Evaluation of Capillary Blood Gases in Medical Personnel Caring for Patients Isolated Due to SARS-CoV-2 in Intensive Care Units before and after Using Enhanced Filtration Masks: A Prospective Cohort Study
Abstract
:1. Introduction
Aim
2. Methods
2.1. Study Design, Setting, Ethical Considerations
2.2. Participants Clinical
2.3. Research Procedure
2.4. Data Collection
2.5. Outcomes
2.6. Statistics
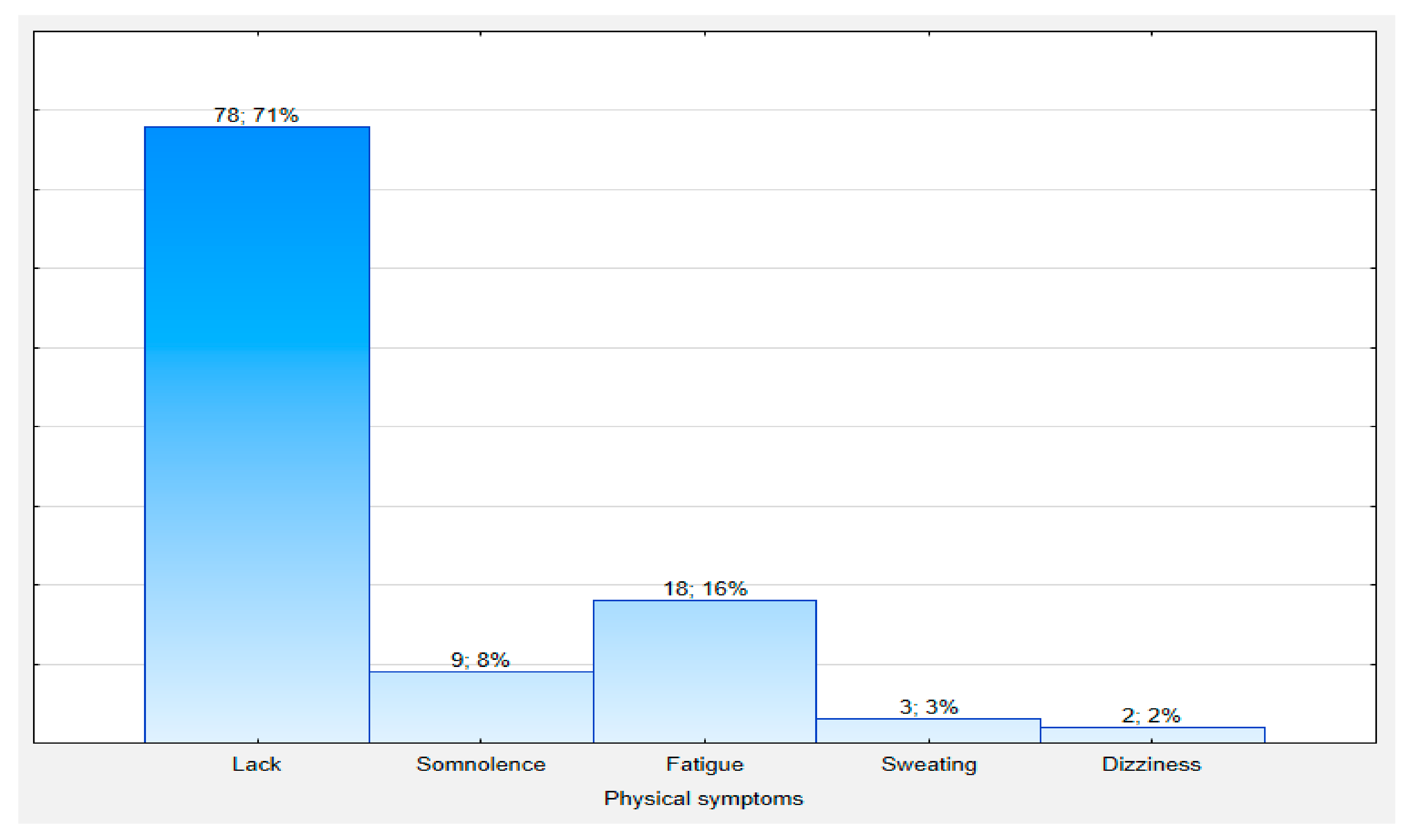
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Implications for Practice
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Calò, F.; Russo, A.; Camaioni, C.; De Pascalis, S.; Coppola, N. Burden, risk assessment, surveillance and management of SARS-CoV-2 infection in health workers: A scoping review. Infect. Dis. Poverty 2020, 9, 139. [Google Scholar] [CrossRef] [PubMed]
- Hick, J.L.; Hanfling, D.; Wynia, M.K.; Pavia, A.T. Duty to Plan: Health Care, Crisis Standards of Care, and Novel Coronavirus SARS-CoV-2. Available online: https://nam.edu/duty-to-plan-health-care-crisis-standards-of-care-and-novel-coronavirus-sars-cov-2/ (accessed on 10 December 2020).
- World Health Organization. Advice on the Use of Masks in the Community, During Home Care and in Health Care Settings in the Context of the Novel Coronavirus (2019-nCoV) Outbreak; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/bitstream/handle/10665/330987/WHO-nCov-IPC_Masks-2020.1-eng.pdf?sequence=1&isAllowed=y (accessed on 8 December 2020).
- Scheid, J.L.; Shannon, P.; Lupien, S.L.; Gregory, S.; Ford, G.S.; West, S.L. Commentary: Physiological and Psychological Impact of Face Mask Usage during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6655. [Google Scholar] [CrossRef]
- Verbeek, J.H.; Rajamaki, B.; Ijaz, S.; Sauni, R.; Toomey, E.; Blackwood, B.; Tikka, C.; Ruotsalainen, J.H.; Balci, F.S.K. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst. Rev. 2020, 15, CD011621. [Google Scholar] [CrossRef]
- Roberge, R.J.; Coca, A.; Williams, W.J.; Powell, J.B.; Palmiero, A.J. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir. Care 2010, 55, 569–577. [Google Scholar] [PubMed]
- Bein, B.; Bachmann, M.; Huggett, S.; Wegermann, P. SARS-CoV-2/COVID-19: Evidence-Based Recommendations on Diagnosis and Therapy. Geburtshilfe Frauenheilkd. 2020, 80, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Ippolito, M.; Ramanan, M.; Bellina, D.; Catalisano, G.; Iozzo, P.; Di Guardo, A.; Moscarelli, A.; Grasselli, G.; Giarratano, A.; Bassetti, M.; et al. Personal protective equipment use by healthcare workers in intensive care unit during the early phase of COVID-19 pandemic in Italy: A secondary analysis of the PPE-SAFE survey. Ther. Adv. Infect. Dis. 2021, 8, 2049936121998562. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Position of the Team of Consultants in the Field of Anaesthesiology and Intensive Care Nursing in Consultation with the Main Board of the Polish Society of Anesthesiology and Intensive Care Nurses Regarding the Necessary Staffing of Nursing Staff in Anaesthesiology and Intensive Care Units (OAIT) in the Care of Patients Infected with SARS-COv-2 Virus. Available online: http://oipip.gda.pl/files/aktualnosci/Stanowisko%20Zespo%C5%82u%20Konsultanto%CC%81w%20w%20sprawie%20obsad%20piele%CC%A8gniarskich%20w%20oddziale%20AIT%20w%20czasie%20pandemii-1.pdf (accessed on 8 November 2020). (In Polish).
- Higgins, C. Capillary Blood Gases—To Arterialize or Not. Available online: https://acutecaretesting.org/en/articles/capillary-blood-gases--to-arterialize-or-not (accessed on 1 April 2021).
- Shein, S.L.; Whitticar, S.; Mascho, K.K.; Pace, E.; Speicher, R.; Deakins, K. The effects of wearing face masks on oxygenation and ventilation atrest and during physical activity. PLoS ONE 2021, 16, e0247414. [Google Scholar] [CrossRef] [PubMed]
- Samannan, R.; Holt, G.; Calderon-Candelario, R.; Mirsaeidi, M.; Campos, M. Effect of Face Masks on Gas Exchange in Healthy Persons and Patients with Chronic Obstructive Pulmonary Disease. Ann. ATS 2021, 18, 539–541. [Google Scholar] [CrossRef]
- Roberge, R.J.; Bayer, E.; Powell, J.B.; Coca, A.; Roberage, M.R.; Benson, S.M. Efect of exhaled moisture on breathing resistance of N95 filtering facepiece respirators. Ann. Occup. Hyg. 2010, 54, 671–677. [Google Scholar] [CrossRef] [Green Version]
- İpek, S.; Yurttutan, S.; Güllü, U.U.; Dalkıran, T.; Acıpayam, C.; Doğaner, A. Is N95 face mask linked to dizziness and headache? Int. Arch. Occup. Environ. Health 2021, 94, 1627–1636. [Google Scholar] [CrossRef] [PubMed]
- Saran, S.; Gurjar, M.; Baronia, A.; Sivapurapu, V.; Ghosh, P.S.; Raju, G.M.; Maurya, I. Heating, ventilation and air conditioning (HVAC) in intensive care unit. Crit. Care 2020, 24, 194. [Google Scholar] [CrossRef]
- Riebl, S.K.; Davy, B.M. The Hydration Equation: Update on Water Balance and Cognitive Performance. ACSMs Health Fit. J. 2013, 17, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Holdsworth, J.E. The importance of human hydration: Perceptions among health care professionals across Europe. Nutr. Bull. 2012, 37, 16–24. [Google Scholar] [CrossRef]
- El-Sharkawy, A.M.; Bragg, D.; Watson, P.; Neal, K.; Sahota, O.; Maughan, R.J.; Lobo, D.N. Hydration amongst nurses and doctors on-call (the HANDS on prospective cohort study). Clin. Nutr. 2016, 35, 935–942. [Google Scholar] [CrossRef] [PubMed]
- Mustofa, N.D. Hydration and nutrition concerns among healthcare workers on full personal protective equipment (PPE) in Covid-19 wards. Clin. Nutr. ESPEN 2020, 40, 616. [Google Scholar] [CrossRef]
| Variables | |
|---|---|
| Age (years) | 28 [24; 43] |
| Body weight (kg) | 70 [65; 78] |
| Body height (cm) | 170 [164; 177] |
| Gender | |
| Female | 74 (67%) |
| Male | 36 (33%) |
| Profession | |
| Nurses | 63 (57%) |
| Paramedics | 47 (43%) |
| Co-morbidities | |
| Cardiovascular system | 4 (4%) |
| Smoking | 42 (38%) |
| Working in an isolation ward (minutes) | 240 [180; 360] |
| Number of entries into isolation ward | |
| One | 68 (62%) |
| Two | 34 (31%) |
| Three | 7 (6%) |
| Four | 1 (1%) |
| Medical protective mask | |
| P2 | 32 (29%) |
| P3 half-face | 30 (27%) |
| P3 full-face | 48 (44%) |
| Parameter | Before (n = 110) | After (n = 110) | Z | p Value |
|---|---|---|---|---|
| pH | 7.42 (7.40; 7.43) | 7.41 (7.39; 7.42) | 1.29 | 0.19 |
| pO2 (mm Hg) | 75.45 (68.40; 81.70) | 76.10 (70.70; 82.20) | 1.44 | 0.15 |
| pCO2 (mm Hg) | 37.70 (35.40; 40.00) | 37.90 (35.80; 40.50) | 0.57 | 0.56 |
| HCO3 (mmol/L) | 24.10 (22.90; 25.20) | 23.85 (22.40; 25.00) | 0.16 | 0.87 |
| SaO2 (%) | 96.25 (94.40; 99.00) | 96.00 (94.20; 98.00) | 1.07 | 0.28 |
| BE (mEq/L) | −0.4 (−1.60; 0.60) | −0.50 (−1.90; 0.50) | 0.35 | 0.72 |
| Variables | No | Yes | χ2 | p Value |
|---|---|---|---|---|
| Gender | ||||
| Female | 54 (73%) | 20 (27%) | 0.46 | 0.49 |
| Male | 24 (67%) | 12 (33%) | ||
| Profession | ||||
| Nurses | 35 (56%) | 28 (44%) | 18.73 | 0.00002 |
| Paramedics | 43 (91%) | 4 (9%) | ||
| Co-morbidities | 31 (67%) | 15 (33%) | 0.47 | 0.49 |
| Medical protective mask | ||||
| FFP2 | 23 (72%) | 9 (28%) | 0.20 | 0.90 |
| FFP3 half-face | 22 (73%) | 8 (27%) | ||
| FFP3 full-face | 33 (69%) | 15 (31%) | ||
| Number of entries into isolation ward | ||||
| 1 | 51 (75%) | 17 (25%) | 1.44 | 0.23 |
| >1 | 27 (64%) | 15 (36%) |
| Variables | B | SE (B) | Wald Test | p | OR (Cl 95%) |
|---|---|---|---|---|---|
| Profession nurse vs. paramedic | 2.15 | 0.58 | 13.72 | 0.0002 | 8.6 (2.75 to 26.86) |
| Age | 0.05 | 0.02 | 6.31 | 0.012 | 1.05 (1.01 to 1.08) |
| Body weight | 0.01 | 0.02 | 0.57 | 0.45 | 1.01 (0.98 to 1.05 |
| Body height | −0.01 | 0.01 | 1.23 | 0.27 | 0.98 (0.96 to 1.01 |
| Gender | 0.3 | 0.44 | 0.46 | 0.49 | 1.35 (057 to 3.18) |
| Smoking | −0.07 | 0.43 | 0.02 | 0.87 | 0.93 (0.39 to 2.19) |
| Time of working in an isolation ward | −0.003 | 0.002 | 1.51 | 0.21 | 0.99 (0.99 to 1.00) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mędrzycka-Dąbrowska, W.; Ślęzak, D.; Robakowska, M.; Żuratyński, P.; Krzyżanowski, K.; Małecka-Dubiela, A.; Dąbrowski, S.; Zorena, K.; Lewandowska, K.; Ozga, D.; et al. Evaluation of Capillary Blood Gases in Medical Personnel Caring for Patients Isolated Due to SARS-CoV-2 in Intensive Care Units before and after Using Enhanced Filtration Masks: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 9425. https://doi.org/10.3390/ijerph18189425
Mędrzycka-Dąbrowska W, Ślęzak D, Robakowska M, Żuratyński P, Krzyżanowski K, Małecka-Dubiela A, Dąbrowski S, Zorena K, Lewandowska K, Ozga D, et al. Evaluation of Capillary Blood Gases in Medical Personnel Caring for Patients Isolated Due to SARS-CoV-2 in Intensive Care Units before and after Using Enhanced Filtration Masks: A Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(18):9425. https://doi.org/10.3390/ijerph18189425
Chicago/Turabian StyleMędrzycka-Dąbrowska, Wioletta, Daniel Ślęzak, Marlena Robakowska, Przemysław Żuratyński, Kamil Krzyżanowski, Anna Małecka-Dubiela, Sebastian Dąbrowski, Katarzyna Zorena, Katarzyna Lewandowska, Dorota Ozga, and et al. 2021. "Evaluation of Capillary Blood Gases in Medical Personnel Caring for Patients Isolated Due to SARS-CoV-2 in Intensive Care Units before and after Using Enhanced Filtration Masks: A Prospective Cohort Study" International Journal of Environmental Research and Public Health 18, no. 18: 9425. https://doi.org/10.3390/ijerph18189425








