Short-Term Effect of Temperature Change on Non-Accidental Mortality in Shenzhen, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data
2.2. Statistical Analysis
2.3. Sensitivity Analysis
3. Results
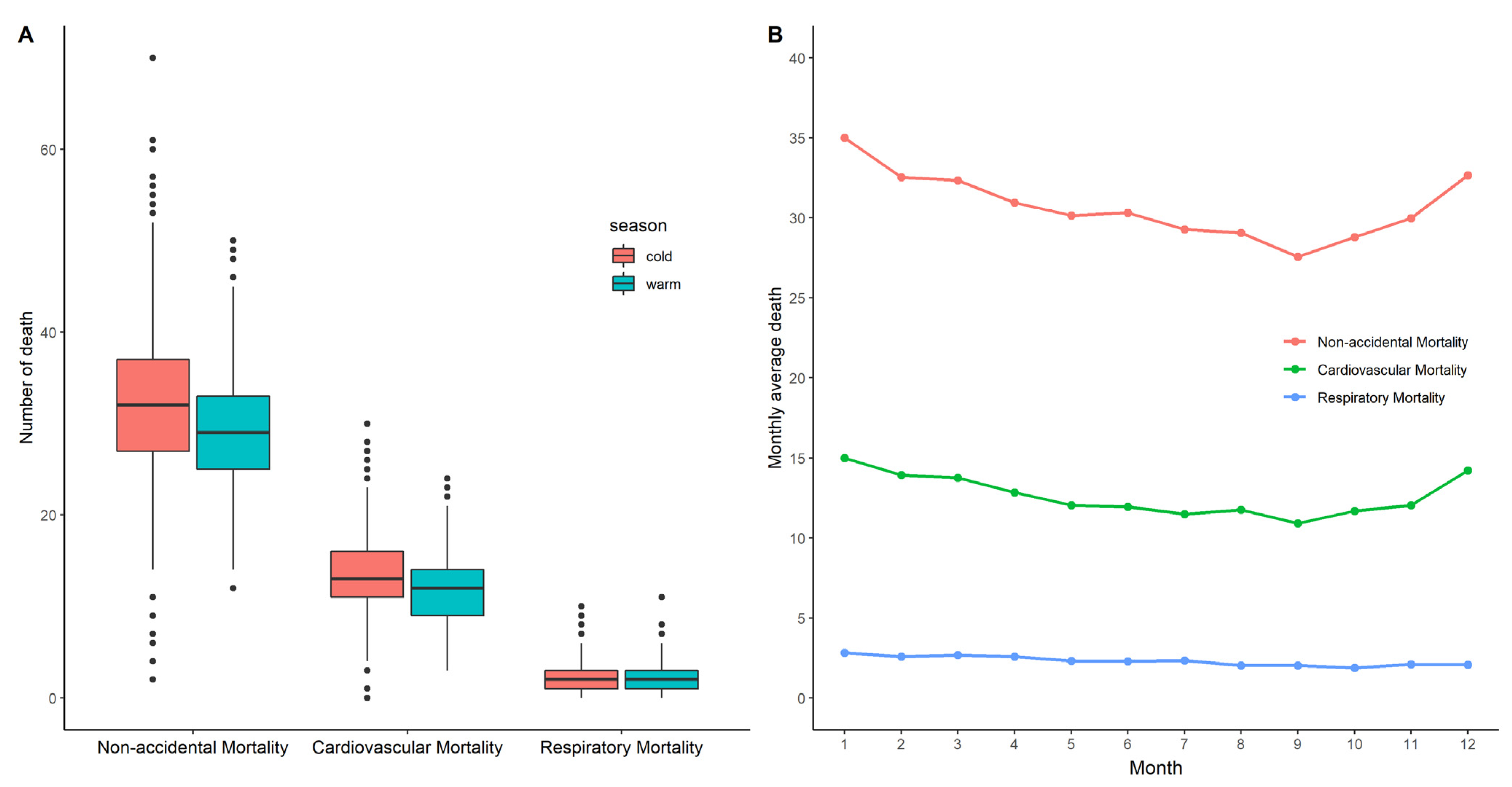
3.1. Descriptive Analysis
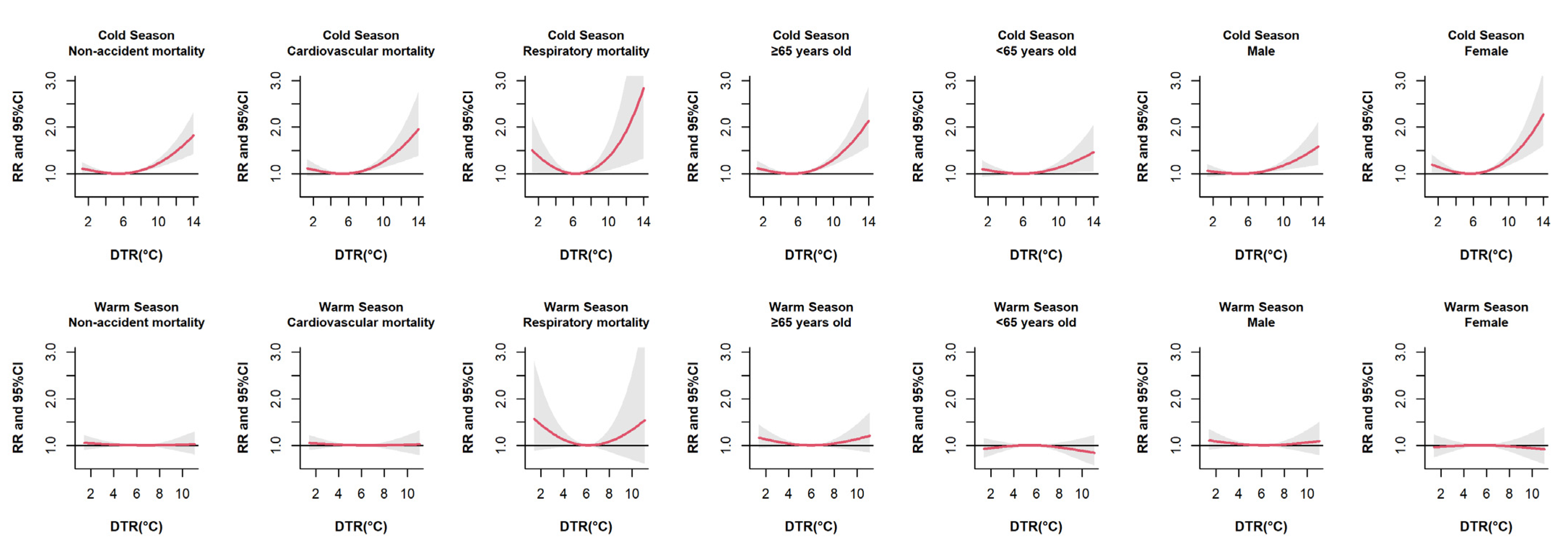
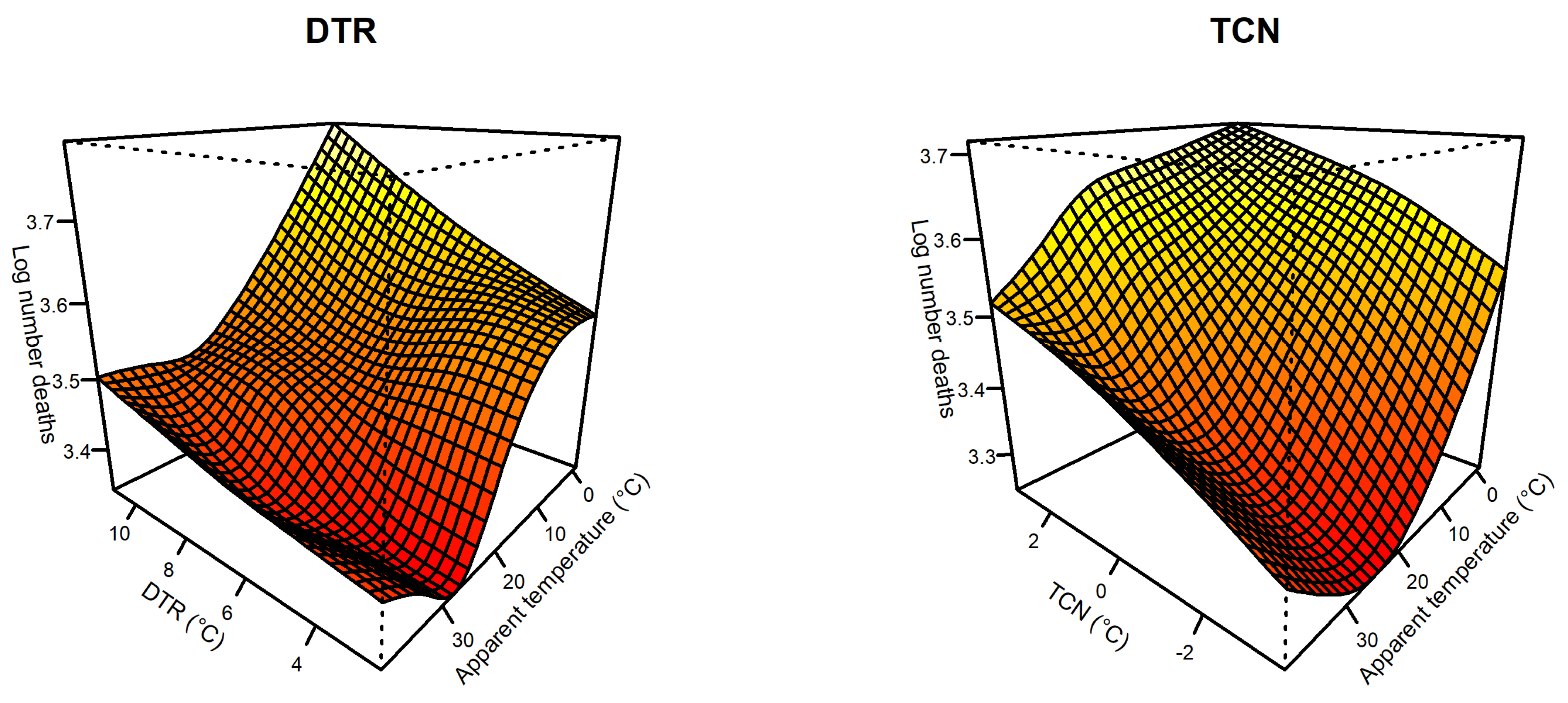
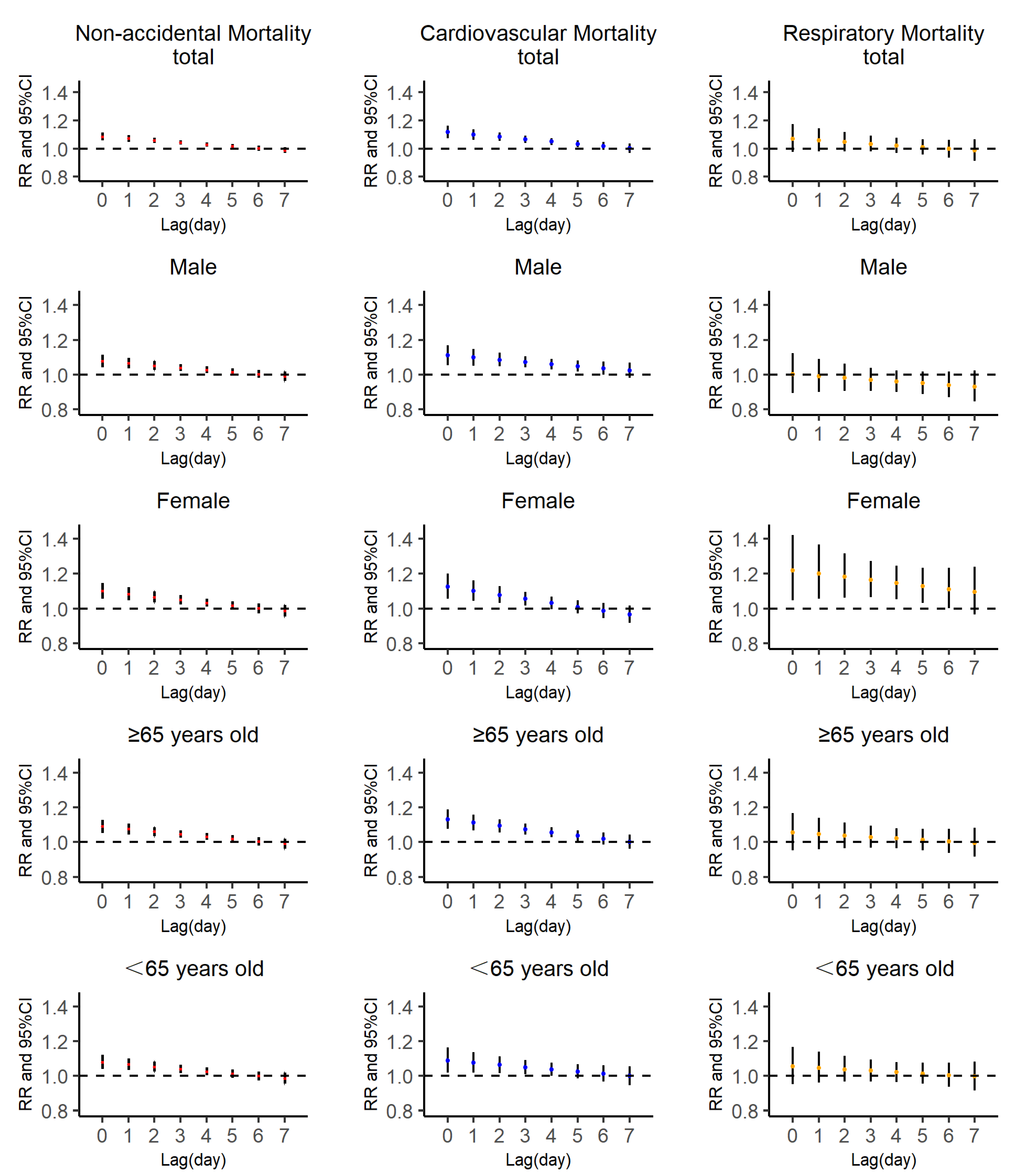
3.2. Effects of DTR on Mortality
3.3. Effects of TCN on Mortality
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- IPCC. Climate Change 2014 Synthesis Report Summary for Policymakers. 2013. Available online: https://www.ipcc.ch/report/ar5/syr/ (accessed on 1 November 2014).
- Yang, Z.; Wang, Q.; Liu, P. Extreme temperature and mortality: Evidence from China. Int. J. Biometeorol. 2018, 63, 29–50. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Xu, Z.; Bambrick, H.; Su, H.; Tong, S.; Hu, W. Impacts of heat, cold, and temperature variability on mortality in Australia, 2000–2009. Sci. Total Environ. 2018, 651, 2558–2565. [Google Scholar] [CrossRef] [PubMed]
- Zha, Q.; Chai, G.; Zhang, Z.-G.; Sha, Y.; Su, Y. Effects of diurnal temperature range on cardiovascular disease hospital admissions in farmers in China’s Western suburbs. Environ. Sci. Pollut. Res. 2021, 1–13. [Google Scholar] [CrossRef]
- Yang, J.; Zhou, M.; Li, M.; Yin, P.; Wang, B.; Pilot, E.; Liu, Y.; van der Hoek, W.; van Asten, L.; Krafft, T.; et al. Diurnal temperature range in relation to death from stroke in China. Environ. Res. 2018, 164, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Zhu, W.; Wang, M.; Shi, Q.; Luo, Y.; Miao, Q.; Nie, Y.; Kang, F.; Mi, X.; Bai, Y. The effect of diurnal temperature range on blood pressure among 46,609 people in Northwestern China. Sci. Total Environ. 2020, 730, 138987. [Google Scholar] [CrossRef]
- Gostimirovic, M.; Novakovic, R.; Rajkovic, J.; Djokic, V.; Terzic, D.; Putnik, S.; Gojkovic-Bukarica, L. The influence of climate change on human cardiovascular function. Arch. Environ. Occup. Health 2020, 75, 406–414. [Google Scholar] [CrossRef]
- Zhang, B.; Li, G.; Ma, Y.; Pan, X. Projection of temperature-related mortality due to cardiovascular disease in beijing under different climate change, population, and adaptation scenarios. Environ. Res. 2018, 162, 152–159. [Google Scholar] [CrossRef]
- Yang, J.; Zhou, M.; Li, M.; Liu, X.; Yin, P.; Sun, Q.; Wang, J.; Wu, H.; Wang, B.; Liu, Q. Vulnerability to the impact of temperature variability on mortality in 31 major Chinese cities. Environ. Pollut. 2018, 239, 631–637. [Google Scholar] [CrossRef]
- Ma, C.; Yang, J.; Nakayama, S.F.; Honda, Y. The association between temperature variability and cause-specific mortality: Evidence from 47 Japanese prefectures during 1972–2015. Environ. Int. 2019, 127, 125–133. [Google Scholar] [CrossRef]
- Zhang, Y.; Peng, M.; Wang, L.; Yu, C. Association of diurnal temperature range with daily mortality in England and Wales: A nationwide time-series study. Sci. Total Environ. 2018, 619–620, 291–300. [Google Scholar] [CrossRef]
- Zhou, X.; Zhao, A.; Meng, X.; Chen, R.; Kuang, X.; Duan, X.; Kan, H. Acute effects of diurnal temperature range on mortality in 8 Chinese cities. Sci. Total Environ. 2014, 493, 92–97. [Google Scholar] [CrossRef]
- Zhan, Z.; Zhao, Y.; Pang, S.; Zhong, X.; Wu, C.; Ding, Z. Temperature change between neighboring days and mortality in United States: A nationwide study. Sci. Total Environ. 2017, 584–585, 1152–1161. [Google Scholar] [CrossRef] [PubMed]
- Steadman, R.G. Norms of apparent temperature in Australia. Aust. Meterol. Mag. 1993, 43, 1–16. [Google Scholar]
- Yang, J.; Liu, H.-Z.; Ou, C.-Q.; Lin, G.-Z.; Zhou, Q.; Shen, G.-C.; Chen, P.-Y.; Guo, Y. Global climate change: Impact of diurnal temperature range on mortality in Guangzhou, China. Environ. Pollut. 2013, 175, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, B. Models for the Relationship Between Ambient Temperature and Daily Mortality. Epidemiology 2006, 17, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A. Modeling exposure-lag-response associations with distributed lag non-linear models. Stat. Med. 2014, 33, 881–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gasparrini, A.; Leone, M. Attributable risk from distributed lag models. BMC Med. Res. Methodol. 2014, 14, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [Green Version]
- Gasparrini, A. Distributed Lag Linear and Non-Linear Models inR: The Packagedlnm. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Huang, K.; Yang, X.-J.; Hu, C.-Y.; Ding, K.; Jiang, W.; Hua, X.-G.; Liu, J.; Cao, J.-Y.; Sun, C.-Y.; Zhang, T.; et al. Short-term effect of ambient temperature change on the risk of tuberculosis admissions: Assessments of two exposure metrics. Environ. Res. 2020, 189, 109900. [Google Scholar] [CrossRef]
- Deng, J.; Hu, X.; Xiao, C.; Xu, S.; Gao, X.; Ma, Y.; Yang, J.; Wu, M.; Liu, X.; Ni, J.; et al. Ambient temperature and non-accidental mortality: A time series study. Environ. Sci. Pollut. Res. 2019, 27, 4190–4196. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.-Z.; Zheng, S.; He, S.-L.; Li, B.; Teng, H.-J.; Wang, S.-G.; Yin, L.; Shang, K.-Z.; Li, T.-S. The association between diurnal temperature range and emergency room admissions for cardiovascular, respiratory, digestive and genitourinary disease among the elderly: A time series study. Sci. Total Environ. 2013, 456–457, 370–375. [Google Scholar] [CrossRef]
- Zhao, Y.; Huang, Z.; Wang, S.; Hu, J.; Xiao, J.; Li, X.; Liu, T.; Zeng, W.; Guo, L.; Du, Q.; et al. Morbidity burden of respiratory diseases attributable to ambient temperature: A case study in a subtropical city in China. Environ. Health 2019, 18, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Cheng, J.; Zhu, R.; Xu, Z.; Xu, X.; Wang, X.; Li, K.; Su, H. Temperature variation between neighboring days and mortality: A distributed lag non-linear analysis. Int. J. Public Health 2014, 59, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Zhang, Y.; Xu, Y.; Xu, X.; Liu, T.; Luo, Y.; Xiao, J.; Wu, W.; Ma, W. Temperature Changes between Neighboring Days and Mortality in Summer: A Distributed Lag Non-Linear Time Series Analysis. PLoS ONE 2013, 8, e66403. [Google Scholar] [CrossRef]
- Wei, Q.; Zhong, L.; Gao, J.; Yi, W.; Pan, R.; Gao, J.; Duan, J.; Xu, Z.; He, Y.; Liu, X.; et al. Diurnal temperature range and childhood asthma in Hefei, China: Does temperature modify the association? Sci. Total Environ. 2020, 724, 138206. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobías, A.; Tong, S.; Rocklöv, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Cao, J.; Cheng, Y.; Zhao, N.; Song, W.; Jiang, C.; Chen, R.; Kan, H. Diurnal Temperature Range is a Risk Factor for Coronary Heart Disease Death. J. Epidemiol. 2009, 19, 328–332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chit-Ming Wong, S.M.; Hedley, A.J.; Lam, T.-H. Effect of Air Pollution on Daily Mortality in Hong Kong. Environ. Health Perspect. 2001, 109, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Li, T.T.; Zhang, Y.H.; Xu, Y.J.; Lao, X.Q.; Rutherford, S.; Chu, C.; Luo, Y.; Zhu, Q.; Xu, X.J.; et al. The short-term effect of ambient ozone on mortality is modified by temperature in Guangzhou, China. Atmos. Environ. 2012, 76, 59–67. [Google Scholar] [CrossRef]
- Zeka, A.; Zanobetti, A.; Schwartz, J. Individual-Level Modifiers of the Effects of Particulate Matter on Daily Mortality. Am. J. Epidemiol. 2006, 163, 849–859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schenker, N.; Gentleman, J.F. On Judging the Significance of Differences by Examining the Overlap Between Confidence Intervals. Am. Stat. 2001, 55, 182–186. [Google Scholar] [CrossRef]
- Kan, H.; London, S.; Chen, H.; Song, G.; Chen, G.; Jiang, L.; Zhao, N.; Zhang, Y.; Chen, B. Diurnal temperature range and daily mortality in Shanghai, China. Environ. Res. 2007, 103, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Ding, Z.; Guo, P.; Xie, F.; Chu, H.; Li, K.; Pu, J.; Pang, S.; Dong, H.; Liu, Y.; Pi, F.; et al. Impact of diurnal temperature range on mortality in a high plateau area in southwest China: A time series analysis. Sci. Total Environ. 2015, 526, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Ding, Z.; Li, L.; Xin, L.; Pi, F.; Dong, W.; Wen, Y.; Au, W.W.; Zhang, Q. High diurnal temperature range and mortality: Effect modification by individual characteristics and mortality causes in a case-only analysis. Sci. Total Environ. 2016, 544, 627–634. [Google Scholar] [CrossRef]
- Luo, Y.; Zhang, Y.; Liu, T.; Rutherford, S.; Xu, Y.; Xu, X.; Wu, W.; Xiao, J.; Zeng, W.; Chu, C.; et al. Lagged Effect of Diurnal Temperature Range on Mortality in a Subtropical Megacity of China. PLoS ONE 2013, 8, e55280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, B.; Chai, G.; Sha, Y.; Zha, Q.; Su, Y.; Gao, Y. Impact of ambient temperature on cardiovascular disease hospital admissions in farmers in China’s Western suburbs. Sci. Total Environ. 2021, 761, 143254. [Google Scholar] [CrossRef] [PubMed]
- Bull, G. The weather and deaths from pneumonia. Lancet 1980, 315, 1405–1408. [Google Scholar] [CrossRef]
- Tang, M.; He, Y.; Zhang, X.; Li, H.; Huang, C.; Wang, C.; Gao, Y.; Li, Y.; Kan, H.; Hu, J.; et al. The acute effects of temperature variability on heart rate variability: A repeated-measure study. Environ. Res. 2020, 194, 110655. [Google Scholar] [CrossRef] [PubMed]
- Togias, A.G.; Naclerio, R.M.; Proud, D.; Fish, J.E.; Adkinson, N.F.; Kagey-Sobotka, A.; Norman, P.S.; Lichtenstein, L.M. Nasal challenge with cold, dry air results in release of inflammatory mediators. Possible mast cell involvement. J. Clin. Investig. 1985, 76, 1375–1381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zanobetti, A.; O’Neill, M.S.; Gronlund, C.J.; Schwartz, J.D. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc. Natl. Acad. Sci. USA 2012, 109, 6608–6613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, Y.; Barnett, A.; Yu, W.; Pan, X.; Ye, X.; Huang, C.; Tong, S. A Large Change in Temperature between Neighbouring Days Increases the Risk of Mortality. PLoS ONE 2011, 6, e16511. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.; Zhao, Y.; Zhou, J.; Jiang, Y.; Yang, S.; Yu, Z. The relationship between diurnal temperature range and COPD hospital admissions in Changchun, China. Environ. Sci. Pollut. Res. 2018, 25, 17942–17949. [Google Scholar] [CrossRef]
- Kenney, W.L.; Hodgson, I.L. Heat tolerance, thermoregulation and ageing. Sports Med. 1987, 4, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-B.; Kim, J.-H.; Murota, H. Perspiration Functions in Different Ethnic, Age, and Sex Populations: Modification of Sudomotor Function. Perspiration Res. 2016, 51, 109–119. [Google Scholar] [CrossRef]
- Lee, W.; Chung, Y.; Choi, H.M.; Kim, D.; Honda, Y.; Guo, Y.L.; Kim, H. Interactive Effect of Diurnal Temperature Range and Temperature on Mortality, Northeast Asia. Epidemiology 2019, 30, S99–S106. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Kim, Y.; Honda, Y.; Kim, H. Association between diurnal temperature range and mortality modified by temperature in Japan, 1972–2015: Investigation of spatial and temporal patterns for 12 cause-specific deaths. Environ. Int. 2018, 119, 379–387. [Google Scholar] [CrossRef]
- Madaniyazi, L.; Zhou, Y.; Li, S.; Williams, G.; Jaakkola, J.; Liang, X.; Liu, Y.; Wu, S.; Guo, Y. Outdoor Temperature, Heart Rate and Blood Pressure in Chinese Adults: Effect Modification by Individual Characteristics. Sci. Rep. 2016, 6, 21003. [Google Scholar] [CrossRef] [Green Version]
- Zhou, X.; Lin, H.; Zhang, S.; Ren, J.; Wang, Z.; Zhang, Y.; Wang, M.; Zhang, Q. Effects of climatic factors on plasma lipid levels: A 5-year longitudinal study in a large Chinese population. J. Clin. Lipidol. 2016, 10, 1119–1128. [Google Scholar] [CrossRef]
- Li, S.; Zhou, Y.; Williams, G.; Jaakkola, J.; Ou, C.; Chen, S.; Yao, T.; Qin, T.; Wu, S.; Guo, Y. Seasonality and temperature effects on fasting plasma glucose: A population-based longitudinal study in China. Diabetes Metab. 2016, 42, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Allen, S.; Cardona, O.; Cutter, S.; Dube, O.P.; Ebi, K.; Handmer, J.; Lavell, A.; Mastrandrea, M.; McBean, G.; Mechler, R.; et al. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2012; p. 19. [Google Scholar]
| Variables | Mean (Standard Deviation) | Minimum Value | 25th Percentile | 50th Percentile | 75th Percentile | 99th Percentile | Maximum Value |
|---|---|---|---|---|---|---|---|
| Weather | |||||||
| DTR (°C) | 5.99 (1.98) | 1.30 | 4.60 | 6.00 | 7.30 | 10.80 | 14.00 |
| TCN (°C) | 0.00 (1.64) | −10.10 | −0.70 | 0.20 | 1.00 | 3.28 | 6.20 |
| Apparent temperature (°C) | 25.65 (8.15) | −1.04 | 19.19 | 27.25 | 32.97 | 36.55 | 39.39 |
| Mean temperature (°C) | 23.45 (5.49) | 3.50 | 19.20 | 24.80 | 28.20 | 30.90 | 33.00 |
| Relative humidity (%) | 75.20 (13.16) | 19.00 | 69.00 | 77.00 | 84.00 | 97.00 | 100.00 |
| Wind speed (m/s) | 1.97 (0.77) | 0.30 | 1.40 | 1.80 | 2.40 | 4.40 | 5.90 |
| Daily air pollutants | |||||||
| PM10 (μg/m3) | 50.80 (27.77) | 8.69 | 29.82 | 43.81 | 65.45 | 138.90 | 181.76 |
| NO2 (μg/m3) | 39.69 (16.51) | 12.00 | 28.32 | 36.10 | 46.97 | 96.55 | 133.71 |
| CO (mg/m3) | 0.95 (0.27) | 0.49 | 0.75 | 0.90 | 1.12 | 1.63 | 1.93 |
| SO2 (μg/m3) | 9.50 (4.11) | 3.52 | 7.00 | 8.55 | 10.80 | 24.94 | 54.81 |
| PM2.5 (μg/m3) | 32.03 (19.65) | 5.64 | 16.76 | 27.72 | 42.28 | 101.57 | 137.07 |
| No. of non-accidental deaths * | |||||||
| Total (A00–A99) | 31 (7) | 2 | 26 | 30 | 35 | 49 | 70 |
| Age | |||||||
| Young people (<65 years) | 14 (4) | 1 | 11 | 14 | 17 | 25 | 30 |
| Elderly (≥65 years) | 17 (5) | 1 | 14 | 16 | 20 | 30 | 40 |
| Sex | |||||||
| Male | 19 (5) | 1 | 16 | 19 | 22 | 32 | 45 |
| Female | 12 (4) | 1 | 9 | 11 | 14 | 22 | 28 |
| Cardiovascular disease (I00–I99) | 13 (4) | 0 | 10 | 12 | 15 | 24 | 30 |
| Age | |||||||
| Young people (<65 years) | 5 (2) | 0 | 3 | 4 | 6 | 11 | 15 |
| Elderly (≥65 years) | 8 (3) | 0 | 6 | 8 | 10 | 17 | 20 |
| Sex | |||||||
| Male | 8 (3) | 0 | 6 | 8 | 10 | 16 | 20 |
| Female | 5 (2) | 0 | 3 | 4 | 6 | 12 | 15 |
| Respiratory disease (J00–J99) | 2 (2) | 0 | 1 | 2 | 3 | 7 | 11 |
| Age | |||||||
| Young people (<65 years) | 0 (1) | 0 | 0 | 0 | 1 | 3 | 5 |
| Elderly (≥65 years) | 2 (1) | 0 | 1 | 2 | 3 | 6 | 10 |
| Sex | |||||||
| Male | 2 (1) | 0 | 1 | 1 | 2 | 5 | 9 |
| Female | 1 (1) | 0 | 0 | 1 | 1 | 3 | 6 |
| Group | Lag 0 | Lag 3 | Lag 0–5 | Lag 0–7 |
|---|---|---|---|---|
| Non-accidental mortality | ||||
| Full year | 1.032 (1.008–1.056) | 1.010 (0.997–1.024) | 1.086 (0.999–1.180) | 1.055 (0.951–1.169) |
| Cold season | 1.063 (1.027–1.100) | 1.046 (1.029–1.064) | 1.333 (1.192–1.491) | 1.407 (1.233–1.606) |
| Warm season | 1.014 (0.991–1.038) | 1.003 (0.991–1.015) | 1.028 (0.952–1.110) | 1.007 (0.920–1.101) |
| Cardiovascular mortality | ||||
| Full year | 1.037 (1.002–1.074) | 1.018 (0.998–1.038) | 1.133 (0.999–1.286) | 1.124 (0.961–1.314) |
| Cold season | 1.066 (1.015–1.119) | 1.052 (1.027–1.077) | 1.371 (1.171–1.606) | 1.470 (1.220–1.771) |
| Warm season | 1.031 (0.984–1.080) | 1.006 (0.983–1.029) | 1.063 (0.914–1.236) | 1.016 (0.851–1.213) |
| Respiratory mortality | ||||
| Full year | 0.961 (0.891–1.036) | 0.986 (0.948–1.025) | 0.895 (0.696–1.151) | 0.924 (0.683–1.250) |
| Cold season | 1.077 (0.969–1.198) | 1.073 (1.017–1.131) | 1.529 (1.082–2.162) | 1.741 (1.157–2.620) |
| Warm season | 0.999 (0.901–1.108) | 1.016 (0.967–1.069) | 1.084 (0.778–1.511) | 1.165 (0.796–1.706) |
| Group | Lag 0 | Lag 3 | Lag 0–5 | Lag 0–7 |
|---|---|---|---|---|
| Full year | ||||
| Male | 1.027 (0.998–1.057) | 1.008 (0.992–1.025) | 1.070 (0.964–1.188) | 1.043 (0.917–1.187) |
| Female | 1.038 (1.002–1.076) | 1.013 (0.992–1.034) | 1.107 (0.973–1.260) | 1.072 (0.913–1.259) |
| ≥65 years old | 1.016 (0.986–1.047) * | 1.016 (0.999–1.034) | 1.102 (0.989–1.229) | 1.140 (0.997–1.303) |
| <65 years old | 1.044 (1.011–1.077) | 0.999 (0.982–1.015) | 1.036 (0.933–1.152) | 0.932 (0.821–1.058) |
| Cold season | ||||
| Male | 1.051 (1.009–1.095) | 1.036 (1.016–1.057) | 1.256 (1.100–1.434) * | 1.306 (1.118–1.527) * |
| Female | 1.082 (1.031–1.137) | 1.063 (1.037–1.089) | 1.467 (1.250–1.721) | 1.587 (1.314–1.917) |
| ≥65 years old | 1.030 (0.987–1.075) * | 1.052 (1.031–1.075) | 1.330 (1.158–1.527) | 1.548 (1.317–1.820) * |
| <65 years old | 1.107 (1.056–1.160) | 1.038 (1.014–1.062) | 1.333 (1.144–1.553) | 1.235 (1.028–1.482) |
| Warm season | ||||
| Male | 1.018 (0.983–1.054) | 1.006 (0.989–1.023) | 1.048 (0.935–1.174) | 1.031 (0.903–1.177) |
| Female | 1.016 (0.968–1.066) | 0.998 (0.975–1.022) | 1.007 (0.860–1.178) | 0.963 (0.802–1.157) |
| ≥65 years old | 1.039 (0.999–1.080) | 1.013 (0.994–1.033) | 1.108 (0.977–1.257) | 1.073 (0.926–1.243) |
| <65 years old | 0.992 (0.950–1.036) | 0.991 (0.970–1.012) | 0.948 (0.824–1.091) | 0.928 (0.788–1.093) |
| Group | Lag 0 | Lag 3 | Lag 0–5 | Lag 0–7 |
|---|---|---|---|---|
| Non-accidental mortality | ||||
| Full year | 1.086 (1.058–1.115) | 1.043 (1.027–1.060) | 1.342 (1.213–1.486) | 1.331 (1.180–1.500) |
| Cold season | 1.132 (1.091–1.175) | 1.071 (1.050–1.093) | 1.258 (1.177–1.345) | 1.611 (1.384–1.876) |
| Warm season | 1.063 (1.023–1.106) | 1.033 (1.009–1.056) | 1.248 (1.077–1.445) | 1.242 (1.043–1.480) |
| Cardiovascular mortality | ||||
| Full year | 1.117 (1.073–1.163) | 1.066 (1.041–1.092) | 1.538 (1.317–1.795) | 1.567 (1.304–1.881) |
| Cold season | 1.145 (1.087–1.207) | 1.087 (1.056–1.118) | 1.289 (1.172–1.417) | 1.814 (1.462–2.250) |
| Warm season | 1.112 (1.045–1.183) | 1.052 (1.015–1.091) | 1.434 (1.136–1.811) | 1.398 (1.058–1.847) |
| Respiratory mortality | ||||
| Full year | 1.071 (0.976–1.175) | 1.034 (0.978–1.093) | 1.265 (0.885–1.809) | 1.246 (0.817–1.899) |
| Cold season | 1.178 (1.048–1.324) | 1.089 (1.022–1.160) | 1.352 (1.095–1.669) | 1.779 (1.096–2.887) |
| Warm season | 1.081 (0.933–1.253) | 1.085 (0.996–1.183) | 1.627 (0.933–2.838) | 1.935 (0.999–3.746) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xiao, Y.; Meng, C.; Huang, S.; Duan, Y.; Liu, G.; Yu, S.; Peng, J.; Cheng, J.; Yin, P. Short-Term Effect of Temperature Change on Non-Accidental Mortality in Shenzhen, China. Int. J. Environ. Res. Public Health 2021, 18, 8760. https://doi.org/10.3390/ijerph18168760
Xiao Y, Meng C, Huang S, Duan Y, Liu G, Yu S, Peng J, Cheng J, Yin P. Short-Term Effect of Temperature Change on Non-Accidental Mortality in Shenzhen, China. International Journal of Environmental Research and Public Health. 2021; 18(16):8760. https://doi.org/10.3390/ijerph18168760
Chicago/Turabian StyleXiao, Yao, Chengzhen Meng, Suli Huang, Yanran Duan, Gang Liu, Shuyuan Yu, Ji Peng, Jinquan Cheng, and Ping Yin. 2021. "Short-Term Effect of Temperature Change on Non-Accidental Mortality in Shenzhen, China" International Journal of Environmental Research and Public Health 18, no. 16: 8760. https://doi.org/10.3390/ijerph18168760
APA StyleXiao, Y., Meng, C., Huang, S., Duan, Y., Liu, G., Yu, S., Peng, J., Cheng, J., & Yin, P. (2021). Short-Term Effect of Temperature Change on Non-Accidental Mortality in Shenzhen, China. International Journal of Environmental Research and Public Health, 18(16), 8760. https://doi.org/10.3390/ijerph18168760






