Distancing Adherence and Negative Emotions among the Israeli Elderly Population during the COVID-19 Pandemic
Abstract
:1. Introduction
- Adherence to distancing instructions will be associated with attitudes, subjective norms, and threat perception regarding COVID-19. Higher threat perception and more positive attitudes and subjective norms towards adherence to instructions will be associated with better adherence.
- Emotional levels will be associated with levels of social support. Higher social support may regulate negative emotions.
- Attitudes and subjective norms will act as mediating factors in the association between threat perception, trust and social support, and distancing adherence and negative emotions.
2. Materials and Methods
2.1. Measures
2.2. Data Analysis
3. Results
4. Discussion
4.1. Adhering to Distancing Instructions
4.2. Negative-Emotion Regulation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Coronavirus Disease (COVID-19) Pandemic, 2020. Available online: https://www.who.int/health-opics/coronavirus#tab=tab_1 (accessed on 20 May 2020).
- CDC. COVIDView-A Weekly Surveillance Summery of U.S COVID-19 Activity, 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/pdf/covidview-04-10-2020.pdf (accessed on 20 May 2020).
- Williams, S.N.; Armitage, C.J.; Tampe, T.; Dienes, K. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: A UK-based focus group study. BMJ Open 2020, 10, e039334. [Google Scholar] [CrossRef] [PubMed]
- Reuben, R.C.; Danladi, M.M.A.; Saleh, D.A.; Ejembi, P.E. Knowledge, Attitudes and Practices Towards COVID-19: An Epidemiological Survey in North-Central Nigeria. J. Community Health 2021, 46, 457–470. [Google Scholar] [CrossRef] [PubMed]
- Gordon, H.S.; Pugach, O.; Berbaum, M.L.; Ford, M.E. Examining patients’ trust in physicians and the VA healthcare system in a prospective cohort followed for six-months after an exacerbation of heart failure. Patient Educ. Couns. 2014, 97, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Siebzehner, M.I.; Bialik, H.; Matalon, A. Doctor-Patient relationships in changing society. Harefuah 2008, 147, 1010–1015. [Google Scholar]
- Rosenstock, I.M. Historical Origins of the Health Belief Model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Fishbein, M.; Ajzen, I. Understanding Attitudes and Predicting Social Behavior; Prentice-Hall: New York, NY, USA, 1980. [Google Scholar]
- Ajzen, I.; Madden, J.T. Prediction of goal-directed behavior: Attitudes, intentions, and perceived behavioral control. J. Exp. Soc. Psychol. 1986, 22, 1986. [Google Scholar] [CrossRef]
- Kan, T.; Zhang, J. Factors influencing seasonal influenza vaccination behaviour among elderly people: A systematic review. Public Health 2018, 156, 67–78. [Google Scholar] [CrossRef]
- Olsen, A.L.; Hjorth, F. Willingness to Distance in the COVID-19 Pandemic. 2020. Work in Progress. Available online: https://osf.io/xpwg2/ (accessed on 20 May 2020).
- Zandifar, A.; Badrfam, R. Iranian mental health during the COVID-19 epidemic. Asian J. Psychiatry 2020, 51, 101990. [Google Scholar] [CrossRef]
- Kunzmann, U.; Schilling, O.; Wrosch, C.; Siebert, J.S.; Katzorreck, M.; Wahl, H.-W.; Gerstorf, D. Negative emotions and chronic physical illness: A lifespan developmental perspective. Heal. Psychol. 2019, 38, 949–959. [Google Scholar] [CrossRef]
- Lerner, J.S.; Li, Y.; Valdesolo, P.; Kassam, K.S. Emotion and Decision Making. Annu. Rev. Psychol. 2015, 66, 799–823. [Google Scholar] [CrossRef] [Green Version]
- Lerner, J.S.; Keltner, D. Fear, anger, and risk. J. Pers. Soc. Psychol. 2001, 81, 146–159. [Google Scholar] [CrossRef] [PubMed]
- Zeelenberg, M.; Nelissen, R.M.A.; Breugelmans, S.L.; Pieters, R. On emotion specificity in decision making: Why feeling is for doing. Judgm. Decis. Mak. 2008, 3, 18–27. [Google Scholar]
- Haque, M.U.; Azhar, S.M.; Ur-Rehman, M. Incorporating emotions as antecedents and mediators in Theory of reasoned action (TRA) model. Bus. Rev. 2014, 9, 2014. [Google Scholar]
- Harland, P.; Staats, H.; Wilke, H.A.M. Explaining pro environmental intention and behavior by personal norms and the theory of planned behavior. J. Appl. Soc. Psychol. 1999, 29, 2505–2528. [Google Scholar] [CrossRef]
- Elster, J. Rationality, emotions, and social norms. Synthese 1994, 98, 21–49. [Google Scholar] [CrossRef]
- Hobfoll, S.E. Social and psychological resources and adaptation. Rev. Gen. Psychol. 2002, 6, 307–324. [Google Scholar] [CrossRef]
- Shirey, M. Social support in the workplace: Nurse leader implications. Nurs. Econ. 2005, 22, 313. [Google Scholar]
- Liu, L.; Gou, Z.; Zuo, J. Social support mediates loneliness and depression in elderly people. J. Health Psychol. 2016, 21, 750–758. [Google Scholar] [CrossRef]
- Epidemiological Report: Highlights on the Topic: The New Corona Virus (COVID-19). Available online: https://www.health.gov.il/PublicationsFiles/covid-19_epi3.pdf (accessed on 20 May 2020).
- Israel Ministry od Health Guidelines to Confront the New Corona Virus Morbidity. Available online: https://govextra.gov.il/ministry-of-health/corona/corona-virus/guidelines/ (accessed on 20 May 2020).
- Egede, L.E.; Ellis, C. Development and Testing of the Multidimensional Trust in Health Care Systems Scale. J. Gen. Intern. Med. 2008, 23, 808–815. [Google Scholar] [CrossRef] [Green Version]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social Learning Theory and the Health Belief Model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Nelms, E.; Wang, L.; Pennell, M.; Wewers, M.E.; Seiber, E.; Adolph, M.D.; Paskett, E.D.; Ferketich, A.K. Trust in physicians among rural Medicaid-enrolled smokers. J. Rural. Health 2013, 30, 214–220. [Google Scholar] [CrossRef] [Green Version]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Zimet, G.; Powell, S.S.; Farley, G.K.; Werkman, S.; Berkoff, K.A. Psychometric Characteristics of the Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1990, 55, 610–617. [Google Scholar] [CrossRef]
- Caterinicchio, P.R. Testing plausible path models of interpersonal trust in patient-physician treatment relationships. Soc. Sci. Med. Part A 1979, 13, 81–99. [Google Scholar] [CrossRef]
- Satran, C.; Ali-Saleh, O.; Mashiach-Eizenberg, M.; Bord, S. Stress and perceived discrimination among the Arab population in Israel: The mediation role of the perceived COVID-19 threat and trust in the healthcare system. Ethn. Health 2021, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Monte Carlo Method for Assessing Mediation: An Interactive Tool for Creating Confidence Intervals for Indirect Effects. 2008. Available online: http://quantpsy.org/ (accessed on 20 May 2020).
- Abdelhafiz, A.S.; Mohammed, Z.; Ibrahim, M.E.; Ziady, H.H.; Alorabi, M.; Ayyad, M.; Sultan, E. Knowledge, Perceptions, and Attitude of Egyptians Towards the Novel Coronavirus Disease (COVID-19). J. Community Health 2020, 45, 881–890. [Google Scholar] [CrossRef]
- Uchmanowicz, B.; Chudiak, A.; Uchmanowicz, I.; Rosińczuk, J.; Froelicher, E.S. Factors influencing adherence to treatment in older adults with hypertension. Clin. Interv. Aging 2018, ume 13, 2425–2441. [Google Scholar] [CrossRef] [Green Version]
- Crossnohere, N.L.; Davey-Rothwell, M.; Latkin, C.; Tseng, T.-Y.; Czaplicki, L.; Knowlton, A. The Interaction of Smoking Cessation Norms and Nicotine Dependence on Quit Attempts: Gender-Stratified Results for Low-Income Smokers in Baltimore, MD. Subst. Use Misuse 2020, 55, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Phipps, D.J.; Hagger, M.S.; Hamilton, K. Predicting limiting ‘free sugar’ consumption using an integrated model of health behavior. Appetite 2020, 150, 104668. [Google Scholar] [CrossRef]
- Hagger, M.S.; Hamilton, K.; Hardcastle, S.J.; Hu, M.; Kwok, S.; Lin, J.; Nawawi, H.; Pang, J.; Santos, R.D.; Soran, H.; et al. Predicting intention to participate in self-management behaviors in patients with Familial Hypercholesterolemia: A cross-national study. Soc. Sci. Med. 2019, 242, 112591. [Google Scholar] [CrossRef]
- Jannuzzi, F.F.; Cornélio, M.E.; São-João, T.M.; Gallani, M.-C.; Godin, G.; Rodrigues, R.C.M. Psychosocial determinants of adherence to oral antidiabetic medication among people with type 2 diabetes. J. Clin. Nurs. 2019, 29, 909–921. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, H.; Brissette, I.; Leventhal, E.; Cameron, L.D. (Eds.) The Self-Regulation of Health and Illness Behavior; Routledge: London, UK, 2003; pp. 42–65. [Google Scholar]
- Brown, M.T.; Bussell, J.; Dutta, S.; Davis, K.; Strong, S.; Mathew, S. Medication Adherence: Truth and Consequences. Am. J. Med Sci. 2016, 351, 387–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birkhäuer, J.; Gaab, J.; Kossowsky, J.; Hasler, S.; Krummenacher, P.; Werner, C.P.; Gerger, H. Trust in the health care professional and health outcome: A meta-analysis. PLoS ONE 2017, 12, e0170988. [Google Scholar] [CrossRef] [Green Version]
- Baumeister, R.F.; Leary, M.R. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychol. Bull. 1995, 117, 497–529. (In English) [Google Scholar] [CrossRef]
- Witte, K.; Allen, M. A Meta-Analysis of Fear Appeals: Implications for Effective Public Health Campaigns. Health Educ. Behav. 2000, 27, 591–615. [Google Scholar] [CrossRef]
- Carey, R.N.; Sarma, K.M. Threat appeals in health communication: Messages that elicit fear and enhance perceived efficacy positively impact on young male drivers. BMC Public Health 2016, 16, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Harper, C.A.; Satchell, L.P.; Fido, D.; Latzman, R.D. Functional Fear Predicts Public Health Compliance in the COVID-19 Pandemic. Int. J. Ment. Health Addict. 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Witte, K. Putting the fear back into fear appeals: The extended parallel process model. Commun. Monogr. 1992, 59, 329–349. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. (In English) [Google Scholar] [CrossRef]
- Gariépy, G.; Honkaniemi, H.; Quesnel-Vallée, A. Social support and protection from depression: Systematic review of current findings in Western countries. Br. J. Psychiatry 2016, 209, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, P. What is recall bias? BMJ 2012, 344, e3519. [Google Scholar] [CrossRef]
| Mean (SD), Range 1–5 | % of Respondents Who Responded 4 or More | |
|---|---|---|
| Adherence | 4.30(0.81) | ___ |
| Family members visited me at home | 1.76(1.22) | 0.15 |
| Neighbors or friends visited me at home | 1.34(0.88) | 0.059 |
| I avoided meeting family members | 4.09(1.20) | 0.742 |
| I avoided meeting neighbors or friends | 4.22(1.15) | 0.789 |
| Mean (SD), Range 1–7 | % of Respondents Who Responded 5 or More | |
| Negative Emotion | 2.86(1.41) | ___ |
| Frustrated | 3.20(1.87) | 0.283 |
| In a bad mood | 3.05(1.73) | 0.252 |
| Stressed | 3.02(1.78) | 0.248 |
| Angry | 2.81(1.74) | 0.211 |
| Anxious | 2.74(1.76) | 0.205 |
| Nervous | 2.73(1.70) | 0.186 |
| Frightened | 2.46(1.66) | 0.156 |
| M (SD) | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Adherance (1–5) | 4.30 (0.81) | −0.01 | 0.12 *** | 0.04 | 0.02 | 0.22 *** | 0.26 *** |
| 2. Negative emotions (1–7) | 2.86 (1.41) | 0.34 *** | −0.03 | −0.16 *** | −0.08 ** | −0.13 *** | |
| 3. Perception of threat (1–5) | 3.61 (0.99) | 0.02 | 0.02 | 0.21 *** | 0.13 *** | ||
| 4. Trust in the healthcare system (1–7) | 4.82 (0.81) | 0.08 ** | 0.20 *** | 0.22 *** | |||
| 5. Social support (1–7) | 5.96 (0.96) | 0.15 *** | 0.21 *** | ||||
| 6. Attitudes (1–7) | 5.95 (1.12) | 0.58 *** | |||||
| 7. Subjective norms (1–7) | 6.06 (0.89) |
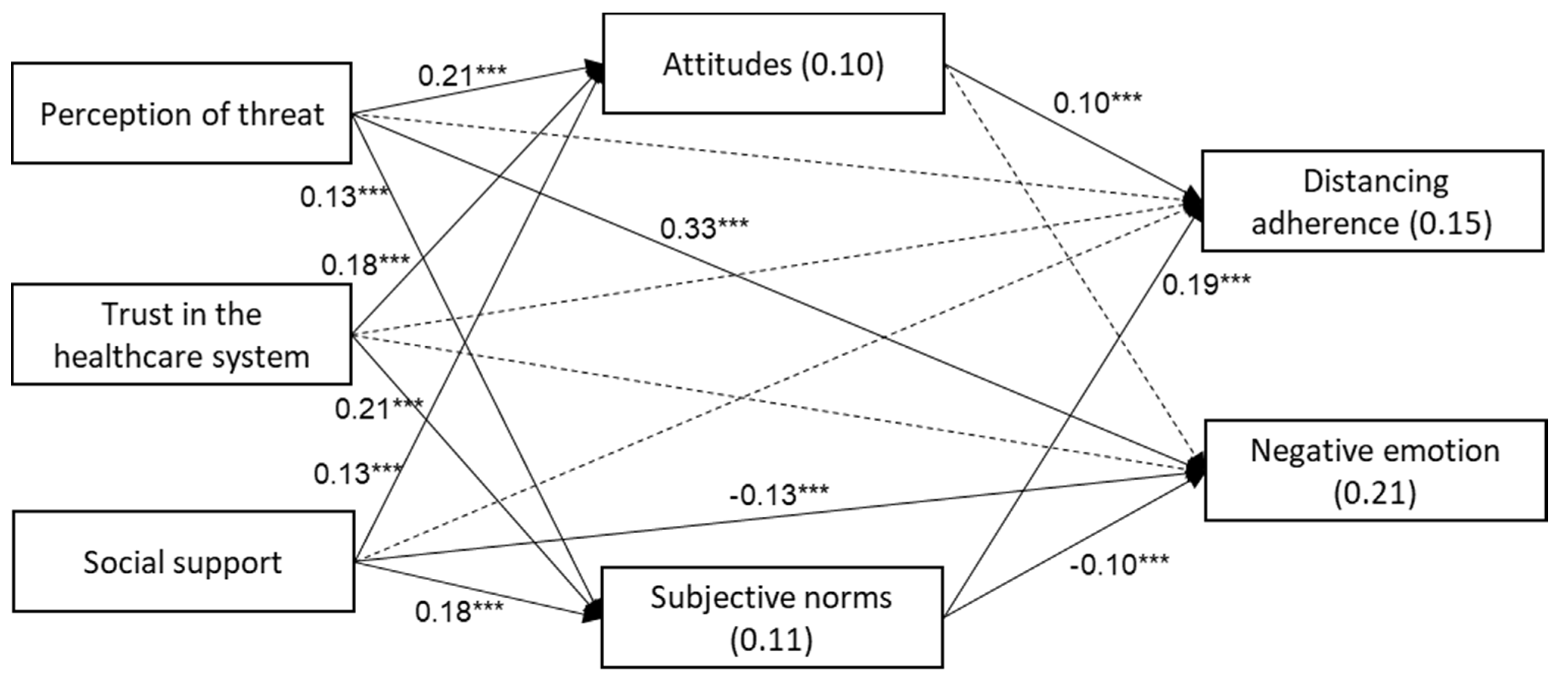
| DV (R2) | IV | β | SE | p |
|---|---|---|---|---|
| Attitudes towards distancing instructions (0.10) | Perception of threat | 0.21 | 0.02 | <0.001 |
| Trust in the healthcare system | 0.18 | 0.02 | <0.001 | |
| Social support | 0.13 | 0.02 | <0.001 | |
| Subjective norms regarding distancing instructions (0.11) | Perception of threat | 0.13 | 0.02 | <0.001 |
| Trust in the healthcare system | 0.21 | 0.02 | <0.001 | |
| Social support | 0.18 | 0.02 | <0.001 | |
| Distancing adherence (0.15) | Perception of threat | 0.05 | 0.02 | 0.018 |
| Trust in the healthcare system | −0.03 | 0.02 | 0.188 | |
| Social support | −0.05 | 0.02 | 0.038 | |
| Attitudes | 0.10 | 0.03 | <0.001 | |
| Subjective norms | 0.19 | 0.03 | <0.001 | |
| Negative emotions (0.21) | Perception of threat | 0.33 | 0.02 | <0.001 |
| Trust in the healthcare system | 0.03 | 0.02 | 0.211 | |
| Social support | −0.13 | 0.02 | <0.001 | |
| Attitudes | −0.06 | 0.03 | 0.032 | |
| Subjective norms | −0.10 | 0.03 | <0.001 |
| DV (R2) | IV | Standardized Indirect Effect | SE | 95% CI |
|---|---|---|---|---|
| Distancing adherence (0.15) | Perception of threat | 0.046 | 0.008 | 0.034, 0.063 |
| Trust in the healthcare system | 0.059 | 0.009 | 0.042, 0.077 | |
| Social support | 0.047 | 0.007 | 0.031, 0.060 | |
| Negative emotions (0.21) | Perception of threat | −0.025 | 0.005 | −0.036, −0.015 |
| Trust in the healthcare system | −0.032 | 0.006 | −0.044, −0.021 | |
| Social support | −0.026 | 0.005 | −0.035, −0.016 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bord, S.; Schor, A.; Satran, C.; Ali Saleh, O.; Inchi, L.; Halperin, D. Distancing Adherence and Negative Emotions among the Israeli Elderly Population during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 8770. https://doi.org/10.3390/ijerph18168770
Bord S, Schor A, Satran C, Ali Saleh O, Inchi L, Halperin D. Distancing Adherence and Negative Emotions among the Israeli Elderly Population during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(16):8770. https://doi.org/10.3390/ijerph18168770
Chicago/Turabian StyleBord, Shiran, Ayelet Schor, Carmit Satran, Ola Ali Saleh, Liron Inchi, and Dafna Halperin. 2021. "Distancing Adherence and Negative Emotions among the Israeli Elderly Population during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 16: 8770. https://doi.org/10.3390/ijerph18168770
APA StyleBord, S., Schor, A., Satran, C., Ali Saleh, O., Inchi, L., & Halperin, D. (2021). Distancing Adherence and Negative Emotions among the Israeli Elderly Population during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(16), 8770. https://doi.org/10.3390/ijerph18168770






