Pharmacists’ Perspectives on Interprofessional Collaboration with Physicians in Poland: A Quantitative Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Study Group
3.2. Pharmacists’ Opinions on Interprofessional Collaboration
3.3. Pharmacists’ Experiences with Interprofessional Collaboration
R111: Belief that cooperation could interfere with the competencies of one of the parties.
R7: Lack of knowledge (awareness) of doctors about the knowledge of pharmacists.
R26: arrogance and underestimating the second profession and the competence of health care workers.
R51: Sense of superiority of physician’s profession over the rest of healthcare professions.
R140: Most physicians treat pharmacists as salespeople.
R142: Physicians do not treat pharmacists as partners but rather as their subordinates because they think that only they [physicians] can cure, and pharmacists do not treat anyone.
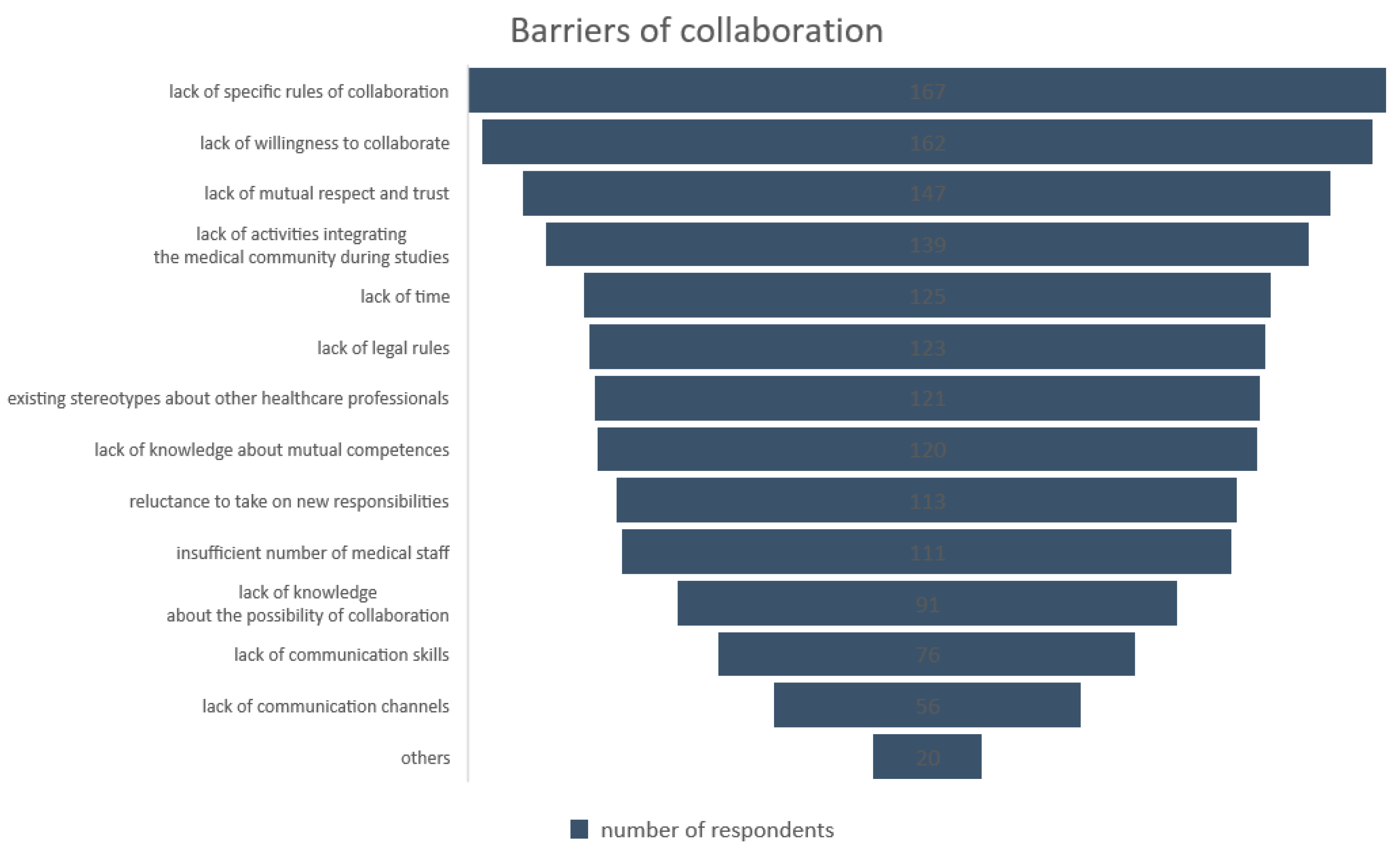
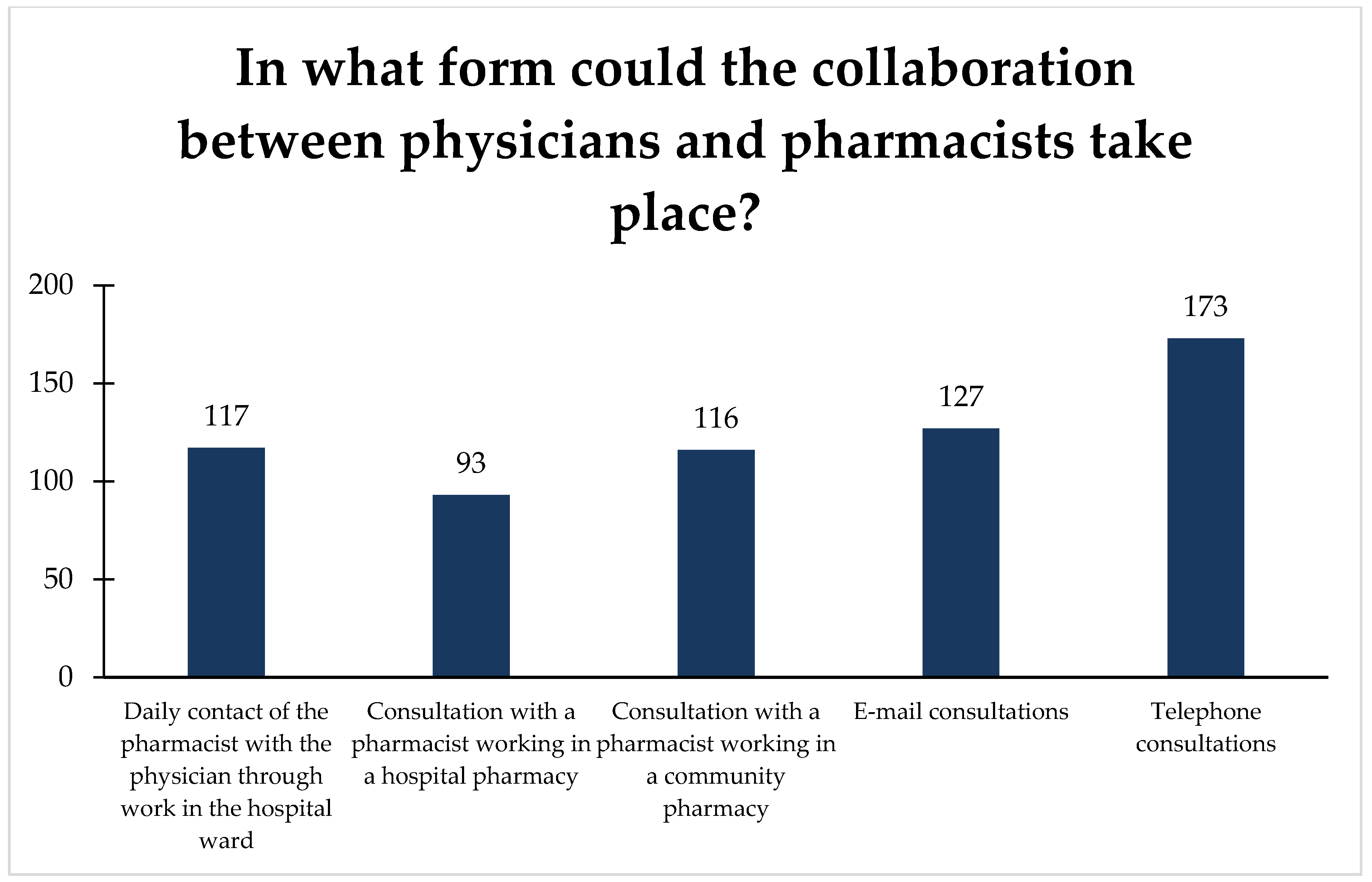
3.4. Pharmacists Expectations toward Interprofessional Collaboration
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raiche, T.; Pammett, R.; Dattani, S.; Dolovich, L.; Hamilton, K.; Kennie-Kaulbach, N.; Mccarthy, L.; Jorgenson, D. Community pharmacists’ evolving role in Canadian primary health care: A vision of harmonization in a patchwork system. Pharm. Pract. 2020, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Gordon, C.; Unni, E.; Montuoro, J.; Ogborn, D.B. Community pharmacist-led clinical services: Physician’s understanding, perceptions and readiness to collaborate in a Midwestern state in the United States. Int. J. Pharm. Pract. 2018, 26, 407–413. [Google Scholar] [CrossRef]
- Guidelines for Pharmacists Providing Home Medicines Review (HMR) Services PSA. Available online: https://www.ppaonline.com.au/wp-content/uploads/2019/01/PSA-Guidelines-for-Providing-Home-Medicines-Review-HMR-Services.pdf (accessed on 1 March 2020).
- Florentinus, S.R.; van Hulten, R.; Kramer, M.; van Dijk, L.; Heerdink, E.R.; Leufkens, H.G.M.; Groenewegen, P.P. Which pharmacists contribute to high-level pharmacotherapy audit meetings with general practitioners? Ann. Pharmacother. 2006, 40, 1640–1646. [Google Scholar] [CrossRef]
- Reeves, S.; Macmillan, K.; Van Soeren, M. Leadership of interprofessional health and social care teams: A socio-historical analysis. J. Nurs. Manag. 2010, 18, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Kludacz, M. The Problem of Availability of Human Resources in the Polish Health Care System Compared to Other Organisation for Economic Cooperation and Development Countries. Ekon. Zarz. 2015, 7, 9–31. [Google Scholar] [CrossRef]
- Sy, M.P. Filipino therapists’ experiences and attitudes of interprofessional education and collaboration: A cross-sectional survey. J. Interprof. Care 2017, 31, 761–770. [Google Scholar] [CrossRef] [PubMed]
- Topór-Mądry, R. Chronic diseases. Burden, quality of life and economic consequences. Zdr. Publiczne Zarz. 2011, 1, 25–49. [Google Scholar] [CrossRef]
- Leathard, A. Going Interprofessional: Working Together for Health and Welfare; Routledge: London, UK, 2002. [Google Scholar]
- Carter, B.L.; Bergus, G.R.; Dawson, J.D.; Farris, K.B.; Doucette, W.R.; Chrischilles, E.A.; Hartz, A.J. A cluster randomized trial to evaluate physician/pharmacist collaboration to improve blood pressure control. J. Clin. Hypertens. 2008, 10, 260–271. [Google Scholar] [CrossRef] [Green Version]
- Carter, B.L.; Ardery, G.; Dawson, J.D.; James, P.A.; Bergus, G.R.; Doucette, W.R.; Chrischilles, E.A.; Franciscus, C.L.; Xu, Y. Physician and pharmacist collaboration to improve blood pressure control. Arch. Intern. Med. 2009, 169, 1996–2002. [Google Scholar] [CrossRef] [Green Version]
- Krass, I.; Armour, C.L.; Mitchell, B.; Brillant, M.; Dienaar, R.; Hughes, J.; Lau, P.; Peterson, G.; Stewart, K.; Taylor, S.; et al. The pharmacy diabetes care program: Assessment of a community pharmacy diabetes service model in Australia. Diabet. Med. 2007, 24, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Armour, C.; Bosnic-Anticevich, S.; Brillant, M.; Burton, D.; Emmerton, L.; Krass, I.; Saini, B.; Smith, L.; Stewart, K. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax 2007, 62, 496–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Framework for Action on Interprofessional Education and Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Al AdAwi, R.M.; Stewart, D.; Ryan, C.; Tonna, A.P. A systematic review of pharmacist input to metabolic syndrome screening, management and prevention. Int. J. Clin. Pharm. 2020, 42, 995–1015. [Google Scholar] [CrossRef]
- Abdulrhim, S.; Sankaralingam, S.; Ibrahim, M.I.M.; Awaisu, A. The impact of pharmacist care on diabetes outcomes in primary care settings: An umbrella review of published systematic reviews. Prim. Care Diabetes 2020, 14, 393–400. [Google Scholar] [CrossRef]
- Hasan Ibrahim, A.S.; Barry, H.E.; Hughes, C.M. A systematic review of general practice-based pharmacists’ services to optimize medicines management in older people with multimorbidity and polypharmacy. Fam. Pract. 2021, 38, 509–523. [Google Scholar] [CrossRef] [PubMed]
- Malone, D.C.; Abarca, J.; Skrepnek, G.H.; Murphy, J.E.; Armstrong, E.P.; Grizzle, A.J.; Rehfeld, R.A.; Woosley, R.L. Pharmacist workload and pharmacy characteristics associated with the dispensing of potentially clinically important drug-drug interactions. Med. Care 2007, 45, 456–462. [Google Scholar] [CrossRef]
- Becker, M.L.; Kallewaard, M.; Caspers, P.W.J.; Schalekamp, T.; Stricker, B.H.C. Potential determinants of drug-drug interaction associated dispensing in community pharmacies. Drug Saf. 2005, 28, 371–378. [Google Scholar] [CrossRef]
- Alipour, F.; Peiravian, F.; Mehralian, G. Perceptions, experiences and expectations of physicians regarding the role of pharmacists in low-income and middle-income countries: The case of Tehran hospital settings. BMJ Open 2018, 8, e019237. [Google Scholar] [CrossRef] [Green Version]
- Żak, K. Pharmaceutical care or professional advice? Barriers to the implementation of pharmaceutical care in Poland. Ekon. Wroc. Econ. Rev. 2018, 4, 65–81. [Google Scholar] [CrossRef] [Green Version]
- Bradley, F.; Ashcroft, D.M.; Noyce, P.R. Integration and differentiation: A conceptual model of general practitioner and community pharmacist collaboration. Res. Soc. Adm. Pharm. 2012, 8, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Piecuch, A.; Makarewicz-Wujec, M.; Kozłowska-Wojciechowska, M. Pharmacist-physician relationships. Farm. Pol. 2014, 70, 353–362. [Google Scholar]
- Lemay, J.; Waheedi, M.; Al-Taweel, D.; Bayoud, T.; Moreau, P. Clinical pharmacy in Kuwait: Services provided, perceptions and barriers. Saudi Pharm. J. 2018, 26, 481–486. [Google Scholar] [CrossRef]
- Zielińska-Tomczak, Ł.; Cerbin-Koczorowska, M.; Przymuszała, P.; Marciniak, R. How to effectively promote interprofessional collaboration?—A qualitative study on physicians’ and pharmacists’ perspectives driven by the theory of planned behavior. BMC Health Serv. Res. 2021, 21, 903. [Google Scholar] [CrossRef]
- Research Online. Available online: http://researchonline.pl/ (accessed on 29 June 2021).
- Polish Medical Registers. Available online: https://rejestrymedyczne.csioz.gov.pl/ra/search/public (accessed on 3 February 2020).
- Polish Central Statistical Office Cities in Numbers. Available online: https://stat.gov.pl/cps/rde/xbcr/gus/oz_miasta_w_liczbach_2009_notatka_infor.pdf (accessed on 20 February 2020).
- Website of the Polish Ministry of Health. Available online: https://www.gov.pl/web/zdrowie/ksztalcenie-podyplomowe-farmaceutow (accessed on 9 September 2021).
- Chiolero, A.; Tremblay, S.; Delmas, P.; Scherrer, F.; Wuerzner, G.; Burnier, M.; Santschi, V. Interprofessional education in hypertension: Foundation for a team-based care culture. Eur. J. Public Health 2017, 27, ckx189.209. [Google Scholar] [CrossRef] [Green Version]
- Merks, P.; Bryła, A.; Harężlak, T.; Chmielewska-Ignatowicz, T. Job satisfaction survey among pharmacist employed in community pharmacies in Poland. Business 2019, 75, 233–237. [Google Scholar] [CrossRef]
- Chief Pharmaceutical Chamber and Aflofarm Foundation Pharmacist in Poland. Nationwide Image Research. Available online: https://www.popierwszefarmaceuta.pl/assets/Uploads/Raport-Farmaceuta-w-Polsce.pdf (accessed on 2 February 2020).
- Cerbin-Koczorowska, M.; Zielinska-Tomczak, L.; Waszyk-Nowaczyk, M.; Michalak, M.; Skowron, A. As the twig is bent, so is the tree inclined: A survey of student attitudes toward interprofessional collaboration supported with the curricula analysis. J. Interprof. Care 2019, 33, 636–644. [Google Scholar] [CrossRef]
- Alkhateeb, F.M.; Clauson, K.A.; McCafferty, R.; Latif, D.A. Physician attitudes toward pharmacist provision of medication therapy management services. Pharm. World Sci. 2009, 31, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Ahgren, B.; Axelsson, R. A decade of integration and collaboration: The development of integrated health care in Sweden 2000–2010. Int. J. Integr. Care 2011, 11, e007. [Google Scholar] [CrossRef] [Green Version]
- Braithwaite, J. Bridging gaps to promote networked care between teams and groups in health delivery systems: A systematic review of non-health literature. BMJ Open 2015, 5, e006567. [Google Scholar] [CrossRef] [Green Version]
- San Martín-Rodríguez, L.; Beaulieu, M.-D.; D’Amour, D.; Ferrada-Videla, M. The determinants of successful collaboration: A review of theoretical and empirical studies. J. Interprof. Care 2005, 19, 132–147. [Google Scholar] [CrossRef]
- Van Mil, J.W.F.; De Boer, W.O.; Tromp, T.F.J. European barriers to the implementation of pharmaceutical care. Int. J. Pharm. Pract. 2001, 9, 163–168. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Bardet, J.D.; Vo, T.H.; Bedouch, P.; Allenet, B. Physicians and community pharmacists collaboration in primary care: A review of specific models. Res. Soc. Adm. Pharm. 2015, 11, 602–622. [Google Scholar] [CrossRef] [PubMed]
- Goldstone, L.W.; Saldaña, S.N.; Werremeyer, A. Pharmacist provision of patient medication education groups. Am. J. Health Pharm. 2015, 72, 487–492. [Google Scholar] [CrossRef]
- Chruściel, T.; Chciałowski, A.; Rolczyk, U. Pharmaceutical Care—Yes, but…Commentary to the Draft Act on the Profession of Pharmacist. Available online: https://papier.gazetalekarska.pl/pdf/Gazeta_Lekarska_10_2007.pdf (accessed on 8 December 2020).
- Act on the Profession of the Pharmacist. Available online: http://orka.sejm.gov.pl/proc9.nsf/ustawy/238_u.htm (accessed on 21 December 2020).
- Cerbin-Koczorowska, M.; Waszyk-Nowaczyk, M.; Przymuszała, P. Pharmacists’ preparedness to patients education at the time of pandemic—A cross-sectional study with an example of sars-cov-2 outbreak in Poland. Int. J. Environ. Res. Public Health 2020, 17, 6659. [Google Scholar] [CrossRef] [PubMed]
- Cerbin-Koczorowska, M.; Przymuszala, P.; Zielinska-Tomczak, L.; Wawrzyniak, E.; Marciniak, R. Is there a time and place for health education in chain pharmacies? Perspectives of Polish community pharmacists. Health Soc. Care Community 2021, 29, e56–e66. [Google Scholar] [CrossRef]
- Costa, F.A.; Scullin, C.; Al-Taani, G.; Hawwa, A.F.; Anderson, C.; Bezverhni, Z.; Binakaj, Z.; Cordina, M.; Foulon, V.; Garcia de Bikuña, B.; et al. Provision of pharmaceutical care by community pharmacists across Europe: Is it developing and spreading? J. Eval. Clin. Pract. 2017, 23, 1336–1347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. World Health Organization Joint FIP/WHO guidelines on good pharmacy practice: Standards for quality of pharmacy services. WHO Tech. Rep. Ser. 2011, 961, 1–18. [Google Scholar]
- Awad, A.; Matowe, L.; Capps, P. Medical doctors’ perceptions and expectations of the role of hospital pharmacists in Sudan. Pharm. World Sci. PWS 2007, 29, 557–564. [Google Scholar] [CrossRef]
- Io, U.M.; Hu, H.; Ung, C.O.L. Physicians’ and pharmacists’ experience and expectations of the roles of pharmacists: Insights into hospital setting in Macau. Trop. J. Pharm. Res. 2013, 12, 1077–1085. [Google Scholar] [CrossRef] [Green Version]
- Bryant, L.J.M.; Coster, G.; Gamble, G.D.; McCormick, R.N. General practitioners’ and pharmacists’ perceptions of the role of community pharmacists in delivering clinical services. Res. Soc. Adm. Pharm. 2009, 5, 347–362. [Google Scholar] [CrossRef] [PubMed]
- El Hajj, M.S.; AL-Saeed, H.S.; Khaja, M. Qatar pharmacists’ understanding, attitudes, practice and perceived barriers related to providing pharmaceutical care. Int. J. Clin. Pharm. 2016, 38, 330–343. [Google Scholar] [CrossRef]
- Cerbin-Koczorowska, M.; Michalak, M.; Skotnicki, M.; Waszyk-Nowaczyk, M. Partnership-is it even possible? Different attitudes of medical and pharmacy students toward interprofessional cooperation. Farmacia 2014, 62, 6. [Google Scholar]
- Iskierski, J.; Zimmermann, A. Social role of the pharmaceutical profession in the eyes of pharmacists and the patients. Farm. Pol. 2006, 62, 210–217. [Google Scholar]
- Ranelli, P.L.; Biss, J. Physicians’ perceptions of communication with and responsibilities of pharmacists. J. Am. Pharm. Assoc. 2000, 40, 625–630. [Google Scholar] [CrossRef]
- Matowe, L.; Abahussain, E.A.; Al-Saffar, N.; Bihzad, S.M.; Al-Foraih, A.; Al-Kandery, A.A. Physicians’ perceptions and expectations of pharmacists’ professional duties in government hospitals in Kuwait. Med. Princ. Pract. 2006, 15, 185–189. [Google Scholar] [CrossRef]
- Kelly, D.V.; Bishop, L.; Young, S.; Hawboldt, J.; Phillips, L.; Keough, T.M. Pharmacist and physician views on collaborative practice: Findings from the community pharmaceutical care project. Can. Pharm. J. 2013, 146, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Hashemian, F.; Emadi, F.; Roohi, E. Collaboration between pharmacists and general practitioners in the health care system in the Islamic Republic of Iran. EMRO 2016, 22, 375–382. [Google Scholar] [CrossRef]
- Albassam, A.; Almohammed, H.; Alhujaili, M.; Koshy, S.; Awad, A. Perspectives of primary care physicians and pharmacists on interprofessional collaboration in Kuwait: A quantitative study. PLoS ONE 2020, 15, e0236114. [Google Scholar] [CrossRef]
- Hammick, M.; Freeth, D.; Koppel, I.; Reeves, S.; Barr, H. A best evidence systematic review of interprofessional education: BEME Guide no. 9. Med. Teach. 2007, 29, 735–751. [Google Scholar] [CrossRef]
- Liaskos, J.; Frigas, A.; Antypas, K.; Zikos, D.; Diomidous, M.; Mantas, J. Promoting interprofessional education in health sector within the European Interprofessional Education Network. Int. J. Med. Inform. 2009, 78, S43–S47. [Google Scholar] [CrossRef]
- Baggs, J.G.; Schmitt, M.H. Nurses’ and resident physicians’ perceptions of the process of collaboration in an MICU. Res. Nurs. Health 1997, 20, 71–80. [Google Scholar] [CrossRef]
- Buring, S.M.; Bhushan, A.; Broeseker, A.; Conway, S.; Duncan-Hewitt, W.; Hansen, L.; Westberg, S. Interprofessional education: Definitions, student competencies, and guidelines for implementation. Am. J. Pharm. Educ. 2009, 73, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cerbin-Koczorowska, M.; Przymuszała, P.; Michalak, M.; Piotrowska-Brudnicka, S.; Kant, P.; Skowron, A. Comparison of medical and pharmacy students’ readiness for interprofessional learning-a cross-sectional study. Farmacia 2020, 68, 1166–1172. [Google Scholar] [CrossRef]
- Bollen, A.; Harrison, R.; Aslani, P.; van Haastregt, J.C.M. Factors influencing interprofessional collaboration between community pharmacists and general practitioners—A systematic review. Health Soc. Care Community 2019, 27, e189–e212. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| n | Percent, % | |
|---|---|---|
| Number of respondents | 207 | 100.0 |
| Workplace 1 | ||
| village | 19 | 9.2 |
| small town | 55 | 26.6 |
| medium town | 65 | 31.4 |
| large town | 68 | 32.9 |
| Seniority (years) | ||
| ≤5 | 62 | 30.0 |
| 6–15 | 60 | 29.0 |
| 16–25 | 52 | 25.1 |
| ≥26 | 33 | 15.9 |
| Foreign internship | ||
| Yes | 16 | 7.7 |
| No | 191 | 92.3 |
| Specialization | ||
| Yes | 62 | 30.0 |
| No | 145 | 70.0 |
| Variables | Results | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Σn | n1+2 | n3 | n4+5 | Dominant | Median | Lower Quartile | Upper Quartile | p-Value | ||
| How is the collaboration between pharmacists and physicians currently shaped? (response options on a scale from 1—cooperation is very bad to 5—cooperation is very good) | ||||||||||
| 182 | 100 (55.0%) | 43 (23.6%) | 39 (21.4%) | 2 | 2 | 2 | 3 | |||
| Specialization | No | 127 | 77 (60.6%) | 27 (21.3%) | 23 (18.1%) | 2 | 2 | 2 | 3 | p = 0.031 |
| Yes | 55 | 23 (41.8%) | 16 (29.1%) | 16 (29.1%) | 2–3 | 3 | 2 | 4 | ||
| Workplace 1 | village | 17 | 10 (58.8%) | 3 (17.7%) | 4 (23.5%) | 2 | 2 | 2 | 3 | ns |
| small town | 49 | 21 (42.9%) | 15 (30.6%) | 13 (26.5%) | 2 | 3 | 2 | 4 | ||
| medium town | 53 | 29 (54.7%) | 14 (26.4%) | 10 (18.9%) | 2 | 2 | 2 | 3 | ||
| large town | 63 | 40 (63.5%) | 11 (17.5%) | 12 (19.1%) | 2 | 2 | 2 | 3 | ||
| Foreign internship | No | 169 | 89 (52.7%) | 42 (24.9%) | 38 (22.5%) | 2 | 2 | 2 | 3 | ns |
| Yes | 13 | 11 (84.6%) | 1 (7.7%) | 1 (7.7%) | 2 | 2 | 2 | 2 | ||
| Is collaboration between a pharmacist and a physician possible? (response options on a scale from 1—definitely not to 5—definitely yes) | ||||||||||
| 207 | 19 (9.2%) | 15 (7.2%) | 173 (83.6%) | 4 | 5 | 4 | 5 | |||
| Specialization | No | 145 | 13 (9.0%) | 11 (7.6%) | 121 (83.4%) | 4–5 | 4 | 4 | 5 | ns |
| Yes | 62 | 6 (9.7%) | 4 (6.4%) | 52 (83.9%) | 5 | 5 | 4 | 5 | ||
| Workplace 1 | village | 19 | 4 (21.1%) | 3 (15.8%) | 12 (63.1%) | 4 | 4 | 3 | 5 | p = 0.026 |
| small town | 55 | 5 (9.1%) | 2 (3.6%) | 48 (87.3%) | 4 | 4 | 4 | 5 | ||
| medium town | 65 | 5 (7.7%) | 6 (9.2%) | 54 (83.1%) | 5 | 4 | 4 | 5 | ||
| large town | 68 | 5 (7.4%) | 4 (5.8%) | 59 (86.8%) | 5 | 5 | 4 | 5 | ||
| Foreign internship | No | 191 | 18 (9.4%) | 14 (7.3%) | 159 (83.3%) | 5 | 4 | 4 | 5 | ns |
| Yes | 16 | 1 (6.3%) | 1 (6.3%) | 14 (87.5%) | 5 | 4 | 4 | 5 | ||
| Assess your attitude to collaboration between a physician and a pharmacist (response options on a scale from 1—very reluctant to 5—very willing) | ||||||||||
| 198 | 24 (12.1%) | 18 (9.1%) | 156 (78.8%) | 5 | 5 | 4 | 5 | |||
| Specialization | No | 140 | 19 (13.6%) | 15 (10.7%) | 106 (75.7%) | 5 | 5 | 4 | 5 | ns |
| Yes | 39 | 5 (12.8%) | 4 (10.7%) | 30 (76.9%) | 5 | 5 | 4 | 5 | ||
| Workplace 1 | Village | 16 | 2 (12.5%) | 7 (43.8%) | 7 (43.8%) | 4–5 | 4 | 4 | 5 | ns |
| small town | 45 | 9 (20.0%) | 8 (17.8%) | 28 (62.2%) | 5 | 4 | 3 | 5 | ||
| medium town | 61 | 10 (16.4%) | 6 (9.8%) | 45 (73.8%) | 5 | 5 | 4 | 5 | ||
| large town | 67 | 3 (4.5%) | 5 (7.5%) | 59 (88.0%) | 5 | 5 | 4 | 5 | ||
| Foreign internship | No | 184 | 24 (13.0%) | 19 (10.7%) | 141 (76.6%) | 5 | 4 | 4 | 5 | p = 0.011 |
| Yes | 15 | 0 (0.0%) | 0 (0.0%) | 15 (100.0%) | 5 | 5 | 5 | 5 | ||
| Variables | Results | |||||||
|---|---|---|---|---|---|---|---|---|
| How Often in the Last Year Have You Made Contact with Physicians Regarding (1—Very Rarely, 5—Very Often) | ||||||||
| Σn | n1+2 | n3 | n4+5 | Dominant | Median | Lower Quartile | Upper Quartile | |
| formal aspects | ||||||||
| correction of a prescription error | 207 | 17 (8.2%) | 36 (17.4%) | 154 (74.4%) | 5 | 4 | 3 | 5 |
| consultation on drug availability at the pharmacy | 207 | 94 (45.4%) | 53 (25.6%) | 60 (29.0%) | 1 | 3 | 1 | 4 |
| substantive aspects | ||||||||
| consultation on drug dosage | 207 | 150 (72.5%) | 40 (19.3%) | 17 (8.2%) | 1 | 2 | 1 | 3 |
| consultation on the choice of a drug substance | 207 | 189 (91.3%) | 14 (6.8%) | 4 (1.9%) | 1 | 1 | 1 | 1 |
| consultation on drug interactions | 197 | 188 (95.5%) | 5 (2.5%) | 4 (2.0%) | 1 | 1 | 1 | 1 |
| consultation on side effects | 207 | 202 (97.6%) | 2 (2.0%) | 3 (1.4%) | 1 | 1 | 1 | 1 |
| prescription drug consultation | 182 | 127 (69.8%) | 47 (25.8%) | 8 (4.4%) | 1 | 2 | 1 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zielińska-Tomczak, Ł.; Cerbin-Koczorowska, M.; Przymuszała, P.; Gałązka, N.; Marciniak, R. Pharmacists’ Perspectives on Interprofessional Collaboration with Physicians in Poland: A Quantitative Study. Int. J. Environ. Res. Public Health 2021, 18, 9686. https://doi.org/10.3390/ijerph18189686
Zielińska-Tomczak Ł, Cerbin-Koczorowska M, Przymuszała P, Gałązka N, Marciniak R. Pharmacists’ Perspectives on Interprofessional Collaboration with Physicians in Poland: A Quantitative Study. International Journal of Environmental Research and Public Health. 2021; 18(18):9686. https://doi.org/10.3390/ijerph18189686
Chicago/Turabian StyleZielińska-Tomczak, Łucja, Magdalena Cerbin-Koczorowska, Piotr Przymuszała, Natalia Gałązka, and Ryszard Marciniak. 2021. "Pharmacists’ Perspectives on Interprofessional Collaboration with Physicians in Poland: A Quantitative Study" International Journal of Environmental Research and Public Health 18, no. 18: 9686. https://doi.org/10.3390/ijerph18189686
APA StyleZielińska-Tomczak, Ł., Cerbin-Koczorowska, M., Przymuszała, P., Gałązka, N., & Marciniak, R. (2021). Pharmacists’ Perspectives on Interprofessional Collaboration with Physicians in Poland: A Quantitative Study. International Journal of Environmental Research and Public Health, 18(18), 9686. https://doi.org/10.3390/ijerph18189686









