Challenges in Documenting Non-Fatal Drowning Disability in Bangladesh: A Community-Based Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Procedures
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Recovery from Non-Fatal Drowning
3.2. Risk Factors for Non-Fatal Drowning
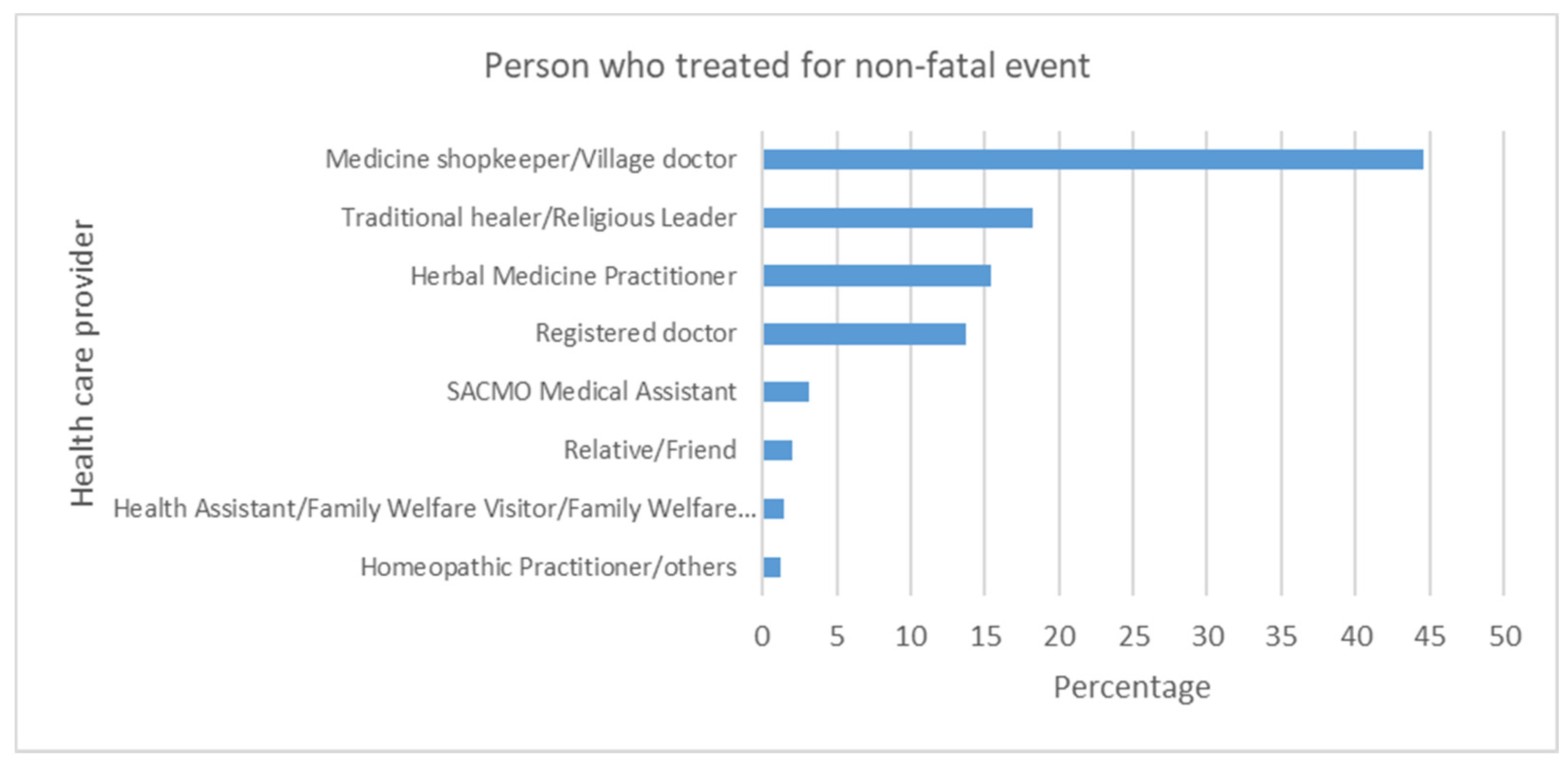
3.3. Care-Seeking Behaviour for Non-Fatal Drowning
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Global Report on Drowning: Preventing a Leading Killer; The World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Rahman, M.A.R.; Shafinaz, S.; Linnan, M. Bangladesh Health and Injury Survey Report on Children; The DGHS: Dhaka, Bangladesh, 2005. [Google Scholar]
- Jagnoor, J.; Bassani, D.; Keay, L.; Ivers, R.Q.; Thakur, J.; Gururaj, G.; Jha, P. Unintentional injury deaths among children younger than 5 years of age in India: A nationally representative study. Inj. Prev. 2011, 17, 151–155. [Google Scholar] [CrossRef] [PubMed]
- WHO; UNICEF. World Report on Child Injury Prevention; World Health Organisation: Geneva, Switzerland, 2008. [Google Scholar]
- Suominen, P.K.; Vähätalo, R. Neurologic long term outcome after drowning in children. Scand. J. Trauma Resusc. Emerg. Med. 2012, 20, 55. [Google Scholar] [CrossRef] [Green Version]
- Ibsen, L.M.; Koch, T. Submersion and asphyxial injury. Crit. Care Med. 2002, 30, S402–S408. [Google Scholar] [CrossRef] [PubMed]
- Peden, M.M.; McGee, K. The epidemiology of drowning worldwide. Inj. Control Saf. Promot. 2003, 10, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Estimates. Available online: http://vizhub.healthdata.org/gbd-compare (accessed on 22 June 2021).
- Mokdad, A.H.; Forouzanfar, M.H.; Daoud, F.; Mokdad, A.A.; El Bcheraoui, C.; Moradi-Lakeh, M.; Kyu, H.H.; Barber, R.M.; Wagner, J.; Cercy, K.; et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2016, 387, 2383–2401. [Google Scholar] [CrossRef]
- Peden, A.E.; Mahony, A.J.; Barnsley, P.D.; Scarr, J. Understanding the full burden of drowning: A retrospective, cross-sectional analysis of fatal and non-fatal drowning in Australia. BMJ Open 2018, 8, e024868. [Google Scholar] [CrossRef]
- Suominen, P.; Sutinen, N.; Valle, S.; Olkkola, K.; Loonqvist, T. Neurocognitive long term follow-up study on drowned children. Resuscitation 2014, 85, 1059–1064. [Google Scholar] [CrossRef]
- Writing Group; Idris, A.H.; Berg, R.A.; Bierens, J.; Bossaert, L.; Branche, C.M.; Gabrielli, A.; Graves, S.A.; Handley, A.J.; Hoelle, R.; et al. Recommended Guidelines for Uniform Reporting of Data From Drowning: The “Utstein Style”. Circulation 2003, 108, 2565–2574. [Google Scholar]
- World Health Organisation; The World Bank. World Report on Disability; The World Health Organisation: Geneva, Switzerland, 2011. [Google Scholar]
- Üstün, T.; Chatterji, S.; Kostanjsek, N.; Rehm, J.; Kennedy, C.; Epping-Jordan, J.; Saxena, S.; von Korff, M.; Pull, C.; WHO/NIH. Joint Project Developing the World Health Organization Disability Assessment Schedule 2.0. Bull. World Health Organ. 2010, 88, 815–823. [Google Scholar] [CrossRef]
- World Health Organisation. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0); World Health Organisation: Geneva, Switzerland, 2010. [Google Scholar]
- Rahman, A.; Jagnoor, J.; Baset, K.U.; Ryan, D.; Ahmed, T.; Rogers, K.; Hossain, M.J.; Ivers, R.; Rahman, A. Vulnerability to fatal drowning among the population in Southern Bangladesh: Findings from a cross-sectional household survey. BMJ Open 2019, 9, e027896. [Google Scholar] [CrossRef] [Green Version]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines; World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- Langley, J.; Brenner, R. What is an injury? Inj. Prev. 2004, 10, 69. [Google Scholar] [CrossRef] [Green Version]
- van Beeck, E.F.; Branche, C.; Szpilman, D.; Modell, J.H.; Bierens, J.J. A new definition of drowning: Towards documentation and prevention of a global public health problem. Bull. World Health Organ. 2005, 83, 853–856. [Google Scholar]
- Rahman, A.; Alonge, O.; Bhuiyan, A.-A.; Agrawal, P.; Salam, S.S.; Talab, A.; Rahman, S.Q.; Hyder, A.A. Epidemiology of Drowning in Bangladesh: An Update. Int. J. Environ. Res. Public Health 2017, 14, 488. [Google Scholar] [CrossRef]
- Yang, L.; Nong, Q.-Q.; Li, C.-L.; Feng, Q.-M.; Lo, S.K. Risk factors for childhood drowning in rural regions of a developing country: A case–control study. Inj. Prev. 2007, 13, 178. [Google Scholar] [CrossRef] [Green Version]
- Clemens, T.; Oporia, F.; Parker, E.M.; Yellman, M.A.; Ballesteros, M.F.; Kobusingye, O. Drowning in Uganda: Examining data from administrative sources. Inj. Prev. 2021. [Google Scholar] [CrossRef] [PubMed]
- Kimber, M.; Rehm, J.; Ferro, M.A. Measurement Invariance of the WHODAS 2.0 in a Population-Based Sample of Youth. PLoS ONE 2015, 10, e0142385. [Google Scholar] [CrossRef]
- Scorza, P.; Stevenson, A.; Canino, G.; Mushashi, C.; Kanyanganzi, F.; Munyanah, M.; Betancourt, T. Validation of the “World Health Organization Disability Assessment Schedule for Children, WHODAS-Child” in Rwanda. PLoS ONE 2013, 8, e57725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suominen, P.; Baillie, C.; Korpela, R.; Rautanen, S.; Ranta, S.; Olkkola, K.T. Impact of age, submersion time and water temperature on outcome in near-drowning. Resuscitation 2002, 52, 247–254. [Google Scholar] [CrossRef]
- Suominen, P.K.; Vähätalo, R.; Sintonen, H.; Haverinen, A.; Roine, R.P. Health-related quality of life after a drowning incident as a child. Resuscitation 2011, 82, 1318–1322. [Google Scholar] [CrossRef]
- Varni, J.W.; Seid, M.; Kurtin, P.S. PedsQL™ 4.0: Reliability and validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in healthy and patient populations. Med. Care 2001, 39, 800–812. [Google Scholar] [CrossRef] [PubMed]
- Jagnoor, J.; Prinja, S.; Christou, A.; Baker, J.; Gabbe, B.; Ivers, R. Health-Related Quality of Life and Function after Paediatric Injuries in India: A Longitudinal Study. Int. J. Environ. Res. Public Health 2017, 14, 1144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Solans, M.; Pane, S.; Estrada, M.D.; Serra-Sutton, V.; Berra, S.; Herdman, M.; Alonso, J.; Rajmil, L. Health-Related Quality of Life Measurement in Children and Adolescents: A Systematic Review of Generic and Disease-Specific Instruments. Value Health 2008, 11, 742–764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ravens-Sieberer, U.; Gosch, A.; Rajmil, L.; Erhart, M.; Bruil, J.; Power, M.; Duer, W.; Auquier, P.; Cloetta, B.; Czemy, L. The KIDSCREEN-52 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Value Health 2008, 11, 645–658. [Google Scholar] [CrossRef] [PubMed]
- Cieza, A.; Sabariego, C.; Anczewska, M.; Ballert, C.; Bickenbach, J.; Cabello, M.; Giovannetti, A.; Kaskela, T.; Mellor, B.; Pitkänen, T. PARADISE 24: A measure to assess the impact of brain disorders on people’s lives. PLoS ONE 2015, 10, e0132410. [Google Scholar] [CrossRef]
- Beerman, S.; Bierens, J.J.L.M.; Clemens, T.; Meddings, D.; Rahman, A.; Szpilman, D. Clarification and Categorization of Non-fatal Drowning A draft Position Statement for review and input by the global drowning community Prepared by the Working Group on Non-fatal Drowning. In Proceedings of the Workshop on Non-Fatal Drowning, Toronto, ON, Canada, 8–9 August 2018. [Google Scholar]
- McConkey, R.; Craig, S.; Kelly, C. The prevalence of intellectual disability: A comparison of national census and register records. Res. Dev. Disabil. 2019, 89, 69–75. [Google Scholar] [CrossRef] [PubMed]
| Variable | Level | % of All NFDs (95% Confidence Limits) |
| Age (years) | 0–4 | 68% (67–70%) |
| 5–9 | 28% (27–30%) | |
| 10–17 | 2% (1–2%) | |
| 18+ | 2% (1–2%) | |
| Gender | Male | 51% (50–53%) |
| Female | 48% (47–50%) | |
| Setting | Rural | 94% (91–96%) |
| Urban | 6% (4–9%) | |
| Monthly household income (taka/month) | 0–7999 | 17% (15–20%) |
| 8000–9999 | 24% (22–27%) | |
| 10,000–11,999 | 19% (17–20%) | |
| 12,000–15,999 | 26% (24–28%) | |
| 16,000+ | 13% (12–15%) | |
| Socioeconomic quintile | 1 (lowest) | 25% (22–27%) |
| 2 | 26% (24–28%) | |
| 3 | 19% (18–21%) | |
| 4 | 17% (15–18%) | |
| 5 (highest) | 14% (12–15%) |
| Male | Female | Rural | Urban | All Persons | |
|---|---|---|---|---|---|
| Age (Years) | Rate per 100,000 (95% CI) | Rate per 100,000 (95% CI) | Rate per 100,000 (95% CI) | Rate per 100,000 (95% CI) | Rate per 100,000 (95% CI) |
| <1 (infant) | 116.4 (23.8–209.0) | 149.4 (35.5–263.4) | 145.3 (58.0–232.6) | 32.6 (0.0–94.7) | 133.0 (53.2–212.8) |
| 1–4 | 6124.2 (5416.6–6831.8) | 5501.2 (4917.3–6085.1) | 6103.2 (5469.2–6737.2) | 3377.7 (2495.2–4260.3) | 5810.8 (5209.9–6411.7) |
| 5–9 | 1806.7 (1581.2–2032.2) | 1868.2 (1601.0–2135.4) | 1905.8 (1672.4–2139.2) | 1217.7 (837.0–1598.5) | 1837.6 (1614.9–2060.4) |
| 10–14 | 65.9 (31.1–100.8) | 127.9 (79.4–176.3) | 97.7 (64.7–130.6) | 91.6 (21.2–162.1) | 97.1 (65.4–128.8) |
| 15–17 | 44.6 (13.8–75.4) | 19.0 (0.0–39.0) | 36.5 (13.5–59.4) | 0 | 32.6 (12.0–53.2) |
| 18–24 | 38.2 (7.3–69.2) | 20.5 (3.6–37.4) | 32.6 (13.5–51.7) | 0 | 28.9 (12.0–45.9) |
| 25–39 | 19.9 (9.0–30.7) | 4.8 (0.0–9.6) | 13.5 (6.7–20.3) | 0.9 (0.0–2.5) | 12.1 (6.1–18.1) |
| 40–59 | 32.1 (13.9–50.3) | 5.9 (0.3–11.6) | 20.5 (10.1–31.0) | 5.8 (0.0–14.1) | 18.9 (9.6–28.3) |
| 60+ | 17.0 (4.4–29.5) | 8.7 (0.0–19.0) | 12.7 (4.1–21.2) | 13.9 (0.0–33.7) | 12.8 (5.0–20.6) |
| Total | 728.8 (644.0–813.6) | 665.6 (592.7–738.5) | 731.9 (653.5–810.2) | 405.2 (300.4–510.1) | 696.7 (622.0–771.4) |
| WHODAS Questions | Weighted Frequency | Mean (SE) | 95% CI |
|---|---|---|---|
| Overall, in the past 30 days, how many days were these difficulties present? | 4859 | 2.4 (0.4) | 1.6, 3.2 |
| In the past 30 days, for how many days were you totally unable to carry out your usual activities or work because of any health condition? | 4866 | 2.2 (0.4) | 1.4, 3.0 |
| In the past 30 days, not counting the days that you were totally unable, for how many days did you cut back or reduce your usual activities or work because of any health condition? | 4702 | 1.7 (0.3) | 1.1, 2,4 |
| WHODAS Items | No Difficulty | Mild Difficulty | Moderate Difficulty | Severe Difficulty | Extreme Difficulty | Not Applicable |
|---|---|---|---|---|---|---|
| In the Past 30 Days… | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| Standing for long periods such as 30 min | 3626 (72.9) | 606 (12.2) | 71 (1.4) | 19 (0.4) | - | 654 (13.1) |
| Difficulty in taking care of household responsibilities | 2177 (43.8) | 123 (2.5) | 43 (0.9) | 4 (0.1) | 27 (0.5) | 2600 (52.3) |
| Difficulty in concentrating on doing something for ten minutes | 2875 (57.9) | 415 (8.4) | 108 (2.2) | 46 (0.9) | 3 (0.1) | 1519 (30.6) |
| Difficulty in joining in community activities (for example, festivities, religious or other activities) | 2644 (53.2) | 147 (3.0) | 45 (0.9) | 10 (0.2) | 1 (<0.001) | 2123 (42.7) |
| Difficulty in emotionally affected by your health problems | 2690 (54.1) | 662 (13.3) | 186 (3.7) | 71 (1.4) | 2 (<0.001) | 1363 (27.4) |
| Difficulty in concentrating on doing something for ten minutes | 2834 (57.1) | 483 (9.7) | 92 (1.9) | 53 (1.1) | 1 (<0.001) | 1504 (30.3) |
| Difficulty in walking a long distance such as a kilometre | 2839 (57.1) | 462 (9.3) | 112 (2.3) | 36 (0.7) | 1 (<0.001) | 1518 (30.6) |
| Difficulty in washing your whole body | 3138 (63.1) | 318 (6.4) | 55 (1.1) | 40 (0.8) | 3 (0.1) | 1418 (28.5) |
| Difficulty have you/the injured household member had in getting dressed | 3250 (65.5) | 201 (4.0) | 35 (0.7) | 25 (0.5) | 3 (0.1) | 1450 (29.2) |
| Difficulty in dealing with people you do not know | 2902 (58.4) | 314 (6.3) | 44 (0.9) | 15 (0.3) | 1 (<0.001) | 1692 (34.1) |
| Difficulty in maintaining a friendship | 2986 (60.1) | 357 (7.2) | 72 (1.4) | 17 (0.3) | 2 (<0.001) | 1533 (30.9) |
| Difficulty in your day-to-day work/school | 2809 (56.6) | 436 (8.8) | 161 (3.2) | 115 (2.3) | 2 (<0.001) | 1436 (29.0) |
| Univariate Analyses | Multivariable | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||
| Gender | ||||||||
| Female | reference | reference | ||||||
| Male | 1.095 | 1.019 | 1.177 | 0.0134 | 1.079 | 1.000 | 1.165 | 0.0508 |
| Age | ||||||||
| 0–4 years | 290.7 | 202.2 | 418.0 | <0.0001 | 271.5 | 190.4 | 387.2 | <0.0001 |
| 5–9 years | 4.1 | 2.8 | 6.0 | 3.7 | 2.5 | 5.5 | 4.149 | |
| 10–17 years | 106.7 | 75.3 | 151.4 | 95.7 | 68.0 | 134.9 | ||
| 18+ years | reference | reference | ||||||
| Maternal education | ||||||||
| None | 1.399 | 0.962 | 2.034 | 1.540 | 1.064 | 2.229 | ||
| 1 to 5 years | 1.559 | 1.103 | 2.203 | <0.0001 | 1.507 | 1.073 | 2.118 | 0.1293 |
| 6 to 8 years | 1.862 | 1.321 | 2.625 | 1.557 | 1.105 | 2.194 | ||
| 9 to 12 years | 1.586 | 1.129 | 2.229 | 1.437 | 1.020 | 2.024 | ||
| 13 to 17 years | reference | reference | ||||||
| Wealth quintile | ||||||||
| Q1 (lowest) | 2.156 | 1.829 | 2.543 | <0.0001 | 1.932 | 1.624 | 2.299 | <0.0001 |
| Q2 | 2.172 | 1.873 | 2.517 | 2.031 | 1.742 | 2.368 | ||
| Q3 | 1.611 | 1.368 | 1.899 | 1.499 | 1.271 | 1.767 | ||
| Q4 | 1.437 | 1.242 | 1.662 | 1.396 | 1.204 | 1.617 | ||
| Q5 (highest) | reference | reference | ||||||
| Number of children in household | ||||||||
| 1 child | Reference | Reference | ||||||
| 2 children | 1.575 | 1.427 | 1.739 | <0.0001 | 1.128 | 1.012 | 1.257 | 0.0258 |
| 3 children | 1.889 | 1.697 | 2.102 | 1.205 | 1.075 | 1.351 | ||
| 4 children | 2.256 | 1.945 | 2.617 | 1.256 | 1.063 | 1.485 | ||
| 5+ children | 2.461 | 1.929 | 3.140 | 1.217 | 0.961 | 1.541 | ||
| No children | 0.026 | 0.013 | 0.053 | 0.819 | 0.429 | 1.562 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jagnoor, J.; Gupta, M.; Christou, A.; Ivers, R.Q.; Bhaumik, S.; Baset, K.U.; Rogers, K.; Rahman, A. Challenges in Documenting Non-Fatal Drowning Disability in Bangladesh: A Community-Based Survey. Int. J. Environ. Res. Public Health 2021, 18, 9738. https://doi.org/10.3390/ijerph18189738
Jagnoor J, Gupta M, Christou A, Ivers RQ, Bhaumik S, Baset KU, Rogers K, Rahman A. Challenges in Documenting Non-Fatal Drowning Disability in Bangladesh: A Community-Based Survey. International Journal of Environmental Research and Public Health. 2021; 18(18):9738. https://doi.org/10.3390/ijerph18189738
Chicago/Turabian StyleJagnoor, Jagnoor, Medhavi Gupta, Aliki Christou, Rebecca Q. Ivers, Soumyadeep Bhaumik, Kamran Ul Baset, Kris Rogers, and Aminur Rahman. 2021. "Challenges in Documenting Non-Fatal Drowning Disability in Bangladesh: A Community-Based Survey" International Journal of Environmental Research and Public Health 18, no. 18: 9738. https://doi.org/10.3390/ijerph18189738
APA StyleJagnoor, J., Gupta, M., Christou, A., Ivers, R. Q., Bhaumik, S., Baset, K. U., Rogers, K., & Rahman, A. (2021). Challenges in Documenting Non-Fatal Drowning Disability in Bangladesh: A Community-Based Survey. International Journal of Environmental Research and Public Health, 18(18), 9738. https://doi.org/10.3390/ijerph18189738








