Psychosomatic Symptoms and Neuroticism following COVID-19: The Role of Online Aggression toward a Stigmatized Group
Abstract
:1. Introduction
1.1. Stigmatization of Hubei/Chinese Residents
1.2. On-Line Aggression toward Stigmatized Groups
1.3. Vulnerability and Aggression
1.4. Mental Problems of Perpetrators
1.5. The Current Research
2. Study 1
2.1. Method
2.2. Results and Discussion
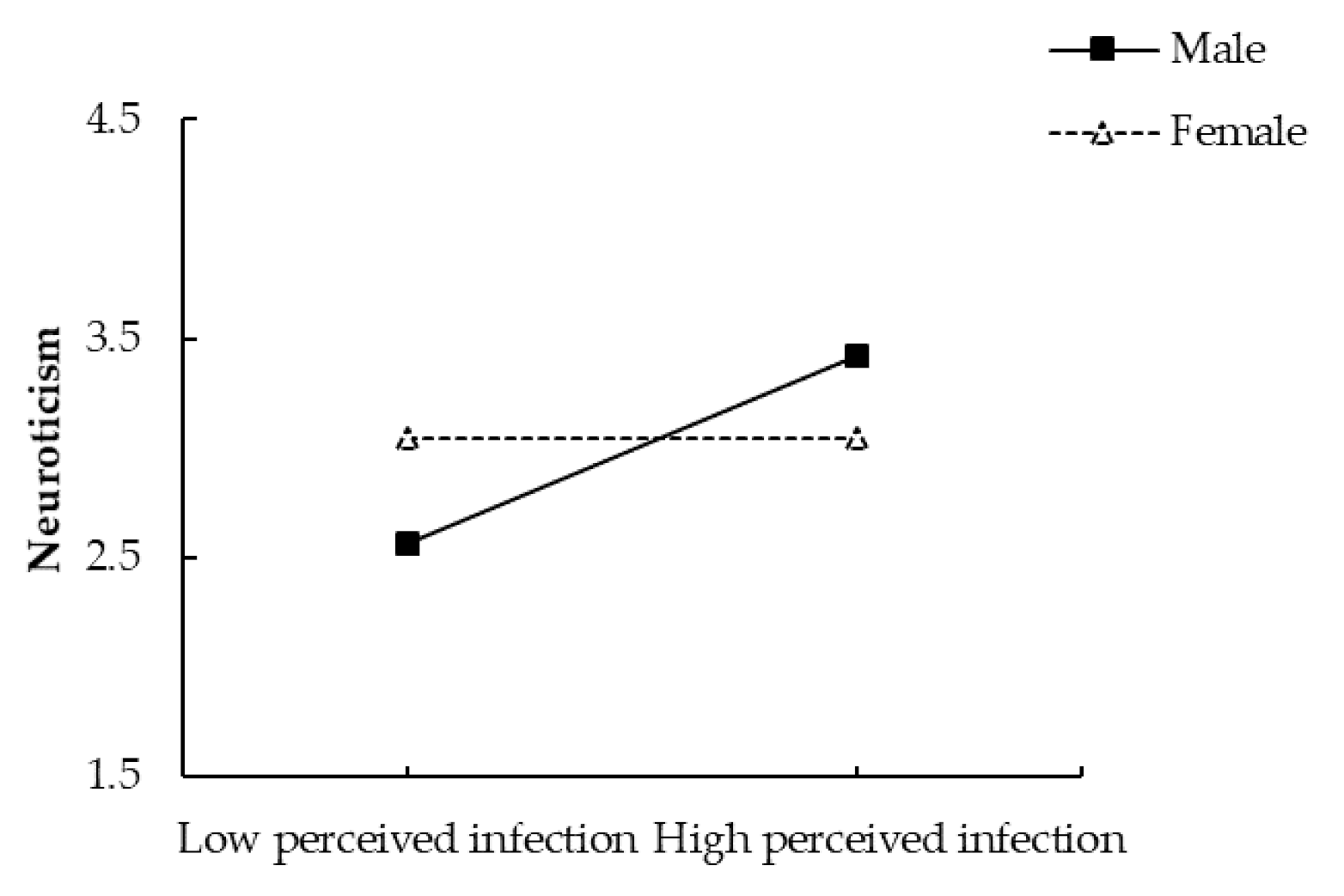
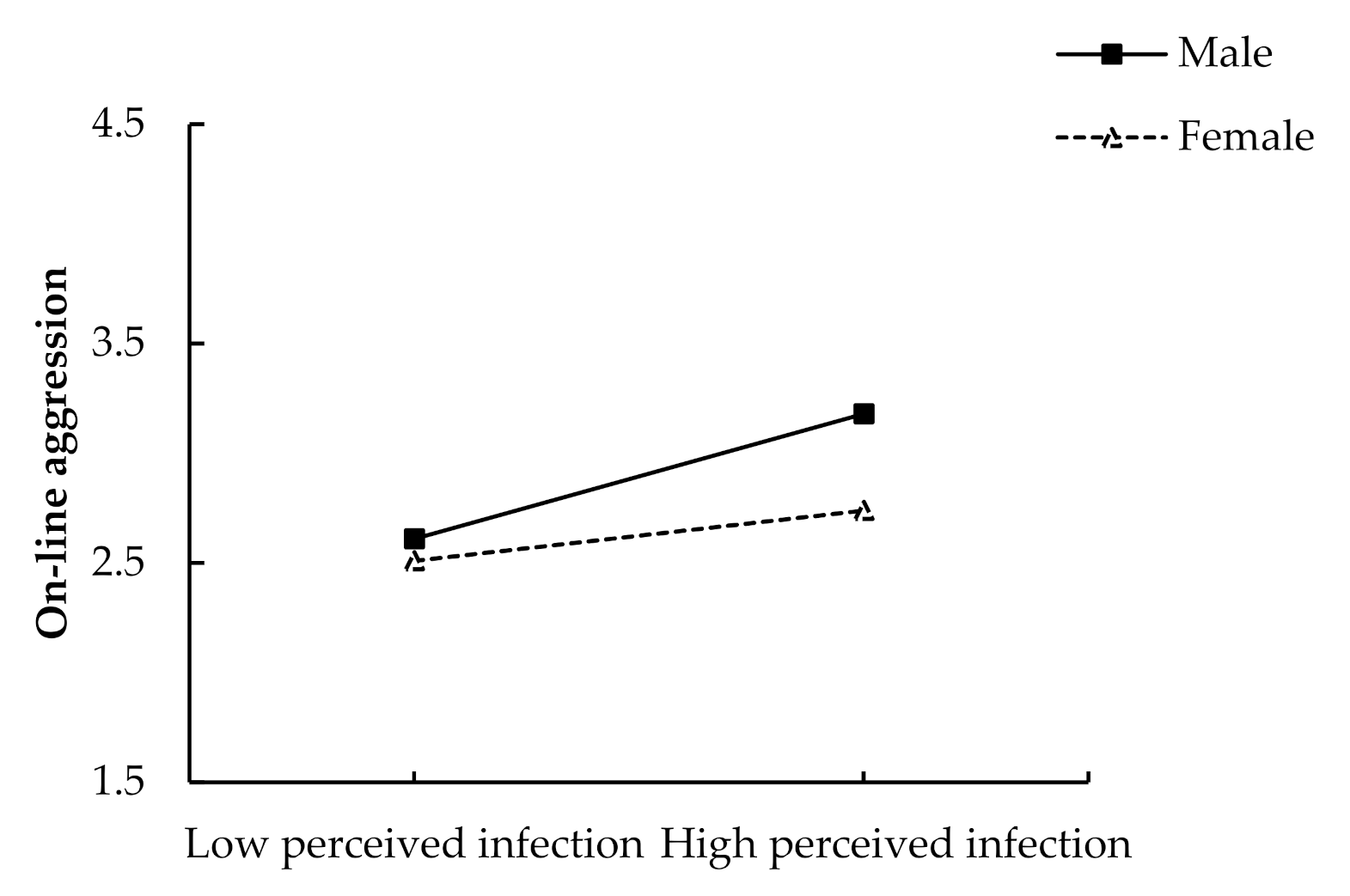
2.2.1. Moderation Analyses
2.2.2. Moderated Mediation Analysis
3. Study 2
3.1. Method
3.2. Results and Discussion
3.2.1. Moderation Analyses
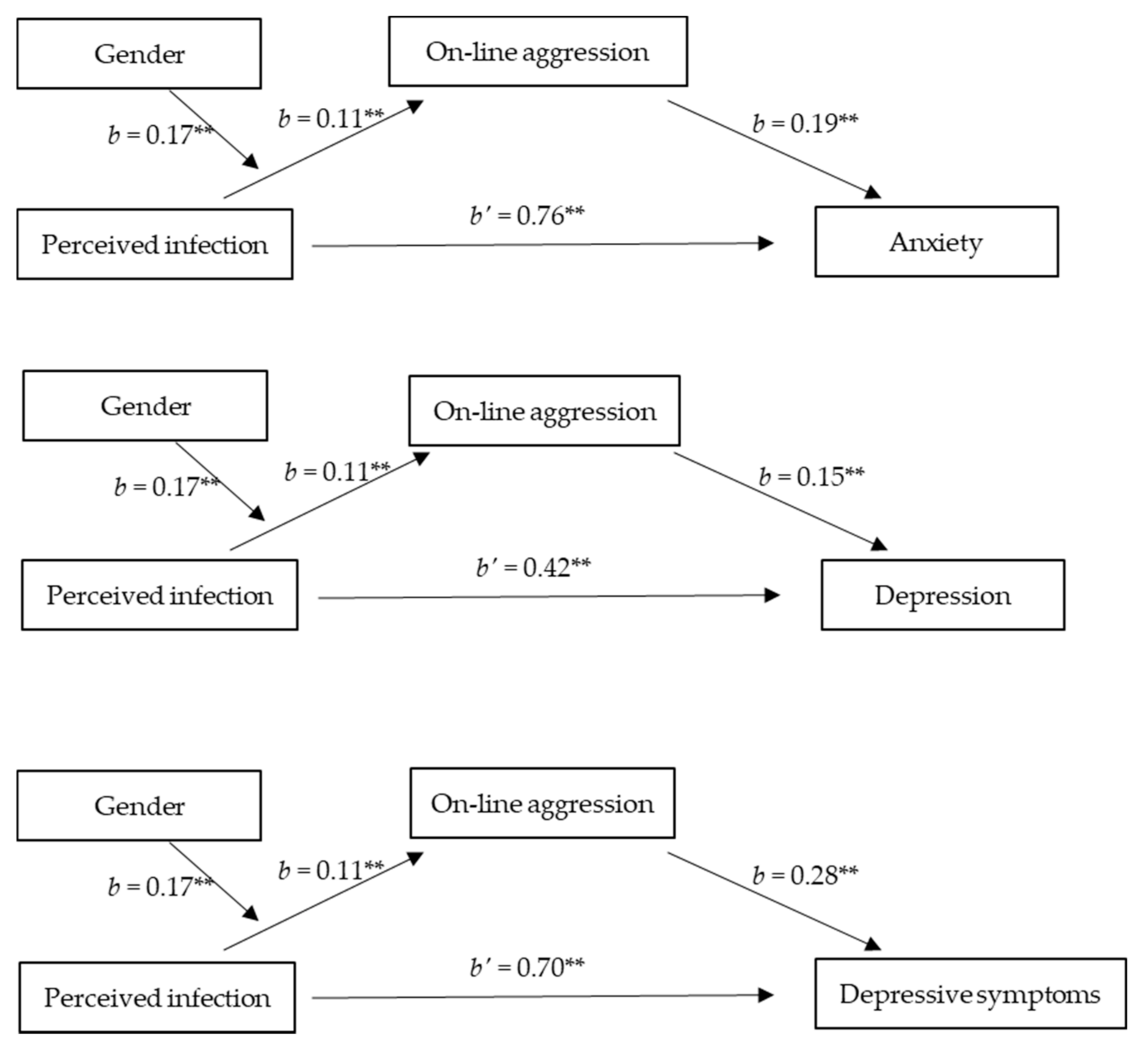
3.2.2. Moderated Mediation Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crandall, C.S.; Coleman, R. Aids-related stigmatization and the disruption of social Relationships. J. Soc. Pers. Relatsh. 1992, 9, 163–177. [Google Scholar] [CrossRef]
- Gilmore, N.; Somerville, M.A. Stigmatization, scapegoating and discrimination in sexually transmitted diseases: Overcoming ‘them’ and ‘us’. Soc. Sci. Med. 1994, 39, 1339–1358. [Google Scholar] [CrossRef]
- Lee, S.; Chan, L.Y.Y.; Chau, A.M.Y.; Kwok, K.P.S.; Kleinman, A. The experience of SARS-related stigma at Amory Gardens. Soc. Sci. Med. 2005, 61, 2038–2046. [Google Scholar] [CrossRef] [PubMed]
- Schaller, M. Parasites, behavioral defenses, and the social psychological mechanisms through which cultures are evoked. Psychol. Inq. 2006, 17, 96–101. [Google Scholar] [CrossRef]
- Kurzban, R.; Leary, M.R. Evolutionary origins of stigmatization: The functions of social exclusion. Psychol. Bull. 2001, 127, 187–208. [Google Scholar] [CrossRef] [Green Version]
- Schaller, M.; Park, J.H.; Mueller, A. Fear of the dark: Interactive effects of beliefs about danger and ambient darkness on ethnic stereotypes. Personal. Soc. Psychol. Bull. 2003, 29, 637–649. [Google Scholar] [CrossRef] [Green Version]
- Zebrowitz, L.A.; Rhodes, G. Sensitivity to “bad genes” and the anomalous face overgeneralization effect: Cue validity, cue utilization, and accuracy in judging intelligence and health. J. Nonverbal Behav. 2004, 28, 167–185. [Google Scholar] [CrossRef]
- Haselton, M.G.; Nettle, D. The Paranoid optimist: An integrative evolutionary model of cognitive biases. Personal. Soc. Psychol. Rev. 2006, 10, 47–66. [Google Scholar] [CrossRef]
- Goffman, E. Asylums: Essays on the Social Situation of Mental Patients and other Inmates; Doubleday: New York, NY, USA; Anchor: New York, NY, USA, 1968. [Google Scholar]
- Stocking, M.A. Tropical soils and food security: The next 50 years. Science 2003, 302, 1356–1359. [Google Scholar] [CrossRef] [Green Version]
- Ferguson, C.J.; Beaver, K.M. Natural born killers: The genetic origins of extreme violence. Aggress. Violent Behav. 2009, 14, 286–294. [Google Scholar] [CrossRef]
- Jokela, M.; Keltikangas-Järvinen, L. Adolescent leadership and adulthood fertility: Revisiting the “central theoretical problem of human sociobiology”. J. Personal. 2009, 77, 213–230. [Google Scholar] [CrossRef] [PubMed]
- Crick, N.R.; Grotpeter, J.K. Relational aggression, gender, and social-psychological adjustment. Child Dev. 1995, 66, 710–722. [Google Scholar] [CrossRef] [PubMed]
- Raskauskas, J.; Stoltz, A.D. Involvement in traditional and electronic bullying among adolescents. Dev. Psychol. 2007, 43, 564–575. [Google Scholar] [CrossRef]
- Slonje, R.; Smith, P.K. Cyberbullying: Another main type of bullying? Scand. J. Psychol. 2008, 49, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.R.; Guerra, N.G. Prevalence and predictors of internet bullying. J. Adolesc. Health 2007, 41, S14–S21. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.; Bauman, S. Cyberbullying: Definition, consequences, prevalence. In Reducing Cyberbullying in Schools: International Evidence-Based Best Practices; Campbell, M.A., Bauman, S., Eds.; Elsevier: London, UK, 2018; pp. 3–16. [Google Scholar]
- Wright, M. Cyberbullying: Description, definition, characteristics, and outcomes. In Optimizing Human-Computer Interaction with Emerging Technologies; Wright, M., Ed.; IGI Global: Hershey, PA, USA, 2017; pp. 161–182. [Google Scholar] [CrossRef]
- Pornari, C.D.; Wood, J. Peer and cyber aggression in secondary school students: The role of moral disengagement, hos-tile attribution bias, and outcome expectancies. Aggress. Behav. 2010, 36, 81–94. [Google Scholar] [CrossRef]
- Runions, K.C.; Bak, M. Online moral disengagement, cyberbullying, and cyber-aggression. Cyberpsychol. Behav. Soc. Netw. 2015, 18, 400–405. [Google Scholar] [CrossRef]
- Cross, D.; Lester, L.; Barnes, A. A longitudinal study of the social and emotional predictors and consequences of cyber and traditional bullying victimization. Int. J. Public Health 2015, 60, 207–217. [Google Scholar] [CrossRef]
- Martínez-Monteagudo, M.C.; Delgado, B.; Inglés, C.J.; García-Fernández, J.M. Cyberbullying in the university setting. Relationship with emotional intelligence. Comput. Hum. Behav. 2019, 91, 220–225. [Google Scholar] [CrossRef]
- Jenaro, C.; Flores, N.; Frías, C. Anxiety and depression in cyberbullied college students: A retrospective study. J. Interpers. Violence 2017, 36, 1–24. [Google Scholar] [CrossRef]
- Schenk, A.M.; Fremouw, W.J. Prevalence, psychological impact, and coping of cyberbully victims among college students. J. Sch. Violence 2012, 11, 21–37. [Google Scholar] [CrossRef]
- Anderson, C.A.; Bushman, B.J. Media violence and the general aggression model. J. Soc. Issues 2018, 74, 386–413. [Google Scholar] [CrossRef]
- Baron, R.A.; Richardson, D.R. Human Aggression; Springer Science & Business Media: Berlin, Germany, 1994. [Google Scholar]
- Dewall, C.N.; Anderson, C.A.; Bushman, B.J. The general aggression model: Theoretical extensions to violence. Psychol. Violence 2011, 1, 245–258. [Google Scholar] [CrossRef] [Green Version]
- Dodge, K.A.; Coie, J.D. Social-information-processing factors in reactive and proactive aggression in children’s peer groups. J. Personal. Soc. Psychol. 1987, 53, 1146–1158. [Google Scholar] [CrossRef]
- Buss, D.M.; Shackelford, T.K. Human aggression in evolutionary psychological perspective. Clin. Psychol. Rev. 1997, 17, 605–619. [Google Scholar] [CrossRef]
- Shorey, R.C.; Meltzer, C.; Cornelius, T.L. Motivations for self-defensive aggression in dating relationships. Violence Vict. 2010, 25, 662–676. [Google Scholar] [CrossRef]
- Karos, K.; Meulders, A.; Goubert, L.; Vlaeyen, J.W.S. Hide your pain: Social threat increases pain reports and aggression, but reduces facial pain expression and empathy. J. Pain 2019, 21, 334–346. [Google Scholar] [CrossRef] [PubMed]
- Inzlicht, M.; Kang, S.K. Stereotype threat spillover: How coping with threats to social identity affects aggression, eating, decision making, and attention. J. Personal. Soc. Psychol. 2010, 99, 467–481. [Google Scholar] [CrossRef] [Green Version]
- Bar-Haim, Y.; Lamy, D.; Pergamin, L.; Bakermans-Kranenburg, M.J.; van Ijzendoorn, M.H. Threat-Related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychol. Bull. 2007, 133, 1–24. [Google Scholar] [CrossRef] [Green Version]
- Elsesser, K.; Sartory, G.; Tackenberg, A. Initial symptoms and reactions to trauma-related stimuli and the development of posttraumatic stress disorder. Depress. Anxiety 2005, 21, 61–70. [Google Scholar] [CrossRef]
- Buades-Rotger, M.; Krämer, U.M. From words to action: Implicit attention to antisocial semantic cues predicts aggression and amygdala reactivity to angry faces in healthy young women. Aggress. Behav. 2018, 44, 624–637. [Google Scholar] [CrossRef]
- Leary, M.R.; Schreindorfer, L.S. The stigmatization of HIV and AIDS: Rubbing salt in the wound. In HIV and Social Interaction; Sage Publications Inc.: Thousand Oaks, CA, USA, 1998; pp. 12–29. [Google Scholar]
- Goldin, C.S. Stigmatization and AIDS: Critical issues in public health. Soc. Sci. Med. 1994, 39, 1359–1366. [Google Scholar] [CrossRef]
- Herek, G.M.; Capitanio, J.P. Symbolic prejudice or fear of infection? A functional analysis of AIDS-related stigma among heterosexual adults. Basic Appl. Soc. Psychol. 1998, 20, 230–241. [Google Scholar] [CrossRef]
- Mak, W.W.; Mo, P.K.; Cheung, R.Y.; Woo, J.; Cheung, F.M.; Lee, D. Comparative stigma of HIV/AIDS, SARS, and tuberculosis in Hong Kong. Soc. Sci. Med. 2006, 63, 1912–1922. [Google Scholar] [CrossRef] [PubMed]
- Rogers, R.W.; Prentice-Dunn, S. Protection motivation theory. In Handbook of Health Behavior Research 1: Personal and Social Determinants; Gochman, D.S., Ed.; Plenum Press: New York, NY, USA, 1997. [Google Scholar]
- Folkman, S.; Lazarus, R.S. Stress, Appraisal and Coping; Springer: Berlin/Heidelberg, Germany, 1984. [Google Scholar]
- Kim, H.S.; Sherman, D.K.; Updegraff, J.A. Fear of Ebola: The influence of collectivism on xenophobic threat responses. Psychol. Sci. 2016, 27, 935–944. [Google Scholar] [CrossRef] [PubMed]
- Li, J.B.; Yang, A.; Dou, K.; Cheung, R.Y. Self-Control moderates the association between perceived severity of the coronavirus disease 2019 (COVID-19) and mental health problems among the Chinese public. Int. J. Environ. Res. Public Health 2020, 17, 4820. [Google Scholar] [CrossRef]
- Hussian, A.; Sharma, S. Anger expression and mental health of bully perpetrators. FWU J. Soc. Sci. 2014, 8, 17–23. [Google Scholar]
- Estévez, E.; Murgui, S.; Musitu, G. Psychosocial adjustment in aggressors, pure victims and aggressive victims at school. Eur. J. Educ. Psychol. 2008, 1, 29–39. [Google Scholar] [CrossRef]
- Nansel, T.R.; Overpeck, M.; Pilla, R.S.; Ruan, W.J.; Simons-Morton, B.; Scheidt, P. Bullying behaviors among US youth prevalence and association with psychosocial adjustment. JAMA 2001, 285, 2094–2100. [Google Scholar] [CrossRef]
- Ulloa, E.C.; Hammett, J.F. The effect of gender and perpetrator–victim role on mental health outcomes and risk behaviors associated with intimate partner violence. J. Interpers. Violence 2016, 31, 1184–1207. [Google Scholar] [CrossRef]
- Ybrandt, H.; Armelius, K. Peer aggression and mental health problems: Self-Esteem as a mediator. Sch. Psychol. Int. 2010, 31, 146–163. [Google Scholar] [CrossRef]
- Hinduja, S.; Patchin, J.W. Bullying, cyberbullying and suicide. Arch. Suicide Res. 2010, 14, 206–221. [Google Scholar] [CrossRef] [PubMed]
- Patchin, J.W.; Hinduja, S. Cyberbullying and self-esteem. J. Sch. Health 2010, 80, 614–621. [Google Scholar] [CrossRef]
- Schneider, S.K.; O’Donnell, L.; Stueve, A.; Coulter, R.W.S. Cyberbullying, school bullying and psychological distress: A regional census of high school students. Am. J. Public Health 2011, 102, 171–177. [Google Scholar] [CrossRef]
- Pemberton, M.B.; Insko, C.A.; Schopler, J. Memory for and experience of differential competitive behavior of individuals and groups. J. Personal. Soc. Psychol. 1996, 71, 953–966. [Google Scholar] [CrossRef]
- Sidanius, J.; Cling, B.J.; Pratto, F. Ranking and linking as a function of sex and gender role attitudes. J. Soc. Issues 1991, 47, 131–149. [Google Scholar] [CrossRef]
- Pratto, F.; Sidanius, J.; Stallworth, L.M.; Malle, B.F. Social dominance orientation: A personality variable predicting social and political attitudes. J. Personal. Soc. Psychol. 1994, 67, 741–763. [Google Scholar] [CrossRef]
- Sidanius, J.; Pratto, F. Social Dominance: An Intergroup Theory of Social Hierarchy and Oppression; Cambridge University Press: New York, NY, USA, 1999. [Google Scholar]
- Yuki, M.; Yokota, K. The primal warrior: Outgroup threat priming enhances intergroup discrimination in men but not women. J. Exp. Soc. Psychol. 2009, 45, 271–274. [Google Scholar] [CrossRef]
- Sugiura, H.; Mifune, N.; Tsuboi, S.; Yokota, K. Gender differences in intergroup conflict: The effect of outgroup threat priming on social dominance orientation. Personal. Individ. Differ. 2017, 104, 262–265. [Google Scholar] [CrossRef]
- Schaller, M.; Park, J.; Faulkner, J. Prehistoric dangers and contemporary prejudices. Eur. Rev. Soc. Psychol. 2003, 14, 105–137. [Google Scholar] [CrossRef] [Green Version]
- Eagly, A.H.; Steffen, V. Gender and aggressive behavior: A meta-analytic review of the social psychological literature. Psychol. Bull. 1986, 100, 309–330. [Google Scholar] [CrossRef] [PubMed]
- Bosson, J.K.; Vandello, J.A.; Burnaford, R.M.; Weaver, J.R.; Arzu Wasti, S. Precarious manhood and displays of physical aggression. Personal. Soc. Psychol. Bull. 2009, 35, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Costa, P.T.; McCrae, R.R. Neuroticism, somatic complaints, and disease: Is the bark worse than the bite? J. Personal. 1987, 55, 299–316. [Google Scholar] [CrossRef] [PubMed]
- Lucas, R.E.; Fujita, F. Factors influencing the relation between extraversion and pleasant affect. J. Personal. Soc. Psychol. 2000, 79, 1039–1056. [Google Scholar] [CrossRef]
- Clark, L.A.; Watons, D.; Mineka, S. Temperament, personality, and the mood and anxiety disorders. J. Abnorm. Psychol. 1994, 103, 103–116. [Google Scholar] [CrossRef]
- Ormel, J.; Oldehinkel, A.J.; Nolen, W.A.; Vollebergh, W. Vulnerability before, during, and after a major depressive episode. A 3-wave population-based study. Arch. Gen. Psychiatry 2004, 61, 387–392. [Google Scholar] [CrossRef]
- Van Os, J.; Jones, P.B. Neuroticism as a risk factor for schizophrenia. Psychol. Med. 2001, 31, 1129–1134. [Google Scholar] [CrossRef]
- Goodwin, R.D.; Fergusson, D.M.; Horwood, L.J. Neuroticism in adolescence and psychotic symptoms in adulthood. Psychol. Med. 2003, 33, 1089–1097. [Google Scholar] [CrossRef]
- Ormel, J.; Rosmalen, J.; Farmer, A. Neuroticism: A non-informative marker of vulnerability to psychopathology. Soc. Psychiatry Psychiatr. Epidemiol. 2004, 39, 906–912. [Google Scholar] [CrossRef]
- Buhrmester, M.D.; Blanton, H.; Swann, W.B., Jr. Implicit self-esteem: Nature, measurement, and a new way forward. J. Personal. Soc. Psychol. 2011, 100, 365–385. [Google Scholar] [CrossRef]
- Donnellan, M.B.; Oswald, F.L.; Baird, B.M.; Lucas, R.E. The Mini-IPIP Scales: Tiny-yet-effective measures of the Big Five Factors of personality. Psychol. Assess. 2006, 18, 192–203. [Google Scholar] [CrossRef]
- Adler, N.E.; Epel, E.S.; Castellazzo, G.; Ickovics, J.R. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, White women. Health Psychol. 2000, 19, 586–592. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Qian, M.; Wu, Q.; Wu, P.; Hou, Z.; Liang, Y.; Cowling, B.J.; Yu, H. Psychological responses, behavioral changes and public perceptions during the early phase of the COVID-19 outbreak in China: A population based cross-sectional survey. BMJ Open 2020, in press. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, Y.; Chen, L.; Ji, H.; Xi, M.; Fang, Y.; Li, Y. The risk and prevention of novel coronavirus pneumonia infections among inpatients in psychiatric hospitals. Neurosci. Bull. 2020, 36, 299–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, C.; Wong, W.-m.; Tsang, K.W. Perception of benefits and costs during SARS outbreak: An 18-month prospective study. J. Consult. Clin. Psychol. 2006, 74, 870–879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dorfan, N.M.; Woody, S.R. Danger appraisals as prospective predictors of disgust and avoidance of contaminants. J. Soc. Clin. Psychol. 2011, 30, 105–132. [Google Scholar] [CrossRef]
- Vartti, A.-M.; Oenema, A.; Schreck, M.; Uutela, A.; de Zwart, O.; Brug, J.; Aro, A.R. SARS knowledge, perceptions, and Behaviors: A comparison between Finns and the Dutch during the SARS Outbreak in 2003. Int. J. Behav. Med. 2009, 16, 41–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, J.Z.; Chu, H. Who is afraid of the Ebola outbreak? The influence of discrete emotions on risk perception. J. Risk Res. 2018, 21, 834–853. [Google Scholar] [CrossRef]
- Shi, J.; Chen, Z.; Wang, X.; Teng, F.; Yang, Y.; Chen, H. Dominate others, hurt self: Social dominance orientation predicts depression during the COVID-19 pandemic. Personal. Individ. Differ. 2021, 175, 110710. [Google Scholar] [CrossRef]
- Frenkel, S.; Alba, D.; Zhong, R. Surge of virus misinformation stumps Facebook and Twitter. The New York Times, 8 March 2020. Available online: https://www.nytimes.com/2020/03/08/technology/coronavirus-misinformation-social-media.html(accessed on 15 August 2021).
- Russonello, G. Afraid of Coronavirus? That Might Say Something about Your Politics. The New York Times, 13 March 2020. [Google Scholar]
- Pennycook, G.; McPhetres, J.; Zhang, Y.; Lu, J.G.; Rand, D.G. Fighting COVID19 misinformation on social media: Experimental evidence for a scalable accuracy nudge intervention. Psychol. Sci. 2020. [Google Scholar] [CrossRef] [PubMed]
- Pellecchia, U.; Crestani, R.; Decroo, T.; Bergh, R.; Al-Kourdi, Y. Social consequences of Ebola containment measures in Liberia. PLoS ONE 2015, 10, e0143036. [Google Scholar] [CrossRef] [Green Version]
- Person, B.; Sy, F.; Holton, K.; Govert, B.; Liang, A. Fear and stigma: The epidemic within the SARS outbreak. Emerg. Infect. Dis. 2004, 10, 358–363. [Google Scholar] [CrossRef]
- Kowalski, R.M.; Limber, S.P. Psychological, physical, and academic correlates of cyberbullying and traditional bullying. J. Adolesc. Health 2013, 53, S13–S20. [Google Scholar] [CrossRef] [Green Version]
- Law, D.M.; Shapka, J.D.; Domene, J.F.; Gagné, M.H. Are cyberbullies really bullies? An investigation of reactive and proactive online aggression. Comput. Hum. Behav. 2012, 28, 664–672. [Google Scholar] [CrossRef]
- Schultze-Krumbholz, A.; Scheithauer, H. Measuring Cyberbullying and Cybervictimisation by Using Behavioral Categories–The Berlin Cyberbullying-Cybervictimisation Questionnaire (BCCQ); Poster Presented at the Postconference Workshop of COST (Action IS0801): Vilnius, Lithuania, 2009 2009. [Google Scholar]
- Menesini, E.; Nocentini, A.; Calussi, P. The measurement of cyberbullying: Dimensional structure and relative item severity and discrimination. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 267–274. [Google Scholar] [CrossRef] [Green Version]
- Masten, A.S. Ordinary magic. Resilience processes in development. Am. Psychol. 2001, 56, 227–238. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-Y.; Yang, Y.; Zhang, X.-M.; Xu, X.; Dou, Q.-L.; Zhang, W.-W.; Cheng, A.S.K. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol. Infect. 2020, 148, e98. [Google Scholar] [CrossRef] [PubMed]


| Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | (n = 367) | (n = 337) | |||
| M | SD | M | SD | |||||||
| 1. Perceived infection | 0.52 *** | 0.34 *** | −0.16 *** | 0.38 *** | 0.20 *** | 4.45 | 1.22 | 4.53 | 1.07 | |
| 2. Neuroticism | −0.004 | 1 | 0.38 *** | −0.28 *** | 0.52 *** | 0.27 *** | 3.02 | 1.40 | 3.01 | 1.46 |
| 3. On-line aggression | 0.20 *** | 0.12 * | 1 | −0.25 *** | 0.14 ** | 0.02 | 2.96 | 1.89 | 2.18 | 1.58 |
| 4. Age | −0.03 | −0.27 *** | −0.12 * | 1 | −0.16 ** | −0.02 | 41.04 | 13.03 | 44.39 | 12.14 |
| 5. SES | 0.12 ** | −0.14 ** | 0.34 *** | −0.002 | 1 | 0.47 *** | 5.62 | 2.11 | 5.29 | 1.86 |
| 6. Education | −0.05 | 0.02 | 0.05 | −0.04 | 0.37 *** | 1 | 4.57 | 1.30 | 4.33 | 1.34 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | Male (n = 574) | Female (n = 1377) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||||||
| 1. Perceived infection | – | 0.33 *** | 0.18 *** | 0.15 *** | 0.23 *** | 0.07 | −0.12 ** | 4.75 | 1.39 | 5.12 | 1.25 |
| 2. Anxiety | 0.26 *** | – | 0.70 *** | 0.54 *** | 0.17 *** | 0.03 | −0.16 *** | 4.28 | 3.90 | 4.40 | 2.75 |
| 3. Depression | 0.16 *** | 0.63 *** | – | 0.59 *** | 0.08 * | −0.004 | −0.23 *** | 4.74 | 3.39 | 4.15 | 2.96 |
| 4. Depressive symptoms | 0.17 *** | 0.55 *** | 0.62 *** | – | 0.15 *** | 0.01 | −0.17 *** | 5.84 | 5.41 | 5.57 | 4.88 |
| 5. On-line aggression | 0.10 *** | 0.10 *** | 0.08 ** | 0.06 * | – | −0.02 | −0.06 | 2.83 | 1.33 | 2.63 | 1.20 |
| 6. Age | 0.01 | 0.04 | 0.04 | −0.03 | 0.004 | – | 0.09 * | 21.29 | 5.50 | 20.90 | 4.65 |
| 7. SES | −0.06 * | −0.07 ** | −0.1 *** | −0.09 ** | −0.03 | 0.10 *** | – | 4.59 | 1.77 | 4.64 | 1.56 |
| Gender | Anxiety | Depression | Depressive Disorder | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Effect | Boot SE | Boot LLCI | Boot ULCI | Effect | Boot SE | Boot LLCI | Boot ULCI | Effect | Boot SE | Boot LLCI | Boot ULCI | |
| Female | 0.02 | 0.01 | 0.01 | 0.04 | 0.02 | 0.01 | 0.004 | 0.04 | 0.03 | 0.02 | 0.01 | 0.07 |
| Male | 0.06 | 0.02 | 0.02 | 0.10 | 0.04 | 0.02 | 0.01 | 0.09 | 0.08 | 0.03 | 0.02 | 0.16 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teng, F.; Wang, X.; Shi, J.; Chen, Z.; Huang, Q.; Cheng, W. Psychosomatic Symptoms and Neuroticism following COVID-19: The Role of Online Aggression toward a Stigmatized Group. Int. J. Environ. Res. Public Health 2021, 18, 8672. https://doi.org/10.3390/ijerph18168672
Teng F, Wang X, Shi J, Chen Z, Huang Q, Cheng W. Psychosomatic Symptoms and Neuroticism following COVID-19: The Role of Online Aggression toward a Stigmatized Group. International Journal of Environmental Research and Public Health. 2021; 18(16):8672. https://doi.org/10.3390/ijerph18168672
Chicago/Turabian StyleTeng, Fei, Xijing Wang, Jiaxin Shi, Zhansheng Chen, Qianying Huang, and Wanrong Cheng. 2021. "Psychosomatic Symptoms and Neuroticism following COVID-19: The Role of Online Aggression toward a Stigmatized Group" International Journal of Environmental Research and Public Health 18, no. 16: 8672. https://doi.org/10.3390/ijerph18168672
APA StyleTeng, F., Wang, X., Shi, J., Chen, Z., Huang, Q., & Cheng, W. (2021). Psychosomatic Symptoms and Neuroticism following COVID-19: The Role of Online Aggression toward a Stigmatized Group. International Journal of Environmental Research and Public Health, 18(16), 8672. https://doi.org/10.3390/ijerph18168672






