Mental Health and Personality Traits during COVID-19 in China: A Latent Profile Analysis
Abstract
1. Introduction
1.1. Person-Centered Approaches
1.2. The Present Study
2. Methods
2.1. Participants
2.2. Measures
2.3. Statistical Analysis
3. Results
Comparison among Latent Profiles
4. Discussion
5. Limitations and Recommendations
6. Implications
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahmed, M.Z.; Ahmed, O.; Aibao, Z.; Hanbin, S.; Siyu, L.; Ahmad, A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatry 2020, 51, 102092. [Google Scholar] [CrossRef]
- Worldometer. China Coronavirus Cases. 2020. Available online: https://www.worldometers.info/coronavirus/country/china/ (accessed on 6 December 2020).
- Tandon, R. COVID-19 and mental health: Preserving humanity, maintaining sanity, and promoting health. Asian J. Psychiatry 2020, 51, 102256. [Google Scholar] [CrossRef]
- Coronavirus: 4.5 Billion People Confined. Available online: https://www.barrons.com/news/coronavirus-4-5-billion-people-confined-01587139808 (accessed on 17 January 2021).
- Denworth, L. The Biggest Psychological Experiment in History is Running Now. Scientific American. 2020. Available online: https://www.scientificamerican.com/interactive/the-biggest-psychological-experiment-in-history-is-running-now/ (accessed on 27 November 2020).
- Galea, S.; Merchant, R.M.; Lurie, N. The mental health consequences of COVID-19 and physical distancing. JAMA Intern. Med. 2020, 180, 817. [Google Scholar] [CrossRef]
- Semo, B.; Frissa, S.M. The mental health impact of the COVID-19 pandemic: Implications for sub-Saharan Africa. Psychol. Res. Behav. Manag. 2020, 13, 713–720. [Google Scholar] [CrossRef]
- Wan, W. The coronavirus pandemic is pushing America into a mental health crisis. Washington Post. 5 May 2020. Available online: https://www.washingtonpost.com/health/2020/05/04/mental-health-coronavirus/ (accessed on 22 January 2021).
- Pan, K.; Kok, A.A.; Eikelenboom, M.; Horsfall, M.; Jörg, F.; Luteijn, R.A.; Penninx, B.W. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry 2021, 8, 121–129. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Zortea, T.C.; Brenna, C.T.A.; Joyce, M.; McClelland, H.; Tippett, M.; Tran, M.M.; Arensman, E.; Corcoran, P.; Hatcher, S.; Heisel, M.J.; et al. The Impact of Infectious Disease-Related Public Health Emergencies on Suicide, Suicidal Behavior, and Suicidal Thoughts. Crisis 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Ammerman, B.A.; Burke, T.A.; Jacobucci, R.; McClure, K. Preliminary investigation of the association between COVID-19 and suicidal thoughts and behaviors in the U.S. J. Psychiatr. Res. 2021, 134, 32–38. [Google Scholar] [CrossRef]
- Aschwanden, D.; Strickhouser, J.E.; Sesker, A.A.; Lee, J.H.; Luchetti, M.; Stephan, Y.; Terracciano, A. Psychological and behavioural responses to coronavirus disease 2019: The role of personality. Eur. J. Personal. 2021, 35, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Sutin, A.R.; Luchetti, M.; Aschwanden, D.; Lee, J.H.; Sesker, A.A.; Strickhouser, J.E.; Terracciano, A. Change in five-factor model personality traits during the acute phase of the coronavirus pandemic. PLoS ONE 2020, 15, e0237056. [Google Scholar] [CrossRef] [PubMed]
- Hill, P.L.; Turiano, N.A.; Hurd, M.D.; Mroczek, D.K.; Roberts, B.W. Conscientiousness and longevity: An examination of possible mediators. Health Psychol. 2011, 30, 536–541. [Google Scholar] [CrossRef] [PubMed]
- McCrae, R.R.; Terracciano, A. Universal features of personality traits from the observer’s perspective: Data from 50 cultures. J. Personal. Soc. Psychol. 2005, 88, 547–561. [Google Scholar] [CrossRef] [PubMed]
- Turiano, N.A.; Chapman, B.P.; Gruenewald, T.L.; Mroczek, D.K. Personality and the leading behavioral contributors of mortality. Health Psychol. 2015, 34, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Jokela, M.; Hintsanen, M.; Hakulinen, C.; Batty, G.D.; Nabi, H.; Singh-Manoux, A.; Kivimäki, M. Association of personality with the development and persistence of obesity: A meta-analysis based on individual—Participant data. Obes. Rev. 2012, 14, 315–323. [Google Scholar] [CrossRef]
- Kern, M.L.; Friedman, H.S. Personality and pathways of influence on physical health. Soc. Personal. Psychol. Compass 2011, 5, 76–87. [Google Scholar] [CrossRef]
- Buecker, S.; Maes, M.; Denissen, J.J.; Luhmann, M. Loneliness and the Big Five Personality Traits: A Meta-analysis. Eur. J. Personal. 2020, 34, 8–28. [Google Scholar] [CrossRef]
- Modersitzki, N.; Phan, L.V.; Kuper, N.; Rauthmann, J.F. Who Is mpacted? Personality predicts individual differences in psychological consequences of the COVID-19 pandemic in Germany. Soc. Psychol. Personal. Sci. 2020, 12, 1110–1130. [Google Scholar] [CrossRef]
- Liu, S.; Lithopoulos, A.; Zhang, C.; Garcia-Barrera, M.A.; Rhodes, R.E. Personality and perceived stress during COVID-19 pandemic: Testing the mediating role of perceived threat and efficacy. Personal. Individ. Differ. 2021, 168, 110351. [Google Scholar] [CrossRef]
- Mõttus, R.; Realo, A.; Allik, J.; Esko, T.; Metspalu, A. History of the diagnosis of a sexually transmitted disease is linked to normal variation in personality traits. J. Sex. Med. 2012, 9, 2861–2867. [Google Scholar] [CrossRef]
- Weiss, A.; Deary, I.J. A new look at neuroticism: Should we worry so much about worrying? Curr. Dir. Psychol. Sci. 2019, 29, 92–101. [Google Scholar] [CrossRef]
- Srivastava, S.; Angelo, K.M.; Vallereux, S.R. Extraversion and positive affect: A day reconstruction study of person—environment transactions. J. Res. Personal. 2008, 42, 1613–1618. [Google Scholar] [CrossRef]
- Harris, K.; English, T.; Harms, P.D.; Gross, J.J.; Jackson, J.J. Why are extraverts more satisfied? Personality, social experiences, and subjective well-being in college. Eur. J. Personal. 2017, 31, 170–186. [Google Scholar] [CrossRef]
- Asendorpf, J.B.; Wilpers, S. Personality effects on social relationships. J. Personal. Soc. Psychol. 1998, 74, 1531–1544. [Google Scholar] [CrossRef]
- Steel, P.; Schmidt, J.; Shultz, J. Refining the relationship between personality and subjective well-being. Psychol. Bull. 2008, 134, 138–161. [Google Scholar] [CrossRef] [PubMed]
- Keiser, C. How the Big Five Personality Traits Predicted COVID Shelter-in-Place Compliance (4 November 2020). Available online: https://www.verywellmind.com/personality-and-shelter-in-place-compliance-5085423 (accessed on 28 November 2020).
- Stadler, M.; Niepel, C.; Botes, E.; Dörendahl, J.; Krieger, F.; Greiff, S. Individual Psychological Responses to the SARS-CoV-2 Pandemic: Different Clusters and Their Relation to Risk-Reducing Behavior. arXiv 2020, arXiv:PPR330587. [Google Scholar]
- Carvalho, L.D.; Pianowski, G.; Gonçalves, A.P. Personality differences and COVID-19: Are extroversion and conscientiousness personality traits associated with engagement with containment measures? Trends Psychiatry Psychother. 2020, 42, 179–184. [Google Scholar] [CrossRef]
- Blagov, P.S. Adaptive and Dark Personality in the COVID-19 Pandemic: Predicting Health-Behavior Endorsement and the Appeal of Public-Health Messages. Soc. Psychol. Personal. Sci. 2020, 12, 697–707. [Google Scholar] [CrossRef]
- Bogg, T.; Milad, E. Demographic, personality, and social cognition correlates of coronavirus guideline adherence in a U.S. sample. Health Psychol. 2021, 39, 1026–1036. [Google Scholar] [CrossRef] [PubMed]
- Asendorpf, J.B. Person-centered approaches to personality. In APA Handbook of Personality and Social Psychology, Vol. 4. Personality Processes and Individual Differences; Mikulincer, M., Shaver, P.R., Cooper, M.L., Larsen, R.J., Eds.; American Psychological Association: Washington, DC, USA, 2015; pp. 403–424. [Google Scholar] [CrossRef]
- Masyn, K.E. Latent class analysis and finite mixture modeling. In the Oxford Handbook of Quantitative Methods; Little, T.D., Ed.; Oxford University Press: New York, NY, USA, 2013; Volume 2, pp. 551–611. [Google Scholar] [CrossRef]
- Isler, L.; Fletcher, G.J.O.; Liu, J.H.; Sibley, C.G. Validation of the four-profile configuration of personality types within the Five-Factor Model. Personal. Individ. Differ. 2017, 106, 257–262. [Google Scholar] [CrossRef]
- Robins, R.W.; John, O.P.; Caspi, A.; Moffitt, T.E.; Stouthamer-Loeber, M. Resilient, overcontrolled, and undercontrolled boys: Three replicable personality types. J. Personal. Soc. Psychol. 1996, 70, 157–171. [Google Scholar] [CrossRef]
- Asendorpf, J.B.; Borkenau, P.; Ostendorf, F.; Aken, M.A. Carving personality description at its joints: Confirmation of three replicable personality prototypes for both children and adults. Eur. J. Personal. 2001, 15, 169–198. [Google Scholar] [CrossRef]
- Barbaranelli, C. Evaluating cluster analysis solutions: An application to the Italian NEO personality inventory. Eur. J. Personal. 2002, 16, S43–S55. [Google Scholar] [CrossRef]
- Boehm, B.; Asendorpf, J.B.; Avia, M.D. Replicable types and subtypes of personality: Spanish NEO-PI samples. Eur. J. Personal. 2002, 16, S25–S41. [Google Scholar] [CrossRef]
- Bohane, L.; Maguire, N.; Richardson, T. Resilients, overcontrollers and undercontrollers: A systematic review of the utility of a personality typology method in understanding adult mental health problems. Clin. Psychol. Rev. 2017, 57, 75–92. [Google Scholar] [CrossRef]
- McDevitt-Murphy, M.E.; Shea, M.T.; Yen, S.; Grilo, C.M.; Sanislow, C.A.; Markowitz, J.C.; Skodol, A.E. Prospective investigation of a PTSD personality typology among individuals with personality disorders. Compr. Psychiatry 2012, 53, 441–450. [Google Scholar] [CrossRef]
- Ashton, M.C.; Lee, K. An investigation of personality types within the HEXACO personality framework. J. Individ. Differ. 2009, 30, 181–187. [Google Scholar] [CrossRef]
- Daljeet, K.N.; Bremner, N.L.; Giammarco, E.A.; Meyer, J.P.; Paunonen, S.V. Taking a person-centered approach to personality: A latent-profile analysis of the HEXACO model of personality. J. Res. Personal. 2017, 70, 241–251. [Google Scholar] [CrossRef]
- Isler, L.; Liu, J.H.; Sibley, C.G.; Fletcher, G.J.O. Self—Regulation and Personality Profiles: Empirical Development, Longitudinal Stability and Predictive Ability. Eur. J. Personal. 2016, 30, 274–287. [Google Scholar] [CrossRef]
- Costa, P.T.; Herbst, J.H.; McCrae, R.R.; Samuels, J.; Ozer, D.J. The replicability and utility of three personality types. Eur. J. Personal. 2002, 16, S73–S87. [Google Scholar] [CrossRef]
- Asendorpf, J.B. Head-to-head comparison of the predictive validity of personality types and dimensions. Eur. J. Personal. 2003, 17, 327–346. [Google Scholar] [CrossRef]
- Asendorpf, J.B.; Denissen, J.J.A. Predictive validity of personality types versus personality dimensions from early childhood to adulthood: Implications for the distinction between core and surface traits. Merrill-Palmer Q. 2006, 52, 486–513. [Google Scholar] [CrossRef]
- Hart, D.; Atkins, R.; Fegley, S. Personality and development in childhood: A person-centered approach. Monogr. Soc. Res. Child Dev. 2003, 68, vii-109. [Google Scholar] [CrossRef]
- Herzberg, P.Y.; Hoyer, J. Personality prototypes in adult offenders. Crim. Justice Behav. 2008, 36, 259–274. [Google Scholar] [CrossRef]
- Ekehammar, B.; Akrami, N. The relation between personality and prejudice: A variable- and a person-centred approach. Eur. J. Personal. 2003, 17, 449–464. [Google Scholar] [CrossRef]
- Ahmed, O.; Hossain, K.N.; Siddique, R.F.; Jobe, M.C. COVID-19 fear, stress, sleep quality and coping activities during lockdown, and personality traits: A person-centered approach analysis. Personal. Individ. Differ. 2021, 178, 110873. [Google Scholar] [CrossRef]
- Bienvenu, O.J.; Stein, M.B. Personality and anxiety disorders: A review. J. Personal. Disord. 2003, 17, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Brandes, M.; Bienvenu, O.J. Personality and anxiety disorders. Curr. Psychiatry Rep. 2006, 8, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Klein, D.N.; Kotov, R.; Bufferd, S.J. Personality and depression: Explanatory models and review of the evidence. Annu. Rev. Clin. Psychol. 2011, 7, 269–295. [Google Scholar] [CrossRef] [PubMed]
- Jakšić, N.; Brajković, L.; Ivezić, E.; Topić, R.; Jakovljević, M. The role of personality traits in posttraumatic stress disorder (PTSD). Psychiatr. Danub. 2012, 24, 256–266. [Google Scholar]
- Mochcovitch, M.D.; Nardi, A.E.; Cardoso, A. Temperament and character dimensions and their relationship to major depression and panic disorder. Rev. Bras. Psiquiatr. 2012, 34, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Davide, P.; Andrea, P.; Martina, O.; Andrea, E.; Davide, D.; Mario, A. The impact of the COVID-19 pandemic on patients with OCD: Effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res. 2020, 291, 113213. [Google Scholar] [CrossRef]
- Shafran, R.; Coughtrey, A.; Whittal, M. Recognising and addressing the impact of COVID-19 on obsessive-compulsive disorder. Lancet Psychiatry 2020, 7, 570–572. [Google Scholar] [CrossRef]
- Lochner, C.; Seedat, S.; du Toit, P.L.; Nel, D.G.; Niehaus, D.J.; Sandler, R.; Stein, D.J. Obsessive-compulsive disorder and trichotillomania: A phenomenological comparison. BMC Psychiatry 2005, 5, 2. [Google Scholar] [CrossRef]
- Zinbarg, R.E.; Barlow, D.H. Structure of anxiety and the anxiety disorders: A hierarchical model. J. Abnorm. Psychol. 1996, 105, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. JAMA Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Wang, B.D. A Study on the Application of PHQ-9 and GAD-7 in Patients with Malignant Tumors. Master’s Dissertation, Central South University, Beijing, China, 2013. (In Chinese) [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Litz, B.T.; Herman, D.S.; Huska, J.A.; Keane, T.M. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. In Proceedings of the 9th Annual Meeting of International Society for Traumatic Stress Studies (Trauma 1993, Coping, and Adaptation), San Antonio, TX, USA, 1 January 1993. [Google Scholar]
- Yang, X.Y.; Yang, H.A.; Liu, Q.G.; Yang, L.Z. The research on the reliability and validity of PCL-C and influence factors. J. Chin. Health Psychol. 2007, 15, 6–9. [Google Scholar]
- Goodman, W.K.; Price, L.H.; Rasmussen, S.A.; Mazure, C.; Fleischmann, R.L.; Hill, C.L.; Charney, D.S. The Yale-Brown Obsessive Compulsive Scale: I. Development 1989, use, and reliability. Arch. Gen. Psychiatry 1989, 46, 1006–1011. [Google Scholar] [CrossRef]
- Chunyan, Z. Study on False Feedback Processing Characteristics and Neural Mechanisms in Patients with Obsessive Compulsive Disorder. Ph.D. Thesis, Anhui Medical University, Hefei, China, 2014. (In Chinese). [Google Scholar]
- Rammstedt, B.; John, O.P. Measuring personality in one minute or less: A 10-item short version of the Big Five Inventory in English and German. J. Res. Personal. 2007, 41, 203–212. [Google Scholar] [CrossRef]
- Deng, S.-C.; Gao, J. Big Five personality and impulsive buying: The mediation of self-control and sensation seeking. Chin. J. Clin. Psychol. 2015, 23, 1098–1101. [Google Scholar] [CrossRef]
- Clark, L.A.; Watson, D. Constructing validity: Basic issues in objective scale development. Psychol. Assess. 1995, 7, 309–319. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications and Programming; Routledge: New York, NY, USA, 2016. [Google Scholar]
- Fisher, P.A.; Robie, C. A latent profile analysis of the Five Factor Model of personality: A constructive replication and extension. Personal. Individ. Differ. 2019, 139, 343–348. [Google Scholar] [CrossRef]
- Ferguson, S.L.; Hull, D.M. Personality profiles: Using latent profile analysis to model personality typologies. Personal. Individ. Differ. 2018, 122, 177–183. [Google Scholar] [CrossRef]
- Merz, E.L.; Roesch, S.C. A latent profile analysis of the Five Factor Model of personality: Modeling trait interactions. Personal. Individ. Differ. 2011, 51, 915–919. [Google Scholar] [CrossRef] [PubMed]
- Musek, J. A general factor of personality: Evidence for the Big One in the five-factor model. J. Res. Personal. 2007, 41, 1213–1233. [Google Scholar] [CrossRef]
- Musek, J. The General Factor of Personality, 1st ed.; Academic Press: London, UK, 2017. [Google Scholar]
- Duggan, C.; Milton, J.; Egan, V.; McCarthy, L.; Palmer, B.; Lee, A. Theories of general personality and mental disorder. Br. J. Psychiatry 2003, 182, S19–S23. [Google Scholar] [CrossRef]
- Hu, T.; Zhang, D.; Wang, J. A meta-analysis of the trait resilience and mental health. Personal. Individ. Differ. 2015, 76, 18–27. [Google Scholar] [CrossRef]
- Bienvenu, O.J.; Samuels, J.F.; Costa, P.T.; Reti, I.M.; Eaton, W.W.; Nestadt, G. Anxiety and depressive disorders and the five-factor model of personality: A higher- and lower-order personality trait investigation in a community sample. Depress. Anxiety 2004, 20, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Klimstra, T.A.; Akse, J.; Hale, W.W.; Raaijmakers, Q.A.; Meeus, W.H. Longitudinal associations between personality traits and problem behavior symptoms in adolescence. J. Res. Personal. 2010, 44, 273–284. [Google Scholar] [CrossRef]
- Chang, H.J.; Chen, W.X.; Lin, E.C.; Tung, Y.Y.; Fetzer, S.; Lin, M.F. Delay in seeking medical evaluations and predictors of self-efficacy among women with newly diagnosed breast cancer: A longitudinal study. Int. J. Nurs. Stud. 2014, 51, 1036–1047. [Google Scholar] [CrossRef]
- Fernández, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Pedreira, M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J. Affect. Disord. 2020, 277, 75–84. [Google Scholar] [CrossRef]
- Ferguson, E. Personality and coping traits: A joint factor analysis. Br. J. Health Psychol. 2001, 6, 311–325. [Google Scholar] [CrossRef]
- Lewis, E.G.; Cardwell, J.M. The big Five personality traits, perfectionism and their association with mental health among UK students on professional degree programmes. BMC Psychol. 2020, 8, 54. [Google Scholar] [CrossRef] [PubMed]
- Sperandeo, R.; Messina, G.; Iennaco, D.; Sessa, F.; Russo, V.; Polito, R.; Monda, V.; Monda, M.; Messina, A.; Mosca, L.L.; et al. What does personality mean in the context of mental health? A topic modeling approach based on abstracts published in Pubmed over the last 5 years. Front. Psychiatry 2020, 10, 938. [Google Scholar] [CrossRef] [PubMed]
- Ornell, F.; Halpern, S.C.; Kessler, F.H.; Narvaez, J.C. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. Cadernos De Saúde Pública 2020, 36, e00063520. [Google Scholar] [CrossRef] [PubMed]
- Gloster, A.T.; Lamnisos, D.; Lubenko, J.; Presti, G.; Squatrito, V.; Constantinou, M.; Nicolaou, C.; Papacostas, S.; Aydın, G.; Chong, Y.Y.; et al. Impact of covid-19 pandemic on mental health: An international study. PLoS ONE 2020, 15, e0244809. [Google Scholar] [CrossRef] [PubMed]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and social isolation as risk factors for mortality. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef]
| Variables | Groups | Frequency (%) |
|---|---|---|
| Gender | Female | 603 (52.6%) |
| Male | 543 (47.4%) | |
| Education | Junior school and below | 135 (11.8%) |
| High school/technical secondary school/technical school | 355 (31%) | |
| University degree (specialized) | 379 (33.1%) | |
| Bachelor | 260 (22.7%) | |
| Masters | 17 (1.5%) | |
| Marital Status | Unmarried | 174 (15.2%) |
| Married | 937 (81.8%) | |
| Divorced | 30 (2.6%) | |
| Widow/Widower | 5 (0.4%) | |
| Profession | Student | 83 (7.2%) |
| Full time employee | 391 (34.1%) | |
| Part time employee | 243 (21.2%) | |
| Business management | 104 (9.1%) | |
| Self employed | 203 (17.7%) | |
| Unemployed | 103 (9.0%) | |
| Other | 19 (1.7%) | |
| Monthly Income | 0–5000 Yuan | 917 (80.1%) |
| 5001–10,000 Yuan | 152 (13.2%) | |
| 10,001 and above Yuan | 49 (4.3%) | |
| Don’t want to disclose | 28 (2.4%) |
| Solutions | AIC | BIC | SABIC | Entropy | LMRT (p Value) | Class Size | Average Class Probabilities for Most Likely Latent Class Membership by Latent Class | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||||||
| 2 | 14,784.20 | 14,858.43 | 14,807.63 | 0.84 | 1234.19 (<0.001) | 484 (63.3%) | 0.956 | 0.044 | ||
| 281 (36.7%) | 0.051 | 0.949 | ||||||||
| 3 | 14,445.30 | 14,547.38 | 14,477.52 | 0.80 | 342.30 (0.001) | 176 (23.0%) | 0.895 | 0.105 | 0.000 | |
| 386 (50.5%) | 0.068 | 0.901 | 0.031 | |||||||
| 203 (26.5%) | 0.000 | 0.077 | 0.923 | |||||||
| 4 | 14,358.69 | 14,488.60 | 14,399.69 | 0.77 | 96.20 (0.072) | 101 (13.2%) | 0.882 | 0.000 | 0.000 | 0.118 |
| 99 (12.9%) | 0.000 | 0.895 | 0.105 | 0.000 | ||||||
| 208 (27.2%) | 0.000 | 0.069 | 0.834 | 0.097 | ||||||
| 357 (46.7%) | 0.057 | 0.000 | 0.068 | 0.088 | ||||||
| Outcomes | Model 1 | Model 2 | ||
|---|---|---|---|---|
| Profiles | Traits | Traits | Profiles | |
| Depression | 0.015 | 0.015 * | 0.028 | 0.003 |
| Anxiety | 0.028 | 0.011 | 0.030 | 0.009 * |
| PTSD symptoms | 0.034 | 0.014 | 0.043 | 0.004 |
| OCD symptoms | 0.006 | 0.014 | 0.017 | 0.004 |
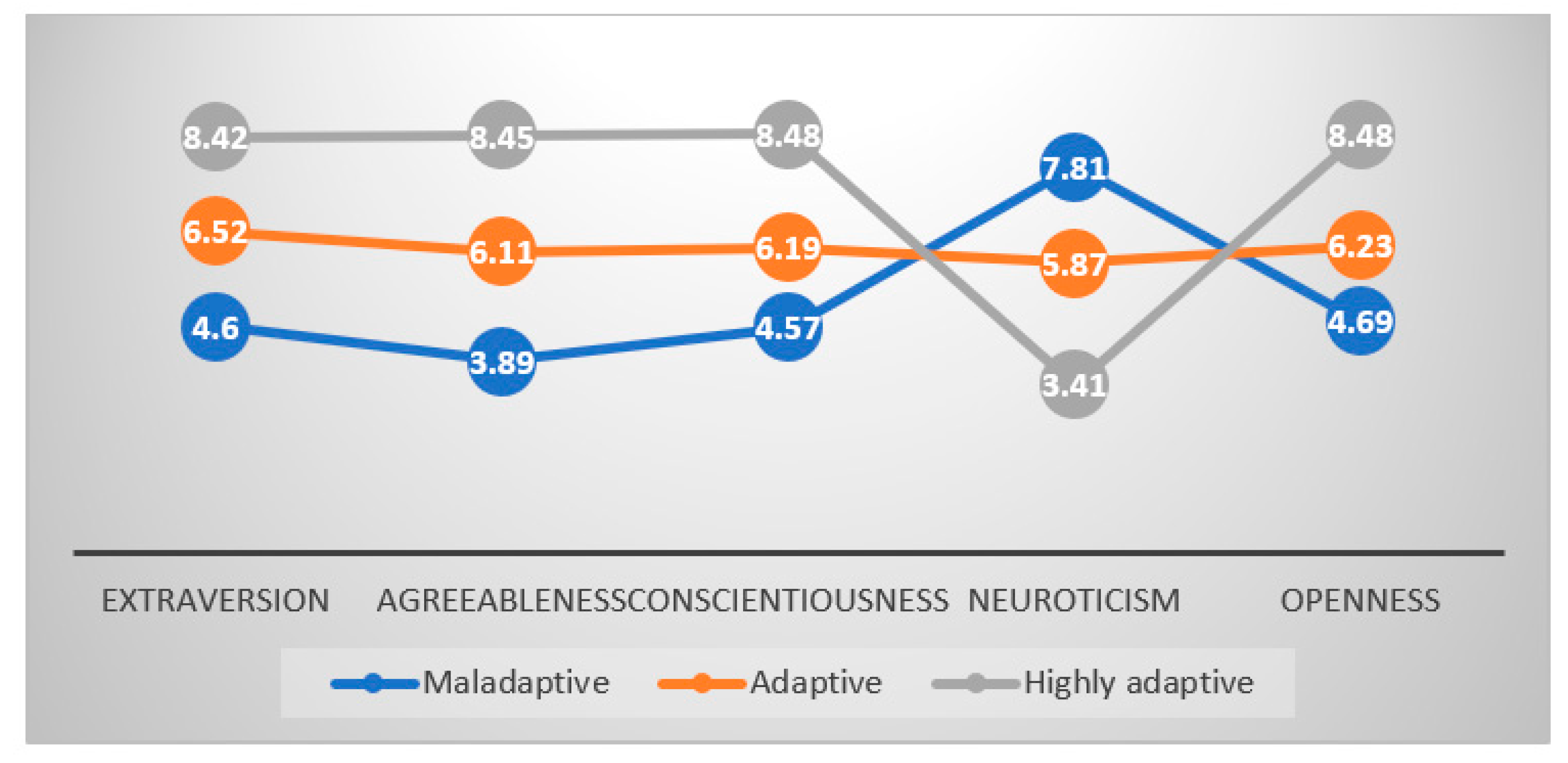
| Profiles | n | Extraversion | Agreeableness | Conscientiousness | Neuroticism | Openness |
|---|---|---|---|---|---|---|
| Maladaptive | 176 | 4.60 (1.33) | 3.89 (1.07) | 4.57 (1.33) | 7.81 (1.14) | 4.69 (1.34) |
| Adaptive | 386 | 6.52 (1.47) | 6.11 (1.42) | 6.19 (1.43) | 5.87 (1.36) | 6.23 (1.41) |
| Highly adaptive | 203 | 8.42 (1.24) | 8.45 (1.24) | 8.48 (1.17) | 3.41 (1.13) | 8.48 (1.21) |
| Maladaptive | Adaptive | Highly Adaptive | F-Value (sig.) | Partial Eta Squared | |
|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |||
| Anxiety | 7.46(6.25) | 7.53 (5.46) | 5.41 (4.79) | 10.15 (<0.001) | 0.028 |
| Depression | 9.59 (7.19) | 9.36 (6.09) | 7.66 (5.89) | 5.04 (0.003) | 0.015 |
| PTSD symptoms | 42.04 (18.09) | 41.23 (14.51) | 35.36 (11.13) | 13.22 (<0.001) | 0.034 |
| OCD symptoms | 10.98 (7.49) | 11.71 (6.69) | 10.44 (6.44) | 2.43 (0.088) | 0.006 |
| Dependent Variable | (I) Latent Profiles | (J) Latent Profiles | Mean Difference (I–J) | Sig. | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Anxiety | Maladaptive | Adaptive | −0.07 | 0.887 | −1.05 | 0.91 |
| Highly adaptive | 2.05 | <0.001 | 0.94 | 3.16 | ||
| Adaptive | Highly adaptive | 2.12 | <0.001 | 1.19 | 3.06 | |
| Depression | Maladaptive | Adaptive | 0.23 | 0.692 | −0.90 | 1.35 |
| Highly adaptive | 1.93 | 0.003 | 0.65 | 3.20 | ||
| Adaptive | Highly adaptive | 1.70 | 0.002 | 0.62 | 2.77 | |
| PTSD symptoms | Maladaptive | Adaptive | 0.81 | 0.541 | −1.80 | 3.43 |
| Highly adaptive | 6.68 | <0.001 | 3.72 | 9.64 | ||
| Adaptive | Highly adaptive | 5.87 | <0.001 | 3.37 | 8.36 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, M.; Ahmed, M.Z.; Hiramoni, F.A.; Zhou, A.; Ahmed, O.; Griffiths, M.D. Mental Health and Personality Traits during COVID-19 in China: A Latent Profile Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8693. https://doi.org/10.3390/ijerph18168693
Li M, Ahmed MZ, Hiramoni FA, Zhou A, Ahmed O, Griffiths MD. Mental Health and Personality Traits during COVID-19 in China: A Latent Profile Analysis. International Journal of Environmental Research and Public Health. 2021; 18(16):8693. https://doi.org/10.3390/ijerph18168693
Chicago/Turabian StyleLi, Mei, Md Zahir Ahmed, Fatema Akhter Hiramoni, Aibao Zhou, Oli Ahmed, and Mark D. Griffiths. 2021. "Mental Health and Personality Traits during COVID-19 in China: A Latent Profile Analysis" International Journal of Environmental Research and Public Health 18, no. 16: 8693. https://doi.org/10.3390/ijerph18168693
APA StyleLi, M., Ahmed, M. Z., Hiramoni, F. A., Zhou, A., Ahmed, O., & Griffiths, M. D. (2021). Mental Health and Personality Traits during COVID-19 in China: A Latent Profile Analysis. International Journal of Environmental Research and Public Health, 18(16), 8693. https://doi.org/10.3390/ijerph18168693






