A.; Wongdhamma, W.; Bukkapatnam, S.T. Wireless wearable multisensory suite and real-time prediction of obstructive sleep apnea episodes. IEEE J. Transl. Eng. Health Med. 2013, 1, 2700109. [Google Scholar] [CrossRef]
- Zhang, J.; Soangra, R.E.; Lockhart, T. Automatic Detection of Dynamic and Static Activities of the Elderly using a Wearable Sensor and Support Vector Machines. Science 2020, 2, 38. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistics notes: Measurement error proportional to the mean. BMJ 1996, 313, 106. [Google Scholar] [CrossRef]
- Masanovic, B.; Gardasevic, J.; Arifi, F. Relationship between foot length measurements and body height. Anthropologie 2019, 57, 227–234. [Google Scholar] [CrossRef]
- Uhrová, P.; Beňuš, R.; Masnicová, S.; Obertová, Z.; Kramárová, D.; Kyselicová, K.; Dörnhöferová, M.; Bodoriková, S.; Neščáková, E. Estimation of stature using hand and foot dimensions in Slovak adults. Leg. Med. 2015, 17, 92–97. [Google Scholar] [CrossRef]
- Ning, X.; Zhou, J.; Dai, B.; Jaridi, M. The assessment of material handling strategies in dealing with sudden loading: The effects of load handling position on trunk biomechanics. Appl. Ergon. 2014, 45, 1399–1405. [Google Scholar] [CrossRef]
- Mourcou, Q.; Fleury, A.; Franco, C.; Klopcic, F.; Vuillerme, N. Performance evaluation of smartphone inertial sensors measurement for range of motion. Sensors 2015, 15, 23168–23187. [Google Scholar] [CrossRef] [PubMed]
- Keogh, J.W.; Cox, A.; Anderson, S.; Liew, B.; Olsen, A.; Schram, B.; Furness, J. Reliability and validity of clinically accessible smartphone applications to measure joint range of motion: A systematic review. PLoS ONE 2019, 14, e0215806. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.-H. The effects of handle height, load’s CoG height and load on lifting tasks. Appl. Ergon. 2021, 91, 103294. [Google Scholar] [CrossRef]
- Lin, F.; Song, C.; Xu, X.; Cavuoto, L.; Xu, W. Patient handling activity recognition through pressure-map manifold learning using a footwear sensor. Smart Health 2017, 1, 77–92. [Google Scholar] [CrossRef]
- Lin, F.; Wang, A.; Cavuoto, L.; Xu, W. Toward unobtrusive patient handling activity recognition for injury reduction among at-risk caregivers. IEEE J. Biomed. Health Inform. 2016, 21, 682–695. [Google Scholar] [CrossRef]
- Malhi, A.; Gao, R.X. PCA-based feature selection scheme for machine defect classification. IEEE Trans. Instrum. Meas. 2004, 53, 1517–1525. [Google Scholar] [CrossRef]
- Kabir, M.M.; Islam, M.M.; Murase, K. A new wrapper feature selection approach using neural network. Neurocomputing 2010, 73, 3273–3283. [Google Scholar] [CrossRef]
- Duffy, N.; Helmbold, D. Boosting methods for regression. Mach. Learn. 2002, 47, 153–200. [Google Scholar] [CrossRef]
- Breiman, L. Bagging predictors. Mach. Learn. 1996, 24, 123–140. [Google Scholar] [CrossRef]
- Merryweather, A.S.; Loertscher, M.C.; Bloswick, D.S. A revised back compressive force estimation model for ergonomic evaluation of lifting tasks. Work 2009, 34, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Kodama, J.; Watanabe, T. Examination of inertial sensor-based estimation methods of lower limb joint moments and ground reaction force: Results for squat and sit-to-stand movements in the sagittal plane. Sensors 2016, 16, 1209. [Google Scholar] [CrossRef] [PubMed]
- Coviello, G.; Avitabile, G.; Florio, A. The importance of data synchronization in multiboard acquisition systems. In Proceedings of the 2020 IEEE 20th Mediterranean Electrotechnical Conference (MELECON), Palermo, Italy, 16–18 June 2020; IEEE: Manhattan, NY, USA, 2020; pp. 293–297. [Google Scholar]
- Sakuru, K.S.P.; Kondapalli, S.R.R. Performance Evaluation of Sink Node Selection for Time Synchronization in WSN. In Proceedings of the 2014 International Conference on Devices, Circuits and Communications (ICDCCom), Ranchi, India, 12–13 September 2014; IEEE: Manhattan, NY, USA, 2014; pp. 1–5. [Google Scholar]

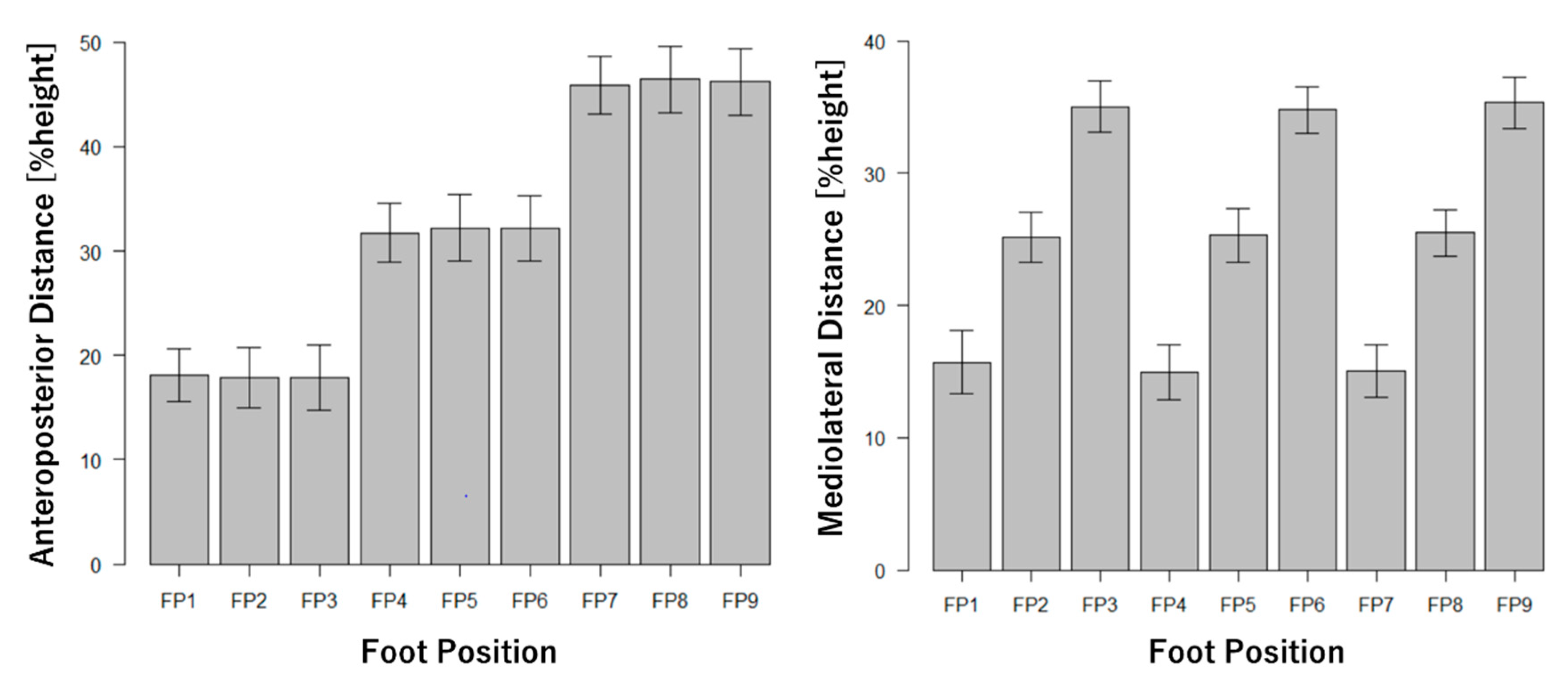
| Mediolateral Distance [%Height] | ||||
|---|---|---|---|---|
| 10–20 | 21–30 | 31–40 | ||
| Anteroposterior Distance [%height] | 10–25 | Position 1 | Position 2 | Position 3 |
| 26–40 | Position 4 | Position 5 | Position 6 | |
| 41–55 | Position 7 | Position 8 | Position 9 | |
| Specification/Parameter | Status/Value | |
|---|---|---|
| Number of Layer | Input Layer | 1 |
| Hidden Layer | 1 | |
| Output Layer | 1 | |
| Number of Neuron / Node | Input Layer | At most 70 (based on features) |
| Hidden Layer | At most 70 (based on features) | |
| Output Layer | 1 | |
| Activation | Hidden Layer | Sigmoid |
| Output Layer | Linear | |
| Learning Rate | 0.3 | |
| Momentum | 0.2 | |
| Training Method | Back Propagation | |
| Specification/Parameter | Status/Value |
|---|---|
| Kernel | RBF Kernel |
| Hyperparameter γ | 1.0 |
| Specification/Parameter | Status/Value |
|---|---|
| Weight | Uniform |
| Distance | Euclidean Distance |
| Hyperparameter K | 1 |
| Specification/Parameter | Status/Value |
|---|---|
| Feature Selection | M5 Method |
| Ridge Parameter R | 1.0 × e−8 |
| Specification/Parameter | Status/Value |
|---|---|
| Training | Sequential Minimal Optimization |
| Kernel | RBF Kernel |
| Hyperparameter γ | 0.01 |
| Feature Pattern | Algorithm | RMSE [%Height] |
|---|---|---|
| Only Inertial Sensor | ANN | 11.5 |
| Gaussian process | 7.20 | |
| kNN | 8.43 | |
| Linear regression | 8.40 | |
| SVR | 9.69 | |
| Only Shoe-type Force Sensors | ANN | 10.6 |
| Gaussian process | 7.10 | |
| kNN | 9.14 | |
| Linear regression | 7.85 | |
| SVR | 8.02 | |
| All Wearable Sensors | ANN | 7.93 |
| Gaussian process | 6.06 | |
| kNN | 6.89 | |
| Linear regression | 6.62 | |
| SVR | 7.30 |
| Feature Pattern | Algorithm | RMSE [%Height] |
|---|---|---|
| Only Inertial Sensor | ANN | 11.0 |
| Gaussian process | 7.16 | |
| kNN | 8.72 | |
| Linear regression | 7.72 | |
| SVR | 8.03 | |
| Only Shoe-type Force Sensors | ANN | 10.9 |
| Gaussian process | 6.50 | |
| kNN | 8.80 | |
| Linear regression | 6.88 | |
| SVR | 7.39 | |
| All Wearable Sensors | ANN | 9.77 |
| Gaussian process | 6.30 | |
| kNN | 8.01 | |
| Linear regression | 6.80 | |
| SVR | 7.00 |
| Foot Position | Paired t-Test (Error vs. Zero) | Correlation (Estimated vs. Actual) | |
|---|---|---|---|
| Significant Difference | Power | ||
| Anteroposterior | N.S. | 0.0284 | 0.891 * |
| Mediolateral | N.S. | 0.0289 | 0.692 * |
| Foot Position | Limitation of Agreement [%Height] | Correlation (as Proportional Error) |
|---|---|---|
| Anteroposterior | −10.9 to 10.9 | 0.682 * |
| Mediolateral | −11.4 to 11.3 | 0.758 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kitagawa, K.; Gorordo Fernandez, I.; Nagasaki, T.; Nakano, S.; Hida, M.; Okamatsu, S.; Wada, C. Foot Position Measurement during Assistive Motion for Sit-to-Stand Using a Single Inertial Sensor and Shoe-Type Force Sensors. Int. J. Environ. Res. Public Health 2021, 18, 10481. https://doi.org/10.3390/ijerph181910481
Kitagawa K, Gorordo Fernandez I, Nagasaki T, Nakano S, Hida M, Okamatsu S, Wada C. Foot Position Measurement during Assistive Motion for Sit-to-Stand Using a Single Inertial Sensor and Shoe-Type Force Sensors. International Journal of Environmental Research and Public Health. 2021; 18(19):10481. https://doi.org/10.3390/ijerph181910481
Chicago/Turabian StyleKitagawa, Kodai, Ibai Gorordo Fernandez, Takayuki Nagasaki, Sota Nakano, Mitsumasa Hida, Shogo Okamatsu, and Chikamune Wada. 2021. "Foot Position Measurement during Assistive Motion for Sit-to-Stand Using a Single Inertial Sensor and Shoe-Type Force Sensors" International Journal of Environmental Research and Public Health 18, no. 19: 10481. https://doi.org/10.3390/ijerph181910481
APA StyleKitagawa, K., Gorordo Fernandez, I., Nagasaki, T., Nakano, S., Hida, M., Okamatsu, S., & Wada, C. (2021). Foot Position Measurement during Assistive Motion for Sit-to-Stand Using a Single Inertial Sensor and Shoe-Type Force Sensors. International Journal of Environmental Research and Public Health, 18(19), 10481. https://doi.org/10.3390/ijerph181910481






