Environmental Health-Related Policies and Practices of Oklahoma Licensed Early Care and Education Programs: Implications for Childhood Asthma
Abstract
1. Introduction
2. Materials and Methods
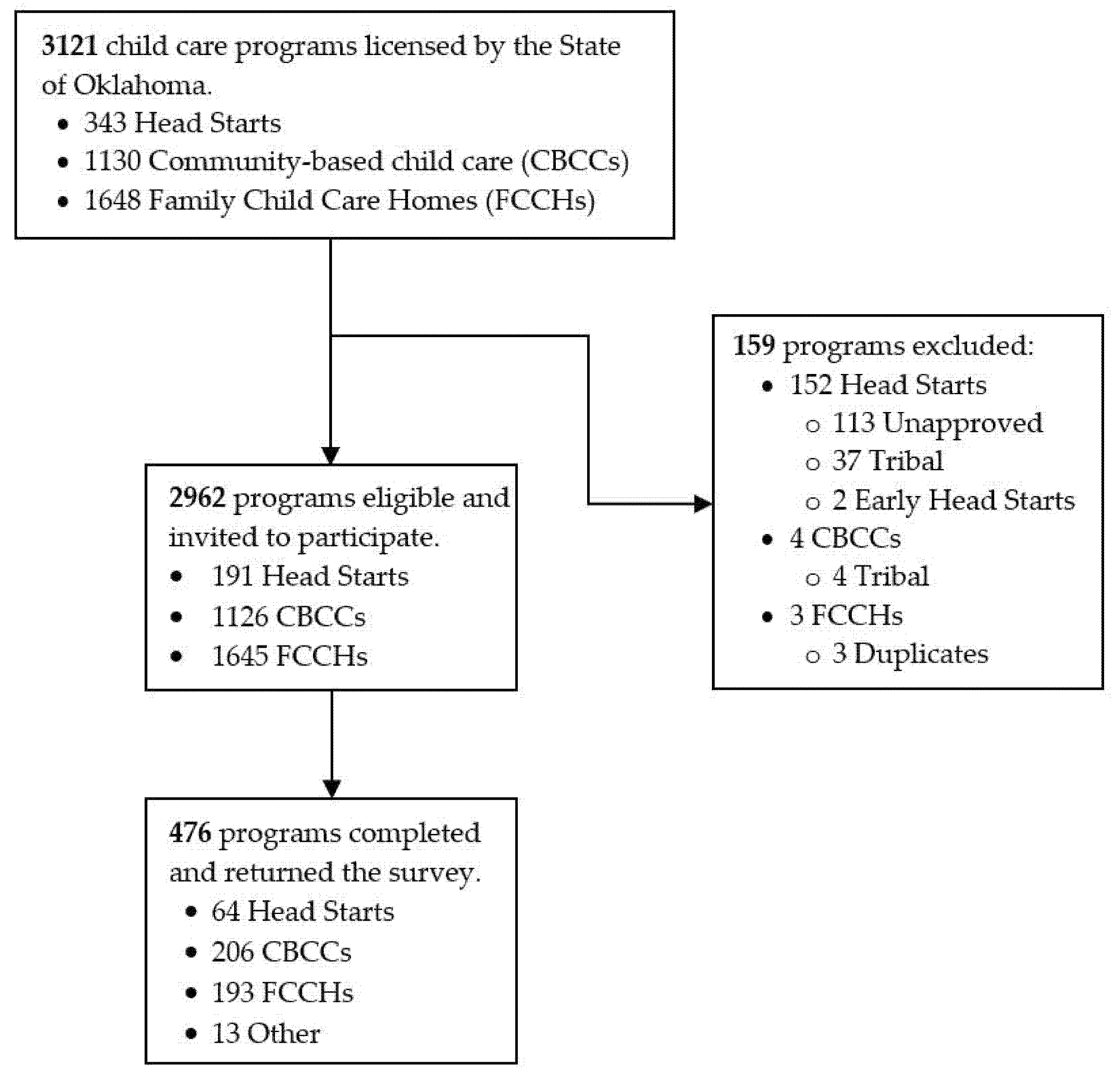
2.1. Study Design
2.2. Data Collection
2.3. Measures
2.3.1. Program Characteristics
2.3.2. Asthma-Related Training, Policies, and Practices
2.3.3. Bleach and Air Fresheners
2.3.4. Pesticide Use and Pest Control
2.4. Data Analyses
3. Results
3.1. Program Characteristics
3.2. Asthma-Related Training, Policies and Practices
3.3. Bleach and Air Fresheners
3.4. Pesticide Use and Pest Control
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Laughlin, L. Who’s Minding the Kids? Child Care Arrangements: Spring 2011; U.S. Census Bureau: Washington, DC, USA, 2013; pp. 70–135. [Google Scholar]
- Committee on Early Childhood, Adoption, and Dependent Care. Quality Early Education and Child Care From Birth to Kindergarten. Pediatrics 2017, 140, 187–191. [Google Scholar] [CrossRef]
- Hoang, T.; Castorina, R.; Gaspar, F.; Maddalena, R.; Jenkins, P.L.; Zhang, Q.; McKone, T.E.; Benfenati, E.; Shi, A.Y.; Bradman, A. VOC exposures in California early childhood education environments. Indoor Air 2017, 27, 609–621. [Google Scholar] [CrossRef]
- Bradman, A.; Gaspar, F.; Castorina, R.; Tong-Lin, E.; Mckone, T. Environmental Exposures in Early Childhood Education Environments. Available online: https://ww2.arb.ca.gov/sites/default/files/classic//research/apr/past/08-305.pdf (accessed on 15 November 2020).
- Bradman, A.; Castorina, R.; Gaspar, F.; Nishioka, M.; Colon, M.; Weathers, W.; Egeghy, P.P.; Maddalena, R.; Williams, J.; Jenkins, P.L.; et al. Flame retardant exposures in California early childhood education environments. Chemosphere 2014, 116, 61–66. [Google Scholar] [CrossRef]
- Breysse, P.; Farr, N.; Galke, W.; Lanphear, B.; Morley, R.; Bergofsky, L. The relationship between housing and health: Children at risk. Environ. Health Perspect. 2004, 112, 1583–1588. [Google Scholar] [CrossRef]
- Gaspar, F.W.; Castorina, R.; Maddalena, R.L.; Nishioka, M.G.; McKone, T.E.; Bradman, A. Phthalate exposure and risk assessment in California child care facilities. Environ. Sci. Technol. 2014, 48, 7593–7601. [Google Scholar] [CrossRef]
- Quiros-Alcala, L.; Wilson, S.; Witherspoon, N.; Murray, R.; Perodin, J.; Trousdale, K.; Raspanti, G.; Sapkota, A. Volatile organic compounds and particulate matter in child care facilities in the District of Columbia: Results from a pilot study. Environ. Res. 2016, 146, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Tulve, N.S.; Jones, P.A.; Nishioka, M.G.; Fortmann, R.C.; Croghan, C.W.; Zhou, J.Y.; Fraser, A.; Cavel, C.; Friedman, W. Pesticide measurements from the first national environmental health survey of child care centers using a multi-residue GC/MS analysis method. Environ. Sci. Technol. 2006, 40, 6269–6274. [Google Scholar] [CrossRef]
- Nazaroff, W.W.; Weschler, C.J. Cleaning products and air fresheners: Exposure to primary and secondary air pollutants. Atmos. Environ. 2004, 38, 2841–2856. [Google Scholar] [CrossRef]
- Neal, R.; Spurlock, F.; Segawa, R. Annual Report on Volatile Organic Compound Emissions from Pesticides: Emissions for 1990–2010. Available online: https://www.cdpr.ca.gov/docs/emon/vocs/vocproj/2017_voc_annual_report.pdf (accessed on 1 August 2021).
- Anderson, J.O.; Thundiyil, J.G.; Stolbach, A. Clearing the air: A review of the effects of particulate matter air pollution on human health. J. Med. Toxicol. 2012, 8, 166–175. [Google Scholar] [CrossRef]
- Kim, K.-H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, H.; Schuepp, K. The occurrence of ultrafine particles in the specific environment of children. Paediatr. Respir. Rev. 2012, 13, 89–94. [Google Scholar] [CrossRef]
- Salvi, S. Health effects of ambient air pollution in children. Paediatr. Respir. Rev. 2007, 8, 275–280. [Google Scholar] [CrossRef] [PubMed]
- ATDSR. Toxicological Profile for Carbon Tetrachloride. Available online: https://www.atsdr.cdc.gov/toxprofiles/tp30.pdf (accessed on 12 January 2021).
- United States Environmental Protection Agency. Exposure Factors Handbook 2011 Edition (Final). Available online: https://www.nrc.gov/docs/ML1400/ML14007A666.pdf (accessed on 20 January 2021).
- Goldizen, F.C.; Sly, P.D.; Knibbs, L.D. Respiratory effects of air pollution on children. Pediatr. Pulmonol. 2016, 51, 94–108. [Google Scholar] [CrossRef] [PubMed]
- Harving, H.; Dahl, R.; Mølhave, L. Lung Function and Bronchial Reactivity in Asthmatics during Exposure to Volatile Organic Compounds. Am. Rev. Respir. Dis. 1991, 143, 751–754. [Google Scholar] [CrossRef] [PubMed]
- Koren, H.S.; Graham, D.E.; Devlin, R.B. Exposure of Humans to a Volatile Organic Mixture. III. Inflammatory Response. Arch. Environ. Health Int. J. 1992, 47, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Mortimer, K.; Neugebauer, R.; Lurmann, F.; Alcorn, S.; Balmes, J.; Tager, I. Air pollution and pulmonary function in asthmatic children: Effects of prenatal and lifetime exposures. Epidemiology 2008, 19, 550–557. [Google Scholar] [CrossRef]
- Norbäck, D.; Björnsson, E.; Janson, C.; Widström, J.; Boman, G. Asthmatic symptoms and volatile organic compounds, formaldehyde, and carbon dioxide in dwellings. Occup. Environ. Med. 1995, 52, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Hollenbach, J.P.; Cloutier, M.M. Childhood Asthma Management and Environmental Triggers. Pediatr. Clin. N. Am. 2015, 62, 1199–1214. [Google Scholar] [CrossRef]
- Jia, C.; Batterman, S.; Godwin, C. VOCs in industrial, urban and suburban neighborhoods—Part 2: Factors affecting indoor and outdoor concentrations. Atmos. Environ. 2008, 42, 2101–2116. [Google Scholar] [CrossRef]
- Wieslander, G.; Norbäck, D.; Björnsson, E.; Janson, C.; Boman, G. Asthma and the indoor environment: The significance of emission of formaldehyde and volatile organic compounds from newly painted indoor surfaces. Int. Arch. Occup. Environ. Health 1997, 69, 115–124. [Google Scholar] [CrossRef]
- Cox, S.S.; Little, J.C.; Hodgson, A.T. Predicting the Emission Rate of Volatile Organic Compounds from Vinyl Flooring. Environ. Sci. Technol. 2002, 36, 709–714. [Google Scholar] [CrossRef]
- Wilke, O.; Jann, O.; Brödner, D. VOC- and SVOC-emissions from adhesives, floor coverings and complete floor structures. Indoor Air 2004, 14 (Suppl. 8), 98–107. [Google Scholar] [CrossRef]
- Jo, W.-J.; Sohn, J.-Y. The effect of environmental and structural factors on indoor air quality of apartments in Korea. Build. Environ. 2009, 44, 1794–1802. [Google Scholar] [CrossRef]
- Singer, B.C.; Destaillats, H.; Hodgson, A.T.; Nazaroff, W.W. Cleaning products and air fresheners: Emissions and resulting concentrations of glycol ethers and terpenoids. Indoor Air 2006, 16, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Parks, J.; McCandless, L.; Dharma, C.; Brook, J.; Turvey, S.E.; Mandhane, P.; Becker, A.B.; Kozyrskyj, A.L.; Azad, M.B.; Moraes, T.J. Association of use of cleaning products with respiratory health in a Canadian birth cohort. CMAJ 2020, 192, E154–E161. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.M.; Callahan, P.J.; Nishioka, M.G.; Brinkman, M.C.; O’Rourke, M.K.; Lebowitz, M.D.; Moschandreas, D.J. Residential environmental measurements in the National Human Exposure Assessment Survey (NHEXAS) pilot study in Arizona: Preliminary results for pesticides and VOCs. J. Expo. Sci. Environ. Epidemiol. 1999, 9, 456–470. [Google Scholar] [CrossRef]
- Ott, W.R.; Roberts, J.W. Everyday exposure to toxic pollutants. Sci. Am. 1998, 278, 86–91. [Google Scholar] [CrossRef]
- Chin, J.Y.; Godwin, C.; Parker, E.; Robins, T.; Lewis, T.; Harbin, P.; Batterman, S. Levels and sources of volatile organic compounds in homes of children with asthma. Indoor Air 2014, 24, 403–415. [Google Scholar] [CrossRef]
- Beamer, P.; Castano, A.; Leckie, J. Vertical Profile Particulate Matter Measurements in a California Daycare. Available online: https://www.irbnet.de/daten/iconda/CIB6560.pdf (accessed on 30 July 2021).
- Gruchalla, R.S.; Pongracic, J.; Plaut, M.; Evans, R., III; Visness, C.M.; Walter, M.; Crain, E.F.; Kattan, M.; Morgan, W.J.; Steinbach, S.; et al. Inner City Asthma Study: Relationships among sensitivity, allergen exposure, and asthma morbidity. J. Allergy Clin. Immunol. 2005, 115, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Torjusen, E.N.; Diette, G.B.; Breysse, P.N.; Curtin-Brosnan, J.; Aloe, C.; Matsui, E.C. Dose–response relationships between mouse allergen exposure and asthma morbidity among urban children and adolescents. Indoor Air 2013, 23, 268–274. [Google Scholar] [CrossRef]
- Sheehan, W.J.; Rangsithienchai, P.A.; Wood, R.A.; Rivard, D.; Chinratanapisit, S.; Perzanowski, M.S.; Chew, G.L.; Seltzer, J.M.; Matsui, E.C.; Phipatanakul, W. Pest and allergen exposure and abatement in inner-city asthma: A work group report of the American Academy of Allergy, Asthma & Immunology Indoor Allergy/Air Pollution Committee. J. Allergy Clin. Immunol. 2010, 125, 575–581. [Google Scholar] [CrossRef]
- Morgan, W.J.; Crain, E.F.; Gruchalla, R.S.; O’Connor, G.T.; Kattan, M.; Evans, R.; Stout, J.; Malindzak, G.; Smartt, E.; Plaut, M.; et al. Results of a Home-Based Environmental Intervention among Urban Children with Asthma. N. Eng. J. Med. 2004, 351, 1068–1080. [Google Scholar] [CrossRef]
- Arbes, S.J.; Sever, M.; Mehta, J.; Collette, N.; Thomas, B.; Zeldin, D.C. Exposure to indoor allergens in day-care facilities: Results from 2 North Carolina counties. J. Allergy Clin. Immunol. 2005, 116, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Perry, T.T.; Vargas, P.A.; Bufford, J.; Feild, C.; Flick, M.; Simpson, P.M.; Hamilton, R.G.; Jones, S.M. Classroom aeroallergen exposure in Arkansas head start centers. Ann. Allergy Asthma Immunol. 2008, 100, 358–363. [Google Scholar] [CrossRef]
- Phipatanakul, W.; Cronin, B.; Wood, R.A.; Eggleston, P.A.; Shih, M.C.; Song, L.; Tachdjian, R.; Oettgen, H.C. Effect of environmental intervention on mouse allergen levels in homes of inner-city Boston children with asthma. Ann. Allergy Asthma Immunol. 2004, 92, 420–425. [Google Scholar] [CrossRef]
- Chaudhuri, N. Interventions to improve children’s health by improving the housing environment. Rev. Environ. Health 2004, 19, 197–222. [Google Scholar] [CrossRef] [PubMed]
- Katial, R.K. Cockroach allergy. Immunol. Allergy Clin. N. Am. 2003, 23, 483–499. [Google Scholar] [CrossRef]
- Eggleston, P.A. Methods and effectiveness of indoor environmental control. Ann. Allergy Asthma Immunol. 2001, 87, 44–47. [Google Scholar] [CrossRef]
- Fournier, A.; Johnson, T. Implementation of Pilot Integrated pest Management Programs in Indiana Schools and Child Care Facilities, Executive Summary; IPM School Technical Resource Center: West Lafayette, IN, USA, 2003. [Google Scholar]
- Piper, C.; Owens, K. Are schools making the grade? School districts nationwide adopt safer pest management policies. Pestic. You 2002, 22, 11–20. [Google Scholar]
- Anderson, M.; Glynn, T.; Enache, A. EPA Region 2 Pesticides in Child Care Initiative 2010 Staten Island Pilot Project Final Report. Available online: https://www.epa.gov/sites/production/files/documents/StatenPilot2010.pdf (accessed on 12 November 2020).
- Amoah, A.O.; Witherspoon, N.O.; Pérodin, J.; Paulson, J.A. Findings from a pilot environmental health intervention at early childhood centers in the District of Columbia. J. Public Health 2016, 38, e209–e217. [Google Scholar] [CrossRef][Green Version]
- Gilden, R.; McElroy, K.; Friedmann, E.; Witherspoon, N.O.; Paul, H. Evaluation of the children’s environmental health network’s environmental stewardship checklist responses. J. Environ. Health 2015, 77, 22–29. [Google Scholar] [PubMed]
- Young, C.A.; Stookey, J.; Patel, A.I.; Chan, C.; Evans, J.; Cohn, K.; Agana, L.; Yen, I.H.; Fernandez, A.; Cabana, M.D. San Francisco childcare centers’ preparedness in the prevention and management of asthma among preschool-aged children. J. Asthma 2016, 53, 691–698. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alkon, A.; Nouredini, S.; Swartz, A.; Sutherland, A.M.; Stephens, M.; Davidson, N.A.; Rose, R. Integrated Pest Management Intervention in Child Care Centers Improves Knowledge, Pest Control, and Practices. J. Pediatr. Health Care 2016, 30, e27–e41. [Google Scholar] [CrossRef] [PubMed]
- Stephens, M.; Hazard, K.; Moser, D.; Cox, D.; Rose, R.; Alkon, A. An Integrated Pest Management Intervention Improves Knowledge, Pest Control, and Practices in Family Child Care Homes. Int. J. Environ. Res. Public Health 2017, 14, 1299. [Google Scholar] [CrossRef]
- Goveia, M.; Shaikh, N.; Windham, G.; Bembom, O.; Feldman, K.; Kreutzer, R. Asthma-Related Environmental Practices and Asthma Awareness in California Child Care Centers. Pediatr. Asthma Allergy Immunol. 2005, 18, 12–24. [Google Scholar] [CrossRef]
- Attar, K.; Paul, H. Let’s Clear the Air: Creating Eco-Friendly, Healthy Learning Environments. Available online: https://www.naeyc.org/resources/pubs/tyc/oct2019/eco-friendly-environment (accessed on 2 February 2020).
- University of California Agriculture and Natural Resources. What Is Integrated Pest Management (IPM)? Available online: https://www2.ipm.ucanr.edu/What-is-IPM/ (accessed on 5 April 2021).
- Center for Disease Control and Prevention. Table C1 Child Current Asthma Prevalence and Weighted Number by State or Territory: Behavioral Risk Factor Surveillance System 2016. Available online: https://www.cdc.gov/asthma/brfss/2016/child/C1_508.pdf (accessed on 10 March 2021).
- Centers for Disease Control and Prevention. AsthmaStats Uncontrolled Asthma among Children, 2012–2014. Available online: https://www.cdc.gov/asthma/asthma_stats/documents/AsthmaStats_Asthma_Uncontrolled_Child_PDF_Cleared_H.pdf (accessed on 15 May 2021).
- Oklahoma Department of Human Services. Licensing Requirements for Child Care Programs. Available online: http://www.okdhs.org/OKDHS%20Publication%20Library/14-05.pdf (accessed on 25 March 2020).
- Oklahoma Department of Human Services. Licensing Requirements for Family Child Care Homes and Large Child Care Homes. Available online: http://www.okdhs.org/OKDHS%20Publication%20Library/86-104.pdf (accessed on 20 November 2020).
- Williams, B.D.; Sisson, S.B.; Dev, D.A.; Lowery, B.; Horm, D.; Campbell, J.; Finneran, D.; Graef-Downard, J.; Whaley, L. Associations between Community Built Environments with Early Care and Education Classroom Physical Activity Practices and Barriers. Int. J. Environ. Res. Public Health 2021, 18, 6524. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Young, C.A.; Chan, C.; Stookey, J.; Patel, A.I.; Evans, J.; Cohn, K.; Agana, L.; Yen, I.H.; Fernandez, A.; Cabana, M.D. Development of a Tool to Evaluate Asthma Preparedness and Management in Child-Care Centers. Pediatr. Allergy Immunol. Pulmonol. 2015, 28, 121–128. [Google Scholar] [CrossRef]
- The Center for Children’s Environmental Health Research. Pest Management and Pesticide Use in California Child Care Centers. Available online: https://cerch.berkeley.edu/sites/default/files/pest_mangement_and_pesticide_use_in_california_child_care_centers.pdf (accessed on 30 July 2019).
- Holm, S. A simple sequentially rejective multiple test procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Agana, L.; Melgoza, C. Bleach Exposure in Child Care Settings: Strategies for Elimination or Reduction. Available online: https://www.asthmacommunitynetwork.org/sites/default/files/resource_files/ATF-Final-Project-Report_March-2011.pdf (accessed on 27 March 2020).
- Uhde, E.; Schulz, N. Impact of room fragrance products on indoor air quality. Atmos. Environ. 2015, 106, 492–502. [Google Scholar] [CrossRef]
- Kim, S.; Hong, S.H.; Bong, C.K.; Cho, M.H. Characterization of air freshener emission: The potential health effects. J. Toxicol. Sci. 2015, 40, 535–550. [Google Scholar] [CrossRef]
- Steinemann, A. Volatile emissions from common consumer products. Air Qual. Atmos. Health 2015, 8, 273–281. [Google Scholar] [CrossRef]
- Trantallidi, M.; Dimitroulopoulou, C.; Wolkoff, P.; Kephalopoulos, S.; Carrer, P. EPHECT III: Health risk assessment of exposure to household consumer products. Sci. Total Environ. 2015, 536, 903–913. [Google Scholar] [CrossRef] [PubMed]
- Nørgaard, A.W.; Kudal, J.D.; Kofoed-Sørensen, V.; Koponen, I.K.; Wolkoff, P. Ozone-initiated VOC and particle emissions from a cleaning agent and an air freshener: Risk assessment of acute airway effects. Environ. Int. 2014, 68, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Holm, S.M.; Leonard, V.; Durrani, T.; Miller, M.D. Do we know how best to disinfect child care sites in the United States? A review of available disinfectant efficacy data and health risks of the major disinfectant classes. Am. J. Infect. Control 2019, 47, 82–91. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency. About List N: Disinfectants for Coronavirus (COVID-19). Available online: https://www.epa.gov/coronavirus/about-list-n-disinfectants-coronavirus-covid-19-0 (accessed on 27 July 2021).
- United States Department of Labor. Hazard Communication. Available online: https://www.osha.gov/hazcom (accessed on 27 July 2021).
- Roberts, J.R.; Karr, C.J. Pesticide exposure in children. Pediatrics 2012, 130, e1765–e1788. [Google Scholar] [CrossRef]
- Geiger, C.; Tootelian, D. Healthy Schools Act spurs integrated pest management in California public schools. Calif. Agric. 2005, 59, 235–241. [Google Scholar] [CrossRef]
- Mir, D.F.; Finkelstein, Y.; Tulipano, G.D. Impact of integrated pest management (IPM) training on reducing pesticide exposure in Illinois childcare centers. NeuroToxicol. 2010, 31, 621–626. [Google Scholar] [CrossRef]
- Alkon, A.; Kalmar, E.; Leonard, V.; Flint, M.L.; Kuo, D.; Davidson, N.; Bradman, A. Development and Evaluation of an Integrated Pest Management Toolkit for Child Care Providers. Early Child. Res. Pract. 2012, 14, n2. [Google Scholar]
- Al-Hemoud, A.; Al-Awadi, L.; Al-Khayat, A.; Behbehani, W. Streamlining IAQ guidelines and investigating the effect of door opening/closing on concentrations of VOCs, formaldehyde, and NO2 in office buildings. Build. Environ. 2018, 137, 127–137. [Google Scholar] [CrossRef]
- Hudson, G.; Miller, G.G.; Seikel, K. Regulations, policies, and guidelines addressing environmental exposures in early learning environments: A review. J. Environ. Health 2014, 76, 24–34. [Google Scholar] [PubMed]
| Total 1 (n = 476) | Center 2 (n = 270) | FCCH 3 (n = 193) | ||
|---|---|---|---|---|
| Program Characteristics | n (%) | n (%) | n (%) | p-value 4 |
| Program Hours | ||||
| Half day | 24 (5.0%) | 19 (7.1%) | 3 (1.6%) | - |
| Full day | 441 (92.7%) | 248 (92.9%) | 187 (98.4%) | 0.01 |
| Fully Enrolled | ||||
| Yes | 315 (66.2%) | 166 (61.5%) | 141 (73.1%) | - |
| No | 161 (33.8%) | 104 (38.5%) | 52 (26.9%) | 0.01 |
| NAEYC Accreditation | ||||
| Yes | 58 (12.2%) | 43 (15.9%) | 15 (7.8%) | - |
| No | 418 (87.8%) | 227 (84.1%) | 178 (92.2%) | 0.01 |
| Program Characteristics | Mean (SD) | Mean (SD) | Mean (SD) | p-value 5 |
| Number of Classrooms | ||||
| Total classrooms | 4.2 (3.8) | 5.9 (3.9) | 1.6 (1.7) | <0.001 |
| Preschool aged classrooms | 2.1 (2.4) | 2.6 (2.8) | 1.3 (1.4) | <0.001 |
| Number of Children | ||||
| Total children | 43.7 (52.3) | 67.9 (57.0) | 8.8 (4.1) | <0.001 |
| Preschool-aged children | 21.9 (38.5) | 34.4 (46.5) | 3.7 (2.4) | <0.001 |
| Survey Items | Total (n = 476) | Center (n = 270) | FCCH (n = 193) | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | p-Value 1 | |
| Ever received any type of asthma training | ||||
| Yes | 251 (52.7%) | 166 (61.0%) | 81 (42.0%) | - |
| No | 225 (47.3%) | 104 (39.0%) | 112 (58.0%) | <0.0001 |
| Type of asthma training received | ||||
| Asthma basics | - | - | - | - |
| Yes | 204 (42.9%) | 131 (49.0%) | 70 (36.0%) | - |
| No | 272 (57.1%) | 139 (51.0%) | 123 (64.0%) | 0.01 |
| Reducing asthma allergens and irritants | - | - | - | - |
| Yes | 88 (18.5%) | 58 (21.0%) | 28 (15.0%) | - |
| No | 388 (81.5%) | 212 (79.0%) | 165 (85.0%) | 0.06 |
| Asthma medications use and types | - | - | - | - |
| Yes | 139 (29.2%) | 99 (37.0%) | 37 (19.0%) | - |
| No | 337 (70.8%) | 171 (63.0%) | 156 (81.0%) | <0.0001 |
| Asthma management plans | - | - | - | - |
| Yes | 65 (13.7%) | 46 (17.0%) | 18 (9.0%) | - |
| No | 411 (86.3%) | 224 (83.0%) | 175 (91.0%) | 0.02 |
| Proper administration of asthma medications | - | - | - | - |
| Yes | 170 (35.75%) | 116 (43.0%) | 50 (26.0%) | - |
| No | 306 (64.3%) | 154 (57.0%) | 143 (74.0%) | <0.0001 |
| Policies/guidelines about managing asthma medications | ||||
| Yes | 378 (82.4%) | 237 (88.0%) | 132 (68.0%) | - |
| No | 81 (17.7%) | 33 (12.0%) | 61 (32.0%) | <0.0001 |
| Policies/guidelines about reducing asthma allergens and irritants | ||||
| Yes | 175 (36.8%) | 109 (40.0%) | 63 (33.0%) | - |
| No | 301 (63.2%) | 161 (60.0%) | 130 (67.0%) | 0.09 |
| Pets present at facility | ||||
| Yes | 130 (27.3%) | 19 (7.0%) | 110 (57.0%) | - |
| No | 346 (72.7%) | 251 (93.0%) | 83 (43.0%) | <0.0001 |
| Facility has wall-to-wall carpet | ||||
| Yes | 120 (25.2%) | 60 (22.0%) | 58 (30.0%) | - |
| No | 356 (74.8%) | 210 (78.0%) | 135 (70.0%) | 0.06 |
| Staff smoke or vape on facility property | ||||
| Yes, but outside only | 48 (10.1%) | 39 (14.0%) | 9.0 (5.0%) | <0.0001 |
| Yes, both inside and outside | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - |
| No | 428 (89.9%) | 231 (86.0%) | 184 (95.0%) | - |
| Survey Items | Total (n = 476) | Center (n = 270) | FCCH (n = 193) | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | p-Value 1 | |
| Use bleach at facility | ||||
| Yes | 421 (88.5%) | 233 (86.0%) | 178 (92.0%) | - |
| No | 55 (11.6%) | 37 (14.0%) | 15 (8.0%) | 0.05 |
| Frequency of bleach use at facility | ||||
| Every few months or less often | - | - | - | - |
| Yes | 15 (3.2%) | 6 (2.2%) | 7 (3.6%) | - |
| No | 461 (96.9%) | 264 (97.8%) | 186 (96.4%) | 0.37 |
| Monthly or a few times a month | - | - | - | - |
| Yes | 17 (3.6%) | 8 (3.0%) | 9 (4.7%) | - |
| No | 459 (96.4%) | 262 (97.0%) | 184 (95.3%) | 0.34 |
| Weekly or a few times a week | - | - | - | - |
| Yes | 49 (10.3%) | 15 (5.6%) | 33 (17.1%) | - |
| No | 427 (89.7%) | 255 (94.4%) | 160 (82.9%) | <0.0001 |
| Daily or a few times a day | - | - | - | - |
| Yes | 340 (71.4%) | 204 (75.6%) | 129 (66.8%) | - |
| No | 136 (28.6%) | 66 (24.4%) | 64 (33.2%) | 0.04 |
| Use “low toxicity” or “less toxic” cleaners at facility | ||||
| Yes | 295 (62.0%) | 156 (58.0%) | 131 (68.0%) | - |
| No | 181 (38.0%) | 114 (42.0%) | 62 (32.0%) | 0.03 |
| Use air fresheners at facility | ||||
| Yes | 323 (73.6%) | 164 (61.0%) | 153 (79.0%) | - |
| No | 116 (26.4%) | 106 (39.0%) | 40 (21.0%) | <0.0001 |
| Types of air fresheners used | ||||
| Scented candles | 42 (8.8%) | 6 (2.0%) | 36 (19.0%) | <0.0001 |
| Spray air fresheners | 190 (39.9%) | 106 (39.0%) | 81 (42.0%) | 0.56 |
| Continuous release (such as a plug-in) | 112 (23.5%) | 52 (19.0%) | 59 (31.0%) | <0.0001 |
| Incense | 6 (1.3%) | 2 (1.0%) | 4 (2.0%) | 0.24 |
| Essential oils (reed diffuser or other type of diffuser) | 73 (15.3%) | 34 (13.0%) | 36 (19.0%) | 0.07 |
| Essential oils electric or battery diffuser | 71 (14.9%) | 31 (11.0%) | 39 (20.0%) | 0.01 |
| Potpourri | 1 (0.2%) | 0 (0.0%) | 1 (1.0%) | 0.42 |
| Gel canister | 10 (2.1%) | 6 (2.0%) | 3 (2.0%) | 0.74 |
| Scented wax melts | 25 (5.3%) | 10 (4.0%) | 15 (8.0%) | 0.06 |
| Other types | 13 (2.7%) | 5 (2.0%) | 8 (4.0%) | 0.14 |
| Survey Items | Total (n = 476) | Center (n = 270) | FCCH (n = 193) | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | p-Value 1 | |
| Have indoor pest problem(s) | ||||
| Yes | 225 (47.3%) | 142 (53.0%) | 78 (40.0%) | - |
| No | 251 (52.7%) | 128 (47.0%) | 115 (60.0%) | 0.01 |
| Have outdoor pest problem(s) | ||||
| Yes | 271 (56.9%) | 153 (57.0%) | 114 (59.0%) | - |
| No | 205 (43.1%) | 117 (43.0%) | 79 (41.0%) | 0.61 |
| Use pesticides indoors | ||||
| Do not use pesticides | ||||
| Yes | 120 (25.2%) | 37 (14.0%) | 82 (42.0%) | - |
| No | 356 (74.8%) | 233 (86.0%) | 111 (58.0%) | <0.0001 |
| Pesticides applied by pest control company | - | - | - | - |
| Yes | 233 (49.0%) | 173 (64.0%) | 52 (27.0%) | - |
| No | 243 (51.1%) | 97 (36.0%) | 141 (73.0%) | <0.0001 |
| Pesticides applied by director or someone else | - | - | - | - |
| Yes | 104 (21.9%) | 45 (17.0%) | 57 (30.0%) | - |
| No | 372 (78.2%) | 225 (83.0%) | 136 (70.0%) | <0.0001 |
| Use pesticides outdoors | ||||
| Do not use pesticides | - | - | - | - |
| Yes | 121 (25.4%) | 53 (20.0%) | 66 (34.0%) | - |
| No | 355 (74.6%) | 217 (80.0%) | 127 (66.0%) | <0.0001 |
| Pesticides applied by pest control company | - | - | - | - |
| Yes | 206 (43.3%) | 137 (51.0%) | 62 (32.0%) | - |
| No | 270 (56.7%) | 133 (49.0%) | 131 (68.0%) | <0.0001 |
| Pesticides applied by director or someone else | - | - | - | - |
| Yes | 149 (31.3%) | 79 (29.0%) | 68 (35.0%) | - |
| No | 327 (68.7%) | 191 (71.0%) | 125 (65.0%) | 0.17 |
| Frequency of pesticide used indoors | ||||
| Pesticides were used, but not sprayed, scattered, or “bombed” | - | - | - | - |
| Yes | 168 (35.3%) | 61 (23.0%) | 104 (54.0%) | |
| No | 308 (64.7%) | 209 (77.0%) | 89 (46.0%) | <0.0001 |
| Weekly or monthly | - | - | - | - |
| Yes | 112 (23.5%) | 94 (35.0%) | 12 (6.0%) | - |
| No | 364 (76.5%) | 176 (65.0%) | 181 (94.0%) | <0.0001 |
| Yearly or a few times a year | - | - | - | - |
| Yes | 117 (24.6%) | 67 (25.0%) | 50 (26.0%) | - |
| No | 359 (75.4%) | 203 (75.0%) | 143 (74.0%) | 0.79 |
| Whenever pests become problem | - | - | - | - |
| Yes | 49 (10.3%) | 26 (10.0%) | 22 (11.0%) | - |
| No | 427 (89.7%) | 244 (90.0%) | 171 (89.0%) | 0.54 |
| Frequency of pesticide used outdoors | ||||
| Pesticides were used, but not sprayed, scattered, or “bombed” | - | - | - | - |
| Yes | 153 (32.1%) | 74 (27.0%) | 77 (40.0%) | - |
| No | 323 (67.9%) | 196 (73.0%) | 116 (60%) | <0.0001 |
| Weekly or monthly | - | - | - | - |
| Yes | 74 (15.6%) | 54 (20.0%) | 16 (8.0%) | - |
| No | 402 (84.5%) | 216 (80.0%) | 177 (92.0%) | <0.0001 |
| Yearly or a few times a year | - | - | - | - |
| Yes | 143 (30.0%) | 74 (27.0%) | 67 (35.0%) | - |
| No | 333 (70.0%) | 196 (73.0%) | 126 (65.0%) | 0.09 |
| Whenever pests become a problem | - | - | - | - |
| Yes | 81 (17.0%) | 53 (20.0%) | 27 (14.0%) | - |
| No | 395 (83.0%) | 217 (80.0%) | 166 (86.0%) | 0.11 |
| Written policy for pesticide use 2 | ||||
| Yes | 87 (21.8%) | 73 (31.0%) | 12 (8.0%) | - |
| No | 313 (78.3%) | 164 (69.0%) | 138 (92.0%) | <0.0001 |
| Staff are notified before pesticides are applied 3 | ||||
| Yes | 274 (71.7%) | 166 (72.0%) | 103 (75.0%) | - |
| No | 108 (28.3%) | 66 (28.0%) | 35 (25.0%) | 0.52 |
| Parents are notified before pesticides are applied 4 | ||||
| Yes | 129 (36.7%) | 69 (29.0%) | 59 (42.0%) | - |
| No | 223 (63.4%) | 166 (71.0%) | 80 (58.0%) | 0.01 |
| Survey Items | Indoors | Outdoors | ||
|---|---|---|---|---|
| n | (%) | n | (%) | |
| Type of pest problems (listed in alphabetical order) | ||||
| None | 203 | (42.7%) | 159 | (33.4%) |
| Ants | 125 | (26.3%) | 131 | (27.7%) |
| Aphids | 0 | (0.0%) | 2 | (0.4%) |
| Bed bugs | 7 | (1.5%) | 0 | (0.0%) |
| Cockroaches | 61 | (12.8%) | 6 | (1.3%) |
| Crickets | 5 | (1.1%) | 0 | (0.0%) |
| Fleas | 9 | (1.9%) | 14 | (2.9%) |
| Head lice | 55 | (11.6%) | 0 | (0.0%) |
| Mold | 6 | (1.3%) | 0 | (0.0%) |
| Mosquitoes | 0 | (0.0%) | 17 | (3.6%) |
| Rodents | 38 | (8.0%) | 18 | (3.8%) |
| Scorpions | 0 | (0.0%) | 6 | (1.3%) |
| Snails/Slugs | 3 | (0.6%) | 6 | (1.3%) |
| Snakes | 0 | (0.0%) | 6 | (1.3%) |
| Spiders | 88 | (18.5%) | 99 | (20.8%) |
| Termites | 4 | (0.8%) | 5 | (1.1%) |
| Ticks | 0 | (0.0%) | 3 | (0.6%) |
| Wasps/Yellow Jackets | 5 | (1.1%) | 147 | (30.9%) |
| Other Pests | 15 | (3.2%) | 19 | (30.9%) |
| Pest control methods used | ||||
| Nothing used | 104 | (21.9%) | 109 | (22.9%) |
| Other methods | 10 | (2.1%) | 8 | (1.7%) |
| Chemical Pest Control Methods Used | - | - | - | - |
| Sprayed Pesticides | 220 | (46.2%) | 224 | (47.1%) |
| Poison pellets or powders | 7 | (1.5%) | 17 | (3.6%) |
| Moth balls | 4 | (0.8%) | 0 | (0.0%) |
| Applied weed killer | 0 | (0.0%) | 60 | (12.6%) |
| Non-chemical Pest Control Methods Used | - | - | - | - |
| Cleaned the area | 151 | (31.7%) | 79 | (16.6%) |
| Sealed cracks/openings | 76 | (16.0%) | 35 | (7.4%) |
| Removed food sources | 62 | (13.0%) | 16 | (3.4%) |
| Mouse or rat traps | 53 | (11.1%) | 13 | (2.7%) |
| Bait Stations or poison traps | 53 | (11.1%) | 27 | (5.7%) |
| Fixed leaks | 26 | (5.5%) | 11 | (2.3%) |
| Sticky fly strips | 22 | (4.6%) | 12 | (2.5%) |
| Installed screens or other barriers | 14 | (2.9%) | 11 | (2.3%) |
| Cut grass or weeds | 0 | (0.0%) | 147 | (30.9%) |
| Who applies pesticides at facility | ||||
| No one, nothing used | 120 | (25.2%) | 121 | (25.4%) |
| Pest control company | 233 | (49.0%) | 206 | (43.3%) |
| Me (participant her/himself) | 54 | (11.3%) | 62 | (13.0%) |
| Property owner | 18 | (3.8%) | 30 | (6.3%) |
| Custodial/janitorial staff | 18 | (3.8%) | 37 | (7.8%) |
| Facility director | 16 | (3.4%) | 12 | (2.5%) |
| Another staff member | 7 | (1.5%) | 12 | (2.5%) |
| Someone else (Other) | 4 | (0.8%) | 5 | (1.1%) |
| Not Sure | 3 | (0.6%) | 4 | (0.8%) |
| A family member | 2 | (0.4%) | 5 | (1.1%) |
| Frequency of pesticide use | ||||
| Nothing used | 152 | (31.9%) | 141 | (29.6%) |
| Once a week | 2 | (0.4%) | 4 | (0.8%) |
| Once a month | 110 | (23.1%) | 71 | (14.9%) |
| Once a year | 26 | (5.5%) | 43 | (9.0%) |
| A few times a year | 91 | (19.1%) | 101 | (21.2%) |
| Whenever pests become a problem | 49 | (10.3%) | 81 | (17.0%) |
| Pesticides were used, but not sprayed, scattered, or “bombed” | 17 | (3.6%) | 13 | (2.7%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Querdibitty, C.D.; Williams, B.; Wetherill, M.S.; Sisson, S.B.; Campbell, J.; Gowin, M.; Stephens, L.; Salvatore, A.L. Environmental Health-Related Policies and Practices of Oklahoma Licensed Early Care and Education Programs: Implications for Childhood Asthma. Int. J. Environ. Res. Public Health 2021, 18, 8491. https://doi.org/10.3390/ijerph18168491
Querdibitty CD, Williams B, Wetherill MS, Sisson SB, Campbell J, Gowin M, Stephens L, Salvatore AL. Environmental Health-Related Policies and Practices of Oklahoma Licensed Early Care and Education Programs: Implications for Childhood Asthma. International Journal of Environmental Research and Public Health. 2021; 18(16):8491. https://doi.org/10.3390/ijerph18168491
Chicago/Turabian StyleQuerdibitty, Cassandra D., Bethany Williams, Marianna S. Wetherill, Susan B. Sisson, Janis Campbell, Mary Gowin, Lancer Stephens, and Alicia L. Salvatore. 2021. "Environmental Health-Related Policies and Practices of Oklahoma Licensed Early Care and Education Programs: Implications for Childhood Asthma" International Journal of Environmental Research and Public Health 18, no. 16: 8491. https://doi.org/10.3390/ijerph18168491
APA StyleQuerdibitty, C. D., Williams, B., Wetherill, M. S., Sisson, S. B., Campbell, J., Gowin, M., Stephens, L., & Salvatore, A. L. (2021). Environmental Health-Related Policies and Practices of Oklahoma Licensed Early Care and Education Programs: Implications for Childhood Asthma. International Journal of Environmental Research and Public Health, 18(16), 8491. https://doi.org/10.3390/ijerph18168491








