Evaluating a Low-Cost Technology to Enable People with Intellectual Disability or Psychiatric Disorders to Initiate and Perform Functional Daily Activities
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Settings, Sessions and Activities
2.3. Measures and Recording
2.3.1. Technology System
2.3.2. Experimental Conditions and Data Analysis
2.3.3. Baseline I
2.3.4. Baseline II
2.3.5. Intervention
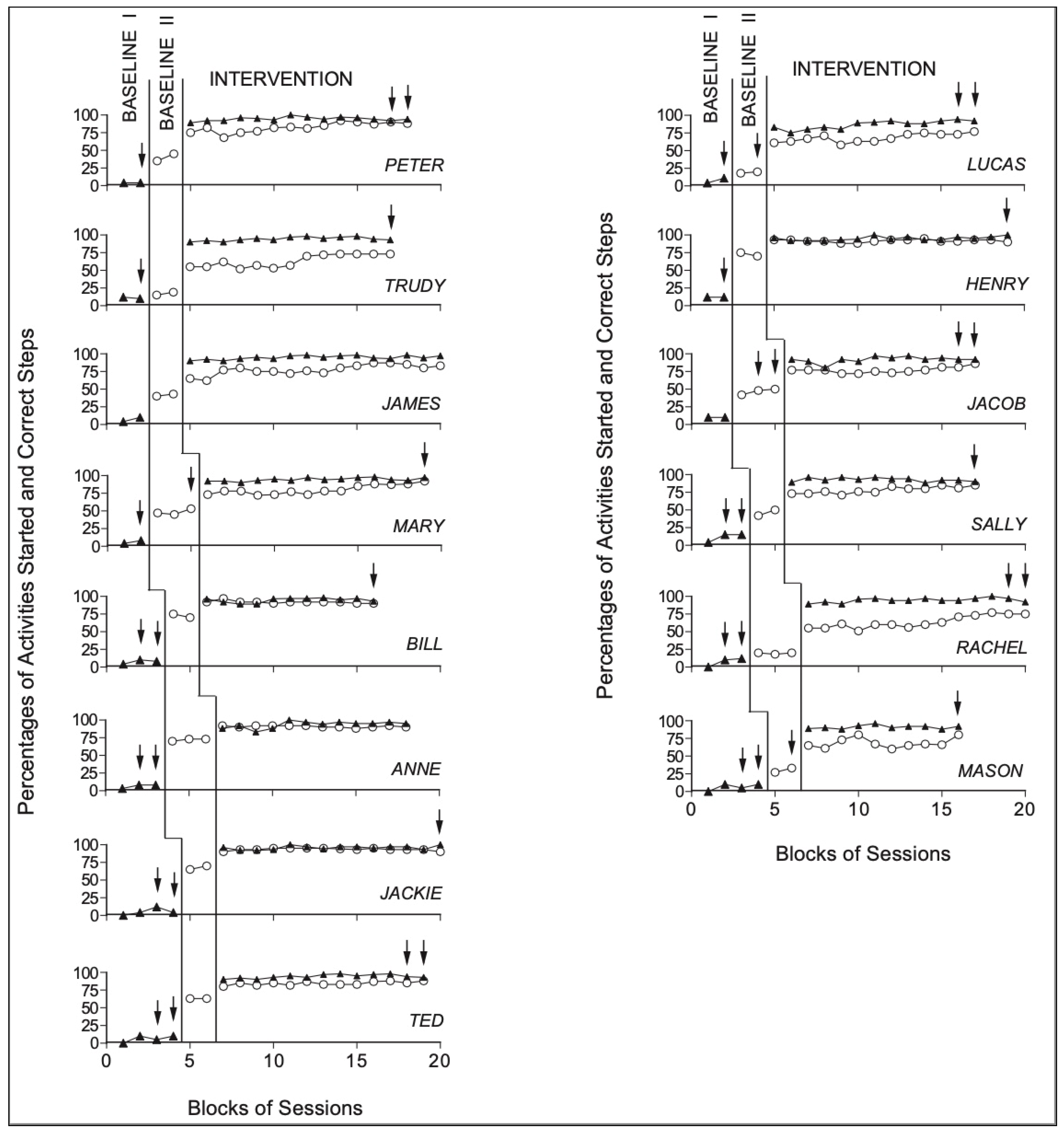
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gildengers, A.G.; Chisholm, D.; Butters, M.A.; Anderson, S.J.; Begley, A.; Holm, M.; Rogers, J.C.; Reynolds, C.F.; Mulsant, B.H. Two-year course of cognitive function and instrumental activities of daily living in older adults with bipolar disorder: Evidence for neuroprogression? Psychol. Med. 2013, 43, 801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Neill, B.; Best, C.; O’Neill, L.; Ramos, S.D.; Gillespie, A. Efficacy of a micro-prompting technology in reducing support needed by people with severe acquired brain injury in activities of daily living: A randomized control trial. J. Head Trauma Rehabil. 2018, 33, E33–E41. [Google Scholar] [CrossRef] [PubMed]
- King, E.; Okodogbe, T.; Burke, E.; McCarron, M.; McCallion, P.; O’Donovan, M.A. Activities of daily living and transition to community living for adults with intellectual disabilities. Scand. J. Occup. Ther. 2017, 24, 357–365. [Google Scholar] [CrossRef]
- Galderisi, S.; Rossi, A.; Rocca, P.; Bertolino, A.; Mucci, A.; Bucci, P.; Gibertoni, D.; Aguglia, E.; Amore, M.; Bellomo, A.; et al. The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry 2014, 13, 275–287. [Google Scholar] [CrossRef] [Green Version]
- Mechling, L.C. Assistive technology as a self-management tool for prompting students with intellectual disabilities to initiate and complete daily tasks: A literature review. Educ. Train. Autism Dev. Disabil. 2007, 42, 252–269. [Google Scholar]
- Spriggs, A.D.; Mims, P.J.; van Dijk, W.; Knight, V.F. Examination of the evidence base for using visual activity schedules with students with intellectual disability. J. Spec. Educ. 2017, 51, 14–26. [Google Scholar] [CrossRef]
- Payne, D.; Cannella-Malone, H.I.; Tullis, C.A.; Sabielny, L.M. The effects of self-directed video prompting with two students with intellectual and developmental disabilities. J. Dev. Phys. Disabil. 2012, 24, 617–634. [Google Scholar] [CrossRef]
- Harvey, P.D.; Strassnig, M. Predicting the severity of everyday functional disability in people with schizophrenia: Cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry 2012, 11, 73–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harr, N.; Dunn, L.; Price, P. Case study on effect of household task participation on home, community, and work opportunities for a youth with multiple disabilities. Work 2011, 39, 445–453. [Google Scholar] [CrossRef]
- Dusseljee, J.C.; Rijken, P.M.; Cardol, M.; Curfs, L.M.G.; Groenewegen, P.P. Participation in daytime activities among people with mild or moderate intellectual disability. J. Intellect. Disabil. Res. 2011, 55, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Fischer, E.P.; Shumway, M.; Owen, R.R. Priorities of consumers, providers, and family members in the treatment of schizophrenia. Psychiatr. Serv. 2002, 53, 724–729. [Google Scholar] [CrossRef]
- Smith, K.A.; Shepley, S.B.; Alexander, J.L.; Ayres, K.M. The independent use of self-instructions for the acquisition of untrained multi-step tasks: A review of the literature. Res. Dev. Disabil. 2015, 40, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Shepley, S.B. Self-instructing with mobile technology: Considerations and applications to increase independence. Teach. Except. Child. 2017, 50, 59–65. [Google Scholar] [CrossRef]
- Rodriguez-Villa, E.; Camacho, E.; Torous, J. Psychiatric rehabilitation through teaching smartphone skills to improve functional outcomes in serious mental illness. Internet Interv. 2021, 23, 100366. [Google Scholar] [CrossRef] [PubMed]
- Mechling, L.C.; Foster, A.M.; Ayres, K.M. Navigation between menu screens and multiple touch points on a touch screen tablet to access and complete multi-step tasks using video prompting. Inclusion 2013, 1, 121–132. [Google Scholar] [CrossRef]
- Goo, M.; Maurer, A.L.; Wehmeyer, M.L. Systematic review of using portable smart devices to teach functional skills to students with intellectual disability. Educ. Train. Autism Dev. Disabil. 2019, 54, 57–68. [Google Scholar]
- Kagohara, D.M.; van der Meer, L.; Ramdoss, S.; O’Reilly, M.F.; Lancioni, G.E.; Davis, T.N.; Rispoli, M.; Lang, R.; Marschik, P.B.; Sutherland, D.; et al. Using iPods and iPads in teaching programs for individuals with developmental disabilities: A systematic review. Res. Dev. Disabil. 2013, 34, 147–156. [Google Scholar] [CrossRef]
- McMahon, D.D.; Smith, C.C.; Cihak, D.F.; Wright, R.; Gibbons, M.M. Effects of digital navigation aids on adults with intellectual disabilities: Comparison of paper map, google maps, and augmented reality. J. Spec. Educ. Technol. 2015, 30, 157–165. [Google Scholar] [CrossRef]
- Desideri, L.; Lancioni, G.; Malavasi, M.; Gherardini, A.; Cesario, L. Step-Instruction Technology to Help People with Intellectual and Other Disabilities Perform Multistep Tasks: A Literature Review. J. Dev. Phys. Disabil. 2020, 1–30. [Google Scholar] [CrossRef]
- Shepley, S.B.; Spriggs, A.D.; Samudre, M.; Elliot, M. Increasing daily living independence using video activity schedules in middle school students with intellectual disability. J. Spec. Educ. Technol. 2018, 33, 71–82. [Google Scholar] [CrossRef]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; Campodonico, F.; Zimbaro, C.; Alberti, G.; Trubia, G.; Zagaria, T. Helping people with multiple disabilities manage an assembly task and mobility via technology-regulated sequence cues and contingent stimulation. Life Span. Disabil. 2018, 21, 143–163. [Google Scholar]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; Alberti, G.; Perilli, V.; Zimbaro, C.; Chiariello, V.; Campodonico, F. Supporting leisure and functional activity engagement in people with multiple disabilities via a technology-aided program. Technol. Disabil. 2018, 29, 173–181. [Google Scholar] [CrossRef]
- Lancioni, G.E.; O’Reilly, M.F.; Sigafoos, J.; Desideri, L.; Alberti, G.; Campodonico, F.; Chiariello, V. Smartphone-Based Technology to Support Functional Occupation and Mobility in People with Intellectual Disability and Visual Impairment. Adv. Neurodev. Disord. 2019, 3, 334–342. [Google Scholar] [CrossRef]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; Alberti, G.; Chiariello, V.; Carrella, L. Everyday Technology to Support Leisure and Daily Activities in People with Intellectual and Other Disabilities. Dev. Neurorehabil. 2020, 23, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Dagnan, D.; Masson, J.; Thwaites, R.; James, A.; Hatton, C. Training therapists to work with people with intellectual disability in improving access to psychological therapies (IAPT) services. J. Appl. Res. Intellect. Disabil. 2018, 31, 760–767. [Google Scholar] [CrossRef] [Green Version]
- Boot, F.H.; Dinsmore, J.; Khasnabis, C.; MacLachlan, M. Intellectual disability and assistive technology: Opening the GATE wider. Front. Public Health 2017, 5, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramsten, C.; Martin, L.; Dag, M.; Hammar, L.M. Information and communication technology use in daily life among young adults with mild-to-moderate intellectual disability. J. Intellect. Disabil. 2020, 24, 289–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Connolly, S.L.; Kuhn, E.; Possemato, K.; Torous, J. Digital Clinics and Mobile Technology Implementation for Mental Health Care. Curr. Psychiatry Rep. 2021, 23, 1–7. [Google Scholar] [CrossRef]
- Pedhazur, E.; Schmelkin, L. Measurement Design and Analysis: An Integrated Approach; Psychology Press: New York, NY, USA, 1991. [Google Scholar]
- Measso, G.; Cavarzeran, F.; Zappalà, G.; Lebowitz, B.D.; Crook, T.H.; Pirozzolo, F.J.; Amaducci, L.A.; Massari, D.C.; Grigoletto, F. The mini-mental state examination: Normative study of an Italian random sample. Dev. Neuropsychol. 1993, 9, 77–85. [Google Scholar] [CrossRef]
- Dubois, B.; Slachevsky, A.; Litvan, I.; Pillon, B.F.A.B. The FAB: A frontal assessment battery at bedside. Neurology 2000, 55, 1621–1626. [Google Scholar] [CrossRef] [Green Version]
- Appollonio, I.; Leone, M.; Isella, V.; Piamarta, F.; Consoli, T.; Villa, M.L.; Forapani, E.; Russo, A.; Nichelli, P. The Frontal Assessment Battery (FAB): Normative values in an Italian population sample. Neurol. Sci. 2005, 26, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Katz, S. Assessing self-maintenance: Activities of daily living, mobility, and instrumental activities of daily living. J. Am. Geriatr. Soc. 1983, 31, 721–727. [Google Scholar] [CrossRef]
- Graf, C. The Lawton instrumental activities of daily living (IADL) scale. AJN Am. J. Nurs. 2008, 108, 52–62. [Google Scholar] [CrossRef] [Green Version]
- Barlow, D.H.; Nock, M.; Hersen, M. Single-Case Experimental Designs: Strategies for Studying Behavior Change, 3rd ed.; Allyn & Bacon: New York, NY, USA, 2009. [Google Scholar]
- Siegel, S.; Castellan, N.J. Nonparametric Statistics for the Behavioral Sciences, 2nd ed.; Macgraw-Hill: New York, NY, USA, 1988. [Google Scholar]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; Boccasini, A.; Alberti, G.; Lang, R. People with multiple disabilities use basic reminding technology to engage in daily activities at the appropriate times. J. Dev. Phys. Disabil. 2014, 26, 347–355. [Google Scholar] [CrossRef]
- Bouck, E.C.; Shurr, J.C.; Tom, K.; Jasper, A.D.; Bassette, L.; Miller, B.; Flanagan, S.M. Fix it with TAPE: Repurposing technology to be assistive technology for students with high-incidence disabilities. Prev. Sch. Fail. 2012, 56, 121–128. [Google Scholar] [CrossRef]
- O’Brien, A.M.; Schlosser, R.W.; Yu, C.; Allen, A.A.; Shane, H.C. Repurposing a smartwatch to support individuals with autism spectrum disorder: Sensory and operational considerations. J. Spec. Educ. Technol. 2020. [Google Scholar] [CrossRef]
- Tebbutt, E.; Brodmann, R.; Borg, J.; MacLachlan, M.; Khasnabis, C.; Horvath, R. Assistive products and the sustainable development goals (SDGs). Glob. Health 2016, 12, 79. [Google Scholar] [CrossRef] [Green Version]
- Shahat, A.R.S.; Greco, G. The Economic Costs of Childhood Disability: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 3531. [Google Scholar] [CrossRef] [PubMed]
- Madara Marasinghe, K. Assistive technologies in reducing caregiver burden among informal caregivers of older adults: A systematic review. Disabil. Rehabil. Assist. Technol. 2016, 11, 353–360. [Google Scholar] [CrossRef]
- Desideri, L.; Mingardi, A.; Stefanelli, B.; Tanzini, D.; Bitelli, C.; Roentgen, U.; de Witte, L. Assessing children with multiple disabilities for assistive technology: A framework for quality assurance. Technol. Disabil. 2013, 25, 159–166. [Google Scholar] [CrossRef]
| Participant (Pseudonyms) | Chronological Age (Years) | Main Diagnosis | MMSE | FAB | ADL | IADL |
|---|---|---|---|---|---|---|
| Group 1: Psychiatric conditions and cognitive dysfunctions | ||||||
| Peter (PVA) | 50 | Schizoaffective disorder | 19,89 | 0 | 3/6 | 2/5 |
| Trudy (MR) | 48 | Major depressive disorder | 10,31 | 0 | 5/6 | 7/8 |
| James (RC) | 62 | Schizophrenia | 17,99 | 0 | 4/6 | 4/5 |
| Mary (LA) | 47 | Schizophrenia | 13,62 | 0 | 3/6 | 5/8 |
| Bill (GO) | 59 | Schizophrenia | 22,97 | 0 | 2/6 | 3/5 |
| Anne (DMG) | 62 | Schizophrenia | 22,53 | 0 | 3/6 | 5/8 |
| Jackie (RS) | 45 | Schizoaffective disorder | 22,21 | 1 | 2/6 | 4/8 |
| Ted (VF) | 60 | Schizophrenia | 23,74 | 0 | 2/6 | 4/5 |
| Group 2: Intellectual disability | ||||||
| Lucas (BG) | 40 | Intellectual disability * | 14,42 | 0 | 3/6 | 4/5 |
| Henry (DLR) | 36 | Intellectual disability * | 22,42 | 0 | 2/6 | 3/5 |
| Jacob (CVG) | 25 | Severe intellectual disability | 15,59 | 0 | 3/6 | 4/5 |
| Sally (NG) | 40 | Severe intellectual disability | 21,42 | 0 | 2/6 | 5/8 |
| Rachel (DMS) | 35 | Moderate intellectual disability | 9,42 | 0 | 3/6 | 5/8 |
| Mason (MG) | 27 | Severe intellectual disability | 15,59 | 0 | 2/6 | 3/5 |
| Exemplar Activity 1: “Brush Your Teeth” | Exemplar Activity 2: “Prepare for Sleep” |
|---|---|
| Go to your room Take off your shoes Take off your pants Take off your sweatshirt Put them in order in the wardrobe Put on the pajamas Take the keys for the operator Open the locker and take your beauty case Wash your teeth with your toothbrush and the toothpaste Put the beauty case back in its place When you are done, return the keys to the operator Go to your room Go to sleep |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Resta, E.; Brunone, L.; D’Amico, F.; Desideri, L. Evaluating a Low-Cost Technology to Enable People with Intellectual Disability or Psychiatric Disorders to Initiate and Perform Functional Daily Activities. Int. J. Environ. Res. Public Health 2021, 18, 9659. https://doi.org/10.3390/ijerph18189659
Resta E, Brunone L, D’Amico F, Desideri L. Evaluating a Low-Cost Technology to Enable People with Intellectual Disability or Psychiatric Disorders to Initiate and Perform Functional Daily Activities. International Journal of Environmental Research and Public Health. 2021; 18(18):9659. https://doi.org/10.3390/ijerph18189659
Chicago/Turabian StyleResta, Emanuela, Lucia Brunone, Fiora D’Amico, and Lorenzo Desideri. 2021. "Evaluating a Low-Cost Technology to Enable People with Intellectual Disability or Psychiatric Disorders to Initiate and Perform Functional Daily Activities" International Journal of Environmental Research and Public Health 18, no. 18: 9659. https://doi.org/10.3390/ijerph18189659
APA StyleResta, E., Brunone, L., D’Amico, F., & Desideri, L. (2021). Evaluating a Low-Cost Technology to Enable People with Intellectual Disability or Psychiatric Disorders to Initiate and Perform Functional Daily Activities. International Journal of Environmental Research and Public Health, 18(18), 9659. https://doi.org/10.3390/ijerph18189659






