Ergonomic Comparison of Four Dental Workplace Concepts Using Inertial Motion Capture for Dentists and Dental Assistants
Abstract
:1. Background
2. Materials and Methods
2.1. Subjects
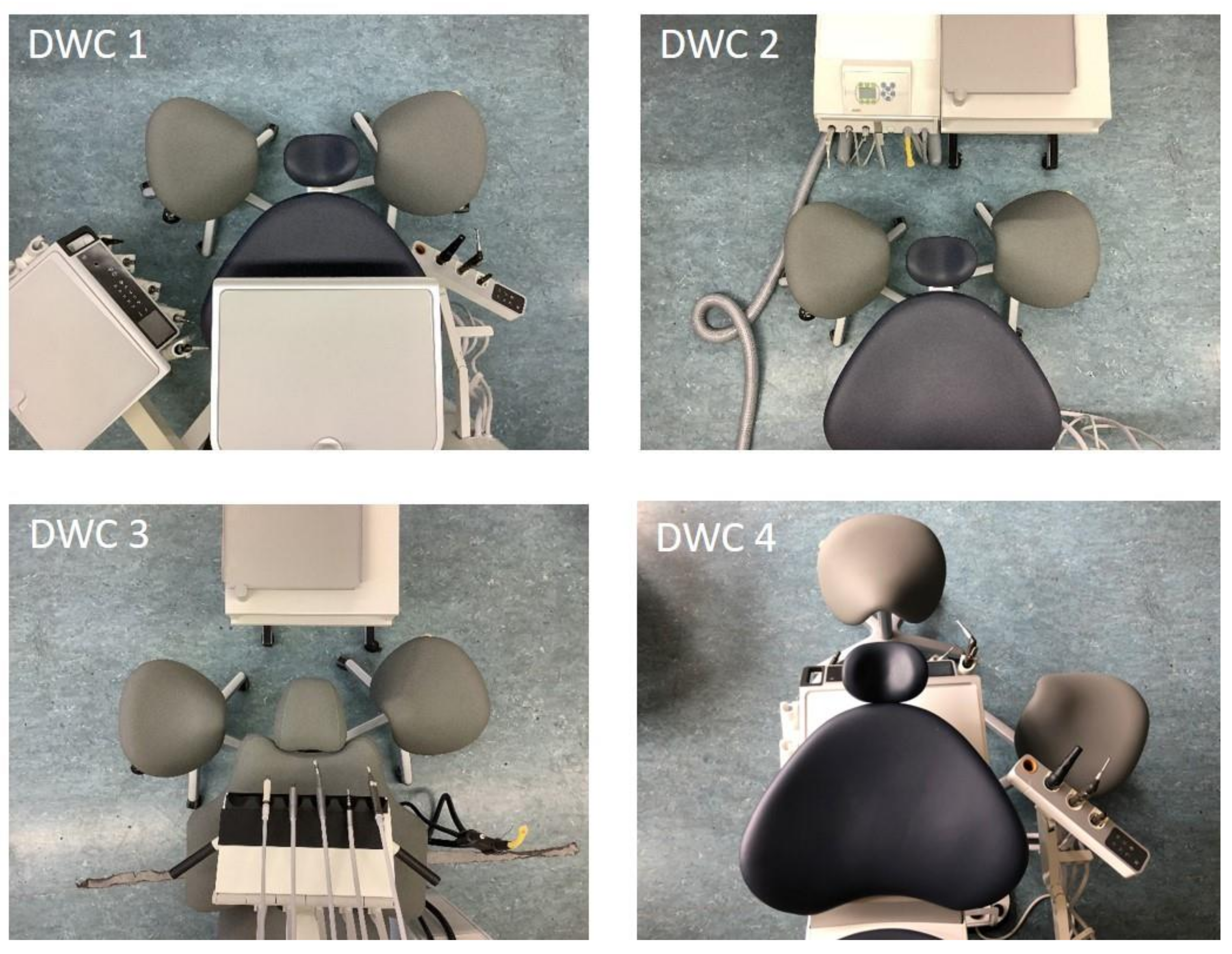
2.2. Dental Working Concepts (DWCs)
2.3. Measurement System
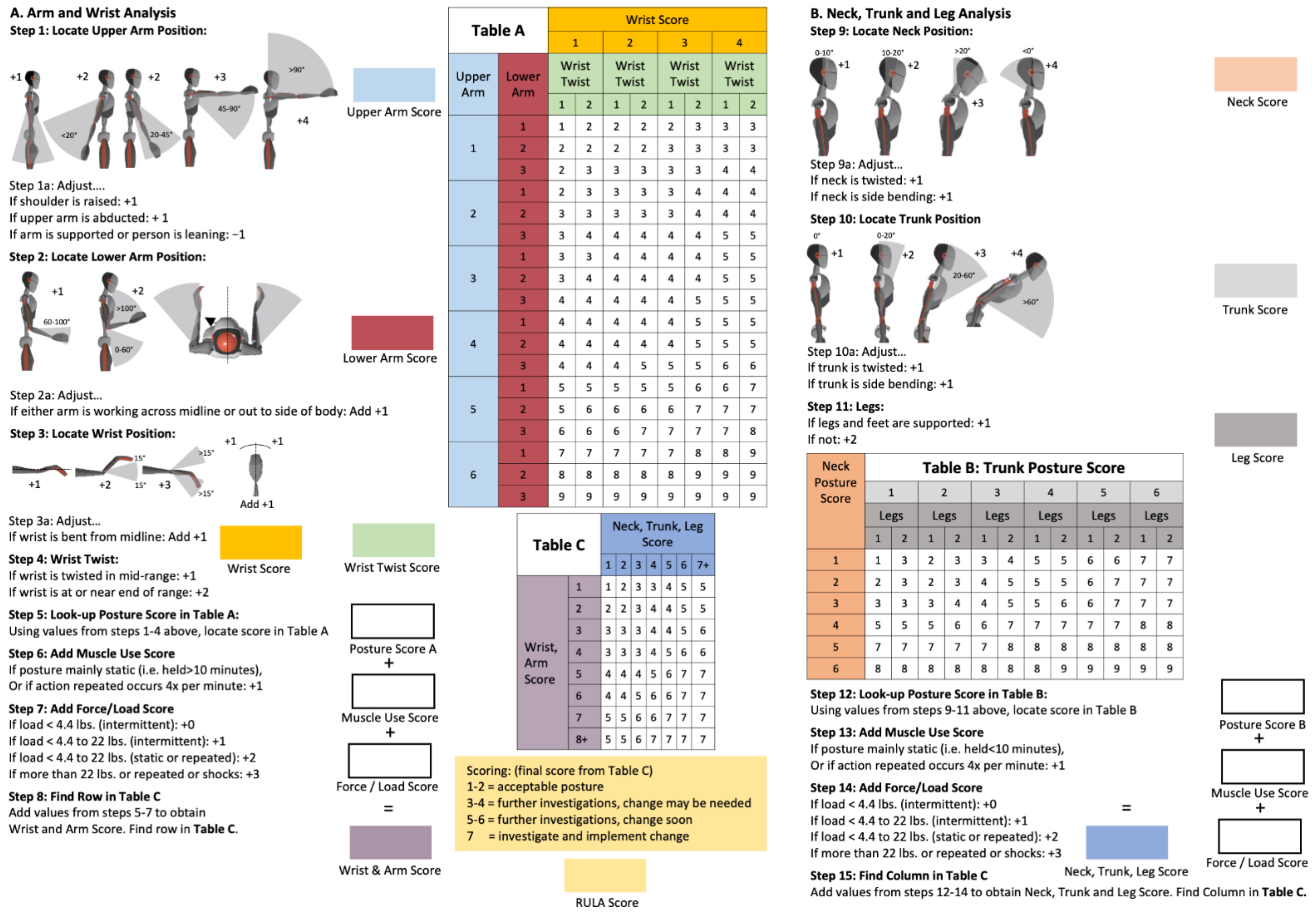
2.4. Rapid Upper Limb Assessment (RULA)
2.5. Measurement Protocol
2.6. Data Analysis
2.7. Statistical Analysis
3. Results
3.1. Dental Assistants
3.2. Dentists
3.3. Differences in the Ergonomic Risk between Dentists and Dental Assistants by Dental Workplace Concept
3.4. DWC 1
3.5. DWC 2
3.6. DWC 3
3.7. DWC 4
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ohlendorf, D.; Haas, Y.; Naser, A.; Haenel, J.; Maltry, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brüggmann, D.; et al. Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants. Int. J. Environ. Res. Public Health 2020, 17, 3490. [Google Scholar] [CrossRef]
- Hayes, M.; Cockrell, D.; Smith, D.R. A systematic review of musculoskeletal disorders among dental professionals. Int. J. Dent. Hyg. 2009, 7, 159–165. [Google Scholar] [CrossRef]
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef] [Green Version]
- Ohlendorf, D.; Maltry, L.; Hänel, J.; Betz, W.; Erbe, C.; Maurer-Grubinger, C.; Holzgreve, F.; Wanke, E.M.; Brüggmann, D.; Nienhaus, A.; et al. SOPEZ: Study for the optimization of ergonomics in the dental practice—Musculoskeletal disorders in dentists and dental assistants: A study protocol. J. Occup. Med. Toxicol. 2020, 15, 22. [Google Scholar] [CrossRef]
- Kimmel, K. Die Basiskonzepte. Grundlage der Behandlungsplatzgestaltung. Quintessenz Zahntech. 1989, 40, 2251–2258. [Google Scholar]
- Kimmel, K. Ein Identifikationssystem für die zahnärztliche Ausrüstung. Zahnarztl. Mitt. 1973, 65, 522–527. [Google Scholar]
- Kimmel, K. Der zahnärztliche Arbeitsplatz. Funktion und Gestaltung. Zahnärztliche Welt 1980, 89, 40–52. [Google Scholar]
- Ohlendorf, D.; Naser, A.; Haas, Y.; Haenel, J.; Fraeulin, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brueggmann, D.; et al. Prevalence of Musculoskeletal Disorders among Dentists and Dental Students in Germany. Int. J. Environ. Res. Public Health 2020, 17, 8740. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Burke, F.J.; Macdonald, E.B.; Gilmour, H.; Hill, K.B.; Morris, A.J.; White, D.A.; Muirhead, E.K.; Murray, K. Dental practitioners and ill health retirement: Causes, outcomes and re-employment. Br. Dent. J. 2010, 209, E7. [Google Scholar] [CrossRef]
- Hill, K.B.; Burke, F.J.; Brown, J.; Macdonald, E.B.; Morris, A.J.; White, D.A.; Murray, K. Dental practitioners and ill health retirement: A qualitative investigation into the causes and effects. Br. Dent. J. 2010, 209, E8. [Google Scholar] [CrossRef] [Green Version]
- Alnaser, M.Z.; Almaqsied, A.M.; Alshatti, S.A. Risk factors for work-related musculoskeletal disorders of dentists in Kuwait and the impact on health and economic status. Work 2021, 68, 213–221. [Google Scholar] [CrossRef]
- Leggat, P.; Kedjarune, U.; Smith, D. Occupational Health Problems in Modern Dentistry: A Review. Ind. Health 2007, 45, 611–621. [Google Scholar] [CrossRef] [Green Version]
- McAtamney, L.; Nigel Corlett, E. RULA: A survey method for the investigation of work-related upper limb disorders. Appl. Ergon. 1993, 24, 91–99. [Google Scholar] [CrossRef]
- Golchha, V.; Sharma, P.; Wadhwa, J.; Yadav, D.; Paul, R. Ergonomic risk factors and their association with musculoskeletal disorders among Indian dentist: A preliminary study using Rapid Upper Limb Assessment. Indian J. Dent. Res. 2014, 25, 767–771. [Google Scholar] [CrossRef] [PubMed]
- Plantard, P.; Shum, H.P.H.; Le Pierres, A.-S.; Multon, F. Validation of an ergonomic assessment method using Kinect data in real workplace conditions. Appl. Ergon. 2017, 65, 562–569. [Google Scholar] [CrossRef] [PubMed]
- Vignais, N.; Bernard, F.; Touvenot, G.; Sagot, J.C. Physical risk factors identification based on body sensor network combined to videotaping. Appl. Ergon. 2017, 65, 410–417. [Google Scholar] [CrossRef]
- Vignais, N.; Miezal, M.; Bleser, G.; Mura, K.; Gorecky, D.; Marin, F. Innovative system for real-time ergonomic feedback in industrial manufacturing. Appl. Ergon. 2013, 44, 566–574. [Google Scholar] [CrossRef] [PubMed]
- van der Straaten, R.; Bruijnes, A.K.B.D.; Vanwanseele, B.; Jonkers, I.; De Baets, L.; Timmermans, A. Reliability and Agreement of 3D Trunk and Lower Extremity Movement Analysis by Means of Inertial Sensor Technology for Unipodal and Bipodal Tasks. Sensors 2019, 19, 141. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.T.; Novak, A.C.; Brouwer, B.; Li, Q. Concurrent validation of Xsens MVN measurement of lower limb joint angular kinematics. Physiol. Meas. 2013, 34, N63–N69. [Google Scholar] [CrossRef]
- Lobo, D.; Anuarbe, P.; Lopez-Higuera, J.M.; Viera, J.; Castillo, N.; Megia, R. Estimation of surgeons’ ergonomic dynamics with a structured light system during endoscopic surgery. Int. Forum Allergy Rhinol. 2019, 9, 857–864. [Google Scholar] [CrossRef]
- Schoen, F. Teamarbeit in der zahnarztlichen Praxis; Quintessenz: Cologne, Germany, 1972. [Google Scholar]
- Kilpatrick, H.C. Work Simplification in Dental Practice, 3rd ed.; Saunders: Philadelphia, PA, USA, 1974. [Google Scholar]
- Guastamacchia, C. Elementi di Ergonomia e Pratica Professionale Odontoiatrica; Maason: Milan, Italy, 1988. [Google Scholar]
- Skovsgaard, H. Dancing Hands; Quintessence Publishing Co., Ltd.: London, UK, 2013. [Google Scholar]
- Robinson, M. Home Position Dentistry—The Beach Philosophy of Dental Practice; Bikensha Col.: Kyoto, Japan, 1976. [Google Scholar]
- Maurer-Grubinger, C.; Holzgreve, F.; Fraeulin, L.; Betz, W.; Erbe, C.; Brueggmann, D.; Wanke, E.M.; Nienhaus, A.; Groneberg, D.A.; Ohlendorf, D. Combining Ergonomic Risk Assessment (RULA) with Inertial Motion Capture Technology in Dentistry—Using the Benefits from Two Worlds. Sensors 2021, 21, 4077. [Google Scholar] [CrossRef]
- Technologies, X. Xsens MVN User Manual. Technical Report Document MV0319P, Revision U; Xsens Technologies B. V.: Enschede, The Netherlands, 2017. [Google Scholar]
- Rasch, B.; Born, J. About sleep’s role in memory. Physiol. Rev. 2013, 93, 681–766. [Google Scholar] [CrossRef]
- Alghadir, A.; Zafar, H.; Iqbal, Z.A. Work-related musculoskeletal disorders among dental professionals in Saudi Arabia. J. Phys. Ther. Sci. 2015, 27, 1107–1112. [Google Scholar] [CrossRef] [Green Version]
- Hodacova, L.; Sustova, Z.; Cermakova, E.; Kapitan, M.; Smejkalova, J. Self-reported risk factors related to the most frequent musculoskeletal complaints among Czech dentists. Ind. Health 2015, 53, 48–55. [Google Scholar] [CrossRef] [Green Version]
- Nokhostin, M.R.; Zafarmand, A.H. “Musculoskeletal problem”: Its prevalence among Iranian dentists. J. Int. Soc. Prev. Community Dent. 2016, 6, S41–S46. [Google Scholar] [CrossRef] [Green Version]
- Proteau, R.-A. Prevention of Work-Related Musculoskeletal Disorders (MSDs) in Dental Clinics; Assication Paritaire pour la Santé et la Sécurité du travail du Secteur Affaires Sociales: Quebec, QC, Canada, 2007. [Google Scholar]
- Feng, B.; Liang, Q.; Wang, Y.; Andersen, L.L.; Szeto, G. Prevalence of work-related musculoskeletal symptoms of the neck and upper extremity among dentists in China. BMJ Open 2014, 4, e006451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gandolfi, M.G.; Zamparini, F.; Spinelli, A.; Risi, A.; Prati, C. Musculoskeletal Disorders among Italian Dentists and Dental Hygienists. Int. J. Environ. Res. Public Health 2021, 18, 2705. [Google Scholar] [CrossRef] [PubMed]
- De Sio, S.; Traversini, V.; Rinaldo, F.; Colasanti, V.; Buomprisco, G.; Perri, R.; Mormone, F.; La Torre, G.; Guerra, F. Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: An umbrella review. PeerJ 2018, 6, e4154. [Google Scholar] [CrossRef]
- Barrett, J.M.; McKinnon, C.; Callaghan, J.P. Cervical spine joint loading with neck flexion. Ergonomics 2020, 63, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Diao, H.; Xin, H.; Jin, Z. Prediction of in vivo lower cervical spinal loading using musculoskeletal multi-body dynamics model during the head flexion/extension, lateral bending and axial rotation. Proc. Inst. Mech. Eng. H 2018, 232, 1071–1082. [Google Scholar] [CrossRef] [PubMed]
- Quarrington, R.D.; Costi, J.J.; Freeman, B.J.C.; Jones, C.F. The effect of axial compression and distraction on cervical facet mechanics during anterior shear, flexion, axial rotation, and lateral bending motions. J. Biomech. 2019, 83, 205–213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- RKI. Gesundheitsberichterstattung des Bundes—Gemeinsam Getragen von RKI und Destatis; Robert-Koch-Institut: Berlin, Germany, 2015. [Google Scholar]
- Yiu, X.Y.; Maguire, A.; Johnson, M.; Wåhlin, C.; Johnston, V. A 10-week exercise intervention can improve work posture but not neck/shoulder symptoms in dental health students: A pilot cohort study. Work 2020, 67, 239–249. [Google Scholar] [CrossRef] [PubMed]
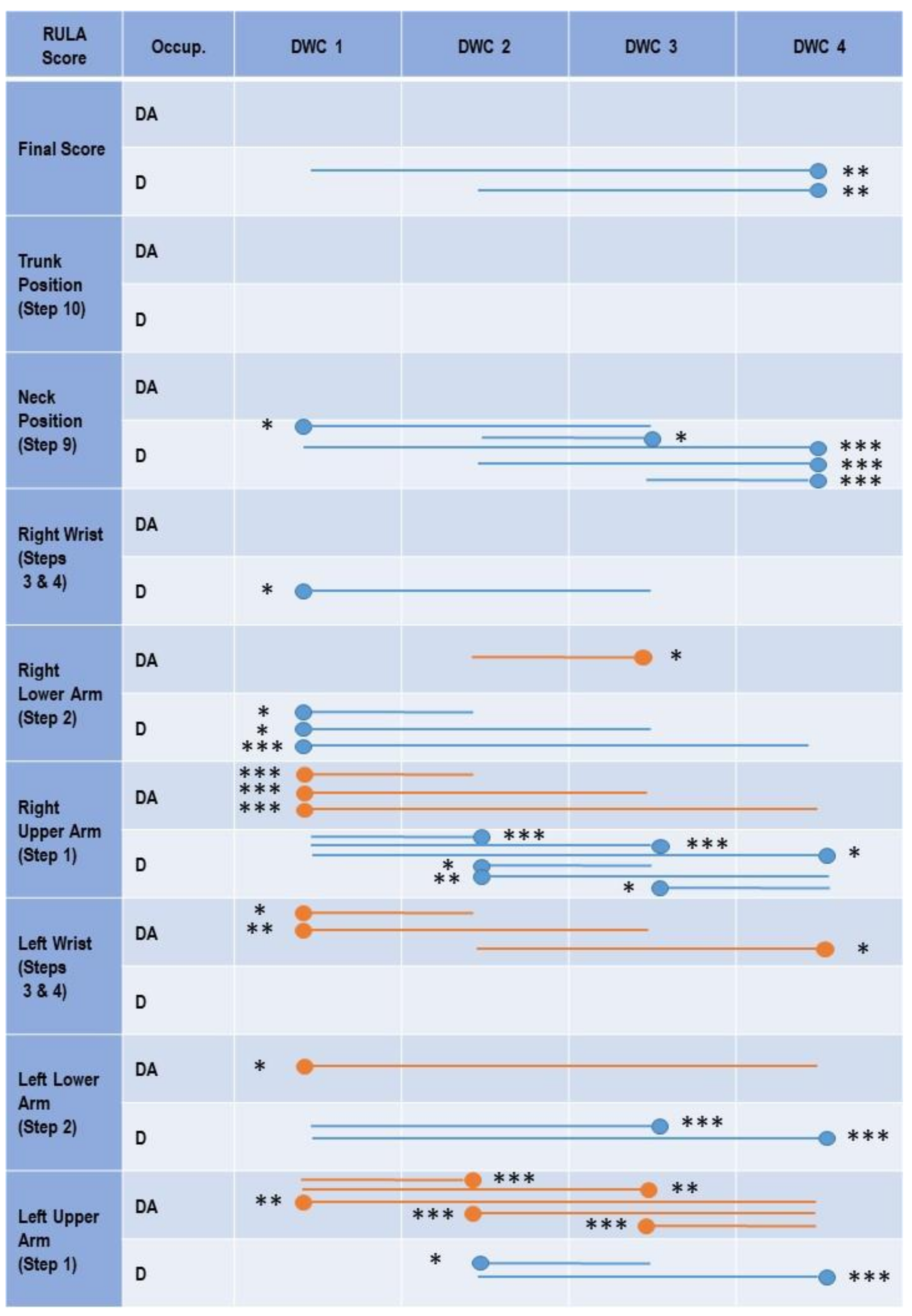

| RULA Score | Occupation | DWC 1 | DWC 2 | DWC 3 | DWC 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQD) | Rel. av. RST | ERP (%) | Median (IQD) | Rel. av. RST | ERP | Median (IQD) | Rel. av. RST | ERP (%) | Median (IQD) | Rel. av. RST | ERP (%) | ||
| Final (Max. Score 7) | DA | 7 (0.5) | 6.75 | 96.43 | 7 (0) | 6.77 | 96.71 | 7 (0.5) | 6.75 | 96.43 | 7 (1) | 6.78 | 96.86 |
| D | 7 (0.5) | 6.71 | 95.86 | 7 (0.5) | 6.73 | 96.14 | 7 (0.5) | 6.74 | 96.29 | 7 (0) ** | 6.64 *** | 94.86 | |
| Trunk Position–Step 10 | DA | 2 (0.5) | 2.27 * | 37.83 | 2 (1) | 2.38 | 39.64 | 2 (1) ** | 2.33 | 38.86 | 2 (1) | 2.32 | 38.72 |
| D | 2.5 (1) | 2.51 | 41.84 | 3 (1) * | 2.56 * | 42.74 | 3 (1) | 2.56 | 42.60 | 3 (1) | 2.57 | 42.90 | |
| Neck Position–Step 9 | DA | 3 (1) | 3.52 | 58.71 | 3.5 (1) | 3.59 | 59.90 | 3.5 (1) | 3.57 | 59.42 | 3.5 (1) | 3.54 | 58.99 |
| D | 3 (1) | 3.49 | 58.22 | 3 (1) | 3.53 | 58.87 | 3 (1) | 3.51 | 58.53 | 3 (0.5) *** | 3.27 *** | 54.49 | |
| Right Wrist–Steps 3 & 4 | DA | 4.5 (1) | 4.47 | 74.44 | 4 (1) | 4.33 | 72.12 | 4 (1) | 4.37 | 72.88 | 4.5 (1) | 4.38 | 72.96 |
| D | 4 (1) * | 4.30 * | 71.59 | 4 (1) | 4.37 | 72.77 | 4 (1) | 4.36 | 72.72 | 4 (1) | 4.31 | 71.85 | |
| Right Lower Arm–Step 2 | DA | 2.5 (1) | 2.48 | 82.53 | 2.5 (1) | 2.48 | 82.73 | 2 (1) | 2.42 | 80.62 | 2.5 (1) | 2.51 | 83.74 |
| D | 2 (1) *** | 2.25 *** | 75.14 | 2 (1) ** | 2.30 *** | 76.62 | 2 (1) | 2.30 ** | 76.51 | 2 (1) *** | 2.30 *** | 76.60 | |
| Right Upper Arm–Step 1 | DA | 1.5 (1) *** | 1.58 *** | 26.37 | 2 (1) | 1.78 | 29.60 | 2 (1) | 1.79 | 29.82 | 2 (0.5) | 1.75 * | 29.22 |
| D | 2 (0) | 1.97 | 32.75 | 2 (1) | 1.78 | 29.60 | 2 (0.5) | 1.83 | 30.46 | 2 (0.5) | 1.88 | 31.38 | |
| Left Wrist–Steps 3 & 4 | DA | 4 (1) | 4.26 | 71.05 | 4 (1) | 4.40 | 73.40 | 4.5 (1) | 4.38 | 73.01 | 4 (1) | 4.31 * | 71.77 |
| D | 4.5 (1) | 4.44 | 73.95 | 4.5 (1) | 4.39 | 73.09 | 4.5 (1) | 4.45 | 74.19 | 5 (1) | 4.51 | 75.21 | |
| Left Lower Arm–Step 2 | DA | 2 (1) | 2.44 | 81.27 | 2.5 (1) | 2.50 | 83.17 | 2.5 (1) | 2.49 | 82.84 | 3 (1) | 2.56 | 85.30 |
| D | 2.5 (1) | 2.46 | 82.12 | 2 (1) | 2.38 | 79.43 | 2 (1) | 2.35 | 78.25 | 2 (1) ** | 2.32 *** | 77.20 | |
| Left Upper Arm–Step 1 | DA | 1..5 (1) | 1.60 | 26.58 | 1 (1) | 1.40 | 23.29 | 1.5 (1) | 1.49 | 24.86 | 2 (1) | 1.74 | 28.99 |
| D | 1 (1) | 1.41 | 23.50 | 1 (1) | 1.47 | 24.44 | 1 (1) | 1.47 | 24.50 | 1 (1) * | 1.42 *** | 23.58 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohlendorf, D.; Fraeulin, L.; Haenel, J.; Betz, W.; Erbe, C.; Holzgreve, F.; Wanke, E.M.; Brueggmann, D.; Nienhaus, A.; Maurer-Grubinger, C.; et al. Ergonomic Comparison of Four Dental Workplace Concepts Using Inertial Motion Capture for Dentists and Dental Assistants. Int. J. Environ. Res. Public Health 2021, 18, 10453. https://doi.org/10.3390/ijerph181910453
Ohlendorf D, Fraeulin L, Haenel J, Betz W, Erbe C, Holzgreve F, Wanke EM, Brueggmann D, Nienhaus A, Maurer-Grubinger C, et al. Ergonomic Comparison of Four Dental Workplace Concepts Using Inertial Motion Capture for Dentists and Dental Assistants. International Journal of Environmental Research and Public Health. 2021; 18(19):10453. https://doi.org/10.3390/ijerph181910453
Chicago/Turabian StyleOhlendorf, Daniela, Laura Fraeulin, Jasmin Haenel, Werner Betz, Christina Erbe, Fabian Holzgreve, Eileen M. Wanke, Doerthe Brueggmann, Albert Nienhaus, Christian Maurer-Grubinger, and et al. 2021. "Ergonomic Comparison of Four Dental Workplace Concepts Using Inertial Motion Capture for Dentists and Dental Assistants" International Journal of Environmental Research and Public Health 18, no. 19: 10453. https://doi.org/10.3390/ijerph181910453
APA StyleOhlendorf, D., Fraeulin, L., Haenel, J., Betz, W., Erbe, C., Holzgreve, F., Wanke, E. M., Brueggmann, D., Nienhaus, A., Maurer-Grubinger, C., & Groneberg, D. A. (2021). Ergonomic Comparison of Four Dental Workplace Concepts Using Inertial Motion Capture for Dentists and Dental Assistants. International Journal of Environmental Research and Public Health, 18(19), 10453. https://doi.org/10.3390/ijerph181910453











