Review: Prevalence of Addictions among Transgender and Gender Diverse Subgroups
Abstract
1. Introduction
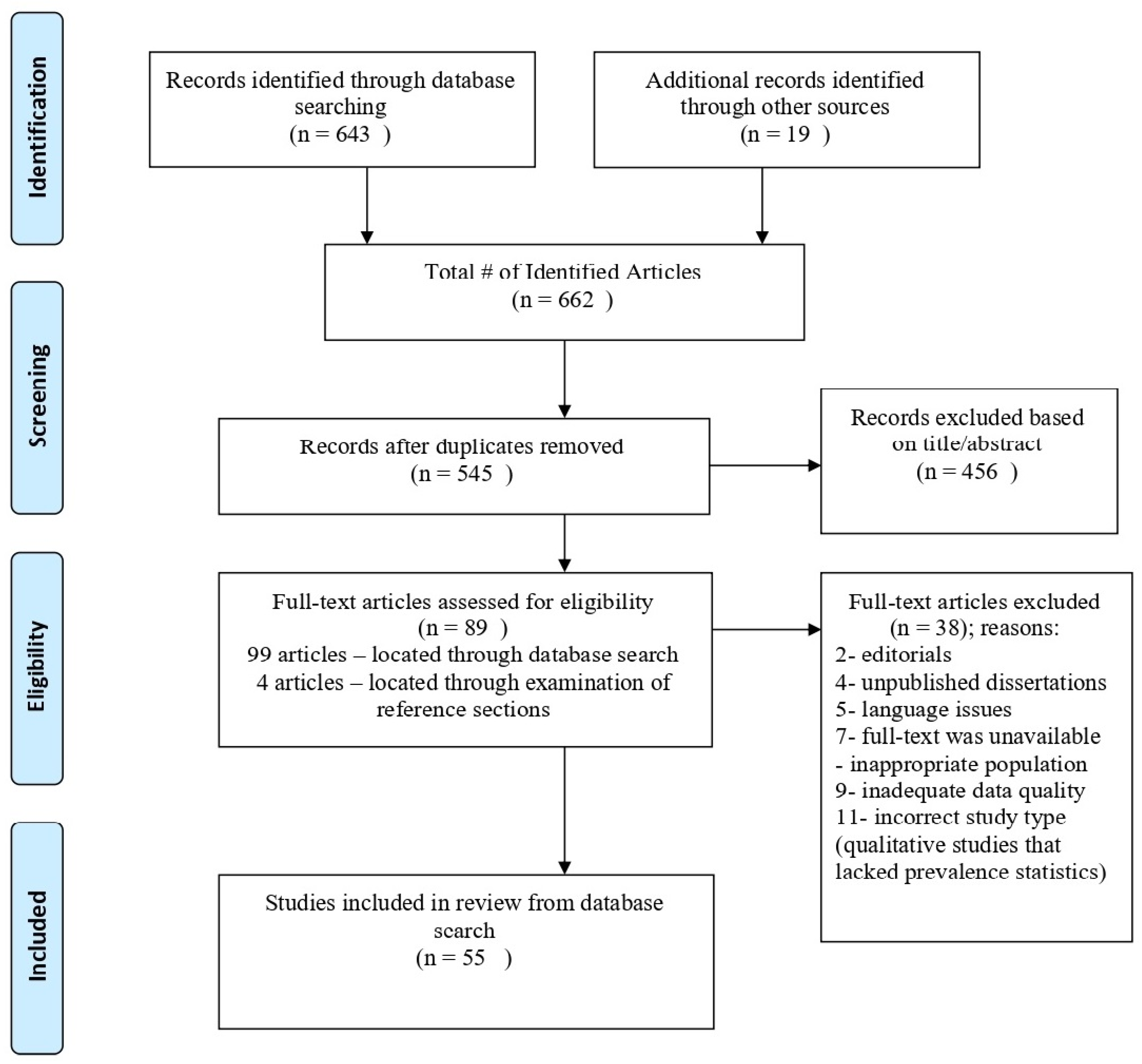
2. Methods
- The study samples included adult patients (defined as 18+ years of age) who identified as either transgender, gender nonbinary, and/or gender nonconforming.
- Studies addressed the prevalence of at least one SUD or behavioral addiction; proxies for addictions (i.e., heavy episodic drinking for AUD) were also considered.
- Studies included more than one TGD sub-population in the analysis and/or a cisgender reference group.
- Studies were peer-reviewed.
- Studies were written in English.
3. Results
3.1. Alcohol Use Disorders
3.1.1. Transgender Men
3.1.2. Transgender Women
3.1.3. Nonbinary Individuals
3.2. Nicotine Use Disorders
3.2.1. Transgender vs. Cisgender Sexual Minorities Subgroups
3.2.2. Transgender Men
3.2.3. Transgender Women
3.2.4. Nonbinary Individuals
3.3. Cannabis Use Disorders
3.3.1. Transgender Men
3.3.2. Transgender Women
3.3.3. Nonbinary Individuals
3.4. Illicit Drugs
3.4.1. Transgender Men
3.4.2. Transgender Women
3.4.3. Nonbinary Individuals
3.5. Behavioral Addictions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruppert, R.; Sussman, S.; Kattari, S.K. Prevalence and Co-Occurrence of Addictions among Sexual Minority Subgroups. Ann. LGBTQ Public Popul. Health 2020, 1, 210–248. [Google Scholar] [CrossRef]
- James, S.; Herman, J.; Rankin, S.; Keisling, M.; Mottet, L.; Anafi, M.A. The Report of the 2015 US Transgender Survey; National Center for Transgender Equality: Washington, DC, USA, 2016. [Google Scholar]
- Center for American Progress. Paying an Unfair Price: The Financial Penalty for Being Transgender in America; Movement Advancement Project; Center for American Progress: Washington, DC, USA, 2015. [Google Scholar]
- Pflum, S.R.; Testa, R.J.; Balsam, K.F.; Goldblum, P.B.; Bongar, B. Social support, trans community connectedness, and mental health symptoms among transgender and gender nonconforming adults. Psychol. Sex. Orientat. Gend. Divers. 2015, 2, 281–286. [Google Scholar] [CrossRef]
- Birtel, M.D.; Wood, L.; Kempa, N.J. Stigma and social support in substance abuse: Implications for mental health and well-being. Psychiatry Res. 2017, 252, 1–8. [Google Scholar] [CrossRef]
- Bockting, W.; Huang, C.-Y.; Ding, H.; Robinson, B.; Rosser, B.S. Are transgender persons at higher risk for HIV than other sexual minorities? A comparison of HIV prevalence and risks. Int. J. Transgend. 2005, 8, 123–131. [Google Scholar] [CrossRef]
- Chakrapani, V.; Newman, P.A.; Shunmugam, M.; Logie, C.H.; Samuel, M. Syndemics of depression, alcohol use, and victimisation, and their association with HIV-related sexual risk among men who have sex with men and transgender women in India. Glob. Public Health 2017, 12, 250–265. [Google Scholar] [CrossRef] [PubMed]
- Matsuno, E.; Budge, S. Non-binary/Genderqueer Identities: A Critical Review of the Literature. Curr. Sex. Health Rep. 2017, 9, 116–120. [Google Scholar] [CrossRef]
- Sussman, S.; Lisha, N.; Griffiths, M. Prevalence of the Addictions: A Problem of the Majority or the Minority? Eval. Health Prof. 2010, 34, 3–56. [Google Scholar] [CrossRef]
- Luczak, S.E.; Khoddam, R.; Yu, S.; Wall, T.L.; Schwartz, A.; Sussman, S. Prevalence and co-occurrence of addictions in US ethnic/racial groups: Implications for genetic research. Am. J. Addict. 2017, 26, 424–436. [Google Scholar] [CrossRef]
- American Psychiatric Association. Substance use disorders. In Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). Drinking Levels Defined. 2021. Available online: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking (accessed on 18 July 2021).
- Keuroghlian, A.; Reisner, S.L.; White, J.M.; Weiss, R.D. Substance use and treatment of substance use disorders in a community sample of transgender adults. Drug Alcohol Depend. 2015, 152, 139–146. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Vital signs: Binge drinking prevalence, frequency, and intensity among adults-United States, 2010. Morb. Mortal. Wkly. Rep. 2012, 61, 14–19. [Google Scholar]
- Christian, R.; Mellies, A.A.; Bui, A.G.; Lee, R.; Kattari, L.; Gray, C. Measuring the health of an invisible population: Lessons from the Colorado Transgender Health Survey. J. Gen. Intern. Med. 2018, 33, 1654–1660. [Google Scholar] [CrossRef]
- Day, J.K.; Fish, J.N.; Perez-Brumer, A.; Hatzenbuehler, M.L.; Russell, S.T. Transgender youth substance use disparities: Results from a population-based sample. J. Adolesc. Health 2017, 61, 729–735. [Google Scholar] [CrossRef]
- Blosnich, J.R.; Lehavot, K.; Glass, J.E.; Williams, E. Differences in Alcohol Use and Alcohol-Related Health Care Among Transgender and Nontransgender Adults: Findings From the 2014 Behavioral Risk Factor Surveillance System. J. Stud. Alcohol Drugs 2017, 78, 861–866. [Google Scholar] [CrossRef]
- Bradford, J.; Reisner, S.L.; Honnold, J.A.; Xavier, J. Experiences of transgender-related discrimination and implications for health: Results from the Virginia Transgender Health Initiative Study. Am. J. Public Health 2013, 103, 1820–1829. [Google Scholar] [CrossRef]
- Grant, B.F.; Goldstein, R.B.; Saha, T.D.; Chou, S.P.; Jung, J.; Zhang, H.; Hasin, D.S. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 2015, 72, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Coulter, R.W.; Blosnich, J.R.; Bukowski, L.A.; Herrick, A.; Siconolfi, D.E.; Stall, R.D. Differences in alcohol use and alcohol-related problems between transgender- and nontransgender-identified young adults. Drug Alcohol Depend. 2015, 154, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Peitzmeier, S.M.; Malik, M.; Kattari, S.K.; Marrow, E.; Stephenson, R.; Agénor, M.; Reisner, S.L. Intimate Partner Violence in Transgender Populations: Systematic Review and Meta-analysis of Prevalence and Correlates. Am. J. Public Health 2020, 110, e1–e14. [Google Scholar] [CrossRef] [PubMed]
- Scheim, A.I.; Bauer, G.R.; Shokoohi, M. Heavy episodic drinking among transgender persons: Disparities and predictors. Drug Alcohol Depend. 2016, 167, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Kcomt, L.; Evans-Polce, R.J.; Boyd, C.J.; McCabe, S.E. Association of transphobic discrimination and alcohol misuse among transgender adults: Results from the US Transgender Survey. Drug Alcohol Depend. 2020, 215, 108223. [Google Scholar] [CrossRef]
- Tomita, K.K.; Testa, R.J.; Balsam, K.F. Gender-affirming medical interventions and mental health in transgender adults. Psychol. Sex. Orientat. Gend. Divers. 2019, 6, 182–193. [Google Scholar] [CrossRef]
- Santos, G.M.; Rapues, J.; Wilson, E.C.; Macias, O.; Packer, T.; Colfax, G.; Raymond, H.F. Alcohol and substance use among transgender women in S an F rancisco: Prevalence and association with human immunodeficiency virus infection. Drug Alcohol Rev. 2014, 33, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Reback, C.J.; Fletcher, J.B. HIV Prevalence, Substance Use, and Sexual Risk Behaviors among Transgender Women Recruited Through Outreach. AIDS Behav. 2014, 18, 1359–1367. [Google Scholar] [CrossRef]
- Hotton, A.L.; Garofalo, R.; Kuhns, L.M.; Johnson, A.K. Substance Use as a Mediator of the Relationship between Life Stress and Sexual Risk among Young Transgender Women. AIDS Educ. Prev. 2013, 25, 62–71. [Google Scholar] [CrossRef]
- Restar, A.J.; Jin, H.; Ogunbajo, A.; Goedel, W.C.; Millett, G.; Sherwood, J.; Kuhns, L.; Reisner, S.L.; Garofalo, R.; Mimiaga, M.J. Prevalence and Risk Factors of Nonmedical Prescription Opioid Use among Transgender Girls and Young Women. JAMA Netw. Open 2020, 3, e201015. [Google Scholar] [CrossRef] [PubMed]
- Herrera, M.; Konda, K.; Leon, S.; Deiss, R.; Brown, B.; Calvo, G.; Salvatierra, H.; Caceres, C.; Klausner, J. Impact of alcohol use on sexual behavior among men who have sex with men and transgender women in Lima, Peru. Drug Alcohol Depend. 2016, 161, 147–154. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tupler, L.A.; Zapp, D.; DeJong, W.; Ali, M.; O’Rourke, S.; Looney, J.; Swartzwelder, H.S. Alcohol-related blackouts, negative alcohol-related consequences, and motivations for drinking reported by newly matriculating transgender college students. Alcohol. Clin. Exp. Res. 2017, 41, 1012–1023. [Google Scholar] [CrossRef]
- Azagba, S.; Latham, K.; Shan, L. Cigarette, smokeless tobacco, and alcohol use among transgender adults in the United States. Int. J. Drug Policy 2019, 73, 163–169. [Google Scholar] [CrossRef]
- Staples, J.M.; Neilson, E.C.; George, W.H.; Flaherty, B.; Davis, K.C. A descriptive analysis of alcohol behaviors across gender subgroups within a sample of transgender adults. Addict. Behav. 2018, 76, 355–362. [Google Scholar] [CrossRef]
- Newcomb, M.E.; Hill, R.; Buehler, K.; Ryan, D.T.; Whitton, S.W.; Mustanski, B. High Burden of Mental Health Problems, Substance Use, Violence, and Related Psychosocial Factors in Transgender, Non-Binary, and Gender Diverse Youth and Young Adults. Arch. Sex. Behav. 2020, 49, 645–659. [Google Scholar] [CrossRef]
- Delahanty, J.; Ganz, O.; Hoffman, L.; Guillory, J.; Crankshaw, E.; Farrelly, M. Tobacco use among lesbian, gay, bisexual and transgender young adults varies by sexual and gender identity. Drug Alcohol Depend. 2019, 201, 161–170. [Google Scholar] [CrossRef]
- Walsh, C.F.; O’Connell, R.P.; Kvach, E. Patterns of Healthcare Access and Utilization among Nonurban Transgender and Nonbinary Patients at a Large Safety Net Health System in Colorado. Ann. LGBTQ Public Popul. Health 2020, 1, 186–199. [Google Scholar] [CrossRef]
- Hoffman, L.; Delahanty, J.; Johnson, S.E.; Zhao, X. Sexual and gender minority cigarette smoking disparities: An analysis of 2016 Behavioral Risk Factor Surveillance System data. Prev. Med. 2018, 113, 109–115. [Google Scholar] [CrossRef]
- Kcomt, L.; Evans-Polce, R.J.; Veliz, P.T.; Boyd, C.J.; McCabe, S.E. Use of Cigarettes and E-Cigarettes/Vaping among Transgender People: Results from the 2015 U.S. Transgender Survey. Am. J. Prev. Med. 2020, 59, 538–547. [Google Scholar] [CrossRef]
- Rath, J.M.; Villanti, A.C.; Rubenstein, B.R.A.; Vallone, D.M. Tobacco Use by Sexual Identity among Young Adults in the United States. Nicotine Tob. Res. 2013, 15, 1822–1831. [Google Scholar] [CrossRef]
- Rimes, K.A.; Goodship, N.; Ussher, G.; Baker, D.; West, E. Non-binary and binary transgender youth: Comparison of mental health, self-harm, suicidality, substance use and victimization experiences. Int. J. Transgend. 2017, 20, 230–240. [Google Scholar] [CrossRef] [PubMed]
- Gerend, M.A.; Newcomb, M.E.; Mustanski, B. Prevalence and correlates of smoking and e-cigarette use among young men who have sex with men and transgender women. Drug Alcohol Depend. 2017, 179, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Benotsch, E.G.; Zimmerman, R.; Cathers, L.; McNulty, S.; Pierce, J.; Heck, T.; Perrin, P.; Snipes, D. Non-medical use of prescription drugs, polysubstance use, and mental health in transgender adults. Drug Alcohol Depend. 2013, 132, 391–394. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, C.A.; Gallego, J.D.; Bockting, W.O. Demographic Characteristics, Components of Sexuality and Gender, and Minority Stress and Their Associations to Excessive Alcohol, Cannabis, and Illicit (Noncannabis) Drug Use among a Large Sample of Transgender People in the United States. J. Prim. Prev. 2017, 38, 419–445. [Google Scholar] [CrossRef] [PubMed]
- Beckwith, N.; Reisner, S.L.; Zaslow, S.; Mayer, K.H.; Keuroghlian, A.S. Factors Associated with Gender-Affirming Surgery and Age of Hormone Therapy Initiation Among Transgender Adults. Transgender Health 2017, 2, 156–164. [Google Scholar] [CrossRef]
- Reback, C.J.; Clark, K.; Holloway, I.W.; Fletcher, J.B. Health disparities, risk behaviors and healthcare utilization among transgender women in Los Angeles County: A comparison from 1998–1999 to 2015–2016. AIDS Behav. 2018, 22, 2524–2533. [Google Scholar] [CrossRef]
- McLaughlin, K.; Hatzenbuehler, M.L.; Xuan, Z.; Conron, K.J. Disproportionate exposure to early-life adversity and sexual orientation disparities in psychiatric morbidity. Child Abus. Negl. 2012, 36, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Corliss, H.L.; Rosario, M.; Wypij, D.; Wylie, S.A.; Frazier, A.L.; Austin, S.B. Sexual orientation and drug use in a longitudinal cohort study of U.S. adolescents. Addict. Behav. 2010, 35, 517–521. [Google Scholar] [CrossRef]
- Su, D.; Irwin, J.A.; Fisher, C.; Ramos, A.; Kelley, M.; Mendoza, D.A.R.; Coleman, J.D. Mental Health Disparities Within the LGBT Population: A Comparison Between Transgender and Nontransgender Individuals. Transgender Health 2016, 1, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Horvath, K.J.; Iantaffi, A.; Swinburne-Romine, R.; Bockting, W. A Comparison of Mental Health, Substance Use, and Sexual Risk Behaviors between Rural and Non-Rural Transgender Persons. J. Homosex. 2014, 61, 1117–1130. [Google Scholar] [CrossRef]
- Reisner, S.L.; Biello, K.B.; Hughto JM, W.; Kuhns, L.; Mayer, K.H.; Garofalo, R.; Mimiaga, M.J. Psychiatric diagnoses and comorbidities in a diverse, multicity cohort of young transgender women: Baseline findings from project lifeskills. JAMA Pediatrics 2016, 170, 481–486. [Google Scholar] [CrossRef]
- Reisner, S.L.; Gamarel, K.E.; Nemoto, T.; Operario, D. Dyadic effects of gender minority stressors in substance use behaviors among transgender women and their non-transgender male partners. Psychol. Sex. Orientat. Gend. Divers. 2014, 1, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, R.S.; Benotsch, E.G.; Shoemaker, S.; Snipes, D.J.; Cathers, L.; Perrin, P.B.; McMillan, D.; Pierce, J.; McNulty, S.; Heck, T. Mediational models linking psychosocial context, mental health problems, substance use, and HIV risk behaviors in transgender women. Health Psychol. Behav. Med. 2015, 3, 379–390. [Google Scholar] [CrossRef]
- Stephens, S.C.; Bernstein, K.T.; Philip, S.S. Male to Female and Female to Male Transgender Persons have Different Sexual Risk Behaviors Yet Similar Rates of STDs and HIV. AIDS Behav. 2011, 15, 683–686. [Google Scholar] [CrossRef]
- Scheim, A.I.; Bauer, G.R.; Shokoohi, M. Drug use among transgender people in Ontario, Canada: Disparities and associations with social exclusion. Addict. Behav. 2017, 72, 151–158. [Google Scholar] [CrossRef]
- Rider, G.N.; McMorris, B.J.; Gower, A.L.; Coleman, E.; Eisenberg, M.E. Gambling behaviors and problem gambling: A population-based comparison of transgender/gender diverse and cisgender adolescents. J. Gambl. Stud. 2019, 35, 79–92. [Google Scholar] [CrossRef]
- Mathy, R.M. Transgender identity and suicidality in a nonclinical sample: Sexual orientation, psychiatric history, and compulsive behaviors. J. Psychol. Hum. Sex. 2003, 14, 47–65. [Google Scholar] [CrossRef]
- Peterson, C.M.; Mara, C.A.; Conard, L.A.E.; Grossoehme, D. The relationship of the UPPS model of impulsivity on bulimic symptoms and non-suicidal self-injury in transgender youth. Eat. Behav. 2020, 39, 101416. [Google Scholar] [CrossRef] [PubMed]
- Linsenmeyer, W.; Reed, J.; Giedinghagen, A.; Lewis, C.; Garwood, S. Nutrition Considerations for Transgender Adolescents and Young Adults: Screening for Disordered Eating and Food Insecurity at a Midwestern Transgender Center. Curr. Dev. Nutr. 2020, 4 (Suppl. 2), 1130. [Google Scholar] [CrossRef]
- Lipson, S.; Sonneville, K. Eating disorder symptoms among undergraduate and graduate students at 12 U.S. colleges and universities. Eat. Behav. 2017, 24, 81–88. [Google Scholar] [CrossRef] [PubMed]
- White, M.; Potenza, M.N. Binge Eating Disorder and Food Addiction. Curr. Drug Abus. Rev. 2011, 4, 201–207. [Google Scholar] [CrossRef]
- Nagata, J.M.; Murray, S.B.; Compte, E.J.; Pak, E.H.; Schauer, R.; Flentje, A.; Capriotti, M.R.; Lubensky, M.E.; Lunn, M.R.; Obedin-Maliver, J. Community norms for the Eating Disorder Examination Questionnaire (EDE-Q) among transgender men and women. Eat. Behav. 2020, 37, 101381. [Google Scholar] [CrossRef] [PubMed]
- Watson, R.J.; Veale, J.F.; Saewyc, E.M. Disordered eating behaviors among transgender youth: Probability profiles from risk and protective factors. Int. J. Eat. Disord. 2017, 50, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Stevens, C.; Zhang, E.; Cherkerzian, S.; Chen, J.A.; Liu, C.H. Problematic internet use/computer gaming among US college students: Prevalence and correlates with mental health symptoms. Depress. Anxiety 2020, 37, 1127–1136. [Google Scholar] [CrossRef]
- Gansner, M.; Nisenson, M.; Carson, N.; Torous, J. A pilot study using ecological momentary assessment via smartphone application to identify adolescent problematic internet use. Psychiatry Res. 2020, 293, 113428. [Google Scholar] [CrossRef]
- Coleman, E. Is your patient suffering from compulsive sexual behavior? Psychiatric Annals 1992, 22, 320–325. [Google Scholar] [CrossRef]
- Carnes, P. Don’t Call It Love: Recovery from Sexual Addiction; Bantam: New York, NY, USA, 1992. [Google Scholar]
- Walton, M.T.; Bhullar, N. Hypersexuality, higher rates of intercourse, masturbation, sexual fantasy, and early sexual interest relate to higher sexual excitation/arousal. Arch. Sex. Behav. 2018, 47, 2177–2183. [Google Scholar] [CrossRef] [PubMed]
- Schvey, N.A.; Klein, D.A.; Pearlman, A.T.; Riggs, D.S. A Descriptive Study of Transgender Active Duty Service Members in the U.S. Military. Transgender Health 2020, 5, 149–157. [Google Scholar] [CrossRef]
- Witcomb, G.L.; Bouman, W.P.; Brewin, N.; Richards, C.; Fernandez-Aranda, F.; Arcelus, J. Body image dissatisfaction and eating-related psychopathology in trans individuals: A matched control study. Eur. Eat. Disord. Rev. 2015, 23, 287–293. [Google Scholar] [CrossRef]
- Amodeo, A.L.; Esposito, C.; Antuoni, S.; Saracco, G.; Bacchini, D. Muscle dysmorphia: What about transgender people? Cult. Health Sex. 2020, 1–16. [Google Scholar] [CrossRef]
- Klein, V.; Briken, P.; Schröder, J.; Fuss, J. Mental health professionals’ pathologization of compulsive sexual behavior: Does clients’ gender and sexual orientation matter? J. Abnorm. Psychol. 2019, 128, 465. [Google Scholar] [CrossRef]
- Rood, B.A.; Reisner, S.L.; Surace, F.; Puckett, J.A.; Maroney, M.R.; Pantalone, D.W. Expecting Rejection: Understanding the Minority Stress Experiences of Transgender and Gender-Nonconforming Individuals. Transgender Health 2016, 1, 151–164. [Google Scholar] [CrossRef]
- Lefevor, G.T.; Boyd-Rogers, C.C.; Sprague, B.M.; Janis, R.A. Health disparities between genderqueer, transgender, and cisgender individuals: An extension of minority stress theory. J. Couns. Psychol. 2019, 66, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Shipherd, J.C.; Berke, D.; Livingston, N.A. Trauma Recovery in the Transgender and Gender Diverse Community: Extensions of the Minority Stress Model for Treatment Planning. Cogn. Behav. Pract. 2019, 26, 629–646. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruppert, R.; Kattari, S.K.; Sussman, S. Review: Prevalence of Addictions among Transgender and Gender Diverse Subgroups. Int. J. Environ. Res. Public Health 2021, 18, 8843. https://doi.org/10.3390/ijerph18168843
Ruppert R, Kattari SK, Sussman S. Review: Prevalence of Addictions among Transgender and Gender Diverse Subgroups. International Journal of Environmental Research and Public Health. 2021; 18(16):8843. https://doi.org/10.3390/ijerph18168843
Chicago/Turabian StyleRuppert, Ryan, Shanna K. Kattari, and Steve Sussman. 2021. "Review: Prevalence of Addictions among Transgender and Gender Diverse Subgroups" International Journal of Environmental Research and Public Health 18, no. 16: 8843. https://doi.org/10.3390/ijerph18168843
APA StyleRuppert, R., Kattari, S. K., & Sussman, S. (2021). Review: Prevalence of Addictions among Transgender and Gender Diverse Subgroups. International Journal of Environmental Research and Public Health, 18(16), 8843. https://doi.org/10.3390/ijerph18168843






