Self-Compassion and Rumination Type Mediate the Relation between Mindfulness and Parental Burnout
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Data Analyses
3. Results
3.1. Sample Characteristics
3.2. Descriptive Statistics at Time 1
3.3. Descriptive Statistics at Time 2
3.4. Mindfulness Practice Effect on Trait Mindfulness at T1 and T2
3.5. The Role of Trait Mindfulness on Parental Burnout, Self-Compassion and Rumination Type
3.6. The Role of Self-Compassion and Rumination Type on Parental Burnout
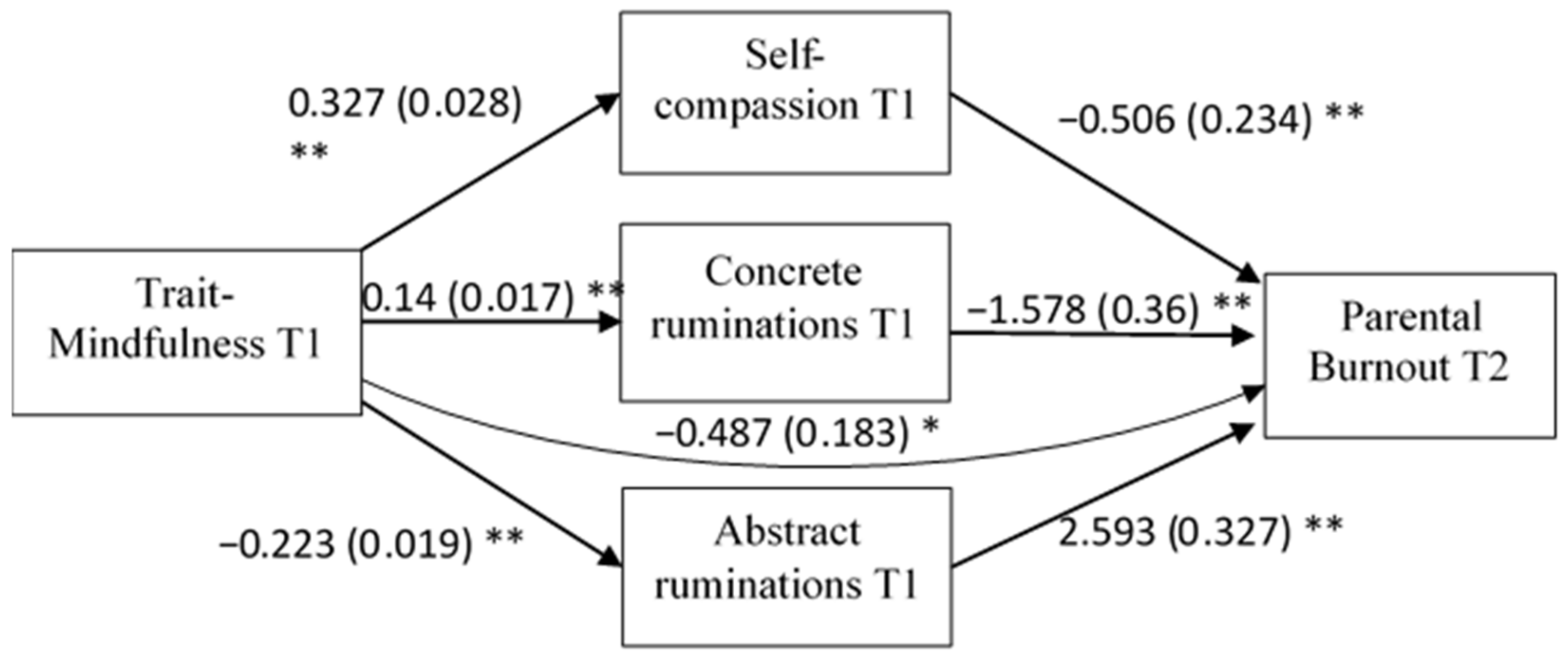
3.7. The Mediating Role of Self-Compassion and Rumination Type on the Relationship between Trait-Mindfulness and Parental Burnout
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Lindström, C.; Åman, J.; Norberg, A.L. Parental burnout in relation to sociodemographic, psychosocial and personality factors as well as disease duration and glycaemic control in children with Type 1 diabetes mellitus. Acta Paediatr. 2011, 100, 1011–1017. [Google Scholar] [CrossRef]
- Roskam, I.; Brianda, M.E.; Mikolajczak, M. A Step Forward in the Conceptualization and Measurement of Parental Burnout: The Parental Burnout Assessment (PBA). Front. Psychol. 2018, 9, 758. [Google Scholar] [CrossRef]
- Mikolajczak, M.; Roskam, I. Parental burnout: Moving the focus from children to parents. New Dir. Child Adolesc. Dev. 2020, 2020, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Roskam, I.; Raes, M.E.; Mikolajczak, M. Exhausted Parents: Development and Preliminary Validation of the Parental Burnout Inventory. Front. Psychol. 2017, 8, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hallsten, L. Burnout and wornout: Concepts and data from a national survey. In Research Companion to Organizational Health Psychology; Edward Elgar Publishing Ltd.: Cheltenham, UK, 2005; pp. 516–536. [Google Scholar]
- Marchetti, D.; Fontanesi, L.; Mazza, C.; Di Giandomenico, S.; Roma, P.; Verrocchio, M.C. Parenting-Related Exhaustion during the Italian COVID-19 Lockdown. J. Pediatr. Psychol. 2020, 45, 1114–1123. [Google Scholar] [CrossRef] [PubMed]
- Fontanesi, L.; Marchetti, D.; Mazza, C.; Di Giandomenico, S.D.; Roma, P.; Verrocchio, M.C. The Effect of the COVID-19 Lockdown on Parents: A Call to Adopt Urgent Measures. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S79. [Google Scholar] [CrossRef] [PubMed]
- Griffith, A.K. Parental Burnout and Child Maltreatment during the COVID-19 Pandemic. J. Fam. Violence 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Mikolajczak, M.; Roskam, I. A Theoretical and Clinical Framework for Parental Burnout: The Balance between Risks and Resources (BR2). Front. Psychol. 2018, 9, 886. [Google Scholar] [CrossRef] [PubMed]
- de Abreu Costa, M.; de Oliveira, G.S.; Tatton-Ramos, T.; Manfro, G.G.; Salum, G.A. Anxiety and Stress-Related Disorders and Mindfulness-Based Interventions: A Systematic Review and Multilevel Meta-analysis and Meta-Regression of Multiple Outcomes. Mindfulness 2019, 10, 996–1005. [Google Scholar] [CrossRef]
- Joo, H.M.; Lee, S.J.; Chung, Y.G.; Shin, I.Y. Effects of Mindfulness Based Stress Reduction Program on Depression, Anxiety and Stress in Patients with Aneurysmal Subarachnoid Hemorrhage. J. Korean Neurosurg. Soc. 2010, 47, 345. [Google Scholar] [CrossRef] [PubMed]
- Keng, S.L.; Smoski, M.J.; Robins, C.J. Effects of mindfulness on psychological health: A review of empirical studies. Clin. Psychol. Rev. 2011, 31, 1041–1056. [Google Scholar] [CrossRef] [Green Version]
- Kuyken, W.; Watkins, E.; Holden, E.; White, K.; Taylor, R.S.; Byford, S.; Evans, A.; Radford, S.; Teasdale, J.D.; Dalgleish, T. How does mindfulness-based cognitive therapy work? Behav. Res. Ther. 2010, 48, 1105–1112. [Google Scholar] [CrossRef]
- Semple, R.J. Does Mindfulness Meditation Enhance Attention? A Randomized Controlled Trial. Mindfulness 2010, 1, 121–130. [Google Scholar] [CrossRef]
- Jha, A.P.; Krompinger, J.; Baime, M.J. Mindfulness training modifies subsystems of attention. Cogn. Affect. Behav. Neurosci. 2007, 7, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Segal, Z.V.; Williams, J.M.; Teasdale, J.D. Mindfulness-Based Cognitive Therapy for Depression; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Contemp. Psychol. A J. Rev. 1992, 37, 609. [Google Scholar] [CrossRef]
- Shankland, R.; Tessier, D.; Strub, L.; Gauchet, A.; Baeyens, C. Improving Mental Health and Well-Being through Informal Mindfulness Practices: An Intervention Study. Appl. Psychol. Health Well-Being 2021, 13, 63–83. [Google Scholar] [CrossRef]
- Kiken, L.G.; Garland, E.L.; Bluth, K.; Palsson, O.S.; Gaylord, S.A. From a state to a trait: Trajectories of state mindfulness in meditation during intervention predict changes in trait mindfulness. Pers. Individ. Dif. 2015, 81, 41–46. [Google Scholar] [CrossRef] [Green Version]
- Dillard, A.J.; Meier, B.P. Trait mindfulness is negatively associated with distress related to COVID-19. Pers. Individ. Dif. 2021, 179, 110955. [Google Scholar] [CrossRef]
- Zheng, M.X.; Masters-Waage, T.C.; Yao, J.; Lu, Y.; Tan, N.; Narayanan, J. Stay Mindful and Carry on: Mindfulness Neutralizes COVID-19 Stressors on Work Engagement via Sleep Duration. Front. Psychol. 2020, 11, 610156. [Google Scholar] [CrossRef] [PubMed]
- Anclair, M.; Lappalainen, R.; Muotka, J.; Hiltunen, A.J. Cognitive behavioural therapy and mindfulness for stress and burnout: A waiting list controlled pilot study comparing treatments for parents of children with chronic conditions. Scand. J. Caring Sci. 2018, 32, 389–396. [Google Scholar] [CrossRef] [Green Version]
- Cousineau, T.M.; Hobbs, L.M.; Arthur, K.C. The role of compassion and mindfulness in building parental resilience when caring for children with chronic conditions: A conceptual model. Front. Psychol. 2019, 10, 1602. [Google Scholar] [CrossRef] [Green Version]
- Brown, K.W.; Ryan, R.M.; Creswell, J.D. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychol. Inq. 2007, 18, 211–237. [Google Scholar] [CrossRef]
- Fall, E.; Shankland, R. The Mediating Role of Dispositional Mindfulness in the Relationship between Parental and Romantic Attachment. J. Adult Dev. 2021, 28, 126–137. [Google Scholar] [CrossRef]
- Deyo, M.; Wilson, K.A.; Ong, J.; Koopman, C. Mindfulness and Rumination: Does Mindfulness Training Lead to Reductions in the Ruminative Thinking Associated with Depression? Explor. J. Sci. Health 2009, 5, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Soysa, C.K.; Wilcomb, C.J. Mindfulness, Self-compassion, Self-efficacy, and Gender as Predictors of Depression, Anxiety, Stress, and Well-being. Mindfulness 2015, 6, 217–226. [Google Scholar] [CrossRef]
- Birnie, K.; Speca, M.; Carlson, L.E. Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR). Stress Health 2010, 26, 359–371. [Google Scholar] [CrossRef]
- Kemper, K.J.; Mo, X.; Khayat, R. Are mindfulness and self-compassion associated with sleep and resilience in health professionals? J. Altern. Complement. Med. 2015, 21, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Keng, S.L.; Smoski, M.J.; Robins, C.J.; Ekblad, A.G.; Brantley, J.G. Mechanisms of change in mindfulness-based stress reduction: Self-compassion and mindfulness as mediators of intervention outcomes. J. Cogn. Psychother. 2012, 26, 270–280. [Google Scholar] [CrossRef]
- Svendsen, J.L.; Kvernenes, K.V.; Wiker, A.S.; Dundas, I. Mechanisms of mindfulness: Rumination and self-compassion. Nord. Psychol. 2017, 69, 71–82. [Google Scholar] [CrossRef]
- Neff, K. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity 2003, 2, 85–101. [Google Scholar] [CrossRef] [Green Version]
- Van Dam, N.T.; Sheppard, S.C.; Forsyth, J.P.; Earleywine, M. Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. J. Anxiety Disord. 2011, 25, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Sorkkila, M.; Aunola, K. Risk Factors for Parental Burnout among Finnish Parents: The Role of Socially Prescribed Perfectionism. J. Child Fam. Stud. 2020, 29, 648–659. [Google Scholar] [CrossRef] [Green Version]
- McLaughlin, K.A.; Nolen-Hoeksema, S. Rumination as a transdiagnostic factor in depression and anxiety. Behav. Res. Ther. 2011, 49, 186–193. [Google Scholar] [CrossRef] [Green Version]
- Nolen-Hoeksema, S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. J. Abnorm. Psychol. 2000, 109, 504–511. [Google Scholar] [CrossRef]
- Watkins, E.; Moulds, M. Distinct modes of ruminative self-focus: Impact of abstract versus concrete rumination on problem solving in depression. Emotion 2005, 5, 319–328. [Google Scholar] [CrossRef]
- Douilliez, C.; Heeren, A.; Lefèvre, N.; Watkins, E.; Barnard, P.; Philippot, P. Validation de la version française d’un questionnaire évaluant les pensées répétitives constructives et non constructives. Can. J. Behav. Sci. 2013, 46, 185–192. [Google Scholar] [CrossRef] [Green Version]
- Moreira, H.; Canavarro, M.C. The Association between Self-Critical Rumination and Parenting Stress: The Mediating Role of Mindful Parenting. J. Child Fam. Stud. 2018, 27, 2265–2275. [Google Scholar] [CrossRef]
- Gouveia, M.J.; Carona, C.; Canavarro, M.C.; Moreira, H. Self-Compassion and Dispositional Mindfulness Are Associated with Parenting Styles and Parenting Stress: The Mediating Role of Mindful Parenting. Mindfulness 2016, 7, 700–712. [Google Scholar] [CrossRef]
- Frostadottir, A.D.; Dorjee, D. Effects of mindfulness based cognitive therapy (MBCT) and compassion focused therapy (CFT) on symptom change, mindfulness, self-compassion, and rumination in clients with depression, anxiety, and stress. Front. Psychol. 2019, 10, 1099. [Google Scholar] [CrossRef] [PubMed]
- Erdfelder, E.; Faul, F.; Buchner, A. GPOWER: A general power analysis program. Behav. Res. Methods Instrum. Comput. 1996, 28, 1–11. [Google Scholar] [CrossRef]
- Brown, K.W.; Ryan, R.M. The Benefits of Being Present: Mindfulness and Its Role in Psychological Well-Being. J. Pers. Soc. Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, T.; Reilly-Spong, M.; Gross, C.R. Mindfulness: A systematic review of instruments to measure an emergent patient-reported outcome (PRO). Qual. Life Res. 2013, 22, 2639–2659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neff, K.D. Self-Compassion Scale. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Barnard, P.; Watkins, E.; Mackintosh, B.; Nimmo-Smith, I. Getting stuck in a mental rut: Some process and experiential attributes. In Proceedings of the 35th Congress of the British Association for Behavioural and Cognitive Psychotherapies, Brighton, UK, 12–14 September 2007. [Google Scholar]
- The Jamovi Project (2021). Jamovi (Version 1.6) [Computer Software]. Sidney, Australia. Available online: https://www.jamovi.org (accessed on 18 August 2021).
- Raes, F.; Pommier, E.; Neff, K.D.; Van Gucht, D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin. Psychol. Psychother. 2011, 18, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Bögels, S.M.; Hellemans, J.; van Deursen, S.; Römer, M.; van der Meulen, R. Mindful parenting in mental health care: Effects on parental and child psychopathology, parental stress, parenting, coparenting, and marital functioning. Mindfulness 2014, 5, 536–551. [Google Scholar] [CrossRef]
- Neece, C.L. Mindfulness-based stress reduction for parents of young children with developmental delays: Implications for parental mental health and child behavior problems. J. Appl. Res. Intellect. Disabil. 2014, 27, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Parent, J.; McKee, L.G.; Rough, J.N.; Forehand, R. The Association of Parent Mindfulness with Parenting and Youth Psychopathology Across Three Developmental Stages. J. Abnorm. Child Psychol. 2016, 44, 191–202. [Google Scholar] [CrossRef]
- Corthorn, C.; Milicic, N. Mindfulness and Parenting: A Correlational Study of Non-meditating Mothers of Preschool Children. J. Child Fam. Stud. 2016, 25, 1672–1683. [Google Scholar] [CrossRef]
- Gershy, N.; Meehan, K.B.; Omer, H.; Papouchis, N.; Schorr Sapir, I. Randomized Clinical Trial of Mindfulness Skills Augmentation in Parent Training. Child Youth Care Forum 2017, 46, 783–803. [Google Scholar] [CrossRef]
- Turpyn, C.C.; Chaplin, T.M. Mindful Parenting and Parents’ Emotion Expression: Effects on Adolescent Risk Behaviors. Mindfulness 2016, 7, 246–254. [Google Scholar] [CrossRef] [Green Version]
- Bogels, S.M.; Emerson, L.M. The mindful family: A systemic approach to mindfulness, relational functioning, and somatic and mental health. Curr. Opin. Psychol. 2019, 28, 138–142. [Google Scholar] [CrossRef] [Green Version]
- Harnett, P.H.; Dawe, S. The contribution of mindfulness-based therapies for children and families and proposed conceptual integration. Child Adolesc. Ment. Health 2012, 17, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Bishop, S.R.; Lau, M.; Shapiro, S.; Carlson, L.; Anderson, N.D.; Carmody, J.; Segal, Z.V.; Abbey, S.; Speca, M.; Velting, D.; et al. Mindfulness: A proposed operational definition. Clin. Psychol. Sci. Pract. 2004, 11, 230–241. [Google Scholar] [CrossRef]
- Raes, F.; Williams, J.M. The Relationship between Mindfulness and Uncontrollability of Ruminative Thinking. Mindfulness 2010, 1, 199–203. [Google Scholar] [CrossRef]
- Freudenthaler, L.; Turba, J.D.; Tran, U.S. Emotion Regulation Mediates the Associations of Mindfulness on Symptoms of Depression and Anxiety in the General Population. Mindfulness 2017, 8, 1339–1344. [Google Scholar] [CrossRef] [Green Version]
- Hill, A.P.; Hall, H.K.; Appleton, P.R.; Kozub, S.A. Perfectionism and burnout in junior elite soccer players: The mediating influence of unconditional self-acceptance. Psychol. Sport Exerc. 2008, 9, 630–644. [Google Scholar] [CrossRef]
- Kotsou, I.; Leys, C.; Fossion, P. Acceptance alone is a better predictor of psychopathology and well-being than emotional competence, emotion regulation and mindfulness. J. Affect. Disord. 2018, 226, 142–145. [Google Scholar] [CrossRef]
- Prikhidko, A.; Long, H.; Wheaton, M.G. The Effect of Concerns about COVID-19 on Anxiety, Stress, Parental Burnout, and Emotion Regulation: The Role of Susceptibility to Digital Emotion Contagion. Front. Public Health 2020, 8, 894. [Google Scholar] [CrossRef]
- Le Vigouroux, S.; Scola, C.; Raes, M.E.; Mikolajczak, M.; Roskam, I. The big five personality traits and parental burnout: Protective and risk factors. Pers. Individ. Dif. 2017, 119, 216–219. [Google Scholar] [CrossRef]
- Brianda, M.E.; Roskam, I.; Gross, J.J.; Franssen, A.; Kapala, F.; Gérard, F.; Mikolajczak, M. Treating Parental Burnout: Impact of Two Treatment Modalities on Burnout Symptoms, Emotions, Hair Cortisol, and Parental Neglect and Violence. Psychother. Psychosom. 2020, 89, 330–332. [Google Scholar] [CrossRef] [PubMed]
- Flett, G.L.; Nepon, T.; Hewitt, P.L. Perfectionism, Worry, and Rumination in Health and Mental Health: A Review and a Conceptual Framework for a Cognitive Theory of Perfectionism. In Perfectionism, Health, and Well-Being; Sirois, F.M., Molnar, D.S., Eds.; Springer International Publishing/Springer Nature: Berlin/Heidelberg, Germany, 2016; pp. 121–155. [Google Scholar] [CrossRef]
- Michl, L.C.; McLaughlin, K.A.; Shepherd, K.; Nolen-Hoeksema, S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: Longitudinal evidence in early adolescents and adults. J. Abnorm. Psychol. 2013, 122, 339–352. [Google Scholar] [CrossRef] [Green Version]
- Potter, R.F.; Yar, K.; Francis, A.J.; Schuster, S. Self-compassion mediates the relationship between parental criticism and social anxiety. Int. J. Psychol. Psychol. Ther. 2014, 14, 33–43. [Google Scholar]
- Coyne, L.W.; Gould, E.R.; Grimaldi, M.; Wilson, K.G.; Baffuto, G.; Biglan, A. First Things First: Parent Psychological Flexibility and Self-Compassion during COVID-19. Behav. Anal. Pract. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Neff, K.D.; McGehee, P. Self-compassion and psychological resilience among adolescents and young adults. Self Identity 2010, 9, 225–240. [Google Scholar] [CrossRef]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 2020, 63, e32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; Yang, Z.; Qiu, H.; Wang, Y.; Jian, L.; Ji, J.; Li, K. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry 2020, 19, 249–250. [Google Scholar] [CrossRef]
- Gorwood, P.; Fiorillo, A. One year after the COVID-19: What have welearnt, what shall we do next? Eur. Psychiatry 2020, 64, e15. [Google Scholar] [CrossRef] [PubMed]
- Ghebreyesus, A. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry 2020, 19, 129–130. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Neff, K.D.; Germer, C.K. A Pilot Study and Randomized Controlled Trial of the Mindful Self-Compassion Program. J. Clin. Psychol. 2013, 69, 28–44. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, P.; Procter, S. Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clin. Psychol. Psychother. 2006, 13, 353–379. [Google Scholar] [CrossRef]
| Variable | n | M | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|---|
| 1. Trait mindfulness | 459 | 55.8 | 8.94 | — | ||||
| 2. Parental burnout | 459 | 40.5 | 34.9 | −0.471 * | — | |||
| 3. Self-compassion | 459 | 22.4 | 6.04 | 0.584 * | −0.462 * | — | ||
| 4. Abstract ruminations | 459 | 17.8 | 4.28 | −0.466 * | 0.588 * | −0.571 * | — | |
| 5. Concrete ruminations | 459 | 16.4 | 3.61 | 0.347 * | −0.503 * | 0.477 * | −0.432 * | — |
| Variable | n | M | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|---|
| 1. Trait mindfulness | 459 | 55.6 | 8.84 | — | ||||
| 2. Parental burnout | 459 | 35 | 32.8 | −0.525 * | — | |||
| 3. Self-compassion | 459 | 22.8 | 6.18 | 0.499 * | −0.489 * | — | ||
| 4. Abstract ruminations | 459 | 15.7 | 3.71 | −0.491 * | 0.567 * | −0.575 * | — | |
| 5. Concrete ruminations | 459 | 18 | 3.75 | 0.403 * | −0.445 * | 0.484 * | −0.324 * | — |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paucsik, M.; Urbanowicz, A.; Leys, C.; Kotsou, I.; Baeyens, C.; Shankland, R. Self-Compassion and Rumination Type Mediate the Relation between Mindfulness and Parental Burnout. Int. J. Environ. Res. Public Health 2021, 18, 8811. https://doi.org/10.3390/ijerph18168811
Paucsik M, Urbanowicz A, Leys C, Kotsou I, Baeyens C, Shankland R. Self-Compassion and Rumination Type Mediate the Relation between Mindfulness and Parental Burnout. International Journal of Environmental Research and Public Health. 2021; 18(16):8811. https://doi.org/10.3390/ijerph18168811
Chicago/Turabian StylePaucsik, Marine, Agata Urbanowicz, Christophe Leys, Ilios Kotsou, Céline Baeyens, and Rebecca Shankland. 2021. "Self-Compassion and Rumination Type Mediate the Relation between Mindfulness and Parental Burnout" International Journal of Environmental Research and Public Health 18, no. 16: 8811. https://doi.org/10.3390/ijerph18168811
APA StylePaucsik, M., Urbanowicz, A., Leys, C., Kotsou, I., Baeyens, C., & Shankland, R. (2021). Self-Compassion and Rumination Type Mediate the Relation between Mindfulness and Parental Burnout. International Journal of Environmental Research and Public Health, 18(16), 8811. https://doi.org/10.3390/ijerph18168811






