The Effects of Forest Therapy on Immune Function
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria for Selection of Existing Studies
2.2. Searching for and Selecting Existing Studies
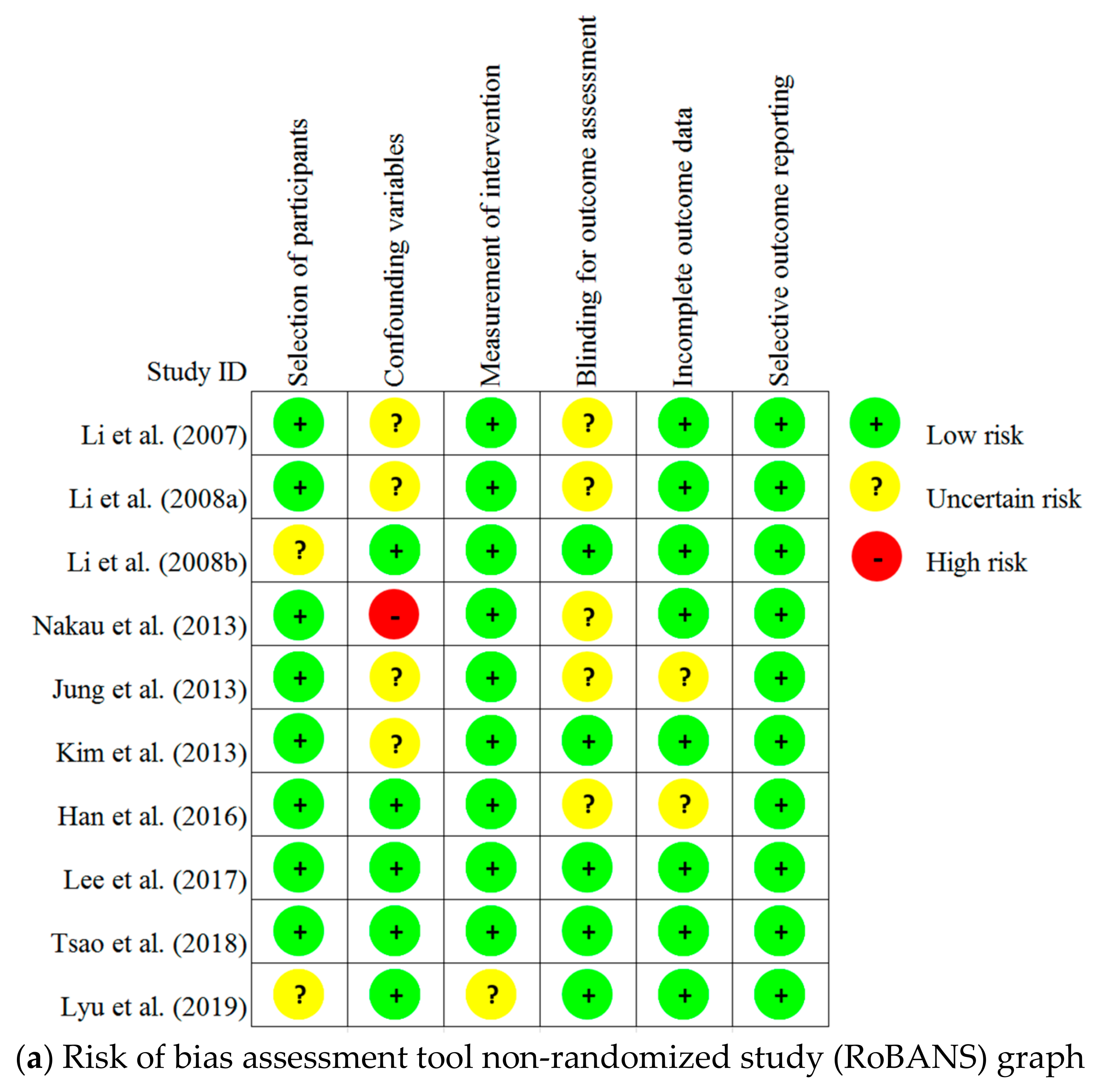
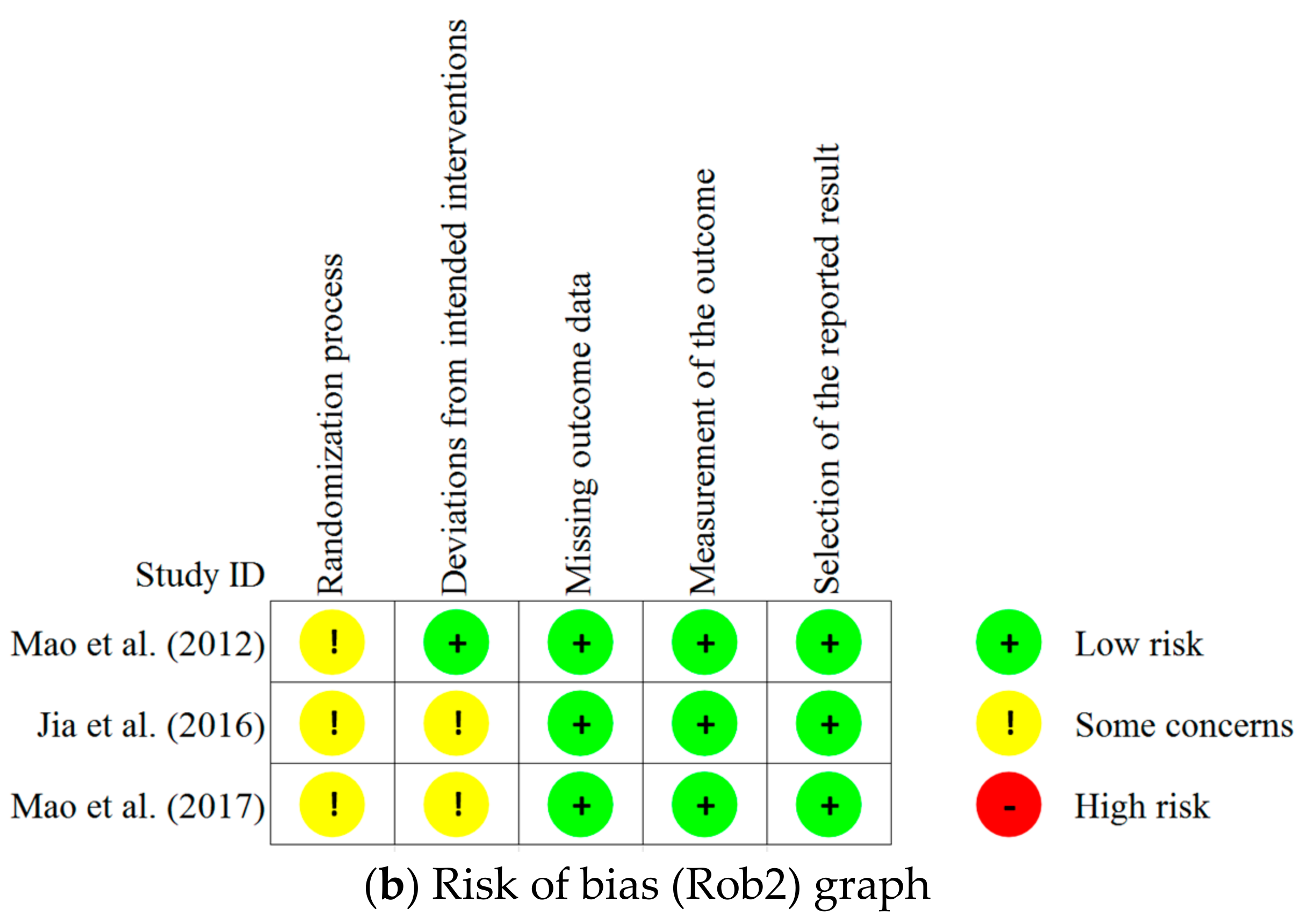
2.3. Risk of Bias Assessment of Individual Studies
2.4. Data Extraction
3. Results
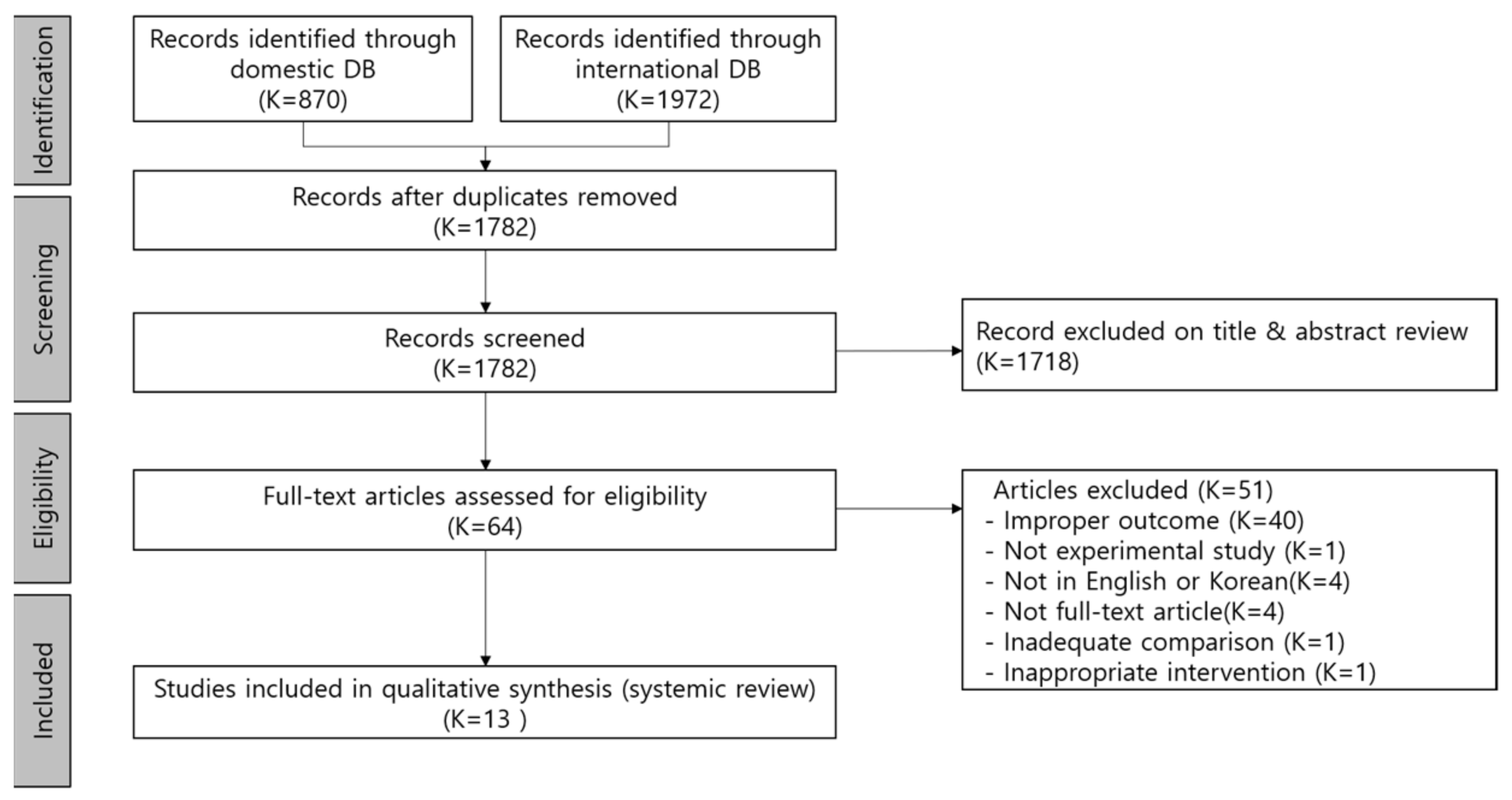
3.1. Study Selection
3.2. Characteristics of the Existing Studies
3.3. Characteristics of the Forest Therapy Program
3.4. Effects of Forest Therapy on Immune Function
3.5. Risk of Bias Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Song, C.; Ikei, H.; Miyazaki, Y. Physiological effects of nature therapy: A review of the research in japan. Int. J. Environ. Res. Public Health 2016, 13, 781. [Google Scholar] [CrossRef]
- Park, J.S.; Yeon, P.S. A network analysis on the forest healing issues using big data—Focused on Korean web news from 2005 to 2019. J. KIFR 2020, 24, 63–71. [Google Scholar]
- Lee, D.G.; Jeong, Y.M.; Lee, M.M.; Shin, W.S.; Yoon, Y.K. The effect of socio-psychological stress on mental well-being mediated by perceived restorativeness-Focusing on visitors whose motive for visiting the forest is ‘COVID-19’. J. KIFR 2020, 24, 99–108. [Google Scholar]
- Lee, I.; Choi, H.; Bang, K.-S.; Kim, S.; Song, M.; Lee, B. Effects of Forest Therapy on Depressive Symptoms among Adults: A Systematic Review. Int. J. Environ. Res. Public Health 2017, 14, 321. [Google Scholar] [CrossRef]
- Oh, B.; Lee, K.J.; Zaslawski, C.; Yeung, A.; Rosenthal, D.; Larkey, L.; Back, M. Health and well-being benefits of spending time in forests: Systematic review. Environ. Health Prev. Med. 2017, 22, 71. [Google Scholar] [CrossRef] [PubMed]
- Chae, Y.R.; Lee, S.H. Systematic review of forest therapy program for adult patients with diseases. J. Korean Biol. Nurs. Sci. 2020, 22, 157–171. [Google Scholar] [CrossRef]
- Woo, J.M.; Park, S.M.; Lim, S.K.; Kim, W. Synergic effect of forest environment and therapeutic program for the treatment of depression. J. Korean Soc. For. Sci. 2012, 101, 677–685. [Google Scholar]
- Li, Q.; Kawada, T. Effect of forest therapy on the human psycho-neuro-endocrino- immune network. Nihon Eiseigaku Zasshi 2011, 66, 645–650. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, B.K.; Lee, H.H. A Study on the effects of human physiology after forest phytoncide therapy. J. Naturopath. 2012, 1, 14–20. [Google Scholar]
- Song, J.H.; Cha, J.G.; Lee, C.Y.; Choi, Y.S.; Yeon, P.S. Effects of forest healing program on stress response and spirituality in female nursing college students and there experience. J. KIFR 2014, 18, 109–125. [Google Scholar]
- Steptoe, A.; Hamer, M.; Chida, Y. The effects of acute psychological stress on circulating inflammatory factors in humans: A review and meta-analysis. Brain Behav. Immun. 2007, 21, 901–912. [Google Scholar] [CrossRef] [PubMed]
- Segerstrom, S.C.; Miller, G.E. Phychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychol. Bull. 2004, 130, 601–630. [Google Scholar] [CrossRef] [Green Version]
- Dhabhar, F.S. Effects of stress on immune function: The good, the bad, and the beautiful. Immunol. Res. 2014, 58, 193–210. [Google Scholar] [CrossRef]
- Walburn, J.; Vedhara, K.; Hankins, M.; Rixon, L.; Weinman, J. Psychological stress and wound healing in humans: A systematic review and meta-analysis. J. Psychosom. Res. 2009, 67, 253–271. [Google Scholar] [CrossRef] [Green Version]
- Webster Marketon, J.I.; Glaser, R. Stress hormones and immune function. Cell. Immunol. 2008, 252, 16–26. [Google Scholar] [CrossRef]
- Roederer, M.; Quaye, L.; Mangino, M.; Beddall, M.H.; Mahnke, Y.; Chattopadhyay, P.; Tosi, I.; Napolitano, L.; Terranova, B.M.; Menni, C.; et al. The genetic architecture of the human immune system: A bioresource for autoimmunity and disease pathogenesis. Cell 2015, 161, 387–403. [Google Scholar] [CrossRef] [Green Version]
- Brodin, P.; Jojic, V.; Gao, T.; Bhattacharya, S.; Angel, C.J.; Furman, D.; Shen-Orr, S.; Dekker, C.L.; Swan, G.E.; Butte, A.J.; et al. Variation in the human immune system is largely driven by non-heritable influences. Cell 2015, 160, 37–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Q.; Morimoto, K.; Nakadai, A.; Inagaki, H.; Katsumata, M.; Shimizu, T.; Hirata, Y.; Hirata, K.; Suzuki, H.; Miyazaki, Y.; et al. Forest bathing enhances human natural killer activity and expression of anti-cancer proteins. Int. J. Immunopathol. Pharmacol. 2007, 20, 3–8. [Google Scholar] [CrossRef]
- Li, Q.; Morimoto, K.; Kobayashi, M.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Shimizu, T.; Li, Y.J.; Wakayama, Y.; et al. A forest bathing trip increases human natural killer activity and expression of anti-cancer proteins in female subjects. J. Biol. Regul. Homeost. Agents. 2008, 22, 45–55. [Google Scholar] [PubMed]
- Li, Q.; Morimoto, K.; Kobayashi, M.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Suzuki, H.; Li, Y.J.; Wakayama, Y.; et al. Visiting forest, but not a city, increases human natural killer activity and expression of anti-cancer proteins. Int. J. Immunopathol. Pharmacol. 2008, 21, 117–127. [Google Scholar] [CrossRef]
- Mao, G.X.; Lan, X.G.; Cao, Y.B.; Chen, Z.M.; He, Z.H.; Lv, Y.D.; Wang, Y.Z.; Hu, X.L.; Wang, G.F.; Yan, J. Effects of short-term forest bathing on human health in a broad-leaved evergreen forest in Zhejiang province, China. Biomed. Environ. Sci. 2012, 25, 317–324. [Google Scholar] [PubMed]
- Nakau, M.; Imanishi, J.; Imanishi, J.; Watanabe, S.; Imanishi, A.; Baba, T.; Hirai, K.; Ito, T.; Chiba, W.; Morimoto, Y. Spiritual care of cancer patients by integrated medicine in urban green space: A pilot study. Explore 2013, 9, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Ideno, Y.; Hayashi, K.; Abe, Y.; Ueda, K.; Iso, H.; Noda, M.; Lee, J.; Suzuki, S. Blood pressure-lowering effect of Shinrin-yoku (Forest bathing): A systematic review and meta-analysis. BMC Complement. Altern. Med. 2017, 17, 409. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomized trials. Br. Med. J. 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.Y.; Park, J.E.; Seo, Y.J.; Jang, B.H.; Son, H.J.; Suh, H.S.; Shin, C.M. NECA’s Guidance for Undertaking Systematic Reviews and Meta-Analyses for Intervention; National Evidence-based Healthcare Collaborating Agency: Seoul, Korea, 2011; pp. 65–78. [Google Scholar]
- Jung, W.H.; Woo, J.M.; Ryu, J.S. Effect of a forest therapy program and the forest environment on female workers’ stress. Urban For. Urban Green. 2015, 14, 274–281. [Google Scholar] [CrossRef]
- Kim, B.J.; Jeong, H.; Park, S.; Lee, S. Forest adjuvant anti-cancer therapy to enhance natural cytotoxicity in urban women with breast cancer: A preliminary prospective interventional study. Eur. J. Integr. Med. 2015, 7, 474–478. [Google Scholar] [CrossRef]
- Jia, B.B.; Yang, Z.X.; Mao, G.X.; Lyu, Y.D.; Wen, X.L.; Xu, W.H.; Lyu, X.L.; Cao, Y.B.; Wang, G.F. Health effect of forest bathing trip on elderly patients with chronic obstructive pulmonary disease. Biomed. Environ. Sci. 2015, 29, 212–218. [Google Scholar]
- Han, J.W.; Choi, H.; Jeon, Y.H.; Yoon, C.H.; Woo, J.M.; Kim, W. The effect of forest therapy on coping with chronic widespread pain: Physiological and psychological differences between participants in a forest therapy program and a control group. Int. J. Environ. Res. Public Health. 2016, 13, 255. [Google Scholar] [CrossRef] [Green Version]
- Mao, G.; Cao, Y.; Wang, B.; Wang, S.; Chen, Z.; Wang, J.; Xing, W.; Ren, X.; Lv, X.; Dong, J.; et al. The salutary influence of forest bathing on elderly patients with chronic heart failure. Int. J. Environ. Res. Public Health. 2017, 14, 368. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.O.; Shin, C.S.; Yeon, P.S.; Shin, M.J.; Lee, J.S.; Choi, J.H. The effects of forest-walking exercise on NK cells and blood melatonin levels of women in their 50s. J. KIFR. 2017, 21, 39–52. [Google Scholar]
- Tsao, T.M.; Tsai, M.J.; Hwang, J.S.; Cheng, W.F.; Wu, C.F.; Chou, C.K.; Su, T.C. Health effects of a forest environment on natural killer cells in humans: An observational pilot study. Oncotarget 2018, 9, 16501–16511. [Google Scholar] [CrossRef] [Green Version]
- Lyu, B.; Zeng, C.; Xie, S.; Li, D.; Lin, W.; Li, N.; Jiang, M.; Liu, S.; Chen, Q. Benefits of a three-day bamboo forest therapy session on the psychophysiology and immune system responses of male college students. Int. J. Environ. Res. Public Health. 2019, 16, 4991. [Google Scholar] [CrossRef] [Green Version]
- Lee, I.; Bang, K.S.; Kim, S.; Song, M.; Kang, K. Status of health promotion programs utilizing forest—Based on 2015–2016 regional healthcare plans in korea. J. Naturopath. 2016, 20, 39–52. [Google Scholar]
- Chae, Y.R.; Kim, J.H.; Kang, H.J. Literature review of forest healing therapy on Korean adult. J. Korean Biol. Nurs. Sci. 2018, 20, 122–131. [Google Scholar] [CrossRef]
- Vivier, E.; Tomasello, E.; Baratin, M.; Walzer, T.; Ugolini, S. Functions of natural killer cells. Nat. Immunol. 2008, 9, 503–510. [Google Scholar] [CrossRef]
- Park, B.J.; Tsunetsugu, Y.; Kasetani, T.; Kagawa, T.; Miyazaki, Y. The physiological effects of Shinrin-yoku (taking in the forest atmosphere or forest bathing): Evidence from field experiments in 24 forests across Japan. Environ. Health Prev. Med. 2010, 15, 18–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trinchieri, G. Biology of natural killer cells. Adv. Immunol. 1989, 47, 187–376. [Google Scholar]
- Na, J.C. Exercise Immunology; DaeKyung Book Publishing: Seoul, Korea, 2002. [Google Scholar]
- Li, Q.; Nakadai, A.; Ishizaki, M.; Morimoto, K.; Ueda, A.; Krensky, A.M.; Kawada, T. Dimethyl 2,2-dichlorovinyl phosphate (DDVP) markedly decreases the expression of perforin, granzyme A and granulysin in human NK-92CI cell line. Toxicology 2005, 213, 107–116. [Google Scholar] [CrossRef]
- Smyth, M.J.; Kelly, J.M.; Sutton, V.R.; Davis, J.E.; Browne, K.A.; Sayers, T.J.; Trapani, J.A. Unlocking the secrets of cytotoxic granule proteins. J. Leukoc. Biol. 2001, 70, 18–29. [Google Scholar] [CrossRef]
- Okada, S.; Li, Q.; Whitin, J.C.; Clayberger, C.; Krensky, A.M. Intracellular mediators of granulysin-induced cell death. J. Immunol. 2003, 171, 2556–2562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krensky, A.M.; Clayberger, C. Granulysin: A novel host defense molecule. Am. J. Transplant. 2005, 5, 1789–1792. [Google Scholar] [CrossRef]
- Smyth, M.J.; Cretney, E.; Kelly, J.M.; Westwood, J.A.; Street, S.E.; Yagita, H.; Takeda, K.; van Dommelen, S.L.; Degli-Esposti, M.A.; Hayakawa, Y. Activation of NK cell cytotoxicity. Mol. Immunol. 2005, 42, 501–510. [Google Scholar] [CrossRef] [PubMed]
- Kägi, D.; Ledermann, B.; Bürki, K.; Seiler, P.; Odermatt, B.; Olsen, K.J.; Podack, E.R.; Zinkernagel, R.M.; Hengartner, H. Cytotoxicity mediated by T cells and natural killer cells is greatly impaired in perforin-deficient mice. Nature 1994, 369, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Heusel, J.W.; Wesselschmidt, R.L.; Shresta, S.; Russell, J.H.; Ley, T.J. Cytotoxic lymphocytes require granzyme B for the rapid induction of DNA fragmentation and apoptosis in allogeneic target cells. Cell 1994, 76, 977–987. [Google Scholar] [CrossRef]
- Tsunetsugu, Y.; Tsunetsugu, Y.; Park, B.J.; Miyazaki, Y. Trends in research related to “Shinrin-yoku” (taking in the forest atmosphere or forest bathing) in Japan. Environ. Health Prev. Med. 2010, 15, 27–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Q.; Kobayashi, M.; Wakayama, Y.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Shimizu, T.; Kawada, T.; Park, B.-J.; et al. Effect of phytoncide from trees on human natural killer cell function. Int. J. Immunopathol. Pharmacol. 2009, 22, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Nakadai, A.; Matsushima, H.; Miyazaki, Y.; Krensky, A.M.; Kawada, T.; Morimoto, K. Phytoncides (wood essential oils) induce human natural killer cell activity. Immunopharmacol. Immunotoxicol. 2006, 28, 319–333. [Google Scholar] [CrossRef] [PubMed]
- Hochman, P.S.; Cudkowicz, G.; Dausset, J. Decline of natural killer cell activity in sublethally irradiated mice. J. Natl. Cancer Inst. 1978, 61, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Shibata, H.; Fujiwara, R.; Iwamoto, M.; Matsuoka, H.; Yokoyama, M.M. Immunological and behavioral effects of fragrance in mice. Int. J. Neurosci. 1991, 57, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Komori, T.; Fujiwara, R.; Tanida, M.; Nomura, J.; Yokoyama, M.M. Effects of citrus fragrance on immune function and depressive states. Neuroimmunomodulation 1995, 2, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Park, S.N. A Study on Anti-Stress Effect of Phytoncides. Ph.D. Thesis, Daejeon University, Daejeon, Korea, 2016. Unpublished. [Google Scholar]
- Kim, H.M.; Cho, J.K.; Ahn, K.M.; Kim, T.Y.; Lee, J.H.; Jang, D.M.; Min, C.K. Antitumor effects of phytoncides: Vitalization of natural killer cells. J. Sci. Educ. Gift. 2013, 5, 96–104. [Google Scholar]
| Characteristic | Categories | N (%) |
|---|---|---|
| Publication year | ≤2006 | 0 (0) |
| 2007–2010 | 3 (23.1) | |
| 2011–2015 | 4 (30.8) | |
| ≥2016 | 6 (46.2) | |
| Participants | Healthy adults | 6 (46.2) |
| Adults with health problems | 5 (38.5) | |
| Not reported | 2 (15.4) | |
| Country/Regions | China | 4 (30.8) |
| Korea | 4 (30.8) | |
| Japan | 4 (30.8) | |
| Taiwan | 1 (7.7) | |
| Study Design | Randomized control group | 3 (23.1) |
| Nonequivalent control group pre-posttest design | 5 (38.5) | |
| One group pre-post test design | 5 (38.5) | |
| Sample size | ≤20 | 7 (53.8) |
| 21–50 | 4 (30.8) | |
| ≥51 | 2 (15.4) | |
| Statement of ethical consideration | Yes | 12 (92.3) |
| No | 1 (7.7) |
| Authors (Years) | Study Design | Participants (n) | Intervention | Control | Outcome (Measurements) | |
|---|---|---|---|---|---|---|
| 1 | Li et al. (2007) [18] | One group pre-posttest design | Healthy male, aged 37~55 years (12) Mean age: 43.1 ± 6.1 | A three-day/two-night trip First day: walked for two hours in the afternoon in a forest field Second day: walked for two hours each in the morning and afternoon in two different forest field On day 3: finished the trip | None | · NK cells **↑, NK activity **↑, · T cells · granulysin **↑, perforin **↑, granzymes A **↑/B **↑ · WBC, (Lymphocytes *↑, Monocytes*↑, Granulocytes **↓) · T-A *↓, D *↓, A-H, F, C, V **↑(POMS) · the hours of sleep |
| 2 | Li et al. (2008) [19] | One group pre-posttest design | Healthy female nurses, aged 25~43 years (13) Mean age: 28.8 ± 4.6 | A three-day/two-night trip First day: walked for two hours in the afternoon in a forest field Second day: walked for two hours each in the morning and afternoon in two different forest field On day 3: finished the trip | None | · NK cells **↑, NK activity **↑ · T cells *↓ · granulysin **↑, perforin **↑, granzymes A **↑/B **↑ · Adrenalin **↓, noradrenaline (Urine) **↓ · Estradiol, progesterone · T-A, D **↓, A-H, F, C, V (POMS) |
| 3 | Li et al. (2008) [20] | None-equivalent control group pre-posttest design | Healthy male, aged 35~56 years (E:12, C:11) Mean age: 45.1 ± 6.7 | A three-day/two-night forest bathing program First day: walked for two hours in the afternoon in a forest field Second day: walked for two hours each in the morning and afternoon in two different forest field On day 3: finished the trip | A three-day/two-night city trip First day: walked for two hours in the afternoon in an old-style district in the city Second day: walked for two hours around baseball Dome in the morning and 2 h around/in airport in the afternoon On day 3: finished the trip | · NK cells *↑, NK activity *↑ · T cells · granulysin **↑, perforin **↑, and granzymes A **↑/B **↑ · WBC · Adrenaline (Urine) *↓ |
| 4 | Mao et al. (2012) [21] | RCT | Healthy male university students (E:10, C:10) Mean age: 20.79 ± 0.54 | two-night trip walked for 1.5 h each in the morning and afternoon in a forest field | walked for 1.5 h each in the morning and afternoon in a city site | · NK cells · T cell, B cell *↑, T-helper cells. suppressor cells, natural killer cells · IL-6*↓, TNF-α *↓ · T-SOD, MDA **↓ · ET-1 **↓, Platelet activation · Cortisol *↓, Testosterone · T-A *↓, D *↓, A-H *↓, F *↓, C, V *↑(POMS) |
| 5 | Nakau et al. (2013) [22] | One group pre-posttest design | Breast cancer or lung cancer (22) Mean age: 58.1 ± 10.8 | Walking in the forest, Horticultural therapy, yoga meditation, and support group therapy, and sessions were conducted once a week for 12 weeks | None | · NK activity **↑ · Well-being of functional and spiritual (FACIT-Sp): GP, GS, GE, GF *↑, Sp *↑ · Quality of life (SF-36): PF *↑, RP *↑, BP, GH *↑, VT **↑, SF, RE *↑, MH *↑ · Fatigue (CFS) **↓ · T-A *↓, D, A-H, F, C **↓, V (POMS) · STAI: State anxiety **↓, Trait anxiety *↓ |
| 6 | Jung et al. (2015) [27] | None-equivalent control group pre-posttest design | Workers in the healthcare and counseling service industries (E:19, C:20) Mean age E: 29.42 ± 8.92, C:36.45 ± 12.23 | 3 days, 2 nights, Walking and meditation in the forest, and exposure to a psychological program using music and cognitive-behavioral therapy. | frequently use the environment without participating in the program | · NK activity · Cortisol *↑ · HRV · MBI-GS **↓, WRSI *↓, REQ **↑ |
| 7 | Kim et al. (2015) [28] | One group pre-posttest design | Stage 3 Breast cancer patient, aged 25~60 years (11) Mean age: 56 ± 5.12 (11) | Stay in the forest for 14 days, Forest therapy program (Walk, forest life) | None | · NK cells **↑ · Perforin *↑, Granzyme B *↑ |
| 8 | Jia et al. (2016) [29] | RCT | elderly patients with chronic obstructive pulmonary disease (E: 10, C: 8) Mean age E: 70.1 C: 70 | 4 days, walking in the forest (total 3 h walk/day) | 4 days, walking in the city (total 3 h walk/day) | · NK cells, NKT-like cell, CD8+ T cells · Perforin **↓, Granzyme B · IL-6 *↓, IL-8 **↓, interleukin-1β *↓, TNF-α interferon-γ *↓, CRP *↓ · Cortisol *↓, Epinephrine *↓ · RARC/CCL-18 **↓, TIMP-1 *↓, SP-D *↓ · T-A **↓, D *↓, A-H *↓, F, C, V (POMS) |
| 9 | Han et al. (2016) [30] | None-equivalent control group pre-posttest design | Full-time employees with chronic widespread pain for more than three months, aged 25~49 years (E: 33, C: 28) Mean age E: 41.6 ± 6.5, C: 37.5 ± 8.4 | 2 days forest therapy program Walking and therapeutic activities in the forest activities (music therapy, psycho-education: coping with pain and stress, bodily exercises, mindfulness-based meditation) | The control group was instructed not to conduct either heavy loads of domestic or occupational work during the enrollment in this study. | · NK activity **↑ · Heart rate variability (HRV) **↑ · Self-reported pain **↓ (VAS) · Depression **↓ (BDI) · Health-related quality of life **↑ (EQ-VAS) |
| 10 | Mao et al. (2017) [31] | RCT | Elderly patients with chronic heart failure, Aged from 65 to 80 years (E: 23, C: 10) Mean age 73.86 ± 5.85 years old | 4 days, Walking in the forest (total 3 h walk/day) | 4 days, Walking in the city (total 3 h walk/day) | · IL-6 *↓, TNF-α, CRP · BNP **↓, N-terminal pro BNP · ET-1 **↓, Renin, AGT, Ang II, AT1, AT2 **↑ · T-SOD *↑, MDA *↓ · T-A *↓, D **↓, A-H **↓, F, C **↓, V (POMS) |
| 11 | Lee et al. (2017) [32] | None-equivalent control group pre-posttest design | Women in their 50 s (E: 9, C: 9) Mean age E: 53.9 ± 2.69, C: 55.5 ± 1.84 | Forest walking exercise for 12 weeks (3 times/week, 110 min/day) | Ground walking exercise for 12 weeks (3 times/week, 110 min/day) | · NK cells *↑ · Melatonin *↑ |
| 12 | Tsao et al. (2018) [33] | One group pre-post test design | Middle-aged subjects (11) Mean age: 60.4 | A five-day/four-night trip (maintain dietary control and walking exercise) First day: walked for 1.5 h in the afternoon in a forest field Next three days: walked for 1.5 h each in the morning and afternoon in two different forest field Fifth day: finished the trip | None | · NK cells, NK activity **↑ |
| 13 | Lyu et al. (2019) [34] | None-equivalent control group pre-posttest design | Male College Students (E: 45, C: 15) Mean age E: 20.9 ± 0.24, C: 21.3 ± 0.45 | Bamboo forest site exposure for three days | City site exposure for three days | · NK cells *↑. NK activity *↑, · granulysin, perforin *↑, granzymes A *↑/B *↑, · corticosterone *↓ · SBP *↓, DBP, HR, SpO2 · T-A *↓, D *↓, A-H *↓, F *↓, C *↓, V *↑ (POMS) |
| Outcome | Article Number | ||
|---|---|---|---|
| Significant | Not Significant | ||
| Number of NK cells | 18, 19, 20, 28, 32, 34 | 21, 29, 33 | |
| NK cells cytotoxic activity | 18, 19, 20, 22, 30, 33, 34 | 27 | |
| T cells | 19 | 18, 20, 21 | |
| B cells | 21 | ||
| T suppressor cells | 21 | ||
| T-helper cells | 21 | ||
| Natural killer T(NKT) like cells | 29 | ||
| Cytotoxic T cells | 29 | ||
| Cytotoxic effector molecules | granulysin | 18, 19, 20 | 34 |
| perforin | 18, 19, 20, 28, 29, 34 | ||
| granzymes A | 18, 19, 20, 34 | ||
| granzymes B | 18, 19, 20, 28. 34 | 29 | |
| Proinflammatory cytokines | interleukin-6 (IL-6) | 21, 29, 31 | |
| interleukin-8 (IL-8) | 29 | ||
| interferon-γ (IFN-γ) | 29 | ||
| interleukin-1β (IL-1β) | 29 | ||
| tumor necrosis factor α (TNF-α) | 21 | 29, 31 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chae, Y.; Lee, S.; Jo, Y.; Kang, S.; Park, S.; Kang, H. The Effects of Forest Therapy on Immune Function. Int. J. Environ. Res. Public Health 2021, 18, 8440. https://doi.org/10.3390/ijerph18168440
Chae Y, Lee S, Jo Y, Kang S, Park S, Kang H. The Effects of Forest Therapy on Immune Function. International Journal of Environmental Research and Public Health. 2021; 18(16):8440. https://doi.org/10.3390/ijerph18168440
Chicago/Turabian StyleChae, Youngran, Sunhee Lee, Youngmi Jo, Soyean Kang, Suyoun Park, and Hyoyoung Kang. 2021. "The Effects of Forest Therapy on Immune Function" International Journal of Environmental Research and Public Health 18, no. 16: 8440. https://doi.org/10.3390/ijerph18168440
APA StyleChae, Y., Lee, S., Jo, Y., Kang, S., Park, S., & Kang, H. (2021). The Effects of Forest Therapy on Immune Function. International Journal of Environmental Research and Public Health, 18(16), 8440. https://doi.org/10.3390/ijerph18168440





