Maternal Psychological Distress and Children’s Internalizing/Externalizing Problems during the COVID-19 Pandemic: The Moderating Role Played by Hypermentalization
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Participants
2.3. Measures
3. Results
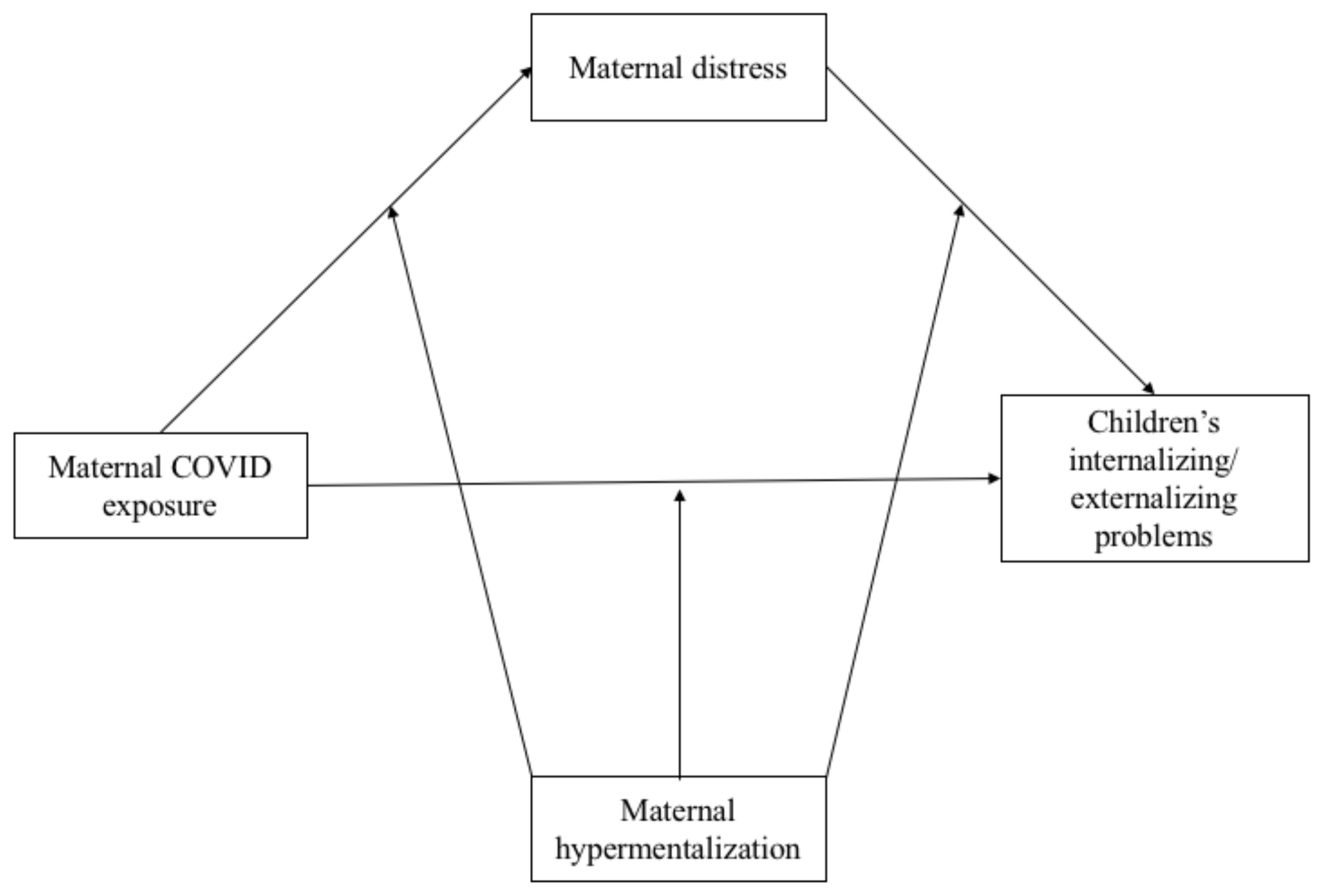
3.1. Statistical Analyses
3.2. Preliminary Analysis
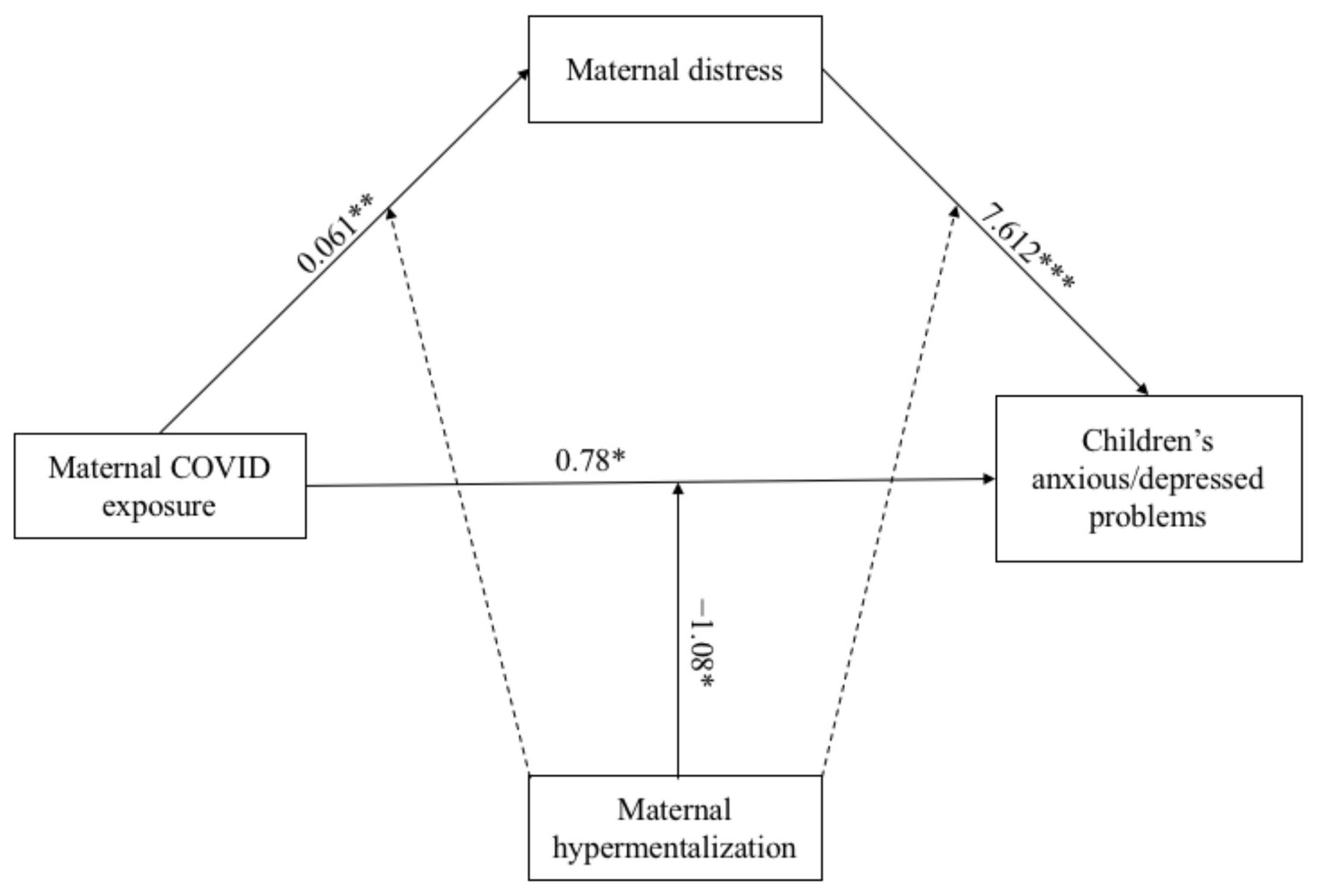
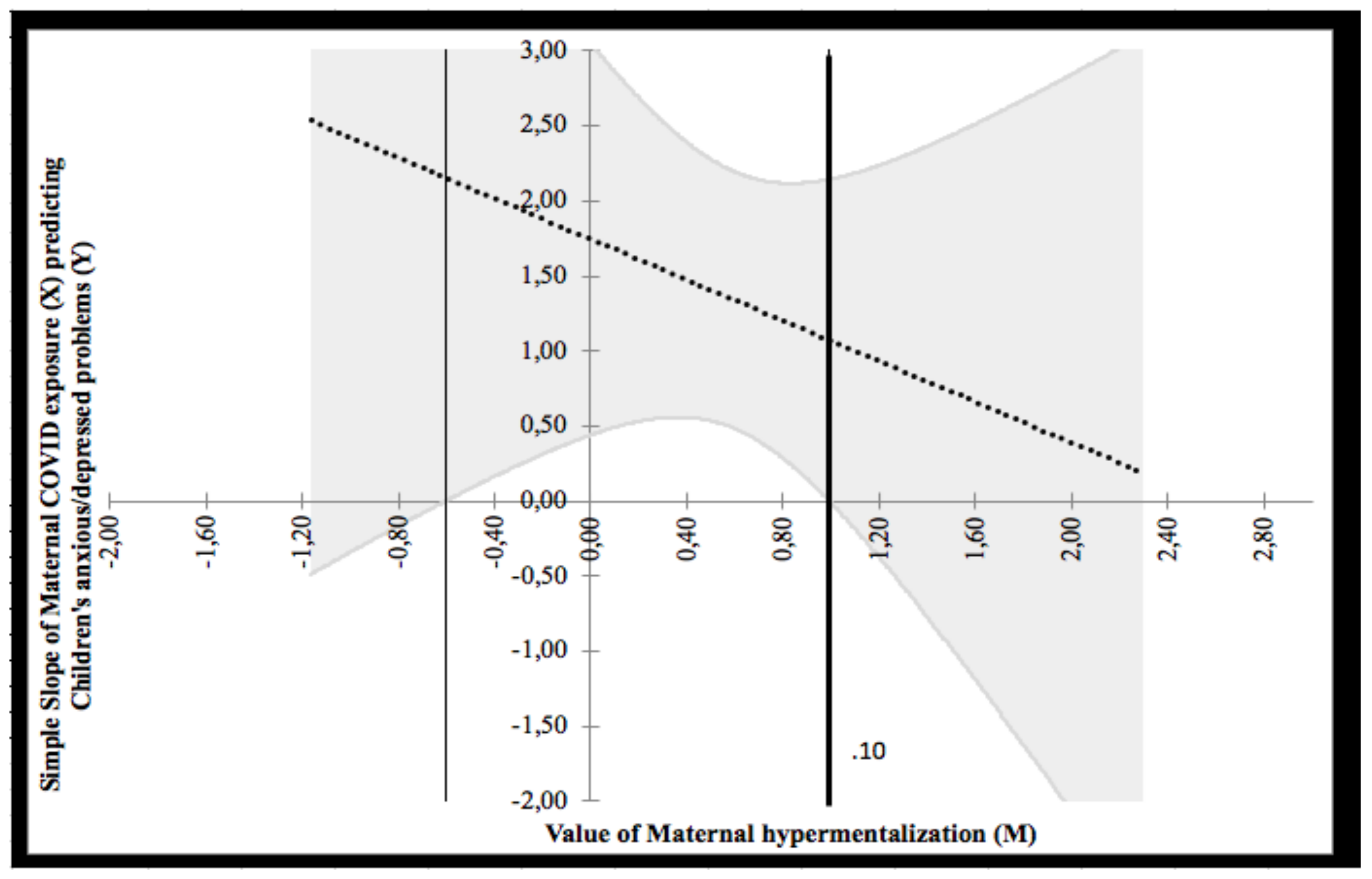
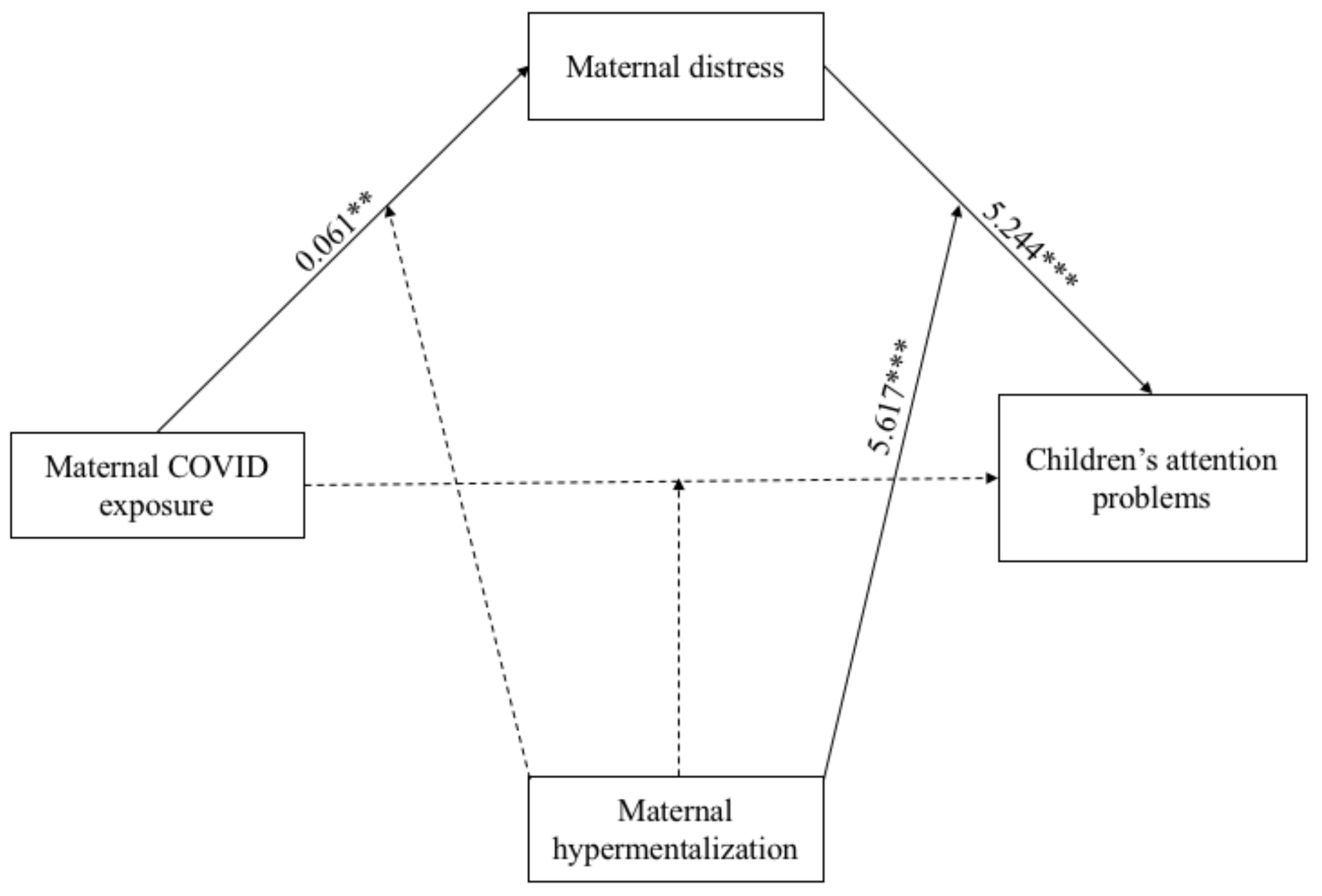
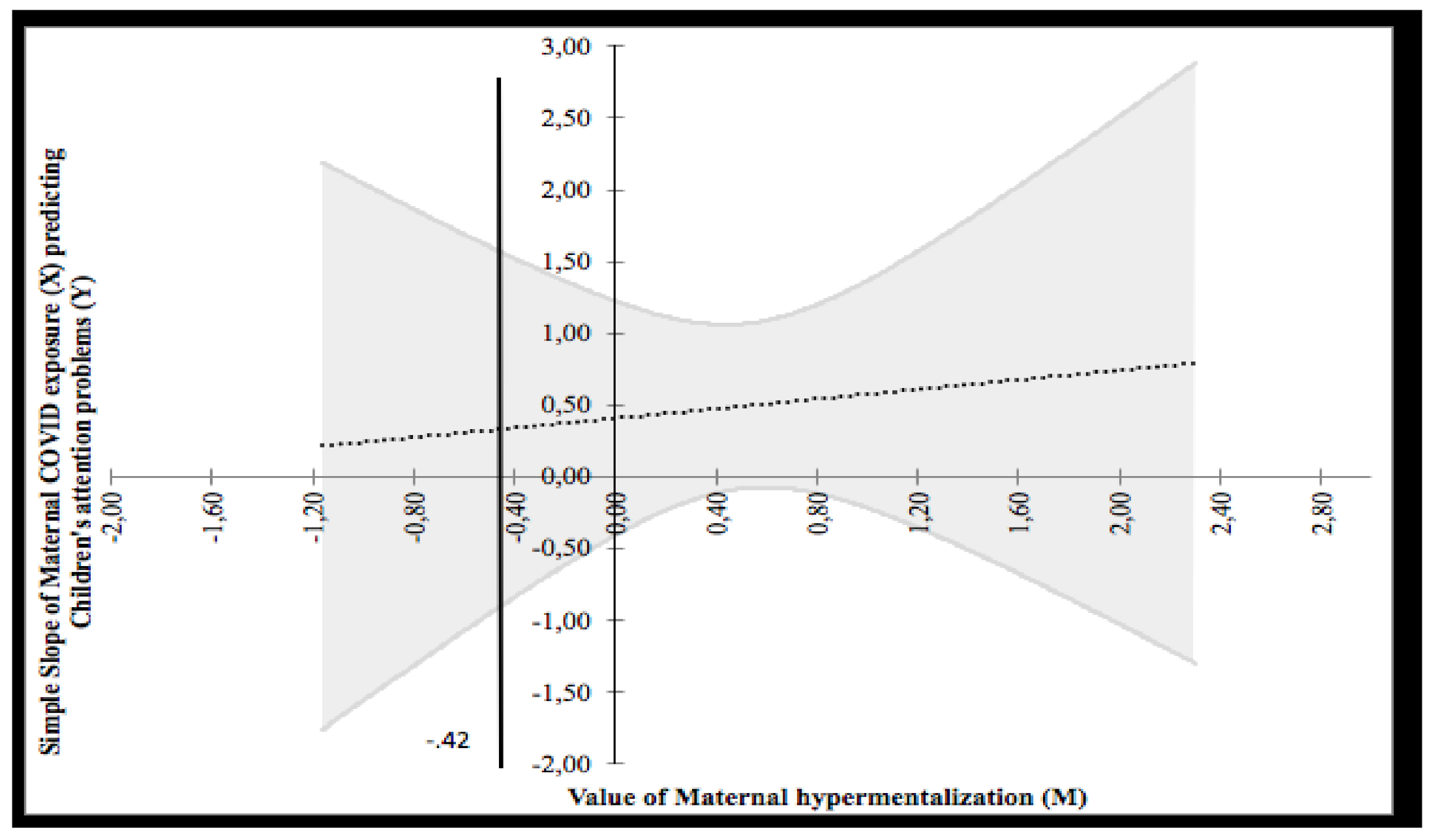
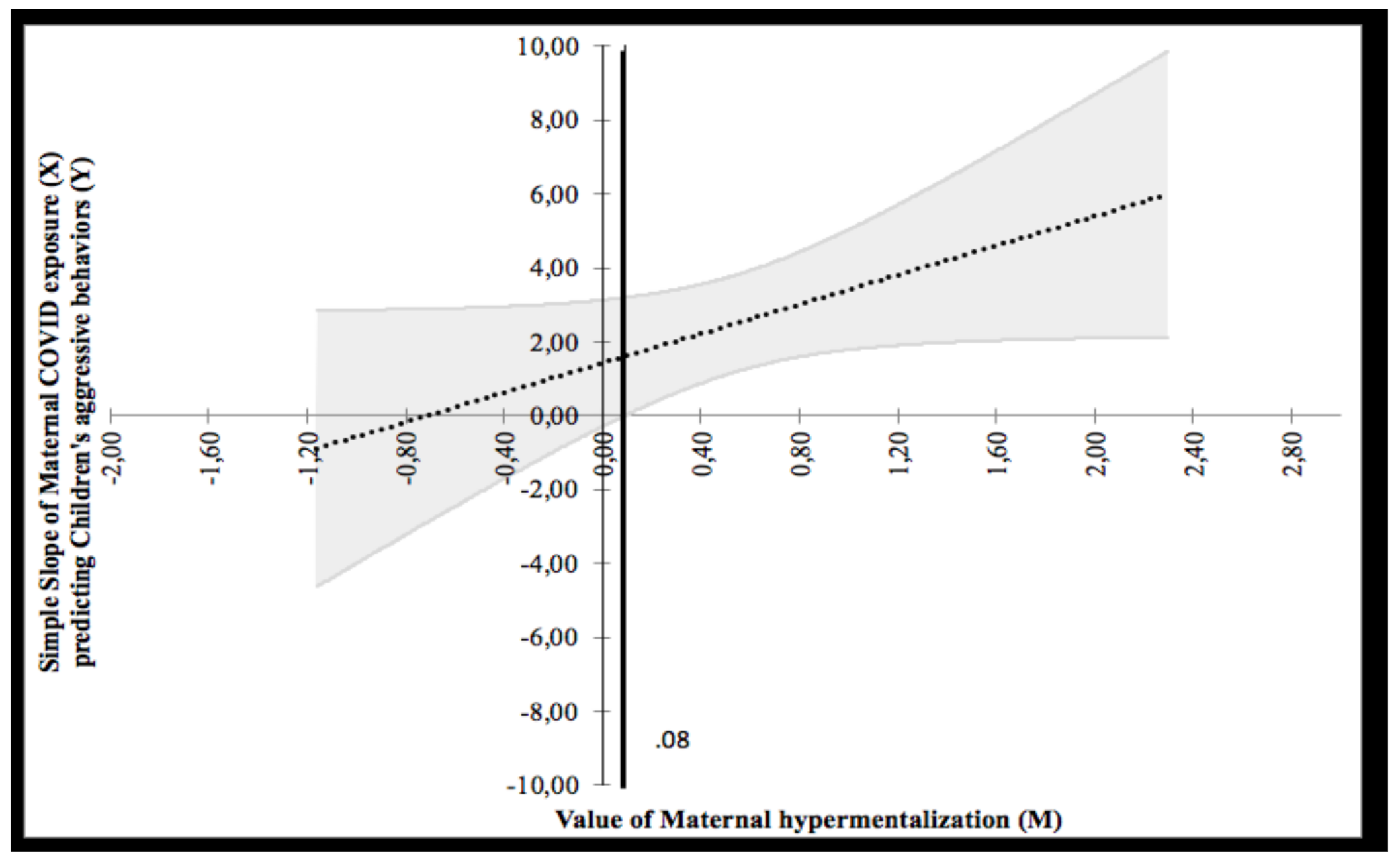
3.3. Moderated Mediation Model

4. Discussion
4.1. Differences between Families Living in Northern Italy vs. Southern Italy
4.2. The Effects of COVID-19 Exposure on Maternal and Children’s Psychological Outcomes
4.3. The Role of RFQ in the Interplay among COVID-19 Exposure and Maternal and Children’s Psychological Outcomes
4.4. Limits
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020, 221, 264–266.e1. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, M.; Lionetti, F.; Pastore, M.; Fasolo, M. Parents’ stress and children’s psychological problems in families facing the COVID-19 outbreak in Italy. Front. Psychol. 2020, 11, 1713. [Google Scholar] [CrossRef]
- Xie, X.; Xue, Q.; Zhou, Y.; Zhu, K.; Liu, Q.; Zhang, J.; Song, R. Mental health status among children in home confinement during the Coronavirus Disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020, 174, 898. [Google Scholar] [CrossRef] [Green Version]
- Di Giorgio, E.; Di Riso, D.; Mioni, G.; Cellini, N. The interplay between mothers’ and children behavioral and psychological factors during COVID-19: An Italian study. Eur. Child Adolesc. Psychiatry 2020, 30, 1401–1412. [Google Scholar] [CrossRef]
- Dellagiulia, A.; Lionetti, F.; Fasolo, M.; Verderame, C.; Sperati, A.; Alessandri, G. Early impact of COVID-19 lockdown on children’s sleep: A 4-week longitudinal study. J. Clin. Sleep Med. 2020, 16, 1639–1640. [Google Scholar] [CrossRef]
- Haig-Ferguson, A.; Cooper, K.; Cartwright, E.; Loades, M.; Daniels, J. Practitioner review: Health anxiety in children and young people in the context of the COVID-19 pandemic. Behav. Cogn. Psychother. 2021, 49, 129–143. [Google Scholar] [CrossRef]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef]
- World Health Organization Mental Health. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak; World Health Organization. Available online: https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2 (accessed on 18 September 2020).
- United Nations. Policy Brief: Covid-19 and the Need for Action on Mental Health; United Nations: New York, NY, USA, 2020. [Google Scholar]
- Masten, A.S.; Narayan, A.J. Child development in the context of disaster, war, and terrorism: Pathways of risk and resilience. Annu. Rev. Psychol. 2012, 63, 227–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morris, A.S.; Silk, J.S.; Steinberg, L.; Myers, S.S.; Robinson, L.R. The role of the family context in the development of emotion regulation. Soc. Dev. 2007, 16, 361–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allen, J.G.; Fonagy, P. The Handbook of Mentalization-Based Treatment; John Wiley & Sons: Hoboken, NJ, USA, 2006. [Google Scholar]
- Sharp, C.; Fonagy, P. The parent’s capacity to treat the child as a psychological agent: Constructs, measures and implications for developmental psychopathology. Soc. Dev. 2008, 17, 737–754. [Google Scholar] [CrossRef] [Green Version]
- Slade, A. Parental reflective functioning: An introduction. Attach. Hum. Dev. 2005, 7, 269–281. [Google Scholar] [CrossRef]
- Castelli, I.; Cavalli, G.; Di Terlizzi, E.; Lecciso, F.; Lucchini, B.; Massaro, D.; Petrocchi, S.; Valle, A. Theory of mind in typical and atypical developmental settings: Some considerations from a contextual perspective. In Reflective Thinking in Educational Settings; Cambridge University Press (CUP): Cambridge, UK, 2014; pp. 102–136. [Google Scholar]
- Rostad, W.L.; Whitaker, D.J. The association between reflective functioning and parent–child relationship quality. J. Child Fam. Stud. 2016, 25, 2164–2177. [Google Scholar] [CrossRef]
- Fonagy, P.; Gergely, G.; Jurist, E.L.; Target, M. Affect Regulation, Mentalization, and the Development of the Self; Routledge: Oxfordshire, UK, 2018. [Google Scholar]
- Benbassat, N.; Priel, B. Parenting and adolescent adjustment: The role of parental reflective function. J. Adolesc. 2012, 35, 163–174. [Google Scholar] [CrossRef]
- Ha, C.; Sharp, C.; Goodyer, I. The role of child and parental mentalizing for the development of conduct problems over time. Eur. Child Adolesc. Psychiatry 2011, 20, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J. Affect. Disord. 2020, 275, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry 2021, 1–11. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239. [Google Scholar] [CrossRef]
- Brown, S.M.; Doom, J.; Lechuga-Peña, S.; Watamura, S.E.; Koppels, T. Stress and parenting during the global COVID-19 pandemic. Child Abus. Negl. 2020, 110, 104699. [Google Scholar] [CrossRef]
- Chung, G.; Lanier, P.; Wong, P.Y.J. Mediating effects of parental stress on harsh parenting and parent-child relationship during Coronavirus (COVID-19) pandemic in Singapore. J. Fam. Violence 2020, 1-12, 1–12. [Google Scholar] [CrossRef]
- Morelli, M.; Cattelino, E.; Baiocco, R.; Trumello, C.; Babore, A.; Candelori, C.; Chirumbolo, A. Parents and children during the COVID-19 lockdown: The influence of parenting distress and parenting self-efficacy on children’s emotional well-being. Front. Psychol. 2020, 11, 584645. [Google Scholar] [CrossRef]
- Petrocchi, S.; Levante, A.; Bianco, F.; Castelli, I.; Lecciso, F. Maternal distress/coping and children’s adaptive behaviors during the COVID-19 lockdown: Mediation through children’s emotional experience. Front. Public Health 2020, 8, 587833. [Google Scholar] [CrossRef] [PubMed]
- Sprang, G.; Silman, M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013, 7, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Ensink, K.; Bégin, M.; Normandin, L.; Godbout, N.; Fonagy, P. Mentalization and dissociation in the context of trauma: Implications for child psychopathology. J. Trauma Dissociation 2017, 18, 11–30. [Google Scholar] [CrossRef] [PubMed]
- Halfon, S.; Besiroglu, B. Parental reflective function and children’s attachment-based mental state talk as predictors of outcome in psychodynamic child psychotherapy. Psychotherapy 2021, 58, 81–94. [Google Scholar] [CrossRef]
- Bateman, A.W.; Fonagy, P. Mentalization-based treatment of BPD. J. Pers. Disord. 2004, 18, 36–51. [Google Scholar] [CrossRef] [Green Version]
- Luyten, P.; Van Houdenhove, B.; Lemma, A.; Target, M.; Fonagy, P. A mentalization-based approach to the understanding and treatment of functional somatic disorders. Psychoanal. Psychother. 2012, 26, 121–140. [Google Scholar] [CrossRef]
- Fonagy, P.; Luyten, P.; Moulton-Perkins, A.; Lee, Y.-W.; Warren, F.; Howard, S.; Ghinai, R.; Fearon, R.; Lowyck, B. Development and validation of a self-report measure of mentalizing: The reflective functioning questionnaire. PLoS ONE 2016, 11, e0158678. [Google Scholar] [CrossRef]
- Sharp, C.; Venta, A. Mentalizing Problems in Children and Adolescents. In Minding the Child: Mentalization-Based Interventions with Children, Young People and Their Families; Midgley, N., Vrouva, I., Eds. Routledge: London, UK, 2013. [Google Scholar]
- Fonagy, P.; Bateman, A.W. Adversity, attachment, and mentalizing. Compr. Psychiatry 2016, 64, 59–66. [Google Scholar] [CrossRef]
- Ballespí, S.; Vives, J.; Sharp, C.; Tobar, A.; Barrantes-Vidal, N. Hypermentalizing in social anxiety: Evidence for a context-dependent relationship. Front. Psychol. 2019, 10, 1501. [Google Scholar] [CrossRef]
- Sharp, C. The Social–Cognitive Basis of BPD: A Theory of hypermentalizing. In Handbook of Borderline Personality Disorder in Children and Adolescents; Springer Science and Business Media LLC: Berlin, Germany, 2014; pp. 211–225. [Google Scholar]
- Michelozzi, P.; De’Donato, F.; Scortichini, M.; De Sario, M.; Noccioli, F.; Rossi, P.; Davoli, M. Mortality impacts of the coronavirus disease (COVID-19) outbreak by sex and age: Rapid mortality surveillance system, Italy, 1 February to 18 April 2020. Eurosurveillance 2020, 25, 2000620. [Google Scholar] [CrossRef]
- Bottesi, G.; Ghisi, M.; Altoè, G.; Conforti, E.; Melli, G.; Sica, C. The italian version of the depression anxiety stress scales-21: Factor structure and psychometric properties on community and clinical samples. Compr. Psychiatry 2015, 60, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M.; Rescorla, L.A. The achenbach system of empirically based assessment (ASEBA) for ages 1.5 to 18 years. In The Use of Psychological Testing for Treatment Planning and Outcomes Assessment; Routledge: Oxfordshire, UK, 2014; pp. 179–214. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows; Version 24.0; Armonk, IBM Corp.: New York, NY, USA, 2016. [Google Scholar]
- Hayes, A.F. PROCESS: A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling. 2012. [Google Scholar]
- Carden, S.W.; Holtzman, N.S.; Strube, M.J. CAHOST: An excel workbook for facilitating the johnson-neyman technique for two-way interactions in multiple regression. Front. Psychol. 2017, 8, 1293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, D.J.; Curran, P.J. Probing Interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivar. Behav. Res. 2005, 40, 373–400. [Google Scholar] [CrossRef] [PubMed]
- Cluver, L.; Lachman, J.M.; Sherr, L.; Wessels, I.; Krug, E.; Rakotomalala, S.; Blight, S.; Hillis, S.; Bachman, G.; Green, O.; et al. Parenting in a time of COVID-19. Lancet 2020, 395, e64. [Google Scholar] [CrossRef]
- Cava, M.A.; Fay, K.E.; Beanlands, H.J.; McCay, E.A.; Wignall, R. Risk perception and compliance with quarantine during the SARS outbreak. J. Nurs. Sch. 2005, 37, 343–347. [Google Scholar] [CrossRef]
- Pirutinsky, S.; Cherniak, A.D.; Rosmarin, D.H. COVID-19, mental health, and religious coping among American orthodox Jews. J. Relig. Health 2020, 59, 2288–2301. [Google Scholar] [CrossRef]
- Petrocchi, S.; Bernardi, S.; Malacrida, R.; Traber, R.; Gabutti, L.; Grignoli, N. Affective empathy predicts self-isolation behaviour acceptance during coronavirus risk exposure. Sci. Rep. 2021, 11, 10153. [Google Scholar] [CrossRef]
- Di Giuseppe, M.; Zilcha-Mano, S.; Prout, T.A.; Perry, J.C.; Orrù, G.; Conversano, C. Psychological impact of Coronavirus Disease 2019 among italians during the first week of lockdown. Front. Psychiatry 2020, 11, 576597. [Google Scholar] [CrossRef] [PubMed]
- Ye, B.; Zeng, Y.; Im, H.; Liu, M.; Wang, X.; Yang, Q. The relationship between fear of COVID-19 and online aggressive behavior: A moderated mediation model. Front. Psychol. 2021, 12, 589615. [Google Scholar] [CrossRef] [PubMed]
- Larsen, R.J. Toward a science of mood regulation. Psychol. Inq. 2000, 11, 129–141. [Google Scholar] [CrossRef]
- Zillmann, D.; Johnson, R.C.; Day, K.D. Attribution of apparent arousal and proficiency of recovery from sympathetic activation affecting excitation transfer to aggressive behavior. J. Exp. Soc. Psychol. 1974, 10, 503–515. [Google Scholar] [CrossRef]
- Eisenberg, N.; Losoya, S.; Fabes, R.A.; Guthrie, I.K.; Reiser, M.; Murphy, B.; Shepard, S.A.; Poulin, R.; Padgett, S.J. Parental socialization of children’s dysregulated expression of emotion and externalizing problems. J. Fam. Psychol. 2001, 15, 183–205. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P.; Gergely, G.; Target, M. The parent-infant dyad and the construction of the subjective self. J. Child Psychol. Psychiatry 2007, 48, 288–328. [Google Scholar] [CrossRef]
- Stein, A.; Lehtonen, A.; Harvey, A.G.; Nicol-Harper, R.; Craske, M. The influence of postnatal psychiatric disorder on child development. Psychopathology 2008, 42, 11–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, X.; Spinrad, T.L.; Cookston, J.T.; Matsumoto, D. The relations of parental emotion dysregulation and emotion socialization to young adults’ emotion dysregulation. J. Child Fam. Stud. 2020, 29, 725–737. [Google Scholar] [CrossRef]
- Sharp, C.; Tackett, J.L. Introduction: An idea whose time has come. In Handbook of Borderline Personality Disorder in Children and Adolescents; Springer Science and Business Media LLC: Berlin, Germany, 2014; pp. 3–8. [Google Scholar]
- Petrocchi, S.; Iannello, P.; Ongaro, G.; Antonietti, A.; Pravettoni, G. The interplay between risk and protective factors during the initial height of the COVID-19 crisis in Italy: The role of risk aversion and intolerance of ambiguity on distress. Curr. Psychol. 2021, 1–12. [Google Scholar] [CrossRef]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Fergus, T.A.; McKay, D.; Asmundson, G.J.G. COVID stress syndrome: Concept, structure, and correlates. Depression Anxiety 2020, 37, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Bak, P.L. Thoughts in mind: Promoting mentalizing communities for children. In Minding the Child: Mentalization-Based Interventions with Children, Young People and Their Families; Vrouva, I., Midgley, N., Eds.; Routledge: London, UK, 2012; pp. 202–218. [Google Scholar]
- Valle, A.; Massaro, D.; Castelli, I.; Intra, F.S.; Lombardi, E.; Bracaglia, E.A.; Marchetti, A. Promoting mentalizing in pupils by acting on teachers: Preliminary italian evidence of the “Thought in Mind” Project. Front. Psychol. 2016, 7, 1213. [Google Scholar] [CrossRef] [Green Version]
| Psychological Variables | M (SD) | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Maternal COVID-19 exposure | 0.66 (1.1) | 0.159 ** | 0.064 | 0.213 *** | 0.106 | 0.273 *** | 0.043 | 0.076 | 0.055 | 0.010 | 0.043 |
| Maternal Distress (1) | 1.58 (.37) | 0.347 *** | 0.489 *** | 0.428 *** | 0.281 *** | −0.049 | 0.073 | −0.035 | −0.079 | 0.064 | |
| Maternal hypermentalization (2) | 0.57 (0.58) | 0.406 *** | 0.344 *** | 0.236 *** | −0.004 | 0.132 ** | 0.031 | −0.071 | −0.155 ** | ||
| Child’s anxious/depressed problems (3) | 58.72 (7.9) | 0.528 *** | 0.442 *** | 0.015 | 0.217 *** | 0.012 | −0.063 | 0.020 | |||
| Child’s attention problems (4) | 55.97 (7.1) | 0.507 *** | −0.092 | −0.042 | −0.038 | −0.081 | -0.014 | ||||
| Child’s aggressive behaviors (5) | 66.11 (14.9) | −0.138 * | 0.056 | −0.097 | −0.090 | 0.174 | |||||
| Child’s age (6) | 10.3 (2.4) | −0.10 * | 0.139 * | 0.394 ** | −0.059 | ||||||
| Child’s gender (7) | 0.088 | −0.067 | −0.056 | ||||||||
| Family size (8) | 2 (0.5) | −0.010 | −0.065 | ||||||||
| Maternal age (9) | 41.9 (5.26) | 0.129 * | |||||||||
| Maternal educational level (10) | - |
| Variables | Maternal Distress | Children’s Anxious/Depressed Problems | ||||
|---|---|---|---|---|---|---|
| β | SE | [95% CI] | β | SE | [95% CI] | |
| Constant | 0.120 | 0.122 | [−0.12; 0.36] | 53.419 *** | 2.390 | [48.71; 58.12] |
| Children’s age | −0.007 | 0.008 | [−0.02; 0.01] | 0.152 | 0.160 | [−0.16; 0.47] |
| Children’s gender | 0.013 | 0.039 | [−0.64; 0.09] | 2.746 ** | 0.767 | [1.24; 4.26] |
| Family size | −0.033 | 0.036 | [−0.10; 0.04] | −0.24 | 0.699 | [−1.62; 1.14] |
| Maternal COVID-19 exposure | 0.061 ** | 0.017 | [0.03; 0.09] | 0.78 * | 0.342 | [0.10; 1.45] |
| Maternal hypermentalization | 0.221 *** | 0.034 | [0.15; 0.29] | 3.212 *** | 0.730 | [1.77; 4.65] |
| Maternal COVID-19 exposure X Maternal hypermentalization | 0.030 | 0.026 | [−0.02; 0.08] | −1.08 * | 0.527 | [−2.12; −0.04] |
| Maternal distress | - | - | - | 7.612 *** | 1.194 | [5.26; 9.96] |
| Maternal distress X maternal hypermentalization | - | - | - | 1.868 | 1.581 | [−1.24; 4.98] |
| F | (6, 297) = 1.369 *** | (8, 295) = 19.754 *** | ||||
| R2 | 0.19 | 0.35 | ||||
| Variables | Maternal Distress | Children’s Attention Problems | ||||
|---|---|---|---|---|---|---|
| β | SE | [95% CI] | β | SE | [95% CI] | |
| Constant | 0.120 | 0.122 | [−0.12; 0.36] | 60.449 *** | 2.27 | [55.97; 64.92] |
| Children’s age | −0.007 | 0.008 | [−0.02; 0.01] | −0.274 | 0.152 | [−0.57; 0.02] |
| Children’s gender | 0.011 | 0.039 | [−0.06; 0.09] | −0.843 | 0.729 | [−2.28; 0.59] |
| Family size | −0.033 | 0.035 | [−0.10; 0.04] | −0.391 | 0.665 | [−1.70; 0.92] |
| Maternal COVID-19 exposure | 0.061 ** | 0.017 | [0.03; 0.09] | 0.173 | 0.325 | [−0.47; 0.81] |
| Maternal hypermentalization | 0.220 *** | 0.340 | [0.15; 0.29] | 2.158 ** | 0.694 | [0.79; 3.52] |
| Maternal COVID-19 exposure X Maternal hypermentalization | 0.031 | 0.026 | [−0.02; 0.08] | −0.511 | 0.502 | [−1.498; 0.477] |
| Maternal distress | − | − | − | 5.244 *** | 1.135 | [3.01; 7.48] |
| Maternal distress X Maternal hypermentalization | − | − | − | 5.617 *** | 1.504 | [2.66; 8.58] |
| F | (6, 298) = 11.350 *** | (8, 296) = 13.499 *** | ||||
| R2 | 0.19 | 0.27 | ||||
| Variables | Maternal Distress | Children’s Aggressive Problems | ||||
|---|---|---|---|---|---|---|
| β | SE | [95% CI] | β | SE | [95% CI] | |
| Constant | 0.121 | 0.122 | [−0.12; 0.36] | 77.885 *** | 4.983 | [66.08; 87.69] |
| Children’s age | −0.007 | 0.008 | [−0.02; 0.01] | −0.820 * | 0.334 | [−1.48; −0.16] |
| Children’s gender | 0.012 | 0.039 | [−0.06; 0.09] | 0.873 | 1.597 | [−2.27; 4.02] |
| Family size | −0.033 | 0.036 | [−0.10; 0.04] | −2.766 | 1.459 | [−5.64; 0.10] |
| Maternal COVID-19 exposure | 0.061 *** | 0.017 | [0.03; 0.09] | 2.276 *** | 0.713 | [0.87; 3.68] |
| Maternal hypermentalization | 0.221 *** | 0.034 | 0.15; 0.29] | 2.412 | 1.522 | [−0.58; 5.41] |
| Maternal COVID-19 exposure X Maternal hypermentalization | 0.031 | 0.026 | [−0.02; 0.08] | 0.690 | 1.099 | [−1.47; 2.85] |
| Maternal distress | - | - | - | 3.774 | 2.487 | [−1.12; 8.67] |
| Maternal distress X Maternal hypermentalization | - | - | - | 12.226 *** | 3.295 | [5.74; 18.71] |
| F | (6, 298) = 11.350 *** | (8, 296) = 9.074 *** | ||||
| R2 | 0.19 | 0.20 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bianco, F.; Levante, A.; Petrocchi, S.; Lecciso, F.; Castelli, I. Maternal Psychological Distress and Children’s Internalizing/Externalizing Problems during the COVID-19 Pandemic: The Moderating Role Played by Hypermentalization. Int. J. Environ. Res. Public Health 2021, 18, 10450. https://doi.org/10.3390/ijerph181910450
Bianco F, Levante A, Petrocchi S, Lecciso F, Castelli I. Maternal Psychological Distress and Children’s Internalizing/Externalizing Problems during the COVID-19 Pandemic: The Moderating Role Played by Hypermentalization. International Journal of Environmental Research and Public Health. 2021; 18(19):10450. https://doi.org/10.3390/ijerph181910450
Chicago/Turabian StyleBianco, Federica, Annalisa Levante, Serena Petrocchi, Flavia Lecciso, and Ilaria Castelli. 2021. "Maternal Psychological Distress and Children’s Internalizing/Externalizing Problems during the COVID-19 Pandemic: The Moderating Role Played by Hypermentalization" International Journal of Environmental Research and Public Health 18, no. 19: 10450. https://doi.org/10.3390/ijerph181910450
APA StyleBianco, F., Levante, A., Petrocchi, S., Lecciso, F., & Castelli, I. (2021). Maternal Psychological Distress and Children’s Internalizing/Externalizing Problems during the COVID-19 Pandemic: The Moderating Role Played by Hypermentalization. International Journal of Environmental Research and Public Health, 18(19), 10450. https://doi.org/10.3390/ijerph181910450








