Teamworking in Healthcare during the COVID-19 Pandemic: A Mixed-Method Study
Abstract
:1. Introduction
1.1. Theoretical Approaches
1.2. Hypotheses
2. Materials and Methods
2.1. Design, Participants and Recruitment Strategy
2.2. Materials
2.2.1. Collective Leadership
2.2.2. Utrecht Work Engagement
2.2.3. Organisational Citizenship Behaviour
2.2.4. Psychological Safety
2.2.5. Open-Ended Questions
2.2.6. Covariates
2.3. Data Analysis
2.3.1. Quantitative Data
2.3.2. Qualitative Data
3. Results
3.1. Descriptive Statistics
3.2. Measurement Model
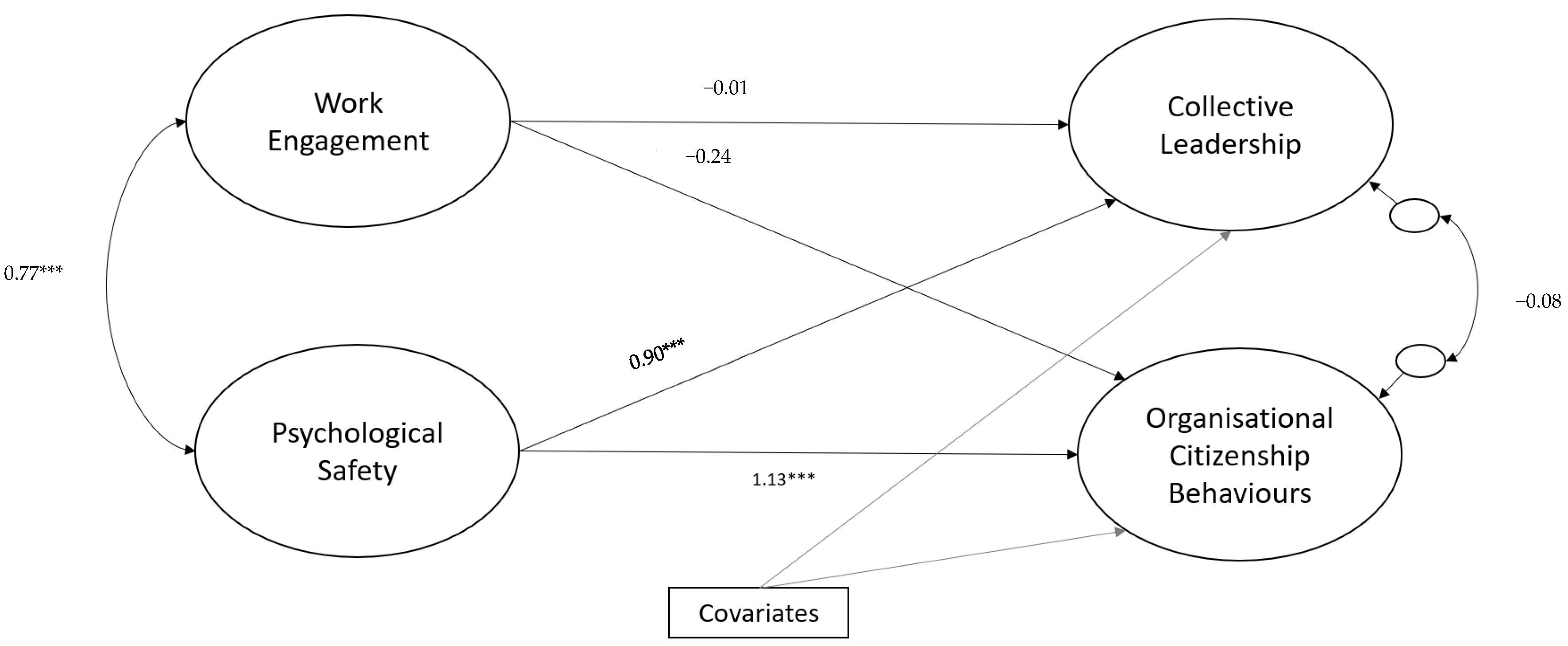
Structural Model
3.3. Qualitative Findings
3.3.1. Contrasting Experiences of Working in a Team during the Pandemic
3.3.2. The Pandemic Response: A Tipping Point for Burnout
4. Discussion
4.1. Theoretical and Practical Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| What, if any, is the most significant change you’ve observed in how your healthcare colleagues are working during the COVID-19 response? |
| Has it been a positive change or a negative change? |
| What has been the impact of this change? |
| What do you think has changed in people’s mind to enable this way of working? |
| Do you think this change will persist after COVID-19? What makes you say this? |
| Was there anything about how your team worked during COVID-19 that you felt unhappy about? Please describe. |
| What aspect/s of how your team worked during COVID-19 would you like to see continue? |
| What do you think would enable your team to sustain these ways of working? |
Appendix B
| Latent Variable | β (SE) |
|---|---|
| Factor loadings | |
| Work engagement | |
| Vigour | 0.96 (0.02) |
| Dedication | 0.87 (0.05) |
| Absorption | 0.82 (0.05) |
| Psychological safety | |
| Team leader | 0.80 (0.05) |
| Team members | 0.93 (0.02) |
| Whole team | 0.92 (0.02) |
| Collective leadership | |
| Planning and organising | 0.96 (0.01) |
| Problem solving | 0.97 (0.01) |
| Support and consideration | 0.92 (0.02) |
| Organisational citizenship behaviours | |
| Altruism | 0.93 (0.02) |
| Courtesy | 0.93 (0.03) |
| Civic virtue | 0.78 (0.05) |
| Variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| – | |||
| 0.77 *** | – | ||
| 0.68 *** | 0.85 *** | – | |
| 0.68 *** | 0.94 *** | 0.84 *** | – |
References
- Wensing, M.; Sales, A.; Armstrong, R.; Wilson, P. Implementation science in times of Covid-19. Implement. Sci. 2020, 15, 1–4. [Google Scholar] [CrossRef]
- Balas, E.; Boren, S. Managing Clinical Knowledge for Health Care Improvement. Yearb. Med. Inform. 2000, 9, 65–70. [Google Scholar] [CrossRef] [Green Version]
- Bauer, M.S.; Damschroder, L.J.; Hagedorn, H.; Smith, J.; Kilbourne, A.M. An introduction to implementation science for the non-specialist. BMC Psychol. 2015, 3, 32. [Google Scholar] [CrossRef] [Green Version]
- Fitzsimons, J. Quality and safety in the time of Coronavirus: Design better, learn faster. Int. J. Qual. Health Care 2020, 33. [Google Scholar] [CrossRef]
- Ní Shé, É.; O’Donnell, D.; O’Shea, M.; Stokes, D. New ways of working? A rapid exploration of emerging evidence regarding the care of older people during COVID19. Int. J. Environ. Res. Public Health 2020, 17, 6442. [Google Scholar] [CrossRef]
- Bailey, S.; West, M. Learning from Staff Experiences of Covid-19: Let the Light come Streaming in: The King’s Fund; 2020. Available online: https://www.kingsfund.org.uk/blog/2020/06/learning-staff-experiences-covid-19 (accessed on 1 April 2021).
- Slater, B. Lessons from Implementation-after the Crisis, What Then? 2020. Available online: https://sites.google.com/nihr.ac.uk/arc-yh/news-events-and-media/blogs/blog-9-beverley-slater (accessed on 1 April 2021).
- Wu, Q.; Cormican, K.; Chen, G. A Meta-Analysis of Shared Leadership: Antecedents, Consequences, and Moderators. J. Leadersh. Organ. Stud. 2018, 27, 49–64. [Google Scholar] [CrossRef]
- De Brún, A.; O’Donovan, R.; McAuliffe, E. Interventions to develop collectivistic approaches to leadership in healthcare settings: A systematic review. BMC Health Serv. Res. 2019, 19, 72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carson, J.B.; Tesluk, P.E.; Marrone, J.A. Shared leadership in teams: An investigation of antecedent conditions and performance. Acad. Manag. J. 2007, 50, 1217–1234. [Google Scholar]
- Fausing, M.S.; Joensson, T.S.; Lewandowski, J.; Bligh, M.C. Antecedents of shared leadership: Empowering leadership and interdependence. Leadersh. Organ. Dev. J. 2015, 36, 271–291. [Google Scholar] [CrossRef]
- Grille, A.; Schulte, E.-M.; Kauffeld, S. Promoting shared leadership: A multilevel analysis investigating the role of prototypical team leader behavior, psychological empowerment, and fair rewards. J. Leadersh. Organ. Stud. 2015, 22, 324–339. [Google Scholar] [CrossRef]
- Nembhard, I.M.; Edmondson, A.C. Making it safe: The effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J. Organ. Behav. 2006, 27, 941–966. [Google Scholar] [CrossRef]
- Edmondson, A. Psychological Safety and Learning Behavior in Work Teams. Adm. Sci. Q. 1999, 44, 350–383. [Google Scholar] [CrossRef] [Green Version]
- Newman, A.; Donohue, R.; Eva, N. Psychological safety: A systematic review of the literature. Hum. Resour. Manag. Rev. 2017, 27, 521–535. [Google Scholar] [CrossRef]
- De Brún, A.; McAuliffe, E. Identifying the context, mechanisms and outcomes underlying collective leadership in teams: Building a realist programme theory. BMC Health Serv. Res. 2020, 20, 261. [Google Scholar] [CrossRef] [PubMed]
- Kahn, W.A. Psychological conditions of personal engagement and disengagement at work. Acad. Manag. J. 1990, 33, 692–724. [Google Scholar]
- Christian, M.S.; Garza, A.S.; Slaughter, J.E. Work Engagement: A Quantitative Review and Test Of Its Relations With Task and Contextual Performance. Personal. Psychol. 2011, 64, 89–136. [Google Scholar] [CrossRef] [Green Version]
- Schaufeli, W.B.; Salanova, M.; González-Romá, V.; Bakker, A.B. The Measurement of Engagement and Burnout: A Two Sample Confirmatory Factor Analytic Approach. J. Happiness Stud. 2002, 3, 71–92. [Google Scholar] [CrossRef]
- Frazier, M.L.; Fainshmidt, S.; Klinger, R.L.; Pezeshkan, A.; Vracheva, V. Psychological Safety: A Meta-Analytic Review and Extension. Personal. Psychol. 2016, 70, 113–165. [Google Scholar] [CrossRef] [Green Version]
- May, D.R.; Gilson, R.L.; Harter, L.M. The psychological conditions of meaningfulness, safety and availability and the engagement of the human spirit at work. J. Occup. Organ. Psychol. 2004, 77, 11–37. [Google Scholar] [CrossRef]
- Bakker, A.B.; Albrecht, S. Work engagement: Current trends. Career Dev. Int. 2018, 23, 4–11. [Google Scholar] [CrossRef]
- Breevaart, K.; Bakker, A.; Hetland, J.J.; Demerouti, E.E.; Olsen, O.K.; Espevik, R. Daily transactional and transformational leadership and daily employee engagement. J. Occup. Organ. Psychol. 2013, 87, 138–157. [Google Scholar] [CrossRef]
- Ghadi, M.Y.; Fernando, M.; Caputi, P. Transformational leadership and work engagement: The mediating effect of meaning in work. Leadersh. Organ. Dev. J. 2013, 34, 532–550. [Google Scholar] [CrossRef]
- Organ, D.W. Organizational Citizenship Behavior: The Good Soldier Syndrome; Lexington Books/DC Heath and Com: Lexinton, MA, USA, 1988. [Google Scholar]
- Podsakoff, P.M.; MacKenzie, S.B.; Paine, J.B.; Bachrach, D.G. Organizational citizenship behaviors: A critical review of the theoretical and empirical literature and suggestions for future research. J. Manag. 2000, 26, 513–563. [Google Scholar] [CrossRef]
- Hiller, N.J.; Day, D.V.; Vance, R.J. Collective enactment of leadership roles and team effectiveness: A field study. Leadersh. Q. 2006, 17, 387–397. [Google Scholar] [CrossRef]
- Seppälä, P.; Mauno, S.; Feldt, T.; Hakanen, J.; Kinnunen, U.; Tolvanen, A.; Schaufeli, W. The Construct Validity of the Utrecht Work Engagement Scale: Multisample and Longitudinal Evidence. J. Happiness Stud. 2008, 10, 459–481. [Google Scholar] [CrossRef] [Green Version]
- Podsakoff, P.M.; MacKenzie, S.B.; Moorman, R.; Fetter, R. The impact of transformational leader behaviors on employee trust, satisfaction, and organizational citizenship behaviors. Leadersh. Q. 1990, 1, 107–142. [Google Scholar] [CrossRef]
- O’Donovan, R.; van Dun, D.; McAuliffe, E. Measuring psychological safety in healthcare teams: Developing an observational measure to complement survey methods. BMC Med. Res. Methodol. 2020, 20, 203. [Google Scholar] [CrossRef]
- VanderWeele, T.J. Principles of confounder selection. Eur. J. Epidemiol. 2019, 34, 211–219. [Google Scholar] [CrossRef] [Green Version]
- Bollen, K.A. Structural Equations with Latent Variables; John Wiley & Sons: Hoboken, NJ, USA, 1989. [Google Scholar]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411. [Google Scholar] [CrossRef]
- Hu Lt Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef]
- Tucker, L.R.; Lewis, C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika 1973, 38, 1–10. [Google Scholar] [CrossRef]
- Steiger, J.H. Structural Model Evaluation and Modification: An Interval Estimation Approach. Multivar. Behav. Res. 1990, 25, 173–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jöreskog, K.G.; Sörbom, D. LISREL V: Analysis of Linear Structural Relationships by Maximum Likelihood and Least Squares Methods; International Education Services: Chicago, IL, USA, 1981. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2018. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Shi, D.; Lee, T.; Maydeu-Olivares, A. Understanding the Model Size Effect on SEM Fit Indices. Educ. Psychol. Meas. 2018, 79, 310–334. [Google Scholar] [CrossRef] [PubMed]
- Deegan, J., Jr. On the occurrence of standardized regression coefficients greater than one. Educ. Psychol. Meas. 1978, 38, 873–888. [Google Scholar] [CrossRef]
- Jöreskog, K.G. How Large Can a Standardized Coefficient Be. 1999. Available online: http://www.statmodel.com/download/Joreskog.pdf (accessed on 1 April 2021).
- Roberto, M.A. Lessons from Everest: The Interaction of Cognitive Bias, Psychological Safety, and System Complexity. Calif. Manag. Rev. 2002, 45, 136–158. [Google Scholar] [CrossRef]
- Schulte, M.; Cohen, N.A.; Klein, K.J. The Coevolution of Network Ties and Perceptions of Team Psychological Safety. Organ. Sci. 2012, 23, 564–581. [Google Scholar] [CrossRef] [Green Version]
- Carmeli, A.; Reiter-Palmon, R.; Ziv, E. Inclusive Leadership and Employee Involvement in Creative Tasks in the Workplace: The Mediating Role of Psychological Safety. Creat. Res. J. 2010, 22, 250–260. [Google Scholar] [CrossRef]
- O’Donovan, R.; De Brún, A.; McAuliffe, E. Healthcare Professionals Experience of Psychological Safety, Voice, and Silence. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef]
- Eppich, W.J.; Schmutz, J.B. From ‘them’ to ‘us’: Bridging group boundaries through team inclusiveness. Med. Educ. 2019, 53, 756–758. [Google Scholar] [CrossRef]
- Organ, D.W.; Ryan, K. A Meta-Analytic Review of Attitudinal and Dispositional Predictors of Organizational Citizenship Behavior. Personal. Psychol. 1995, 48, 775–802. [Google Scholar] [CrossRef]
- Mäkikangas, A.; Feldt, T.; Kinnunen, U.; Mauno, S. Does Personality Matter? A Review of Individual Differences in Occupational Well-Being. In Advances in Positive Organizational Psychology; Emerald Group Publishing Limited: Bingley, UK, 2013; pp. 107–143. [Google Scholar] [CrossRef]
- Wendt, H.; Euwema, M.; van Emmerik, I.H. Leadership and team cohesiveness across cultures. Leadersh. Q. 2009, 20, 358–370. [Google Scholar] [CrossRef] [Green Version]
- Friedrich, T.L.; Vessey, W.B.; Schuelke, M.J.; Ruark, G.A.; Mumford, M.D. A Framework for Understanding Collective Leadership: The Selective Utilization of Leader and Team Expertise within Networks. Leadersh. Q. 2009, 20, 933–958. [Google Scholar] [CrossRef] [Green Version]
- O’Donovan, R.; McAuliffe, E. Exploring psychological safety in healthcare teams to inform the development of interventions: Combining observational, survey and interview data. BMC Health Serv. Res. 2020, 20, 810. [Google Scholar] [CrossRef]
| Sample Characteristic | % (n) | Mean (95% CI) | Median | SD | Range |
|---|---|---|---|---|---|
| Age | |||||
| 18–29 | 3.9 (3) | ||||
| 30–39 | 23.7 (18) | ||||
| 40–49 | 41.1 (32) | ||||
| 50–59 | 28.9 (22) | ||||
| 60+ | 1.3 (1) | ||||
| Sex | |||||
| Female | 84.0 (63) | ||||
| Male | 16.0 (12) | ||||
| Self-Reported Ethnicity | |||||
| White Irish | 75.0 (57) | ||||
| Ethnicity other than White Irish | 25.0 (19) | ||||
| Redeployed | |||||
| Yes | 31.6 (24) | ||||
| No | 68.4 (52) | ||||
| Work engagement | 88.95 (84.52/93.39) | 92.20 | 18.03 | 17–116 | |
| Psychological safety | 95.61 (88.31/102.90) | 108.00 | 29.68 | 19–132 | |
| Collective leadership | 93.83 (86.84/100.83) | 101.50 | 28.46 | 19–131 | |
| Organisational citizenship behaviours | 69.88 (65.04/74.72) | 74.50 | 19.67 | 14–97 | |
| Time employed in healthcare (years) | 19.61 (17.39/21.83) | 20.25 | 9.02 | 1.75–40.08 |
| Collective Leadership | Organisational Citizenship Behaviours | |||
|---|---|---|---|---|
| B (SE) | β (SE) | B (SE) | β (SE) | |
| Latent variables | ||||
| Work engagement | −0.02 (0.16) | −0.01 (0.14) | −15 (0.08) | −0.24 (0.13) |
| Psychological safety | 0.81 *** (0.13) | 0.90 (0.12) | 0.53 *** (0.08) | 1.13 (0.10) |
| Covariates | ||||
| Age (18–39 years) | ||||
| 40–49 years | −0.10 (1.54) | −0.01 (0.10) | 1.19 (0.74) | 0.14 (0.09) |
| 50 years and above | −1.44 (1.77) | −0.08 (0.11) | 1.50 (0.81) | 0.17 (0.09) |
| Sex a | 0.43 (1.42) | 0.02 (0.07) | −0.35 (0.56) | −0.03 (0.05) |
| Self-reported ethnicity b | −5.60 *** (1.31) | −0.31 (0.08) | −2.35 *** (0.62) | −0.25 (0.06) |
| Time employed in healthcare | −0.01 (0.09) | −0.01 (0.11) | −0.06 (0.04) | −0.12 (0.09) |
| Being redeployed | 0.64 (1.15) | 0.04 (0.07) | 0.30 (0.62) | 0.03 (0.07) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anjara, S.; Fox, R.; Rogers, L.; De Brún, A.; McAuliffe, E. Teamworking in Healthcare during the COVID-19 Pandemic: A Mixed-Method Study. Int. J. Environ. Res. Public Health 2021, 18, 10371. https://doi.org/10.3390/ijerph181910371
Anjara S, Fox R, Rogers L, De Brún A, McAuliffe E. Teamworking in Healthcare during the COVID-19 Pandemic: A Mixed-Method Study. International Journal of Environmental Research and Public Health. 2021; 18(19):10371. https://doi.org/10.3390/ijerph181910371
Chicago/Turabian StyleAnjara, Sabrina, Robert Fox, Lisa Rogers, Aoife De Brún, and Eilish McAuliffe. 2021. "Teamworking in Healthcare during the COVID-19 Pandemic: A Mixed-Method Study" International Journal of Environmental Research and Public Health 18, no. 19: 10371. https://doi.org/10.3390/ijerph181910371
APA StyleAnjara, S., Fox, R., Rogers, L., De Brún, A., & McAuliffe, E. (2021). Teamworking in Healthcare during the COVID-19 Pandemic: A Mixed-Method Study. International Journal of Environmental Research and Public Health, 18(19), 10371. https://doi.org/10.3390/ijerph181910371







