Epidemiological Characteristics and Regional Risk Prediction of Hemorrhagic Fever with Renal Syndrome in Shandong Province, China
Abstract
:1. Introduction
2. Materials and Methods
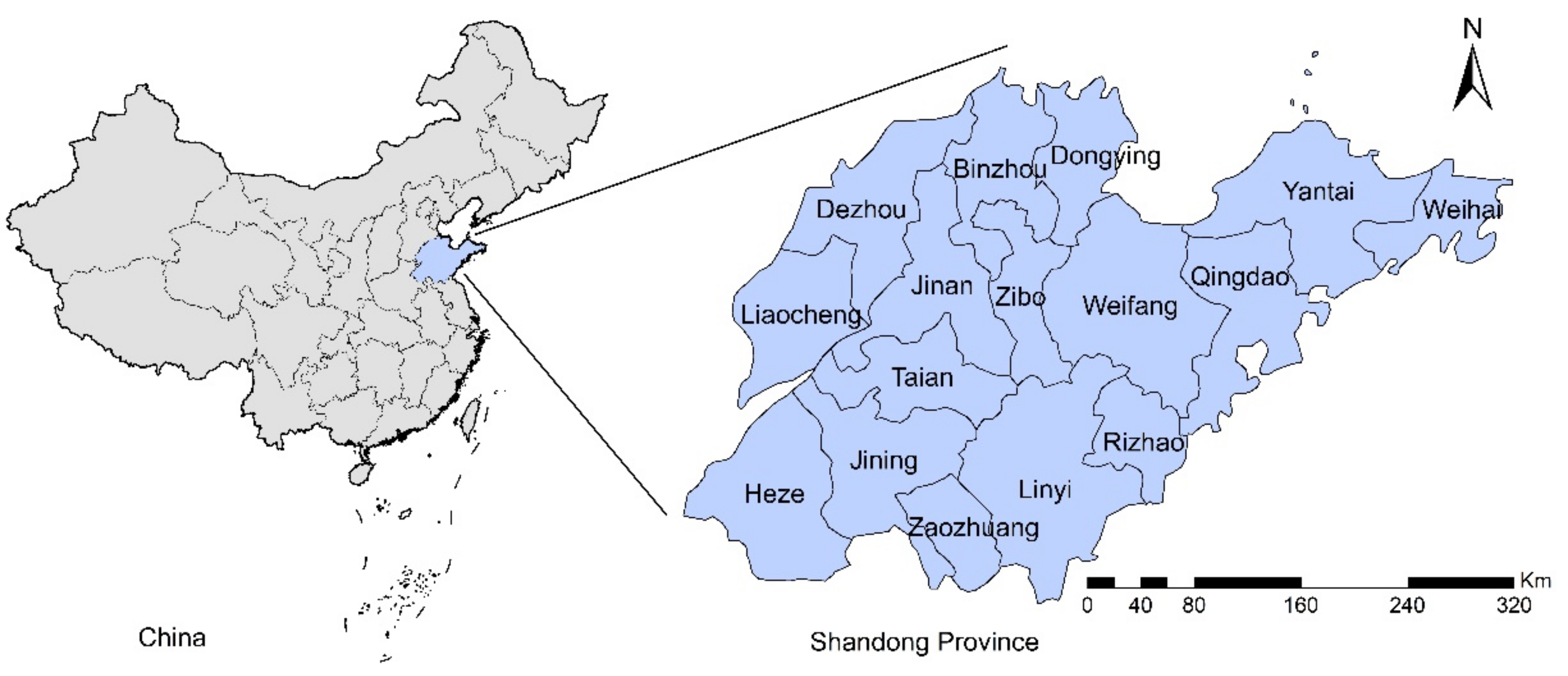
2.1. Study Area
2.2. Data Sources
2.3. Statistical Analysis
3. Results
3.1. Epidemiological Characteristics of HFRS
3.2. Influencing Factors for the Epidemic of HFRS
3.3. Map of HFRS Risk Zones
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Avšič-Županc, T.; Saksida, A.; Korva, M. Hantavirus infections. Clin. Microbiol. Infect. 2019, 21, e6–e16. [Google Scholar] [CrossRef] [Green Version]
- Jiang, H.; Du, H.; Wang, L.M.; Wang, P.Z.; Bai, X.F. Hemorrhagic Fever with Renal Syndrome: Pathogenesis and Clinical Picture. Front. Cell. Infect. Microbiol. 2016, 6, 1. [Google Scholar] [CrossRef] [Green Version]
- Brocato, R.L.; Hooper, J.W. Progress on the Prevention and Treatment of Hantavirus Disease. Viruses 2019, 11, 610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaheri, A.; Henttonen, H.; Voutilainen, L.; Mustonen, J.; Sironen, T.; Vapalahti, O. Hantavirus infections in Europe and their impact on public health. Rev. Med. Virol. 2013, 23, 35–49. [Google Scholar] [CrossRef]
- Connolly-Andersen, A.-M.; Hammargren, E.; Whitaker, H.; Eliasson, M.; Holmgren, L.; Klingström, J.; Ahlm, C. Increased Risk of Acute Myocardial Infarction and Stroke During Hemorrhagic Fever with Renal Syndrome. Circulation 2014, 129, 1295–1302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Connolly-Andersen, A.-M.; Whitaker, H.; Klingstrom, J.; Ahlm, C. Risk of Venous Thromboembolism Following Hemorrhagic Fever with Renal Syndrome: A Self-controlled Case Series Study. Clin. Infect. Dis. 2017, 66, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Klingström, J.; Granath, F.; Ekbom, A.; Björkström, N.K.; Ljunggren, H.-G. Increased Risk for Lymphoma Following Hemorrhagic Fever with Renal Syndrome. Clin. Infect. Dis. 2014, 59, 1130–1132. [Google Scholar] [CrossRef] [Green Version]
- Savira, F.; Magaye, R.; Liew, D.; Reid, C.; Kelly, D.J.; Kompa, A.R.; Sangaralingham, S.J.; Burnett, J.C.; Kaye, D.; Wang, B.H. Cardiorenal syndrome: Multi-organ dysfunction involving the heart, kidney and vasculature. Br. J. Pharmacol. 2020, 177, 2906–2922. [Google Scholar] [CrossRef]
- Kingma, J.G.; Simard, D.; Rouleau, J.R.; Drolet, B.; Simard, C. The Physiopathology of Cardiorenal Syndrome: A Review of the Potential Contributions of Inflammation. J. Cardiovasc. Dev. Dis. 2017, 4, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jonsson, C.B.; Figueiredo, L.T.M.; Vapalahti, O. A Global Perspective on Hantavirus Ecology, Epidemiology, and Disease. Clin. Microbiol. Rev. 2010, 23, 412–441. [Google Scholar] [CrossRef] [Green Version]
- Zou, L.-X.; Sun, L. Analysis of Hemorrhagic Fever with Renal Syndrome Using Wavelet Tools in Mainland China, 2004–2019. Front. Public Health 2020, 8, 571984. [Google Scholar] [CrossRef]
- Wang, Q.; Yue, M.; Yao, P.; Zhu, C.; Ai, L.; Hu, D.; Zhang, B.; Yang, Z.; Yang, X.; Luo, F.; et al. Epidemic Trend and Molecular Evolution of HV Family in the Main Hantavirus Epidemic Areas From 2004 to 2016, in P.R. China. Front. Cell. Infect. Microbiol. 2021, 10, 584814. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, S.; Yin, W.; Liang, M.; Li, J.; Zhang, Q.; Feng, Z.; Li, D. Epidemic characteristics of hemorrhagic fever with renal syndrome in China, 2006–2012. BMC Infect. Dis. 2014, 14, 384. [Google Scholar] [CrossRef] [Green Version]
- Tian, H.; Yu, P.; Bjørnstad, O.N.; Cazelles, B.; Yang, J.; Tan, H.; Huang, S.; Cui, Y.; Dong, L.; Ma, C.; et al. Anthropogenically driven environmental changes shift the ecological dynamics of hemorrhagic fever with renal syndrome. PLoS Pathog. 2017, 13, e1006198. [Google Scholar] [CrossRef]
- Yi, L.; Xu, X.; Ge, W.; Xue, H.; Li, J.; Li, D.; Wang, C.; Wu, H.; Liu, X.; Zheng, D.; et al. The impact of climate variability on infectious disease transmission in China: Current knowledge and further directions. Environ. Res. 2019, 173, 255–261. [Google Scholar] [CrossRef]
- Sun, W.; Liu, X.; Li, W.; Mao, Z.; Sun, J.; Lu, L. Effects and interaction of meteorological factors on hemorrhagic fever with renal syndrome incidence in Huludao City, northeastern China, 2007–2018. PLoS Negl. Trop. Dis. 2021, 15, e0009217. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Fang, L.-Q.; Huang, H.-G.; Zhang, L.-Q.; Feng, D.; Zhao, W.-J.; Zhang, W.-Y.; Li, X.-W.; Cao, W.-C. Landscape Elements and Hantaan Virus–related Hemorrhagic Fever with Renal Syndrome, People’s Republic of China. Emerg. Infect. Dis. 2007, 13, 1301–1306. [Google Scholar] [CrossRef]
- Li, S.; Ren, H.; Hu, W.; Lu, L.; Xu, X.; Zhuang, D.; Liu, Q. Spatiotemporal Heterogeneity Analysis of Hemorrhagic Fever with Renal Syndrome in China Using Geographically Weighted Regression Models. Int. J. Environ. Res. Public Health 2014, 11, 12129–12147. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Tong, X.; Gao, L.; Hu, S.; Tan, H.; Huang, Z.Y.X.; Zhang, G.; Yang, Q.; Li, X.; Huang, R.; et al. Spatial heterogeneity of hemorrhagic fever with renal syndrome is driven by environmental factors and rodent community composition. PLoS Negl. Trop. Dis. 2018, 12, e0006881. [Google Scholar] [CrossRef] [PubMed]
- Tian, H.; Hu, S.; Cazelles, B.; Chowell, G.; Gao, L.; Laine, M.; Li, Y.; Yang, H.; Li, Y.; Yang, Q.; et al. Urbanization prolongs hantavirus epidemics in cities. Proc. Natl. Acad. Sci. USA 2018, 115, 4707–4712. [Google Scholar] [CrossRef] [Green Version]
- Elith, J.; Leathwick, J.R.; Hastie, T. A working guide to boosted regression trees. J. Anim. Ecol. 2008, 77, 802–813. [Google Scholar] [CrossRef]
- Main, A.R.; Michel, N.L.; Headley, J.V.; Peru, K.M.; Morrissey, C. Ecological and Landscape Drivers of Neonicotinoid Insecticide Detections and Concentrations in Canada’s Prairie Wetlands. Environ. Sci. Technol. 2015, 49, 8367–8376. [Google Scholar] [CrossRef] [PubMed]
- Messina, J.P.; Kraemer, M.U.; Brady, O.J.; Pigott, D.M.; Shearer, F.M.; Weiss, D.J.; Golding, N.; Ruktanonchai, C.; Gething, P.; Cohn, E.; et al. Mapping global environmental suitability for Zika virus. eLife 2016, 5, e15272. [Google Scholar] [CrossRef]
- Shearer, F.M.; Longbottom, J.; Browne, A.J.; Pigott, D.M.; Brady, O.J.; Kraemer, M.U.G.; Marinho, F.; Yactayo, S.; de Araújo, V.E.M.; da Nóbrega, A.A.; et al. Existing and potential infection risk zones of yellow fever worldwide: A modelling analysis. Lancet Glob. Health 2018, 6, e270–e278. [Google Scholar] [CrossRef] [Green Version]
- Zhang, D.; Guo, Y.; Rutherford, S.; Qi, C.; Wang, X.; Wang, P.; Zheng, Z.; Xu, Q.; Li, X. The relationship between meteorological factors and mumps based on Boosted regression tree model. Sci. Total Environ. 2019, 695, 133758. [Google Scholar] [CrossRef] [PubMed]
- De’Ath, G. Boosted trees for ecological modeling and prediction. Ecology 2007, 88, 243–251. [Google Scholar] [CrossRef]
- Miao, D.; Liu, M.-J.; Wang, Y.-X.; Ren, X.; Lu, Q.-B.; Zhao, G.-P.; Dai, K.; Li, X.-L.; Li, H.; Zhang, X.-A.; et al. Epidemiology and Ecology of Severe Fever with Thrombocytopenia Syndrome in China, 2010‒2018. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Hijmans, R.J.; Phillips, S.; Leathwick, J.; Elith, J. Package ‘dismo’. Circles 2015, 9, 1–68. [Google Scholar]
- Ridgeway, G. Generalized Boosted Models: A Guide to the GBM Package. Compute 2005, 1, 1–12. [Google Scholar]
- Bi, P.; Tong, S.; Donald, K.; Parton, K.; Ni, J. Climatic, reservoir and occupational variables and the transmission of haemorrhagic fever with renal syndrome in China. Int. J. Epidemiol. 2002, 31, 189–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Cazelles, B.; Yang, G.; Laine, M.; Huang, Z.X.Y.; Cai, J.; Tan, H.; Stenseth, N.C.; Tian, H. Intrinsic and extrinsic drivers of transmission dynamics of hemorrhagic fever with renal syndrome caused by Seoul hantavirus. PLoS Negl. Trop. Dis. 2019, 13, e0007757. [Google Scholar] [CrossRef] [Green Version]
- Zheng, Z.; Wang, P.; Wang, Z.; Zhang, D.; Wang, X.; Zuo, S.; Li, X. The characteristics of current natural foci of hemorrhagic fever with renal syndrome in Shandong Province, China, 2012–2015. PLoS Negl. Trop. Dis. 2019, 13, e0007148. [Google Scholar] [CrossRef] [Green Version]
- Liang, W.; Gu, X.; Li, X.; Zhang, K.; Wu, K.; Pang, M.; Dong, J.; Merrill, H.R.; Hu, T.; Liu, K.; et al. Mapping the epidemic changes and risks of hemorrhagic fever with renal syndrome in Shaanxi Province, China, 2005–2016. Sci. Rep. 2018, 8, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Xiao, H.; Tian, H.-Y.; Gao, L.-D.; Liu, H.-N.; Duan, L.-S.; Basta, N.; Cazelles, B.; Li, X.-J.; Lin, X.-L.; Wu, H.-W.; et al. Animal Reservoir, Natural and Socioeconomic Variations and the Transmission of Hemorrhagic Fever with Renal Syndrome in Chenzhou, China, 2006–2010. PLoS Negl. Trop. Dis. 2014, 8, e2615. [Google Scholar] [CrossRef] [Green Version]
- Lin, H.; Liu, Q.; Guo, J.; Zhang, J.; Wang, J.; Chen, H. Analysis of the geographic distribution of HFRS in Liaoning Province between 2000 and 2005. BMC Public Health 2007, 7, 207. [Google Scholar] [CrossRef] [Green Version]
- Hardestam, J.; Simon, M.; Hedlund, K.O.; Vaheri, A.; Klingström, J.; Lundkvist, A. Ex Vivo Stability of the Rodent-Borne Hantaan Virus in Comparison to That of Arthropod-Borne Members of the Bunyaviridae Family. Appl. Environ. Microbiol. 2007, 73, 2547–2551. [Google Scholar] [CrossRef] [Green Version]
- He, J.; Christakos, G.; Wu, J.; Cazelles, B.; Qian, Q.; Mu, D.; Wang, Y.; Yin, W.; Zhang, W. Spatiotemporal variation of the association between climate dynamics and HFRS outbreaks in Eastern China during 2005–2016 and its geographic determinants. PLoS Negl. Trop. Dis. 2018, 12, e0006554. [Google Scholar] [CrossRef]
- Xiao, H.; Tong, X.; Huang, R.; Gao, L.; Hu, S.; Lidong, G.; Gao, H.; Zheng, P.; Yang, H.; Huang, Z.Y.X.; et al. Landscape and rodent community composition are associated with risk of hemorrhagic fever with renal syndrome in two cities in China, 2006–2013. BMC Infect. Dis. 2018, 18, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bao, C.; Liu, W.; Zhu, Y.; Liu, W.; Hu, J.; Liang, Q.; Cheng, Y.; Wu, Y.; Yu, R.; Zhou, M.; et al. The Spatial Analysis on Hemorrhagic Fever with Renal Syndrome in Jiangsu Province, China Based on Geographic Information System. PLoS ONE 2014, 9, e83848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bi, P.; Wu, X.; Zhang, F.; Parton, K.A.; Tong, S. Seasonal Rainfall Variability, the Incidence of Hemorrhagic Fever with Renal Syndrome, and Prediction of the Disease in Low-lying Areas of China. Am. J. Epidemiol. 1998, 148, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Liu, Z.; Tong, M.; Xiang, J.; Zhang, Y.; Gao, Q.; Zhang, Y.; Lu, L.; Jiang, B.; Bi, P. Real-time forecasting and early warning of bacillary dysentery activity in four meteorological and geographic divisions in China. Sci. Total Environ. 2021, 761, 144093. [Google Scholar] [CrossRef] [PubMed]




| Characteristic | Number of Cases | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 8267 | 72.31 |
| Female | 3165 | 27.69 |
| Age (year) | ||
| ≤10 | 62 | 0.54 |
| 11–20 | 352 | 3.08 |
| 21–30 | 974 | 8.52 |
| 31–40 | 1579 | 13.81 |
| 41–50 | 3048 | 26.66 |
| 51–60 | 2846 | 24.90 |
| 61–70 | 1791 | 15.67 |
| 71–80 | 631 | 5.52 |
| >80 | 149 | 1.30 |
| Occupation | ||
| Farmers | 9653 | 84.44 |
| Workers | 598 | 5.23 |
| Students | 275 | 2.41 |
| Housework and unemployment | 222 | 1.94 |
| Retirees | 171 | 1.50 |
| Others | 513 | 4.49 |
| Predictors | Relative Contributions (%) | |
|---|---|---|
| Mean | Range | |
| Population density | 15.90 | (15.19, 16.50) |
| Elevation | 12.02 | (11.50, 13.28) |
| Percentage coverage of grassland | 11.06 | (9.99, 11.84) |
| Percentage coverage of cultivated land | 9.98 | (9.50, 10.61) |
| Percentage coverage of rural settlement | 9.25 | (7.86, 11.67) |
| Percentage coverage of woodland | 8.71 | (7.61, 9.54) |
| Percentage coverage of water body | 8.63 | (7.35, 11.04) |
| Annual average temperature | 6.20 | (4.56, 7.97) |
| Annual cumulative precipitation | 5.42 | (4.98, 6.13) |
| GDP | 4.95 | (4.18, 6.05) |
| NDVI | 4.57 | (3.84, 5.79) |
| Percentage coverage of urban land | 3.31 | (2.99, 3.63) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
She, K.; Li, C.; Qi, C.; Liu, T.; Jia, Y.; Zhu, Y.; Liu, L.; Wang, Z.; Zhang, Y.; Li, X. Epidemiological Characteristics and Regional Risk Prediction of Hemorrhagic Fever with Renal Syndrome in Shandong Province, China. Int. J. Environ. Res. Public Health 2021, 18, 8495. https://doi.org/10.3390/ijerph18168495
She K, Li C, Qi C, Liu T, Jia Y, Zhu Y, Liu L, Wang Z, Zhang Y, Li X. Epidemiological Characteristics and Regional Risk Prediction of Hemorrhagic Fever with Renal Syndrome in Shandong Province, China. International Journal of Environmental Research and Public Health. 2021; 18(16):8495. https://doi.org/10.3390/ijerph18168495
Chicago/Turabian StyleShe, Kaili, Chunyu Li, Chang Qi, Tingxuan Liu, Yan Jia, Yuchen Zhu, Lili Liu, Zhiqiang Wang, Ying Zhang, and Xiujun Li. 2021. "Epidemiological Characteristics and Regional Risk Prediction of Hemorrhagic Fever with Renal Syndrome in Shandong Province, China" International Journal of Environmental Research and Public Health 18, no. 16: 8495. https://doi.org/10.3390/ijerph18168495
APA StyleShe, K., Li, C., Qi, C., Liu, T., Jia, Y., Zhu, Y., Liu, L., Wang, Z., Zhang, Y., & Li, X. (2021). Epidemiological Characteristics and Regional Risk Prediction of Hemorrhagic Fever with Renal Syndrome in Shandong Province, China. International Journal of Environmental Research and Public Health, 18(16), 8495. https://doi.org/10.3390/ijerph18168495






