Resilience and Equity in a Time of Crises: Investing in Public Urban Greenspace Is Now More Essential Than Ever in the US and Beyond
Abstract
:1. Introduction
2. Four Intersecting Crises: Structural Racism, COVID-19, Climate Change, and Chronic Diseases
2.1. Structural Racism and Health Outcomes
2.1.1. A Brief History of Structural Racism in American Cities
2.1.2. Structural and Environmental Racism
2.2. Structural Racism and COVID-19
2.3. Climate Change and Health Inequity
2.4. Persistent Chronic Disease Burden and Inequity
2.5. Urgent, Intertwined Crises
3. Urban Public Greenspace as a Critical Component of an Antiracist Strategy for Global Environmental Health Equity
3.1. Greenspaces Enable Resilience for the COVID-19 Pandemic
3.2. Greenspaces Improve Chronic Disease Outcomes and Can Reduce Health Inequities
3.3. Greenspaces Are Essential Components of Climate Change Mitigation and Adaptation
4. The Way Forward: Harnessing a Moment of Political Will to Make Strategic Investments in Equitable Urban Greenspaces and Trees
5. Key Strategies and Considerations: Examples from Milwaukee, Wisconsin
5.1. Recognize and Carefully Consider Distinct Types of Greenspaces and Their Various Strengths and Drawbacks before Investing
5.2. Focus on Equity, Prepare for, and Prevent Green Gentrification
5.3. Consider Plantable Spaces and Ensure Connectivity for Greenspaces Safer Use
5.4. Activate Greenspaces for Safety and Maximal Health Benefit
5.5. Leverage the Greenspace for Environmental Education to Build a Culture of Environmental Stewardship
5.6. Maintenance Planning, and How It Will Be Funded, Should Be Discussed from the Start
5.7. Consider, Link to, or Embed Workforce Development Opportunities
5.8. Plan for Waste and Harness the Promise of Urban Wood
5.9. Engage Communities, Local Partners, and Key Stakeholders Early and Often
5.9.1. Engage to Fund and Sustain Investment
5.9.2. Engage to Educate
5.9.3. Engage on Design and to Find a “Fit”
5.9.4. Engage around Ownership, Use and Maintenance
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Patz, J.A.; Gibbs, H.K.; Foley, J.A.; Rogers, J.V.; Smith, K.R. Climate change and global health: Quantifying a growing ethical crisis. Ecohealth 2007, 4, 397–405. [Google Scholar] [CrossRef]
- Madrigano, J.; Shih, R.A.; Izenberg, M.; Fischbach, J.R.; Preston, B.L. Science Policy to Advance a Climate Change and Health Research Agenda in the United States. Int. J. Environ. Res. Public Health 2021, 18, 7868. [Google Scholar] [CrossRef]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Hardeman, R.R.; Medina, E.M.; Kozhimannil, K.B. Structural Racism and Supporting Black Lives-The Role of Health Professionals. N. Engl. J. Med. 2016, 375, 2113–2115. [Google Scholar] [CrossRef] [Green Version]
- Gee, G.C.; Payne-Sturges, D.C. Environmental health disparities: A framework integrating psychosocial and environmental concepts. Environ. Health Perspect. 2004, 112, 1645–1653. [Google Scholar] [CrossRef] [Green Version]
- Turner, T.M.; Luea, H. Homeownership, wealth accumulation and income status. J. Hous. Econ. 2009, 18, 104–114. [Google Scholar] [CrossRef]
- Kolmes, S. Employment-Based, For-Profit Health Care in a Pandemic. Hastings Cent. Rep. 2020, 50, 22. [Google Scholar] [CrossRef]
- Williams, D.R.; Sternthal, M. Understanding Racial-ethnic Disparities in Health: Sociological Contributions. J. Health Soc. Behav. 2010, 51, S15–S27. [Google Scholar] [CrossRef] [PubMed]
- Massey, D.S.; Denton, N.A. American Apartheid: Segregation and the Making of the Underclass; Harvard University Press: Cambridge, MA, USA, 1993; ISBN 978067401821. [Google Scholar]
- Egede, L.E.; Walker, R.J. Structural Racism, Social Risk Factors, and Covid-19—A Dangerous Convergence for Black Americans. N. Engl. J. Med. 2020, 383, e77. [Google Scholar] [CrossRef] [PubMed]
- Link, B.G.; Phelan, J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995, 80–94. [Google Scholar] [CrossRef] [Green Version]
- Reskin, B. The race discrimination system. Annu. Rev. Sociol. 2012, 38, 17–35. [Google Scholar] [CrossRef]
- Krieger, N. Discrimination and health inequities. Int. J. Heal. Serv. 2014, 44, 643–710. [Google Scholar] [CrossRef]
- Massey, D.S. Residential segregation and neighborhood conditions in US metropolitan areas. Am. Becom. Racial Trends Conseq. 2001, 1, 391–434. [Google Scholar]
- Garcia, M.A.; García, C.; Brown, T. The Color of COVID-19: Structural Racism and the Pandemic’s Disproportionate Impact on Older Black and Latinx Adults. Artic. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2020. [Google Scholar] [CrossRef]
- Benfer, E.A.; Wiley, L.F. Health justice strategies to combat COVID-19: Protecting vulnerable communities during a pandemic. Health Aff. Blog 2020. [Google Scholar]
- Smedley, A.; Smedley, B.D. Anthropological and Historical Perspectives on the Social Construction of Race. Available online: http://rws200jspencer.pbworks.com/w/file/fetch/104349117/Race%20as%20Biology%20Is%20Fiction.pdf (accessed on 16 March 2021).
- Ross, M.A. The Supreme Court, Reconstruction, and the Meaning of the Civil War. J. Supreme Court Hist. 2016, 41, 275–294. [Google Scholar] [CrossRef]
- Dickerson, D. The Reconstruction Era: Primary Documents on Events from 1865 to 1877 (Debating Historical Issues in the Media of the Time); Greenwood Press: Westport, CT, USA, 2003. [Google Scholar]
- Center for American Progress Systematic Inequality and Economic Opportunity. Available online: https://www.americanprogress.org/issues/race/reports/2019/08/07/472910/systematic-inequality-economic-opportunity/ (accessed on 16 March 2021).
- Derenoncourt, E. Can you move to opportunity? Evidence from the Great Migration. Available online: https://scholar.harvard.edu/files/elloraderenoncourt/files/derenoncourt_jmp_2018.pdf (accessed on 5 April 2021).
- Du Bois, W.E.B. Darkwater: Voices from Within the Veil; Dover Publications: Mineola, NY, USA, 1999. [Google Scholar]
- Pierce, C.W.E.B. Du Bois and Caste Education: Racial Capitalist Schooling From Reconstruction to Jim Crow. Am. Educ. Res. J. 2017, 54, 23S–47S. [Google Scholar] [CrossRef]
- Seabrook, R.; Wyatt-Nichol, H. The Ugly Side of America: Institutional Oppression and Race. J. Public Manag. Soc. Policy 2016, 23. [Google Scholar]
- Duque, R.B. Black Health Matters Too Especially in the Era of Covid-19: How Poverty and Race Converge to Reduce Access to Quality Housing, Safe Neighborhoods, and Health and Wellness Services and Increase the Risk of Co-morbidities Associated with Global Pandemics. J. Racial Ethn. Health Disparities 2020, 2020, 1–14. [Google Scholar] [CrossRef]
- Taylor, D.E. Black Farmers in the USA and Michigan: Longevity, Empowerment, and Food Sovereignty. J. Afr. Am. Stud. 2018, 22, 49–76. [Google Scholar] [CrossRef] [Green Version]
- Boustan, L.P. Was Postwar Suburbanization “White Flight”? Evidence from the Black Migration. Q. J. Econ. 2010, 125, 417–443. [Google Scholar] [CrossRef]
- Tabellini, M. Racial Heterogeneity and Local Government Finances: Evidence from the Great Migration. SSRN Electron. J. 2018. [Google Scholar] [CrossRef] [Green Version]
- Myrdal, G. Social Trends in American and Strategic Approaches to the Negro Problem. Phylon (1940–1956) 1948, 9, 196–214. [Google Scholar] [CrossRef]
- Wright, R.R. The migration of negroes to the north. Ann. Am. Acad. Pol. Soc. Sci. 1906. [Google Scholar] [CrossRef]
- Du Bois, W. The health and physique of the Negro American: Report of a social study made under the direction of Atlanta University. In Proceedings of the Eleventh Conference for the Study of the Negro Problems, Atlanta, GA, USA, 29 May 1096. [Google Scholar]
- Black, D.A.; Sanders, S.G.; Taylor, E.J.; Taylor, L.J. The Impact of the Great Migration on Mortality of African Americans: Evidence from the Deep South. Am. Econ. Rev. 2015, 105, 477–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hillier, A.E. Redlining and the Homeowners’ Loan Corporation. J. Urban Hist. 2003, 29, 394–420. [Google Scholar] [CrossRef]
- Clark, A. The Poisoned City: Flint’s Water and the American Urban Tragedy; Metropolitan Books: New York, NY, USA, 2018; ISBN 1250125146. [Google Scholar]
- Mapping Inequality. Available online: https://dsl.richmond.edu/panorama/redlining/#loc=5/39.1/-94.58 (accessed on 9 April 2021).
- Faber, J. We Built This: Consequences of New Deal Era Intervention in America’s Racial Geography. Am. Sociol. Rev. 2020, 85, 739–775. [Google Scholar] [CrossRef]
- Aaronson, D.; Faber, J.; Hartley, D.; Mazumder, B.; Sharkey, P. The Long-run Effects of the 1930s HOLC “Redlining” Maps on Place-based Measures of Economic Opportunity and Socioeconomic Success. Reg. Sci. Urban Econ. 2020, 86, 103622. [Google Scholar] [CrossRef]
- Appel, I.; Nickerson, J. Pockets of Poverty: The Long-Term Effects of Redlining. SSRN Electron. J. 2016. [Google Scholar] [CrossRef]
- Jacob, K. Persistence of Prejudice: Estimating the Long Term Effects of Redlining. SocArXiv 2018. [Google Scholar] [CrossRef]
- Faber, J. Contemporary echoes of segregationist policy: Spatial marking and the persistence of inequality. Urban Stud. 2020, 58, 1067–1086. [Google Scholar] [CrossRef]
- Nardone, A.; Rudolph, K.E.; Morello-Frosch, R.; Casey, J.A.; Anthony, N. Redlines and Greenspace: The Relationship between Historical Redlining and 2010 Greenspace across the United States. Environ. Health Perspect. 2021, 129, 17006. [Google Scholar] [CrossRef] [PubMed]
- Howell, J.; Elliott, J.R. As Disaster Costs Rise, So Does Inequality. Socius Sociol. Res. A Dyn. World 2018, 4, 237802311881679. [Google Scholar] [CrossRef]
- Katz, L. Formerly Redlined Areas Have 25% More Home Value At High Flood Risk. Available online: https://www.redfin.com/news/redlining-flood-risk/ (accessed on 28 May 2021).
- President Obama Remarks by the President on Responsible Homeownership. Available online: https://obamawhitehouse.archives.gov/the-press-office/2013/08/06/remarks-president-responsible-homeownership (accessed on 29 August 2019).
- President Bush President Bush Boosts Homeownership in America - Lauds Work by the Department, Non-Profits and Local Volunteers. Available online: https://archives.hud.gov/content/focus/2001-06-12.cfm (accessed on 29 August 2019).
- United States Census Bureau: Housing Vacancies and Homeownership. Available online: https://www.census.gov/housing/hvs/index.html (accessed on 29 August 2019).
- Krivo, L.J.; Kaufman, R.L. Housing and Wealth Inequality: Racial-Ethnic Differences in Home Equity in the United States. Demography 2004, 41, 585–605. [Google Scholar] [CrossRef]
- Killewald, A. Return to Being Black, Living in the Red: A Race Gap in Wealth That Goes Beyond Social Origins. Demography 2013, 50, 1177–1195. [Google Scholar] [CrossRef]
- Hamilton, D.; Darity, W.A. The Political Economy of Education, Financial Literacy, and the Racial Wealth Gap. Review 2017, 99, 59–76. [Google Scholar] [CrossRef] [Green Version]
- Oliver, M.L.; Shapiro, T.M. Disrupting the Racial Wealth Gap. Contexts 2019, 18, 16–21. [Google Scholar] [CrossRef]
- Perry, V.G. A Loan at Last? Race and Racism in Mortgage Lending. In Race in the Marketplace; Springer International Publishing: Cham, Switzerland, 2019; pp. 173–192. [Google Scholar]
- Keister, L.A.; Moller, S. Wealth Inequality in the United States. Annu. Rev. Sociol. 2000, 26, 63–81. [Google Scholar] [CrossRef] [Green Version]
- Perry, A.; Rothwell, J.; Harshbarger, D. The devaluation of assets in black neighborhoods. Available online: https://www.brookings.edu/research/devaluation-of-assets-in-black-neighborhoods/ (accessed on 29 August 2019).
- Namin, S.; Xu, W.; Zhou, Y.; Beyer, K. The legacy of the Home Owners’ Loan Corporation and the political ecology of urban trees and air pollution in the United States. Soc. Sci. Med. 2020, 246, 112758. [Google Scholar] [CrossRef]
- Woo, B.; Kravitz-Wirtz, N.; Sass, V.; Crowder, K.; Teixeira, S.; Takeuchi, D.T. Residential Segregation and Racial/Ethnic Disparities in Ambient Air Pollution. Race Soc. Probl. 2019, 11, 60–67. [Google Scholar] [CrossRef]
- Hartley, T. Environmental Justice: An Environmental Civil Rights Value Acceptable to All World Views. Environ. Ethics 1995, 17, 277–289. [Google Scholar] [CrossRef]
- Commission for Racial Justice: United Church of Christ TOXIC WASTES AND RACE In The United States: A National Report on the Racial and Socio-Economic Characteristics of Communities with Hazardous Waste Sites Exhibit 13. Available online: https://www.nrc.gov/docs/ML1310/ML13109A339.pdf (accessed on 4 March 2021).
- Bullard, R. Anatomy of Environmental Racism and the Environmental Justice Movement. In Confronting Environmental Racism: Voices from the Grassroots; Bullard, R., Ed.; South End Press: Boston, MA, USA, 1993; ISBN 0896084469. [Google Scholar]
- Keehan, C.J. Lessons from Cancer Alley: How the Clean Air Act Has Failed to Protect Public Health in Southern Louisiana. Colo. Nat. Resour. Energy Envtl. L. Rev. 2018, 29, 341. [Google Scholar]
- Whyte, K. The Dakota access pipeline, environmental injustice, and US colonialism. Red Ink Int. J. Indig. Lit. Arts Humanit. 2017, 19, 154–169. [Google Scholar]
- Maantay, J. Zoning, equity, and public health. Am. J. Public Health 2001, 91, 1033–1041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paradies, Y.; Ben, J.; Denson, N.; Elias, A.; Priest, N.; Pieterse, A.; Gupta, A.; Kelaher, M.; Gee, G. Racism as a determinant of health: A systematic review and meta-analysis. PLoS ONE 2015, 10, 1–48. [Google Scholar] [CrossRef] [Green Version]
- Morello-Frosch, R.; Jesdale, B.M. Separate and unequal: Residential segregation and estimated cancer risks associated with ambient air toxins in U.S. metropolitan areas. Environ. Health Perspect. 2006, 114, 386–393. [Google Scholar] [CrossRef] [Green Version]
- Kravitz-Wirtz, N.; Crowder, K.; Hajat, A.; Sass, V. The Long-Term Dynamics of Racial/Ethnic Inequality in Neighborhood Air Pollution Exposure, 1990-2009. Du Bois Rev.Soc. Sci. Res. Race 2016, 13, 237–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawachi, I.; Kennedy, B.P.; Wilkinson, R.G. Crime: Social disorganization and relative deprivation. Soc. Sci. Med. 1999, 48, 719–731. [Google Scholar] [CrossRef]
- Williams, D.R.; Collins, C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Rep. 2001, 116, 404. [Google Scholar] [CrossRef]
- Desmond, M. Eviction and the reproduction of urban poverty. Am. J. Sociol. 2012, 118, 88–133. [Google Scholar] [CrossRef] [Green Version]
- Desmond, M.; Kimbro, R.T. Eviction’s fallout: Housing, hardship, and health. Soc. Forces 2015, 94, 295–324. [Google Scholar] [CrossRef]
- Williams, D.R.; Mohammed, S.A. Discrimination and racial disparities in health: Evidence and needed research. J. Behav. Med. 2009, 32, 20–47. [Google Scholar] [CrossRef] [Green Version]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., III; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Kaufman, J.D.; et al. Particulate Matter Air Pollution and Cardiovascular Disease. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef] [Green Version]
- Pope, C.A.; Bhatnagar, A.; McCracken, J.P.; Abplanalp, W.; Conklin, D.J.; O’Toole, T. Exposure to Fine Particulate Air Pollution Is Associated with Endothelial Injury and Systemic Inflammation. Circ. Res. 2016, 119, 1204–1214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soriano, J.B.; Kendrick, P.J.; Paulson, K.R.; Gupta, V.; Abrams, E.M.; Adedoyin, R.A.; Adhikari, T.B.; Advani, S.M.; Agrawal, A.; Ahmadian, E.; et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2020, 8, 585–596. [Google Scholar] [CrossRef]
- Pope, C.A., III; Dockery, D.W. Health effects of fine particulate air pollution: Lines that connect. J. Air Waste Manage. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef] [PubMed]
- Bailey, Z.D.; Krieger, N.; Agénor, M.; Graves, J.; Linos, N.; Bassett, M.T. Structural racism and health inequities in the USA: Evidence and interventions. Lancet 2017, 389, 1453–1463. [Google Scholar] [CrossRef]
- Gee, G.C.; Ford, C.L. Structural Racism and Health Inequities: Old Issues, New Directions1. Du Bois Rev. Soc. Sci. Res. Race 2011, 8, 115. [Google Scholar] [CrossRef] [Green Version]
- Sarche, M.; Spicer, P. Poverty and health disparities for American Indian and Alaska Native children: Current knowledge and future prospects. Ann. N. Y. Acad. Sci. 2008, 1136, 126. [Google Scholar] [CrossRef] [Green Version]
- Warne, D.; Wescott, S. Social determinants of American Indian nutritional health. Curr. Dev. Nutr. 2019, 3, 12–18. [Google Scholar] [CrossRef] [PubMed]
- McClure, E.S.; Vasudevan, P.; Bailey, Z.; Patel, S.; Robinson, W.R. Racial Capitalism Within Public Health—How Occupational Settings Drive COVID-19 Disparities. Am. J. Epidemiol. 2020, 189, 1244–1253. [Google Scholar] [CrossRef]
- Pirtle, W.N.L. Racial capitalism: A fundamental cause of novel coronavirus (COVID-19) pandemic inequities in the United States. Health Educ. Behav. 2020. [Google Scholar] [CrossRef]
- Robinson, C. Black Marxism: The Making of the Black Radical Tradition; University of North Carolina Press: Chapel Hill, NC, USA, 2000. [Google Scholar]
- Kim, S.J.; Bostwick, W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ. Behav. 2020, 47, 509–513. [Google Scholar] [CrossRef]
- Hawkins, D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am. J. Ind. Med. 2020, 63, 817–820. [Google Scholar] [CrossRef]
- Alkon, A.H.; Bowen, S.; Kato, Y.; Young, K.A. Unequally vulnerable: A food justice approach to racial disparities in COVID-19 cases. Agric. Hum. Values 2020, 37, 535–536. [Google Scholar] [CrossRef]
- Gravlee, C.C. Systemic racism, chronic health inequities, and COVID-19: A syndemic in the making? Am. J. Hum. Biol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, J.F.; Wadhera, R.K.; Lee, D.; Yeh, R.W.; Sommers, B.D. Community-Level Factors Associated With Racial And Ethnic Disparities In COVID-19 Rates In Massachusetts. Health Aff. 2020, 10–1377. [Google Scholar] [CrossRef]
- Horst, M.; Marion, A. Racial, ethnic and gender inequities in farmland ownership and farming in the U.S. Agric. Hum. Values 2019, 36, 1–16. [Google Scholar] [CrossRef]
- Harris, A. (Re)Integrating Spaces: The Color of Farming. Savannah Law Rev. 2015, 2, 157. [Google Scholar]
- Chen, Y.-H.; Glymour, M.; Riley, A.; Balmes, J.; Duchowny, K.; Harrison, R.; Matthay, E.; Bibbins-Domingo, K. Excess mortality associated with the COVID-19 pandemic among Californians 18-65 years of age, by occupational sector and occupation: March through October 2020. PLoS ONE 2021. [Google Scholar] [CrossRef]
- De Salud, C.; Valle, D.; Salinas, D.E. Summary Report Prevalence and Predictors of SARS-COV-2 Infection Among Farmworkers in Monterey County, CA UC Berkeley School of Public Health Executive Summary. Available online: https://cerch.berkeley.edu/sites/default/files/ucb_csvs_white_paper_12_01_20_final_compressed.pdf (accessed on 28 January 2021).
- Food and Agriculture Vulnerability Index. Available online: https://ag.purdue.edu/agecon/Pages/FoodandAgVulnerabilityIndex.aspx?_ga=2.49471334.1159720487.1600111458-250602208.1598985334 (accessed on 28 January 2021).
- Yearby, R.; Mohapatra, S. Law, structural racism, and the COVID-19 pandemic. J. Law Biosci. 2020, 7, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Carrion, D.; Colicino, E.; Pedretti, N.F.; Arfer, K.B.; Rush, J.; DeFelice, N.; Just, A.C. Assessing capacity to social distance and neighborhood-level health disparities during the COVID-19 pandemic. medRxiv 2020. [Google Scholar] [CrossRef]
- Berkowitz, R.L.; Gao, X.; Michaels, E.K.; Mujahid, M.S. Structurally vulnerable neighbourhood environments and racial/ethnic COVID-19 inequities. Cities Health 2020, 1–4. [Google Scholar] [CrossRef]
- Von Seidlein, L.; Alabaster, G.; Deen, J.; Knudsen, J. Crowding has consequences: Prevention and management of COVID-19 in informal urban settlements. Build. Environ. 2020, 107472. [Google Scholar] [CrossRef]
- Guadamuz, J.S.; Wilder, J.R.; Mouslim, M.C.; Zenk, S.N.; Alexander, G.C.; Qato, D.M. Fewer Pharmacies In Black And Hispanic/Latino Neighborhoods Compared With White Or Diverse Neighborhoods, 2007–15. Health Aff. 2021, 40, 802–811. [Google Scholar] [CrossRef]
- Domingo, J.L.; Marquès, M.; Rovira, J. Influence of airborne transmission of SARS-CoV-2 on COVID-19 pandemic. A review. Environ. Res. 2020, 188, 109861. [Google Scholar] [CrossRef]
- Hendryx, M.; Luo, J. COVID-19 prevalence and fatality rates in association with air pollution emission concentrations and emission sources. Environ. Pollut. 2020, 265, 115126. [Google Scholar] [CrossRef]
- Bashir, M.F.; Jiang, B.; Komal, B.; Bashir, M.A.; Farooq, T.H.; Iqbal, N.; Bashir, M. Correlation between environmental pollution indicators and COVID-19 pandemic: A brief study in Californian context. Environ. Res. 2020, 187, 109652. [Google Scholar] [CrossRef]
- Bashir, M.F.; Benghoul, M.; Numan, U.; Shakoor, A.; Komal, B.; Bashir, M.A.; Bashir, M.; Tan, D. Environmental pollution and COVID-19 outbreak: Insights from Germany. Air Qual. Atmos. Health 2020, 13, 1385–1394. [Google Scholar] [CrossRef]
- Tessum, C.W.; Paolella, D.A.; Chambliss, S.E.; Apte, J.S.; Hill, J.D.; Marshall, J.D. PM2. 5 polluters disproportionately and systemically affect people of color in the United States. Sci. Adv. 2021, 7, eabf4491. [Google Scholar] [CrossRef]
- Xiaopeng, L.; Lawrence, L.; Carpenter,, D.O. Association between Residential Proximity to Fuel-Fired Power Plants and Hospitalization Rate for Respiratory Diseases. Environ. Health Perspect. 2012, 120, 807–810. [Google Scholar] [CrossRef] [Green Version]
- U.S. Government Accountability Office (U.S. GAO). Sitting of Hazardous Wastes Landfills and thier correlation with Racial and Economic Status of the Surrounding Communities. Available online: https://www.gao.gov/assets/150/140159.pdf (accessed on 4 March 2021).
- Mikati, I.; Benson, A.F.; Luben, T.J.; Sacks, J.D.; Richmond-Bryant, J. Disparities in distribution of particulate matter emission sources by race and poverty status. Am. J. Public Health 2018, 108, 480–485. [Google Scholar] [CrossRef]
- Servadio, J.L.; Lawal, A.S.; Davis, T.; Bates, J.; Russell, A.G.; Ramaswami, A.; Convertino, M.; Botchwey, N. Demographic Inequities in Health Outcomes and Air Pollution Exposure in the Atlanta Area and its Relationship to Urban Infrastructure. J. Urban Health 2019, 96, 219–234. [Google Scholar] [CrossRef] [PubMed]
- American Lung Association Disparities in the Impact of Air Pollution. Available online: https://www.lung.org/clean-air/outdoors/who-is-at-risk/disparities (accessed on 4 March 2021).
- Hagemeyer, A.N.; Sears, C.G.; Zierold, K.M. Respiratory Health in Adults Residing Near a Coal-Burning Power Plant with Coal Ash Storage Facilities: A Cross-Sectional Epidemiological Study. Int. J. Environ. Res. Public Health 2019, 16, 3642. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.-K.; Lin, R.-T.; Chen, T.; Zigler, C.; Wei, Y.; Christiani, D.C. A global perspective on coal-fired power plants and burden of lung cancer. Environ. Health 2019, 18, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Copat, C.; Cristaldi, A.; Fiore, M.; Grasso, A.; Zuccarello, P.; Signorelli, S.S.; Conti, G.O.; Ferrante, M. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: A systematic review. Environ. Res. 2020, 191, 110129. [Google Scholar] [CrossRef] [PubMed]
- Energy Burden in Milwaukee: Study Reveals Major Disparities & Links to Redlined Areas. Available online: https://www.sierraclub.org/sites/www.sierraclub.org/files/sce-authors/u560/2392%20MilwaukeeEnergy_Report_06_high%20%281%29.pdf (accessed on 28 May 2021).
- Drehobl, A.; Ross, L. Lifting the High Energy Burden in America’s Largest Cities: How Energy Efficiency Can Improve Low Income and Underserved Communities. Available online: https://www.aceee.org/sites/default/files/publications/researchreports/u1602.pdf (accessed on 28 May 2021).
- Yang, T.-C.; Emily Choi, S.; Sun, F. COVID-19 cases in US counties: Roles of racial/ethnic density and residential segregation. Ethn. Health 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Phillips, N.; Park, I.-W.; Robinson, J.R.; Jones, H.P. The perfect storm: Covid-19 health disparities in us blacks. J. Racial Ethn. Health Disparities 2020, 1–8. [Google Scholar] [CrossRef]
- Valderas, J.M.; Starfield, B.; Sibbald, B.; Salisbury, C.; Roland, M. Defining comorbidity: Implications for understanding health and health services. Ann. Fam. Med. 2009, 7, 357–363. [Google Scholar] [CrossRef]
- Lopez, L., III; Hart, L.H., III; Katz, M.H. Racial and Ethnic Health Disparities Related to COVID-19. JAMA 2021, 325, 719–720. [Google Scholar] [CrossRef]
- Egede, L.E.; Walker, R.J.; Garacci, E.; Raymond Sr, J.R. Racial/Ethnic Differences In COVID-19 Screening, Hospitalization, And Mortality In Southeast Wisconsin. Health Aff. 2020, 39, 1926–1934. [Google Scholar] [CrossRef]
- Selden, T.M.; Berdahl, T.A. COVID-19 And Racial/Ethnic Disparities In Health Risk, Employment, And Household Composition: Study examines potential explanations for racial-ethnic disparities in COVID-19 hospitalizations and mortality. Health Aff. 2020, 39, 1624–1632. [Google Scholar] [CrossRef]
- Price-Haywood, E.G.; Burton, J.; Fort, D.; Seoane, L. Hospitalization and Mortality among Black Patients and White Patients with Covid-19. N. Engl. J. Med. 2020, 382, 2534–2543. [Google Scholar] [CrossRef]
- Van Dorn, A.; Cooney, R.E.; Sabin, M.L. COVID-19 exacerbating inequalities in the US. Lancet (Lond. Engl.) 2020, 395, 1243. [Google Scholar] [CrossRef]
- Krieger, N. Enough: COVID-19, structural racism, police brutality, plutocracy, climate change—and time for health justice, democratic governance, and an equitable, sustainable future. Am. J. Public Health 2020, 110, 1620–1623. [Google Scholar] [CrossRef]
- Field, C.B.; Barros, V.; Stocker, T.F.; Dahe, Q. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation: Special Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2012; ISBN 1107025060. [Google Scholar]
- Rudolph, L.; Gould, S. Climate change and health inequities: A framework for action. Ann. Glob. Health 2015, 81. [Google Scholar] [CrossRef] [PubMed]
- Bikomeye, J.C.; Rublee, C.S.; Beyer, K.M.M. Positive Externalities of Climate Change Mitigation and Adaptation for Human Health: A Review and Conceptual Framework for Public Health Research. Int. J. Environ. Res. Public Health 2021, 18, 2481. [Google Scholar] [CrossRef] [PubMed]
- Cardona, O.-D.; van Aalst, M.K.; Birkmann, J.; Fordham, M.; McGregor, G.; Perez, R.; Pulwarty, R.S.; Lisa Schipper, E.F.; Tan Sinh, B.; Décamps, H.; et al. Determinants of Risk: Exposure and Vulnerabilit: Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation 2 Determinants of Risk: Exposure and Vulnerability; Intergovernmental Panel on Climate Change: Melbourne, VIC, Australia, 2012. [Google Scholar]
- National Centers for Environmental Information (NCEI) U.S. Billion-Dollar Weather and Climate Disasters, 1980-Present. Available online: https://www.ncdc.noaa.gov/billions/ (accessed on 16 March 2021).
- National Oceanic and Atmospheric Administration. Record number of Billion-Dollar Disasters Struck U.S. in 2020. Available online: https://www.noaa.gov/stories/record-number-of-billion-dollar-disasters-struck-us-in-2020 (accessed on 16 March 2021).
- Wei, Y.; Wang, Y.; Lin, C.-K.; Yin, K.; Yang, J.; Shi, L.; Li, L.; Zanobetti, A.; Schwartz, J.D. Associations between seasonal temperature and dementia-associated hospitalizations in New England. Environ. Int. 2019, 126, 228–233. [Google Scholar] [CrossRef]
- Islam, N.; Winkel, J. Climate Change and Social Inequality: The Un Department of Economic And Social Affairs (Desa) Working Papers Aim to Stimulate Discussion and Critical Comment on the Broad Range of Economic, Social and Environmental Issues Associated with the United Nation. Available online: https://www.oecd-ilibrary.org/content/paper/2c62335d-en (accessed on 12 February 2021).
- Thomas, K.; Hardy, R.D.; Lazrus, H.; Mendez, M.; Orlove, B.; Rivera-Collazo, I.; Roberts, J.T.; Rockman, M.; Warner, B.P.; Winthrop, R. Explaining differential vulnerability to climate change: A social science review. Wiley Interdiscip. Rev. Clim. Chang. 2019, 10, e565. [Google Scholar] [CrossRef] [Green Version]
- Roberts, J.T.; Parks, B. A Climate of Injustice: Global Inequality, North-South Politics, and Climate Policy; MIT press: Cambridge, MA, USA, 2006; ISBN 0262264412. [Google Scholar]
- Medina-Ramón, M.; Schwartz, J. Temperature, temperature extremes, and mortality: A study of acclimatisation and effect modification in 50 US cities. Occup. Environ. Med. 2007, 64, 827–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Basu, R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ. Health 2009, 8, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, T.; Horton, R.M.; Kinney, P.L. Projections of seasonal patterns in temperature- related deaths for Manhattan, New York. Nat. Clim. Chang. 2013, 3, 717–721. [Google Scholar] [CrossRef] [Green Version]
- Bouwer, L.M. Observed and Projected Impacts from Extreme Weather Events: Implications for Loss and Damage. In Loss and Damage from Climate Change; Mechler, R., Bouwer, L.M., Schinko, T., Surminski, S., Linnerooth-Bayer, J., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 63–82. ISBN 978-3-319-72026-5. [Google Scholar]
- Roy, S.B.; Chen, L.; Girvetz, E.H.; Maurer, E.P.; Mills, W.B.; Grieb, T.M. Projecting water withdrawal and supply for future decades in the U.S. under climate change scenarios. Environ. Sci. Technol. 2012, 46, 2545–2556. [Google Scholar] [CrossRef]
- Brown, T.C.; Foti, R.; Ramirez, J.A. Projected freshwater withdrawals in the United States under a changing climate. Water Resour. Res. 2013, 49, 1259–1276. [Google Scholar] [CrossRef]
- National Climate Assessment Water Supply. Available online: https://nca2014.globalchange.gov/highlights/report-findings/water-supply (accessed on 2 March 2021).
- Kroeker, K.J.; Kordas, R.L.; Crim, R.; Hendriks, I.E.; Ramajo, L.; Singh, G.S.; Duarte, C.M.; Gattuso, J.P. Impacts of ocean acidification on marine organisms: Quantifying sensitivities and interaction with warming. Glob. Chang. Biol. 2013, 19, 1884–1896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doney, S.C.; Ruckelshaus, M.; Emmett Duffy, J.; Barry, J.P.; Chan, F.; English, C.A.; Galindo, H.M.; Grebmeier, J.M.; Hollowed, A.B.; Knowlton, N.; et al. Climate change impacts on marine ecosystems. Ann. Rev. Mar. Sci. 2012, 4, 11–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feely, R.A.; Doney, S.C.; Cooley, S.R. Ocean acidification: Present conditions and future changes in a high-CO 2 world. Oceanography 2009, 22, 36–47. [Google Scholar] [CrossRef] [Green Version]
- Doney, S.C.; Balch, W.M.; Fabry, V.J.; Feely, R.A. Ocean acidification: A critical emerging problem for the ocean sciences. Oceanography 2009, 22, 16–25. [Google Scholar] [CrossRef] [Green Version]
- Cooley, S.R.; Kite-Powell, H.L.; Doney, S.C. Ocean acidification’s potential to alter global marine ecosystem services. Oceanography 2009, 22, 172–181. [Google Scholar] [CrossRef] [Green Version]
- Wisshak, M.; Schönberg, C.H.L.; Form, A.; Freiwald, A. Ocean Acidification Accelerates Reef Bioerosion. PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [Green Version]
- Kroeker, K.J.; Kordas, R.L.; Crim, R.N.; Singh, G.G. Meta-analysis reveals negative yet variable effects of ocean acidification on marine organisms. Ecol. Lett. 2010, 13, 1419–1434. [Google Scholar] [CrossRef]
- National Climate Assessment Agriculture. Available online: https://nca2014.globalchange.gov/highlights/report-findings/agriculture (accessed on 2 March 2021).
- Patz, J.A.; Vavrus, S.J.; Uejio, C.K.; McLellan, S.L. Climate Change and Waterborne Disease Risk in the Great Lakes Region of the U.S. Am. J. Prev. Med. 2008, 35, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Curriero, F.C.; Patz, J.A.; Rose, J.B.; Lele, S. The Association Between Extreme Precipitation and Waterborne Disease Outbreaks in the United States, 1948–1994. Am. J. Public Health 2001, 91, 1194–1199. [Google Scholar] [CrossRef] [PubMed]
- Rice, M.B.; Thurston, G.D.; Balmes, J.R.; Pinkerton, K.E. Climate change. A global threat to cardiopulmonary health. Am. J. Respir. Crit. Care Med. 2014, 189, 512–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Climate Assessment Human Health. Available online: https://nca2014.globalchange.gov/highlights/report-findings/human-health (accessed on 1 March 2021).
- Wilson, K. Climate change and the spread of infectious ideas. Ecology 2009, 90, 901–902. [Google Scholar] [CrossRef]
- Mills, J.N.; Gage, K.L.; Khan, A.S. Potential influence of climate change on vector-borne and zoonotic diseases: A review and proposed research plan. Environ. Health Perspect. 2010, 118, 1507–1514. [Google Scholar] [CrossRef] [Green Version]
- Russell, R.C. Mosquito-borne disease and climate change in Australia: Time for a reality check. Aust. J. Entomol. 2009, 48, 1–7. [Google Scholar] [CrossRef]
- Tabachnick, W.J. Challenges in predicting climate and environmental effects on vector-borne disease episystems in a changing world. J. Exp. Biol. 2010, 213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gage, K.L.; Burkot, T.R.; Eisen, R.J.; Hayes, E.B. Climate and Vectorborne Diseases. Am. J. Prev. Med. 2008, 35, 436–450. [Google Scholar] [CrossRef]
- Keesing, F.; Brunner, J.; Duerr, S.; Killilea, M.; LoGiudice, K.; Schmidt, K.; Vuong, H.; Ostfeld, R.S. Hosts as ecological traps for the vector of Lyme disease. Proc. R. Soc. B Biol. Sci. 2009, 276, 3911–3919. [Google Scholar] [CrossRef] [Green Version]
- Ogden, N.H.; St-Ong, L.; Barker, I.K.; Brazeau, S.; Bigras-Poulin, M.; Charron, D.F.; Francis, C.M.; Heagy, A.; Lindsay, L.; Thompson, R.; et al. Risk maps for range expansion of the Lyme disease vector, Ixodes scapularis, in Canada now and with climate change. Int. J. Health Geogr. 2008, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dennekamp, M.; Carey, M. Air quality and chronic disease: Why action on climate change is also good for health. N. S. W. Public Health Bull. 2010, 21, 115–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prüss-Ustün, A.; van Deventer, E.; Mudu, P.; Campbell-Lendrum, D.; Vickers, C.; Ivanov, I.; Forastiere, F.; Gumy, S.; Dora, C.; Adair-Rohani, H. Environmental risks and non-communicable diseases. BMJ 2019, 364, 1265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, S.; Luo, M.; Walker, R.J.; Liu, X.; Hwang, S.-A.; Chinery, R. Extreme High Temperatures and Hospital Admissions for Respiratory and Cardiovascular Diseases. Epidemiology 2009, 20, 738–746. [Google Scholar] [CrossRef]
- Henderson, S.B.; Brauer, M.; MacNab, Y.C.; Kennedy, S.M. Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environ. Health Perspect. 2011, 119, 1266–1271. [Google Scholar] [CrossRef]
- Delfino, R.J.; Brummel, S.; Wu, J.; Stern, H.; Ostro, B.; Lipsett, M.; Winer, A.; Street, D.H.; Zhang, L.; Tjoa, T.; et al. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup. Environ. Med. 2009, 66, 189–197. [Google Scholar] [CrossRef] [Green Version]
- Natural Resources Defense Council The Costs of Inaction: The Economic Burden of Fossil Fuels and Climate Change on Health in the United States. Available online: https://www.nrdc.org/sites/default/files/costs-inaction-burden-health-report.pdf (accessed on 28 May 2021).
- Kafalenos, R.S.; Leonard, K.J.; Beagan, D.M.; Burkett, V.R.; Keim, B.D.; Meyers, A.; Hunt, D.T.; Hyman, R.C.; Maynard, M.K.; Fritsche, B.; et al. Impacts of Climate Change and Variability on Transportation Systems and Infrastructure: Gulf Study, Phase I. A report by the U.S. Climate Change Science Program and the Subcommittee on Global Change Research. Final Report of Synthesis and Assessment Product; U.S. Department of Transportation: Washington, DC, USA, 2008.
- National Climate Assessment Infrastructure. Available online: https://nca2014.globalchange.gov/highlights/report-findings/infrastructure (accessed on 2 March 2021).
- Friel, S.; Hancock, T.; Kjellstrom, T.; McGranahan, G.; Monge, P.; Roy, J. Urban health inequities and the added pressure of climate change: An action-oriented research agenda. J. Urban Health 2011, 88, 886. [Google Scholar] [CrossRef] [Green Version]
- Salas, R.N.; Knappenberger, P.; Hess, J.J. Lancet Countdown on Health and Climate Change: Policy Brief for the United States of America. London, United Kingdom. 2020. Available online: http://www.lancetcountdownus.org/wp-content/uploads/2020/12/FINAL-2020_12_02_Lancet-Countdown-Policy-Document-USA-ENG.pdf?hsCtaTracking=3d902c23-c855-441f-ab5d-61f4f76a2ea1%7C6d90df30-4bf7-42f3-a282-f61d5292a03e (accessed on 2 March 2021).
- Patz, J.A. Solving the global climate crisis: The greatest health opportunity of our times? Public Health Rev. 2016, 37, 30. [Google Scholar] [CrossRef] [Green Version]
- National Climate Assessment Indigenous Peoples. Available online: https://nca2014.globalchange.gov/highlights/report-findings/indigenous-peoples (accessed on 2 March 2021).
- Oudin Åström, D.; Bertil, F.; Joacim, R. Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas 2011, 69, 99–105. [Google Scholar] [CrossRef]
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Beagley, J.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D. The 2020 report of The Lancet Countdown on health and climate change: Responding to converging crises. Lancet 2020. [Google Scholar] [CrossRef]
- Yu, W.; Mengersen, K.; Wang, X.; Ye, X.; Guo, Y.; Pan, X.; Tong, S. Daily average temperature and mortality among the elderly: A meta-analysis and systematic review of epidemiological evidence. Int. J. Biometeorol. 2012, 56, 569–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zanobetti, A.; O’Neill, M.S.; Gronlund, C.J.; Schwartz, J.D. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc. Natl. Acad. Sci. USA 2012, 109, 6608–6613. [Google Scholar] [CrossRef] [Green Version]
- Stone, B.J.; Mallen, E.; Rajput, M.; Gronlund, C.J.; Broadbent, A.M.; Krayenhoff, E.S.; Augenbroe, G.; O’Neill, M.S.; Georgescu, M. Compound Climate and Infrastructure Events: How Electrical Grid Failure Alters Heat Wave Risk. Environ. Sci. Technol. 2021, 55, 6957–6964. [Google Scholar] [CrossRef] [PubMed]
- Tessum, C.W.; Apte, J.S.; Goodkind, A.L.; Muller, N.Z.; Mullins, K.A.; Paolella, D.A.; Polasky, S.; Springer, N.P.; Thakrar, S.K.; Marshall, J.D. Inequity in consumption of goods and services adds to racial-ethnic disparities in air pollution exposure. Proc. Natl. Acad. Sci. USA 2019, 116, 6001–6006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- US Environmental Protection Agency. Tribal Air and Climate Resources. Available online: https://www.epa.gov/tribal-air (accessed on 1 March 2021).
- American Lung Association. Key Findings | State of the Air. Available online: https://www.lung.org/research/sota/key-findings (accessed on 28 May 2021).
- Schneider, C.; Uhl, S.; Ross, S.; Banks, J.; Mccabe, D.; Graham, J.; Taylor, K.; Fleischman, L.; Franklin, M. Fumes across the fence-line: The health impacts of air pollution from oil & gas facilities on African American communities; Boston Branch NAACP: Boston, MA, USA, 2017. [Google Scholar]
- Cushing, L.J.; Vavra-Musser, K.; Chau, K.; Franklin, M.; Johnston, J.E. Flaring from unconventional oil and gas development and birth outcomes in the Eagle Ford Shale in south Texas. Environ. Health Perspect. 2020, 128, 77003. [Google Scholar] [CrossRef] [PubMed]
- Casey, J.A.; Savitz, D.A.; Rasmussen, S.G.; Ogburn, E.L.; Pollak, J.; Mercer, D.G.; Schwartz, B.S. Unconventional natural gas development and birth outcomes in Pennsylvania, USA. Epidemiology 2016, 27, 163. [Google Scholar] [CrossRef] [Green Version]
- Walker Whitworth, K.; Kaye Marshall, A.; Symanski, E. Drilling and production activity related to unconventional gas development and severity of preterm birth. Environ. Health Perspect. 2018, 126, 37006. [Google Scholar] [CrossRef]
- Emanuel, R.E.; Caretta, M.A.; Rivers, L.; Vasudevan, P. Natural Gas Gathering and Transmission Pipelines and Social Vulnerability in the United States. GeoHealth 2021. [Google Scholar] [CrossRef]
- Rasmussen, S.G.; Ogburn, E.L.; McCormack, M.; Casey, J.A.; Bandeen-Roche, K.; Mercer, D.G.; Schwartz, B.S. Association between unconventional natural gas development in the Marcellus Shale and asthma exacerbations. JAMA Intern. Med. 2016, 176, 1334–1343. [Google Scholar] [CrossRef]
- Willis, M.D.; Jusko, T.A.; Halterman, J.S.; Hill, E.L. Unconventional natural gas development and pediatric asthma hospitalizations in Pennsylvania. Environ. Res. 2018, 166, 402–408. [Google Scholar] [CrossRef]
- Wheeler, T.; Von Braun, J. Climate change impacts on global food security. Science 2013, 341, 508–513. [Google Scholar] [CrossRef]
- Hasegawa, T.; Fujimori, S.; Havlík, P.; Valin, H.; Bodirsky, B.L.; Doelman, J.C.; Fellmann, T.; Kyle, P.; Koopman, J.F.L.; Lotze-Campen, H. Risk of increased food insecurity under stringent global climate change mitigation policy. Nat. Clim. Chang. 2018, 8, 699–703. [Google Scholar] [CrossRef] [Green Version]
- Bowler, D.E.; Buyung-Ali, L.; Knight, T.M.; Pullin, A.S. Urban greening to cool towns and cities: A systematic review of the empirical evidence. Landsc. Urban Plan. 2010, 97, 147–155. [Google Scholar] [CrossRef]
- Aram, F.; Higueras García, E.; Solgi, E.; Mansournia, S. Urban green space cooling effect in cities. Heliyon 2019, 5, e01339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The World Health Organization. The top 10 causes of death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 21 January 2021).
- Murphy, S.L.; Kochanek, K.D.; Xu, J. Deaths: Final data for 2011. Natl. Vital Stat. Reports 2015, 63, 3. [Google Scholar]
- Mehta, L.S.; Watson, K.E.; Barac, A.; Beckie, T.M.; Bittner, V.; Cruz-Flores, S.; Dent, S.; Kondapalli, L.; Ky, B.; Okwuosa, T.; et al. Cardiovascular Disease and Breast Cancer: Where These Entities Intersect: A Scientific Statement From the American Heart Association. Circulation 2018, 137, e30–e66. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; Floyd, J.; Fornage, M.; Gillespie, C.; Isasi, C.R. Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef]
- American Cancer Society. Cancer Facts and Figures. 2020. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf (accessed on 2 May 2021).
- Ahmad, F.B.; Anderson, R.N. The Leading Causes of Death in the US for 2020. JAMA 2021. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA. Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef]
- Woolf, S.H.; Chapman, D.A.; Lee, J.H. COVID-19 as the Leading Cause of Death in the United States. JAMA 2021, 325, 123–124. [Google Scholar] [CrossRef]
- Ahmad, F.B.; Cisewski, J.A.; Miniño, A.; Anderson, R.N. Provisional Mortality Data—United States, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 519–522. [Google Scholar] [CrossRef]
- Weaver, L.C.; Jessup, A.; Mayer, D.K. Cancer survivorship care: Implications for primary care advanced practice nurses. Nurse Pract. 2013, 38, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bertero, E.; Ameri, P.; Maack, C. Bidirectional Relationship Between Cancer and Heart Failure: Old and New Issues in Cardio-oncology. Card. Fail. Rev. 2019, 5, 106–111. [Google Scholar] [CrossRef] [Green Version]
- Koene, R.J.; Prizment, A.E.; Blaes, A.; Konety, S.H. Shared risk factors in cardiovascular disease and cancer. Circulation 2016, 133, 1104–1114. [Google Scholar] [CrossRef] [Green Version]
- Williams, D.R.; Jackson, P.B. Social sources of racial disparities in health. Health Aff. (Millwood) 2005, 24, 325–334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin, A.B.; Hartman, M.; Lassman, D.; Catlin, A. National health care spending in 2019: Steady growth for the fourth consecutive year. Health Aff. 2021, 40, 14–24. [Google Scholar] [CrossRef]
- US Center for Disease Control. Health and Economic Costs of Chronic Diseases. Available online: https://www.cdc.gov/chronicdisease/about/costs/index.htm (accessed on 3 March 2021).
- Park, J.; Look, K.A. Health care expenditure burden of cancer care in the United States. Inq. J. Health Care Organ. Provis. Financ. 2019, 56, 0046958019880696. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R. Heart disease and stroke statistics—2018 update: A report from the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef]
- National Cancer Institute. National Costs for Cancer Sites | Cancer Prevalence and Cost of Care Projections. Available online: https://costprojections.cancer.gov/expenditures.html (accessed on 3 March 2021).
- Leatherman, T. A Space of Vulnerability in Poverty and Health: Political-Ecology and Biocultural Analysis. Ethos 2005, 33, 46–70. [Google Scholar] [CrossRef]
- Quesada, J.; Hart, L.K.; Bourgois, P. Structural Vulnerability and Health: Latino Migrant Laborers in the United States. Med. Anthropol. 2011, 30, 339–362. [Google Scholar] [CrossRef] [Green Version]
- Price, J.H.; Khubchandani, J.; McKinney, M.; Braun, R. Racial/ethnic disparities in chronic diseases of youths and access to health care in the United States. Biomed Res. Int. 2013, 2013. [Google Scholar] [CrossRef] [Green Version]
- Pastor, M.; Morello-Frosch, R. Gaps Matter: Environment, Health, and Social Equity. Generations 2018, 42, 28–33. [Google Scholar]
- American Heart Association. Air Pollution and Heart Disease, Stroke. Available online: https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/air-pollution-and-heart-disease-stroke (accessed on 4 March 2021).
- Bhatnagar, A. Environmental Determinants of Cardiovascular Disease. Circ. Res. 2017, 121, 162–180. [Google Scholar] [CrossRef] [PubMed]
- Vienneau, D.; de Hoogh, K.; Faeh, D.; Kaufmann, M.; Wunderli, J.M.; Röösli, M. More than clean air and tranquillity: Residential green is independently associated with decreasing mortality. Environ. Int. 2017, 108, 176–184. [Google Scholar] [CrossRef]
- Erqou, S.; Clougherty, J.E.; Olafiranye, O.; Magnani, J.W.; Aiyer, A.; Tripathy, S.; Kinnee, E.; Kip, K.E.; Reis, S.E. Particulate matter air pollution and racial differences in cardiovascular disease risk. Arterioscler. Thromb. Vasc. Biol. 2018, 38, 935–942. [Google Scholar] [CrossRef] [Green Version]
- Jones, M.R.; Diez-Roux, A.V.; Hajat, A.; Kershaw, K.N.; O’Neill, M.S.; Guallar, E.; Post, W.S.; Kaufman, J.D.; Navas-Acien, A. Race/ethnicity, residential segregation, and exposure to ambient air pollution: The Multi-Ethnic Study of Atherosclerosis (MESA). Am. J. Public Health 2014, 104, 2130–2137. [Google Scholar] [CrossRef] [PubMed]
- Raaschou-Nielsen, O.; Reynolds, P. Air pollution and childhood cancer: A review of the epidemiological literature. Int. J. Cancer 2006, 118, 2920–2929. [Google Scholar] [CrossRef]
- Eckel, S.P.; Cockburn, M.; Shu, Y.-H.; Deng, H.; Lurmann, F.W.; Liu, L.; Gilliland, F.D. Air pollution affects lung cancer survival. Thorax 2016, 71, 891–898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linder, S.H.; Marko, D.; Ken, S. Cumulative cancer risk from air pollution in houston: Disparities in risk burden and social disadvantage. Environ. Sci. Technol. 2008, 42, 4312–4322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keramatinia, A.; Hassanipour, S.; Nazarzadeh, M.; Wurtz, M.; Monfared, A.B.; Khayyamzadeh, M.; Bidel, Z.; Mhrvar, N.; Mosavi-Jarrahi, A. Correlation between nitrogen dioxide as an air pollution indicator and breast cancer: A systematic review and meta-analysis. Asian Pac. J. Cancer Prev. 2016, 17, 419–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jackson, R.J. The impact of the built environment on health: An emerging field. Am. J. Public Health 2003, 93, 1382. [Google Scholar] [CrossRef] [PubMed]
- Gomez, S.L.; Shariff-Marco, S.; Derouen, M.; Keegan, T.H.M.; Yen, I.H.; Mujahid, M.; Satariano, W.A.; Glaser, S.L. The impact of neighborhood social and built environment factors across the cancer continuum: Current research, methodological considerations, and future directions. Cancer 2015, 121, 2314–2330. [Google Scholar] [CrossRef] [Green Version]
- Malambo, P.; Kengne, A.P.; De Villiers, A.; Lambert, E.V.; Puoane, T. Built environment, selected risk factors and major cardiovascular disease outcomes: A systematic review. PLoS ONE 2016, 11, e0166846. [Google Scholar] [CrossRef] [PubMed]
- Tamura, K.; Langerman, S.D.; Ceasar, J.N.; Andrews, M.R.; Agrawal, M.; Powell-Wiley, T.M. Neighborhood social environment and cardiovascular disease risk. Curr. Cardiovasc. Risk Rep. 2019, 13, 1–13. [Google Scholar] [CrossRef]
- Chow, C.K.; Lock, K.; Teo, K.; Subramanian, S.V.; McKee, M.; Yusuf, S. Environmental and societal influences acting on cardiovascular risk factors and disease at a population level: A review. Int. J. Epidemiol. 2009, 38, 1580–1594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elliott, M. The stress process in neighborhood context. Health Place 2000, 6, 287–299. [Google Scholar] [CrossRef]
- Matheson, F.I.; Moineddin, R.; Dunn, J.R.; Creatore, M.I.; Gozdyra, P.; Glazier, R.H. Urban neighborhoods, chronic stress, gender and depression. Soc. Sci. Med. 2006, 63, 2604–2616. [Google Scholar] [CrossRef]
- Evans, G.W.; Kim, P. Childhood poverty, chronic stress, self-regulation, and coping. Child Dev. Perspect. 2013, 7, 43–48. [Google Scholar] [CrossRef]
- Albert, M.A.; Durazo, E.M.; Slopen, N.; Zaslavsky, A.M.; Buring, J.E.; Silva, T.; Chasman, D.; Williams, D.R. Cumulative psychological stress and cardiovascular disease risk in middle aged and older women: Rationale, design, and baseline characteristics. Am. Heart J. 2017, 192, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Casagrande, S.S.; Whitt-Glover, M.C.; Lancaster, K.J.; Odoms-Young, A.M.; Gary, T.L. Built Environment and Health Behaviors Among African Americans: A Systematic Review. Am. J. Prev. Med. 2009, 36, 174–181. [Google Scholar] [CrossRef]
- Cohen, D.A.; Han, B.; Derose, K.P.; Williamson, S.; Marsh, T.; Rudick, J.; McKenzie, T.L. Neighborhood poverty, park use, and park-based physical activity in a Southern California city. Soc. Sci. Med. 2012, 75, 2317–2325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sallis, J.F.; Floyd, M.F.; Rodríguez, D.A.; Saelens, B.E. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation 2012, 125, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Weimann, H.; Rylander, L.; van den Bosch, M.A.; Albin, M.; Skärbäck, E.; Grahn, P.; Björk, J. Perception of safety is a prerequisite for the association between neighbourhood green qualities and physical activity: Results from a cross-sectional study in Sweden. Health Place 2017, 45, 124–130. [Google Scholar] [CrossRef]
- Janssen, I. Crime and perceptions of safety in the home neighborhood are independently associated with physical activity among 11–15 year olds. Prev. Med. (Balt.) 2014, 66, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Beilin, L.; Huang, R.-C. Childhood Obesity, Hypertension, the Metabolic Syndrome and Adult Cardiovascular Disease. Clin. Exp. Pharmacol. Physiol. 2008, 35, 409–411. [Google Scholar] [CrossRef] [PubMed]
- Van Emmerik, N.M.A.; Renders, C.M.; van de Veer, M.; van Buuren, S.; van der Baan-Slootweg, O.H.; Kist-van Holthe, J.E.; HiraSing, R.A. High cardiovascular risk in severely obese young children and adolescents. Arch. Dis. Child. 2012, 97, 818–821. [Google Scholar] [CrossRef] [Green Version]
- Sallis, J.F.; Slymen, D.J.; Conway, T.L.; Frank, L.D.; Saelens, B.E.; Cain, K.; Chapman, J.E. Income disparities in perceived neighborhood built and social environment attributes. Health Place 2011, 17, 1274–1283. [Google Scholar] [CrossRef]
- Geneau, R.; Stuckler, D.; Stachenko, S.; McKee, M.; Ebrahim, S.; Basu, S.; Chockalingham, A.; Mwatsama, M.; Jamal, R.; Alwan, A. Raising the priority of preventing chronic diseases: A political process. Lancet 2010, 376, 1689–1698. [Google Scholar] [CrossRef]
- Friel, S.; Hattersley, L.; Ford, L.; O’Rourke, K. Addressing inequities in healthy eating. Health Promot. Int. 2015, 30, ii77–ii88. [Google Scholar] [CrossRef] [Green Version]
- Kwarteng, J.L.; Beyer, K.M.M.; Banerjee, A.; Stolley, M.R. Facilitators of behavior change and weight loss in an intervention for African American Breast Cancer Survivors. Cancer Causes Control 2020, 31, 737–747. [Google Scholar] [CrossRef]
- Ball, K.; Carver, A.; Downing, K.; Jackson, M.; O’Rourke, K. Addressing the social determinants of inequities in physical activity and sedentary behaviours. Health Promot. Int. 2015, 30, ii8–ii19. [Google Scholar] [CrossRef] [Green Version]
- Suglia, S.F.; Shelton, R.C.; Hsiao, A.; Wang, Y.C.; Rundle, A.; Link, B.G. Why the neighborhood social environment is critical in obesity prevention. J. Urban Health 2016, 93, 206–212. [Google Scholar] [CrossRef] [Green Version]
- Doh, S. Health insurance and racial disparity in the United States. Int. Rev. Public Adm. 2012, 17, 79–103. [Google Scholar] [CrossRef]
- Carlisle, D.M.; Leake, B.D.; Shapiro, M.F. Racial and ethnic disparities in the use of cardiovascular procedures: Associations with type of health insurance. Am. J. Public Health 1997, 87, 263–267. [Google Scholar] [CrossRef] [Green Version]
- Buys, D.R.; Howard, V.J.; McClure, L.A.; Buys, K.C.; Sawyer, P.; Allman, R.M.; Levitan, E.B. Association between neighborhood disadvantage and hypertension prevalence, awareness, treatment, and control in older adults: Results from the University of Alabama at Birmingham Study of Aging. Am. J. Public Health 2015, 105, 1181–1188. [Google Scholar] [CrossRef]
- Rachele, J.N.; Giles-Corti, B.; Turrell, G. Neighbourhood disadvantage and self-reported type 2 diabetes, heart disease and comorbidity: A cross-sectional multilevel study. Ann. Epidemiol. 2016, 26, 146–150. [Google Scholar] [CrossRef]
- Xiao, Q.; Berrigan, D.; Powell-Wiley, T.M.; Matthews, C.E. Ten-year change in neighborhood socioeconomic deprivation and rates of Total, cardiovascular disease, and Cancer mortality in older US adults. Am. J. Epidemiol. 2018, 187, 2642–2650. [Google Scholar] [CrossRef]
- Namin, S.; Zhou, Y.; Neuner, J.; Beyer, K. The Role of Residential History in Cancer Research: A Scoping Review. Soc. Sci. Med. 2020, 270, 113657. [Google Scholar]
- Hiatt, R.A.; Breen, N. The social determinants of cancer: A challenge for transdisciplinary science. Am. J. Prev. Med. 2008, 35, S141–S150. [Google Scholar] [CrossRef] [PubMed]
- Conroy, S.M.; Shariff-Marco, S.; Koo, J.; Yang, J.; Keegan, T.H.M.; Sangaramoorthy, M.; Hertz, A.; Nelson, D.O.; Cockburn, M.; Satariano, W.A. Racial/ethnic differences in the impact of neighborhood social and built environment on breast cancer risk: The neighborhoods and breast cancer study. Cancer Epidemiol Biomark. Prev. 2017, 26, 541–552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurani, S.S.; McCoy, R.G.; Lampman, M.A.; Doubeni, C.A.; Finney Rutten, L.J.; Inselman, J.W.; Giblon, R.E.; Bunkers, K.S.; Stroebel, R.J.; Rushlow, D.; et al. Association of Neighborhood Measures of Social Determinants of Health With Breast, Cervical, and Colorectal Cancer Screening Rates in the US Midwest. JAMA Netw. Open 2020, 3, e200618. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.Z.; Phelan-Emrick, D.; Castillo-Salgado, C. Evaluating neighborhood correlates and geospatial distribution of breast, cervical, and colorectal cancer incidence. Front. Oncol. 2018, 8, 471. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N.; Quesenberry, C.J.; Peng, T.; Horn-Ross, P.; Stewart, S.; Brown, S.; Swallen, K.; Guillermo, T.; Suh, D.; Alvarez-Martinez, L.; et al. Social class, race/ethnicity, and incidence of breast, cervix, colon, lung, and prostate cancer among Asian, Black, Hispanic, and White residents of the San Francisco Bay Area, 1988-92 (United States). Cancer Causes Control 1999, 10, 525–537. [Google Scholar] [CrossRef]
- Gomez, S.L.; Glaser, S.L.; McClure, L.A.; Shema, S.J.; Kealey, M.; Keegan, T.H.M.; Satariano, W.A. The California Neighborhoods Data System: A new resource for examining the impact of neighborhood characteristics on cancer incidence and outcomes in populations. Cancer Causes Control 2011, 22, 631–647. [Google Scholar] [CrossRef] [Green Version]
- Hossain, F.; Danos, D.; Prakash, O.; Gilliland, A.; Ferguson, T.F.; Simonsen, N.; Leonardi, C.; Yu, Q.; Wu, X.-C.; Miele, L. Neighborhood social determinants of triple negative breast cancer. Front. Public Health 2019, 7, 18. [Google Scholar] [CrossRef]
- Gomez, S.L.; Press, D.J.; Lichtensztajn, D.; Keegan, T.H.M.; Shema, S.J.; Le, G.M.; Kurian, A.W. Patient, hospital, and neighborhood factors associated with treatment of early-stage breast cancer among Asian American women in California. Cancer Epidemiol. Biomark. Prev. 2012, 21, 821–834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polek, C.; Hardie, T.; Deatrick, J.A. Breast cancer survivorship experiences of urban Hispanic women. J. Cancer Educ. 2020, 35, 923–929. [Google Scholar] [CrossRef] [PubMed]
- Cheng, I.; Shariff-Marco, S.; Koo, J.; Monroe, K.R.; Yang, J.; John, E.M.; Kurian, A.W.; Kwan, M.L.; Henderson, B.E.; Bernstein, L.; et al. Contribution of the neighborhood environment and obesity to breast cancer survival: The California Breast Cancer Survivorship Consortium. Cancer Epidemiol. Biomark. Prev. 2015, 24, 1282–1290. [Google Scholar] [CrossRef] [Green Version]
- Collin, L.J.; Gaglioti, A.H.; Beyer, K.M.; Zhou, Y.; Moore, M.A.; Nash, R.; Switchenko, J.M.; Miller-Kleinhenz, J.M.; Ward, K.C.; McCullough, L.E. Neighborhood-level redlining and lending bias are associated with breast cancer mortality in a large and diverse metropolitan area. Cancer Epidemiol. Prev. Biomark. 2021, 30, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Fleisch Marcus, A.; Illescas, A.H.; Hohl, B.C.; Llanos, A.A.M. Relationships between social isolation, neighborhood poverty, and cancer mortality in a population-based study of US adults. PLoS ONE 2017, 12, e0173370. [Google Scholar] [CrossRef] [Green Version]
- Holtgrave, D.R.; Barranco, M.A.; Tesoriero, J.M.; Blog, D.S.; Rosenberg, E.S. Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State. Ann. Epidemiol. 2020, 48, 9–14. [Google Scholar] [CrossRef] [PubMed]
- US Center for Disease Control. Disparities in COVID-19 Deaths. Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-deaths.html (accessed on 21 January 2021).
- Holmes, L.; Enwere, M.; Williams, J.; Ogundele, B.; Chavan, P.; Piccoli, T.; Chinaka, C.; Comeaux, C.; Pelaez, L.; Okundaye, O.; et al. Black—White Risk Differentials in COVID-19 (SARS-COV2) Transmission, Mortality and Case Fatality in the United States: Translational Epidemiologic Perspective and Challenges. Int. J. Environ. Res. Public Health 2020, 17, 4322. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, U.V.; Larkins-Pettigrew, M. Racial demographics and COVID-19 confirmed cases and deaths: A correlational analysis of 2886 US counties. J. Public Health (Bangk.) 2020, 42, 445–447. [Google Scholar] [CrossRef] [PubMed]
- Savitt, T. Abraham Flexner and the black medical schools. 1992. J. Natl. Med. Assoc. 2006, 98, 1415. [Google Scholar]
- Ly, D.P. Historical Trends in the Representativeness and Incomes of Black Physicians, 1900–2018. J. Gen. Intern. Med. 2021, 1–3. [Google Scholar]
- Bulatao, R.A.; Anderson, N.B. Understanding racial and ethnic differences in health in late life: A research agenda; National Academies Press: Washington, DC, USA, 2004; ISBN 0309092477. [Google Scholar]
- Nelson, A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. J. Natl. Med. Assoc. 2002, 94, 666. [Google Scholar]
- Alsan Owen Garrick Grant Graziani, M.C.; Bulow, J.; Casey, K.; Chandrasekhar, A.; Chetty, R.; DellaVigna, S.; Duggan, M.; Eggleston, K.; Field, E.; Gentzkow, M.; et al. Does Diversity Matter for Health?Experimental Evidence from Oakland. Am. Econ. Rev. 2018, 109, 4071–4111. [Google Scholar]
- Beech, B.M.; Calles-Escandon, J.; Hairston, K.G.; Langdon, M.S.E.; Latham-Sadler, B.A.; Bell, R.A. Mentoring programs for underrepresented minority faculty in academic medical centers: A systematic review of the literature. Acad. Med. J. Assoc. Am. Med. Coll. 2013, 88. [Google Scholar] [CrossRef] [Green Version]
- Manzanedo, R.D.; Manning, P. COVID-19: Lessons for the climate change emergency. Sci. Total Environ. 2020, 742, 140563. [Google Scholar] [CrossRef]
- Wendelboe-Nelson, C.; Kelly, S.; Kennedy, M.; Cherrie, J.W. A scoping review mapping research on green space and associated mental health benefits. Int. J. Environ. Res. Public Health 2019, 16, 2081. [Google Scholar] [CrossRef] [Green Version]
- Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. 2018, 166, 628–637. [Google Scholar] [CrossRef]
- Kondo, M.C.; Fluehr, J.M.; McKeon, T.; Branas, C.C. Urban green space and its impact on human health. Int. J. Environ. Res. Public Health 2018, 15, 445. [Google Scholar] [CrossRef] [Green Version]
- James, P.; Banay, R.F.; Hart, J.E.; Laden, F. A Review of the Health Benefits of Greenness. Curr. Epidemiol. Rep. 2015, 2, 131–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shoari, N.; Ezzati, M.; Baumgartner, J.; Malacarne, D.; Fecht, D. Accessibility and allocation of public parks and gardens in England and Wales: A COVID-19 social distancing perspective. PLoS ONE 2020, 15, e0241102. [Google Scholar] [CrossRef] [PubMed]
- Courtemanche, C.; Garuccio, J.; Le, A.; Pinkston, J.; Yelowitz, A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Aff. 2020, 39, 1237–1246. [Google Scholar] [CrossRef]
- Venter, Z.S.; Barton, D.N.; Gundersen, V.; Figari, H. Urban nature in a time of crisis: Recreational use of green space increases during the COVID-19 outbreak in Oslo, Norway. Environ. Res. Lett. 2020, 15, 104075. [Google Scholar] [CrossRef]
- Wray, A.; Martin, G.; Ostermeier, E.; Medeiros, A.; Little, M.; Reilly, K.; Gilliland, J. Evidence synthesis-Physical activity and social connectedness interventions in outdoor spaces among children and youth: A rapid review. Health Promot. Chronic Dis. Prev. Can. Res. Policy Pract. 2020, 40, 104. [Google Scholar]
- Freeman, S.; Eykelbosh, A. COVID-19 and Outdoor Safety: Considerations for Use of Outdoor Recreational Spaces. Available online: https://ncceh.ca/sites/default/files/COVID-19%20Outdoor%20Safety%20-%20April%2016%202020.pdf (accessed on 4 May 2020).
- Weed, M.; Foad, A. Rapid Scoping Review of Evidence of Outdoor Transmission of COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Leclerc, Q.J.; Fuller, N.M.; Knight, L.E.; Funk, S.; Knight, G.M. What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Res. 2020, 5, 83. [Google Scholar] [CrossRef]
- Egli, V.; Oliver, M.; Tautolo, E.-S. The development of a model of community garden benefits to wellbeing. Prev. Med. Rep. 2016, 3, 348–352. [Google Scholar] [CrossRef] [Green Version]
- Veen, E.J. Community gardens in urban areas: A critical reflection on the extent to which they strenghten social cohesion and provide alternative food. PhD Thesis, Wageningen University, Wageningen, The Netherlands, 2015. [Google Scholar]
- ‘Yotti’Kingsley, J.; Townsend, M. ‘Dig in’to social capital: Community gardens as mechanisms for growing urban social connectedness. Urban Policy Res. 2006, 24, 525–537. [Google Scholar] [CrossRef]
- Saldivar-Tanaka, L.; Krasny, M.E. Culturing community development, neighborhood open space, and civic agriculture: The case of Latino community gardens in New York City. Agric. Hum. Values 2004, 21, 399–412. [Google Scholar] [CrossRef]
- Graham, S.; Connell, J. Nurturing relationships: The gardens of Greek and Vietnamese migrants in Marrickville, Sydney. Aust. Geogr. 2006, 37, 375–393. [Google Scholar] [CrossRef]
- McCabe, A. Community gardens to fight urban youth crime and stabilize neighborhoods. Int. J. Child Health Hum. Dev. 2014, 7, 223–236. [Google Scholar]
- Branas, C.C.; Cheney, R.A.; MacDonald, J.M.; Tam, V.W.; Jackson, T.D.; Ten Have, T.R. A difference-in-differences analysis of health, safety, and greening vacant urban space. Am. J. Epidemiol. 2011, 174, 1296–1306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kondo, M.C.; Han, S.H.; Donovan, G.H.; MacDonald, J.M. The association between urban trees and crime: Evidence from the spread of the emerald ash borer in Cincinnati. Landsc. Urban Plan. 2017, 157, 193–199. [Google Scholar] [CrossRef] [Green Version]
- Kondo, M.; Hohl, B.; Han, S.; Branas, C. Effects of greening and community reuse of vacant lots on crime. Urban Stud. 2016, 53, 3279–3295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Younan, D.; Tuvblad, C.; Li, L.; Wu, J.; Lurmann, F.; Franklin, M.; Berhane, K.; McConnell, R.; Wu, A.H.; Baker, L.A. Environmental determinants of aggression in adolescents: Role of urban neighborhood greenspace. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 591–601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez, B.; Kennedy, C.; McPhearson, T. Parks are Critical Urban Infrastructure: Perception and Use of Urban Green Spaces in NYC During COVID-19. Preprints 2020. [Google Scholar] [CrossRef]
- Aram, F.; Solgi, E.; Holden, G. The role of green spaces in increasing social interactions in neighborhoods with periodic markets. Habitat Int. 2019, 84, 24–32. [Google Scholar] [CrossRef]
- Sugiyama, T.; Carver, A.; Koohsari, M.J.; Veitch, J. Advantages of public green spaces in enhancing population health. Landsc. Urban Plan. 2018, 178, 12–17. [Google Scholar] [CrossRef]
- Wisconsin Department of Natural Resources. Find Your Adventure, Go Wild In Wisconsin. Available online: https://dnr.wisconsin.gov/newsroom/release/37751 (accessed on 18 May 2021).
- Coyle, K.J.; Bodor, S. North American Association for Environmental Education and National Wildlife Federation: Guide to Advocating for Outdoor Classrooms in Coronavirus-Era School Reopening Guide to Advocating for Outdoor Classrooms in Coronavirus-era School Reopening. Available online: https://naaee.org/eepro/resources/guide-advocating-outdoor-classrooms (accessed on 10 February 2021).
- US Center for Disease Control. Considerations for Outdoor Learning Gardens and Community Gardens. Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/outdoor-garden.html (accessed on 10 February 2021).
- Leavell, M.A.; Leiferman, J.A.; Gascon, M.; Braddick, F.; Gonzalez, J.C.; Litt, J.S. Nature-based social prescribing in urban settings to improve social connectedness and mental well-being: A review. Curr. Environ. Health Rep. 2019, 6, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, S.-A. Children in the Outdoors: A literature review. Available online: http://www.ltl.org.uk/wp-content/uploads/2019/02/children-in-the-outdoors.pdf (accessed on 5 March 2021).
- Bikomeye, J.; Balza, J.; Beyer, K. The Impact of Schoolyard Greening on Children’s Physical Activity and Socioemotional Health: A Systematic Review of Experimental Studies. Int. J. Environ. Res. Public Health 2021, 18, 535. [Google Scholar] [CrossRef] [PubMed]
- Jennings, V.; Bamkole, O. The relationship between social cohesion and urban green space: An avenue for health promotion. Int. J. Environ. Res. Public Health 2019, 16, 452. [Google Scholar] [CrossRef] [Green Version]
- Berkman, L.F. Social support, social networks, social cohesion and health. Soc. Work Health Care 2000, 31, 3–14. [Google Scholar] [CrossRef]
- Kim, E.S.; Hawes, A.M.; Smith, J. Perceived neighbourhood social cohesion and myocardial infarction. J. Epidemiol. Community. Health 2014, 68, 1020–1026. [Google Scholar] [CrossRef] [Green Version]
- McEachan, R.R.C.; Prady, S.L.; Smith, G.; Fairley, L.; Cabieses, B.; Gidlow, C.; Wright, J.; Dadvand, P.; Van Gent, D.; Nieuwenhuijsen, M.J. The association between green space and depressive symptoms in pregnant women: Moderating roles of socioeconomic status and physical activity. J. Epidemiol. Community. Health 2016, 70, 253–259. [Google Scholar] [CrossRef] [Green Version]
- Beyer, K.M.M.; Kaltenbach, A.; Szabo, A.; Bogar, S.; Nieto, F.J.; Malecki, K.M. Exposure to neighborhood green space and mental health: Evidence from the survey of the health of Wisconsin. Int. J. Environ. Res. Public Health 2014, 11, 3453–3472. [Google Scholar] [CrossRef] [Green Version]
- Roe, J.J.; Thompson, C.W.; Aspinall, P.A.; Brewer, M.J.; Duff, E.I.; Miller, D.; Mitchell, R.; Clow, A. Green space and stress: Evidence from cortisol measures in deprived urban communities. Int. J. Environ. Res. Public Health 2013, 10, 4086–4103. [Google Scholar] [CrossRef] [Green Version]
- Ward Thompson, C.; Roe, J.; Aspinall, P.; Mitchell, R.; Clow, A.; Miller, D. More green space is linked to less stress in deprived communities: Evidence from salivary cortisol patterns. Landsc. Urban Plan. 2012, 105, 221–229. [Google Scholar] [CrossRef] [Green Version]
- Mayer, F.S.; Frantz, C.M.; Bruehlman-Senecal, E.; Dolliver, K. Why is nature beneficial? The role of connectedness to nature. Environ. Behav. 2009, 41, 607–643. [Google Scholar] [CrossRef]
- Gidlow, C.J.; Jones, M.V.; Hurst, G.; Masterson, D.; Clark-Carter, D.; Tarvainen, M.P.; Smith, G.; Nieuwenhuijsen, M. Where to put your best foot forward: Psycho-physiological responses to walking in natural and urban environments. J. Environ. Psychol. 2016, 45, 22–29. [Google Scholar] [CrossRef]
- Song, C.; Ikei, H.; Igarashi, M.; Takagaki, M.; Miyazaki, Y. Physiological and psychological effects of a walk in urban parks in fall. Int. J. Environ. Res. Public Health 2015, 12, 14216–14228. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Nieuwenhuijsen, M.J.; Esnaola, M.; Forns, J.; Basagaña, X.; Alvarez-Pedrerol, M.; Rivas, I.; López-Vicente, M.; De Castro Pascual, M.; Su, J.; et al. Green spaces and cognitive development in primary schoolchildren. Proc. Natl. Acad. Sci. USA 2015, 112, 7937–7942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, G.; Zhang, Y.; Zhao, J.; Zhang, J.; Jiang, F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020, 395, 945–947. [Google Scholar] [CrossRef]
- Lakhan, R.; Agrawal, A.; Sharma, M. Prevalence of Depression, Anxiety, and Stress during COVID-19 Pandemic. J. Neurosci. Rural Pract. 2020, 11, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020. [Google Scholar] [CrossRef]
- Giorgi, G.; Lecca, L.I.; Alessio, F.; Finstad, G.L.; Bondanini, G.; Lulli, L.G.; Arcangeli, G.; Mucci, N. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 7857. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020, 52, 102066. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef]
- Ramadhan, M.H.A.; Putri, A.K.; Melinda, D.; Habibah, U.; Fajriyah, U.N.; Aini, S.; Prananjaya, B.A.; Ikhsan, D.S. Children’s Mental Health in the Time of COVID-19: How Things Stand and the Aftermath. Malays. J. Med. Sci. 2020, 27, 196–201. [Google Scholar] [CrossRef]
- Kessler Psychological Distress Scale (K10 Scale). Available online: https://www.tac.vic.gov.au/files-to-move/media/upload/k10_english.pdf (accessed on 3 April 2021).
- Wang, Z.; Wang, W. An Empirical Study On the Impact of Green Spaces in Residential Areas on the Mental Health of Residents Under Covid-19. Landsc. Archit. Front. 2021, 8, 46–59. [Google Scholar]
- Maes, S.; Leventhal, H.; de Ridder, D.T.D. Coping with chronic diseases. In Handbook of Coping: Theory, Research, Applications; John Wiley & Sons: Hoboken, NJ, USA, 1996. [Google Scholar]
- Paradies, Y. A review of psychosocial stress and chronic disease for 4th world indigenous peoples and African Americans. Ethn. Dis. 2006, 16, 295. [Google Scholar] [PubMed]
- Riggs, D.W.; Yeager, R.; Conklin, D.J.; De Jarnett, N.; Keith, R.J.; De Filippis, A.P.; Rai, S.N.; Bhatnagar, A. Residential proximity to greenness mitigates the hemodynamic effects of ambient air pollution. Am. J. Physiol. Circ. Physiol. 2021, 320, H1102–H1111. [Google Scholar] [CrossRef]
- Smith, J.E.; Richardson, J.; Hoffman, C.; Pilkington, K. Mindfulness-Based Stress Reduction as supportive therapy in cancer care: Systematic review. J. Adv. Nurs. 2005, 52, 315–327. [Google Scholar] [CrossRef]
- Ledesma, D.; Kumano, H. Mindfulness-based stress reduction and cancer: A meta-analysis. Psycho Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2009, 18, 571–579. [Google Scholar] [CrossRef]
- Tacón, A.M.; Caldera, Y.M.; Ronaghan, C. Mindfulness-Based Stress Reduction in women with breast cancer. Fam. Syst. Health 2004, 22, 193. [Google Scholar] [CrossRef]
- Musial, F.; Büssing, A.; Heusser, P.; Choi, K.-E.; Ostermann, T. Mindfulness-based stress reduction for integrative cancer care—A summary of evidence. Complement. Med. Res. 2011, 18, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Carlson, L.E.; Speca, M.; Patel, K.D.; Goodey, E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom. Med. 2003, 65, 571–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zainal, N.Z.; Booth, S.; Huppert, F.A. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: A meta-analysis. Psycho. Oncol. 2013, 22, 1457–1465. [Google Scholar] [CrossRef]
- Carlson, L.E.; Ursuliak, Z.; Goodey, E.; Angen, M.; Speca, M. The effects of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients: 6-month follow-up. Support. Care Cancer 2001, 9, 112–123. [Google Scholar] [CrossRef]
- Schell, L.K.; Monsef, I.; Woeckel, A.; Skoetz, N. Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef]
- Schneider, R.H.; Alexander, C.N.; Salerno, J.; Rainforth, M.; Nidich, S. Stress reduction in the prevention and treatment of cardiovascular disease in African Americans: A review of controlled research on the Transcendental Meditation Program. J. Soc. Behav. Pers. 2005, 17, 159. [Google Scholar]
- Rainforth, M.V.; Schneider, R.H.; Nidich, S.I.; Gaylord-King, C.; Salerno, J.W.; Anderson, J.W. Stress reduction programs in patients with elevated blood pressure: A systematic review and meta-analysis. Curr. Hypertens. Rep. 2007, 9, 520. [Google Scholar] [CrossRef]
- Schneider, R.H.; Grim, C.E.; Rainforth, M.V.; Kotchen, T.; Nidich, S.I.; Gaylord-King, C.; Salerno, J.W.; Kotchen, J.M.; Alexander, C.N. Stress reduction in the secondary prevention of cardiovascular disease: Randomized, controlled trial of transcendental meditation and health education in Blacks. Circ. Cardiovasc. Qual. Outcomes 2012, 5, 750–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sellers, C.E.; Grant, P.M.; Ryan, C.G.; O’Kane, C.; Raw, K.; Conn, D. Take a walk in the park? A cross-over pilot trial comparing brisk walking in two different environments: Park and urban. Prev. Med. (Balt.) 2012, 55, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Almanza, E.; Jerrett, M.; Dunton, G.; Seto, E.; Ann Pentz, M. A study of community design, greenness, and physical activity in children using satellite, GPS and accelerometer data. Health Place 2012, 18, 46–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oreskovic, N.M.; Perrin, J.M.; Robinson, A.I.; Locascio, J.J.; Blossom, J.; Chen, M.L.; Winickoff, J.P.; Field, A.E.; Green, C.; Goodman, E. Adolescents’ use of the built environment for physical activity. BMC Public Health 2015, 15, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Rodríguez, D.A.; Cho, G.-H.; Evenson, K.R.; Conway, T.L.; Cohen, D.; Ghosh-Dastidar, B.; Pickrel, J.L.; Veblen-Mortenson, S.; Lytle, L.A. Out and about: Association of the built environment with physical activity behaviors of adolescent females. Health Place 2012, 18, 55–62. [Google Scholar] [CrossRef] [Green Version]
- Tsai, W.-L.; Yngve, L.; Zhou, Y.; Beyer, K.M.M.; Bersch, A.; Malecki, K.M.; Jackson, L.E. Street-level neighborhood greenery linked to active transportation: A case study in Milwaukee and Green Bay, WI, USA. Landsc. Urban Plan. 2019, 191, 103619. [Google Scholar] [CrossRef]
- Seo, S.; Choi, S.; Kim, K.; Kim, S.M.; Park, S.M. Association between urban green space and the risk of cardiovascular disease: A longitudinal study in seven Korean metropolitan areas. Environ. Int. 2019, 125, 51–57. [Google Scholar] [CrossRef]
- Dalton, A.M.; Jones, A.P. Residential neighbourhood greenspace is associated with reduced risk of cardiovascular disease: A prospective cohort study. PLoS ONE 2020. [Google Scholar] [CrossRef] [Green Version]
- Gascon, M.; Triguero-Mas, M.; Martínez, D.; Dadvand, P.; Rojas-Rueda, D.; Plasència, A.; Nieuwenhuijsen, M.J.; Martinez, D.; Dadvand, P.; Rojas-Rueda, D.; et al. Residential green spaces and mortality: A systematic review. Environ. Int. 2016, 86, 60–67. [Google Scholar] [CrossRef] [Green Version]
- Wilker, E.H.; Wu, C.-D.; McNeely, E.; Mostofsky, E.; Spengler, J.; Wellenius, G.A.; Mittleman, M.A. Green space and mortality following ischemic stroke. Environ. Res. 2014, 133, 42–48. [Google Scholar] [CrossRef] [Green Version]
- Da Silveira, I.H.; Junger, W.L. Green spaces and mortality due to cardiovascular diseases in the city of Rio de Janeiro. Rev. Saude Publica 2018, 52, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Crouse, D.L.; Pinault, L.; Balram, A.; Hystad, P.; Peters, P.A.; Chen, H.; van Donkelaar, A.; Martin, R.V.; Ménard, R.; Robichaud, A. Urban greenness and mortality in Canada’s largest cities: A national cohort study. Lancet Planet. Health 2017, 1, e289–e297. [Google Scholar] [CrossRef]
- Song, C.; Ikei, H.; Igarashi, M.; Miwa, M.; Takagaki, M.; Miyazaki, Y. Physiological and psychological responses of young males during spring-time walks in urban parks. J. Physiol. Anthropol. 2014, 33, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitchell, R.; Popham, F. Effect of exposure to natural environment on health inequalities: An observational population study. Lancet 2008, 372, 1655–1660. [Google Scholar] [CrossRef] [Green Version]
- Sugiyama, T.; Villanueva, K.; Knuiman, M.; Francis, J.; Foster, S.; Wood, L.; Giles-Corti, B. Can neighborhood green space mitigate health inequalities? A study of socio-economic status and mental health. Health Place 2016, 38, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Crawford, D.; Timperio, A.; Giles-Corti, B.; Ball, K.; Hume, C.; Roberts, R.; Andrianopoulos, N.; Salmon, J. Do features of public open spaces vary according to neighbourhood socio-economic status? Health Place 2008, 14, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Astell-Burt, T.; Feng, X.; Mavoa, S.; Badland, H.M.; Giles-Corti, B. Do low-income neighbourhoods have the least green space? A cross-sectional study of Australia’s most populous cities. BMC Public Health 2014, 14, 292. [Google Scholar] [CrossRef] [PubMed]
- Wen, M.; Zhang, X.; Harris, C.D.; Holt, J.B.; Croft, J.B. Spatial disparities in the distribution of parks and green spaces in the USA. Ann. Behav. Med. 2013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mouratidis, K. The impact of urban tree cover on perceived safety. Urban For. Urban Green. 2019, 44, 126434. [Google Scholar] [CrossRef]
- Dai, D. Racial/ethnic and socioeconomic disparities in urban green space accessibility: Where to intervene? Landsc. Urban Plan. 2011, 102, 234–244. [Google Scholar] [CrossRef]
- Beyer, K.M.M.; Zhou, Y.; Matthews, K.; Bemanian, A.; Laud, P.W.; Nattinger, A.B. New spatially continuous indices of redlining and racial bias in mortgage lending: Links to survival after breast cancer diagnosis and implications for health disparities research. Health Place 2016, 40, 34–43. [Google Scholar] [CrossRef]
- Wolf, K.L. The Municipality. Arborist News 2007, 16, 34–36. Available online: https://www.lwm-info.org/DocumentCenter/View/4597/2-21-The-Municipality-Economic-Development (accessed on 3 February 2021).
- Anderson, L.M.; Cordell, H.K. Residential property values improved by landscaping with trees. South. J. Appl. For. 1985, 9, 162–166. [Google Scholar] [CrossRef]
- Anderson, L.M.; Cordell, H.K. Influence of trees on residential property values in Athens, Georgia (USA): A survey based on actual sales prices. Landsc. Urban Plan. 1988, 15, 153–164. [Google Scholar] [CrossRef]
- Pandit, R.; Polyakov, M.; Tapsuwan, S.; Moran, T. The effect of street trees on property value in Perth, Western Australia. Landsc. Urban Plan. 2013, 110, 134–142. [Google Scholar] [CrossRef]
- Soares, A.L.; Rego, F.C.; McPherson, E.G.; Simpson, J.R.; Peper, P.J.; Xiao, Q. Benefits and costs of street trees in Lisbon, Portugal. Urban For. Urban Green. 2011, 10, 69–78. [Google Scholar] [CrossRef]
- Dimke, K.C.; Sydnor, T.D.; Gardner, D.S. The effect of landscape trees on residential property values of six communities in Cincinnati, Ohio. Arboric. Urban For. 2013, 39, 49–55. [Google Scholar]
- Deschane, J. The Municipality | Spring: Time for Economic Thaw 7 Discretionary Immunity in Slip and Fall Case. Available online: https://lwm-info.org/DocumentCenter/View/4597/2-21-The-Municipality-Economic-Development (accessed on 1 March 2021).
- Moran, D.; Turner, J. Turning over a new leaf: The health-enabling capacities of nature contact in prison. Soc. Sci. Med. 2019, 231, 62–69. [Google Scholar] [CrossRef] [PubMed]
- World Prison Brief Highest to Lowest - Prison Population Total. Available online: https://www.prisonstudies.org/highest-to-lowest/prison-population-total?field_region_taxonomy_tid=All (accessed on 3 April 2021).
- Dowell, E.K.P. Health Care Still Largest U.S. Employer. Available online: https://www.census.gov/library/stories/2020/10/health-care-still-largest-united-states-employer.html (accessed on 3 April 2021).
- Roger, S. Ulrich Effects of Gardens on Health Outcomes: Theory and Research. Available online: http://illinois-online.org/krassa/hdes598/Readings/Effects%20of%20Gardens%20on%20Health%20Outcomes.pdf (accessed on 3 April 2021).
- Association of American Medical Colleges. Hospital Roof Gardens Soothe Patients and Staff. Available online: https://www.aamc.org/news-insights/hospital-roof-gardens-soothe-patients-and-staff (accessed on 3 April 2021).
- Weerasuriya, R.; Henderson-Wilson, C.; Townsend, M. Accessing green spaces within a healthcare setting: A mixed studies review of barriers and facilitators. HERD Health Environ. Res. Des. J. 2019, 12, 119–140. [Google Scholar] [CrossRef] [PubMed]
- Naushad, V.A.; Bierens, J.J.L.M.; Nishan, K.P.; Firjeeth, C.P.; Mohammad, O.H.; Maliyakkal, A.M.; ChaliHadan, S.; Schreiber, M.D. A systematic review of the impact of disaster on the mental health of medical responders. Prehosp. Disaster Med. 2019, 34, 632–643. [Google Scholar] [CrossRef]
- George, D.R.; Rovniak, L.S.; Kraschnewski, J.L.; Hanson, R.; Sciamanna, C.N. A growing opportunity: Community gardens affiliated with US hospitals and academic health centers. Prev. Med. Rep. 2015, 2, 35–39. [Google Scholar] [CrossRef] [Green Version]
- Moore, E.O. Prison Environment’S Effect on Health Care Service Demands. J. Environ. Syst. 1981, 11, 17–34. [Google Scholar] [CrossRef]
- Nadkarni, N.M.; Hasbach, P.H.; Thys, T.; Crockett, E.G.; Schnacker, L. Impacts of nature imagery on people in severely nature-deprived environments. Front. Ecol. Environ. 2017, 15, 395–403. [Google Scholar] [CrossRef]
- Van der Linden, S. Green prison programmes, recidivism and mental health: A primer. Crim. Behav. Ment. Health 2015, 25, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Bhuller, M.; Dahl, G.B.; Løken, K.V.; Mogstad, M. Incarceration, Recidivism and Employment. Available online: http://www.nber.org/papers/w22648 (accessed on 3 April 2021).
- Bogar, S.; Beyer, K. Green Space, Violence, and Crime: A Systematic Review. Trauma. Violence Abus. 2015, 17. [Google Scholar] [CrossRef]
- Brink, L.A.; Nigg, C.R.; Lampe, S.M.R.; Kingston, B.A.; Mootz, A.L.; Van Vliet, W. Influence of schoolyard renovations on children’s physical activity: The learning landscapes program. Am. J. Public Health 2010, 100, 1672–1678. [Google Scholar] [CrossRef]
- Hamer, M.; Aggio, D.; Knock, G.; Kipps, C.; Shankar, A.; Smith, L. Effect of major school playground reconstruction on physical activity and sedentary behaviour: Camden active spaces. BMC Public Health 2017. [Google Scholar] [CrossRef] [Green Version]
- Wallner, P.; Kundi, M.; Arnberger, A.; Eder, R.; Allex, B.; Weitensfelder, L.; Hutter, H.P. Reloading pupils’ batteries: Impact of green spaces on cognition and wellbeing. Int. J. Environ. Res. Public Health 2018, 15, 1205. [Google Scholar] [CrossRef] [Green Version]
- Kelz, C.; Evans, G.W.; Röderer, K. The Restorative Effects of Redesigning the Schoolyard: A Multi-Methodological, Quasi-Experimental Study in Rural Austrian Middle Schools. Environ. Behav. 2015, 47, 119–139. [Google Scholar] [CrossRef] [Green Version]
- Van Dijk-Wesselius, J.E.; Maas, J.; Hovinga, D.; van Vugt, M.; van den Berg, A.E. The impact of greening schoolyards on the appreciation, and physical, cognitive and social-emotional well-being of schoolchildren: A prospective intervention study. Landsc. Urban Plan. 2018, 180, 15–26. [Google Scholar] [CrossRef]
- Raney, M.A.; Hendry, C.F.; Yee, S.A. Physical Activity and Social Behaviors of Urban Children in Green Playgrounds. Am. J. Prev. Med. 2019, 56, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Goran, M.I.; Ball, G.D.C.; Cruz, M.L. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J. Clin. Endocrinol. Metab. 2003, 88, 1417–1427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guillaume, M.; Lapidus, L.; Björntorp, P.; Lambert, A. Physical activity, obesity, and cardiovascular risk factors in children. The Belgian Luxembourg Child Study II. Obes. Res. 1997, 5, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Goran, M.I.; Reynolds, K.D.; Lindquist, C.H. Role of physical activity in the prevention of obesity in children. Int. J. Obes. 1999, 23, S18–S33. [Google Scholar] [CrossRef] [Green Version]
- Hills, A.P.; Andersen, L.B.; Byrne, N.M. Physical activity and obesity in children. Br. J. Sports Med. 2011, 45, 866–870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodney, J.P.; Maddock, J.E. HHS Public Access. Physiol. Behav. 2017, 176, 139–148. [Google Scholar] [CrossRef]
- Korczak, D.J.; Madigan, S.; Colasanto, M. Children’s physical activity and depression: A meta-analysis. Pediatrics 2017, 139, e20162266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biddle, S.J.H.; Asare, M. Physical activity and mental health in children and adolescents: A review of reviews. Br. J. Sports Med. 2011, 45, 886–895. [Google Scholar] [CrossRef] [Green Version]
- Bates, C.R.; Bohnert, A.M.; Gerstein, D.E. Green Schoolyards in Low-Income Urban Neighborhoods: Natural Spaces for Positive Youth Development Outcomes. Front. Psychol. 2018, 9, 805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beyer, K.; Bizub, J.; Szabo, A.; Heller, B.; Kistner, A.; Shawgo, E.; Zetts, C. Development and validation of the attitudes toward outdoor play scales for children. Soc. Sci. Med. 2015, 133, 253–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deb, A.; Kanungo, S.; Deb, M.; Nair, G. Impact of climate change on health and strategies for mitigation and adaptation. WHO South East Asia J. Public Health 2012, 1, 8. [Google Scholar] [CrossRef] [PubMed]
- US Environmental Protection Agency. Reduce Urban Heat Island Effect | Green Infrastructure|US EPA. Available online: https://www.epa.gov/green-infrastructure/reduce-urban-heat-island-effect (accessed on 27 November 2020).
- Dadvand, P.; Rivas, I.; Basagaña, X.; Alvarez-Pedrerol, M.; Su, J.; De Castro Pascual, M.; Amato, F.; Jerret, M.; Querol, X.; Sunyer, J.; et al. The association between greenness and traffic-related air pollution at schools. Sci. Total Environ. 2015, 523, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Nurse, J.; Basher, D.; Bone, A.; Bird, W. An ecological approach to promoting population mental health and well-being—a response to the challenge of climate change. Perspect. Public Health 2010, 130, 27–33. [Google Scholar] [CrossRef] [PubMed]
- US Environmental Protection Agency. Using Green Roofs to Reduce Heat Islands | Heat Island Effect. Available online: https://www.epa.gov/heatislands/using-green-roofs-reduce-heat-islands (accessed on 3 April 2021).
- Sailor, D.J.; Elley, T.B.; Gibson, M. Exploring the building energy impacts of green roof design decisions-a modeling study of buildings in four distinct climates. J. Build. Phys. 2012, 35, 372–391. [Google Scholar] [CrossRef]
- Stoltz, J.; Schaffer, C. Salutogenic Affordances and Sustainability: Multiple Benefits With Edible Forest Gardens in Urban Green Spaces. Front. Psychol. 2018, 9, 2344. [Google Scholar] [CrossRef]
- Litt, J.S.; Soobader, M.J.; Turbin, M.S.; Hale, J.W.; Buchenau, M.; Marshall, J.A. The influence of social involvement, neighborhood aesthetics, and community garden participation on fruit and vegetable consumption. Am. J. Public Health 2011, 101, 1466–1473. [Google Scholar] [CrossRef]
- Alaimo, K.; Packnett, E.; Miles, R.A.; Kruger, D.J. Fruit and vegetable intake among urban community gardeners. J. Nutr. Educ. Behav. 2008, 40, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Hanbazaza, M.A.; Triador, L.; Ball, G.D.C.; Farmer, A.; Maximova, K.; Nation, A.F.; Willows, N.D. The impact of school gardening on Cree children’s knowledge and attitudes toward vegetables and fruit. Can. J. Diet. Pract. Res. 2015, 76, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.; Balk, E.M.; Brendel, M.; Ip, S.; Lau, J.; Lee, J.; Lichtenstein, A.; Patel, K.; Raman, G.; Tatsioni, A. Vitamin D and calcium: A systematic review of health outcomes. Evid. Rep. Technol. Assess (Full Rep.) 2009, 183, 1–420. [Google Scholar]
- Veronese, N.; Solmi, M.; Caruso, M.G.; Giannelli, G.; Osella, A.R.; Evangelou, E.; Maggi, S.; Fontana, L.; Stubbs, B.; Tzoulaki, I. Dietary fiber and health outcomes: An umbrella review of systematic reviews and meta-analyses. Am. J. Clin. Nutr. 2018, 107, 436–444. [Google Scholar] [CrossRef] [Green Version]
- Malberg Dyg, P.; Christensen, S.; Peterson, C.J. Community gardens and wellbeing amongst vulnerable populations: A thematic review. Health Promot. Int. 2020, 35, 790–803. [Google Scholar] [CrossRef]
- Frumkin, H.; Bratman, G.N.; Breslow, S.J.; Cochran, B.; Kahn, P.H., Jr.; Lawler, J.J.; Levin, P.S.; Tandon, P.S.; Varanasi, U.; Wolf, K.L.; et al. Nature Contact and Human Health: A Research Agenda. Environ. Health Perspect. 2017, 125, 75001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The White House-The Biden-Harris Administration Immediate Priorities. Available online: https://www.whitehouse.gov/priorities/ (accessed on 3 April 2021).
- President-elect Biden and Vice President-elect Harris Introduce Key Climate Team Members-YouTube. Available online: https://www.youtube.com/watch?v=LSMX3Vlvzds (accessed on 19 December 2020).
- Unites States Government. Climate Change|The Biden-Harris plan to create union jobs by tackling the climate crisis. Available online: https://buildbackbetter.gov/priorities/climate-change/ (accessed on 19 December 2020).
- The Holy Father Pope Francis ENCYCLICAL LETTER LAUDATO SI’ OF THE HOLY FATHER FRANCIS ON CARE FOR OUR COMMON HOME. Available online: http://www.vatican.va/content/francesco/en/encyclicals/documents/papa-francesco_20150524_enciclica-laudato-si.html (accessed on 19 December 2020).
- National Public Radio (NPR). Fact Check: President Biden’s Inauguration Speech: NPR. Available online: https://www.npr.org/2021/01/20/956922884/bidens-inaugural-address-annotated (accessed on 21 January 2021).
- The White House Paris Climate Agreement. Available online: https://www.whitehouse.gov/briefing-room/statements-releases/2021/01/20/paris-climate-agreement/ (accessed on 1 May 2021).
- The White House Remarks by President Biden at the Virtual Leaders Summit on Climate Session 5: The Economic Opportunities of Climate Action. Available online: https://www.whitehouse.gov/briefing-room/speeches-remarks/2021/04/23/remarks-by-president-biden-at-the-virtual-leaders-summit-on-climate-session-5-the-economic-opportunities-of-climate-action/ (accessed on 1 May 2021).
- Masson-Delmotte, V.; Zhai, P.; Pörtner, H.-O.; Roberts, D.; Skea, J.; Shukla, P.R.; Pirani, A.; Moufouma-Okia, W.; Péan, C.; Pidcock, R.; et al. Global Warming of 1.5°C: An IPCC Special Report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change. Available online: https://www.ipcc.ch/site/assets/uploads/sites/2/2019/06/SR15_Summary_Volume_Low_Res.pdf (accessed on 27 January 2021).
- Griscom, B.W.; Adams, J.; Ellis, P.W.; Houghton, R.A.; Lomax, G.; Miteva, D.A.; Schlesinger, W.H.; Shoch, D.; Siikamäki, J.V.; Smith, P.; et al. Natural climate solutions. Proc. Natl. Acad. Sci. USA 2017, 114, 11645–11650. [Google Scholar] [CrossRef] [Green Version]
- Intergovernmental Panel on Climate Change Climate Change and Land: An IPCC Special Report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems WG I WG II WG III IPCC; Summary for Policymakers. Available online: https://www.ipcc.ch/srccl/chapter/summary-for-policymakers/ (accessed on 27 January 2021).
- Irga, P.J.; Burchett, M.D.; Torpy, F.R. Does urban forestry have a quantitative effect on ambient air quality in an urban environment? Atmos. Environ. 2015, 120, 173–181. [Google Scholar] [CrossRef] [Green Version]
- City of Boulder Urban Forest Strategic Plan. Available online: https://bouldercolorado.gov/forestry/urban-forest-strategic-plan (accessed on 28 January 2021).
- Rudee, A. Restoring Trees to the Landscape: Creating ‘Shovel-Ready’Jobs across the United States. WRI COVID-19 Response Spec; World Resources Institute: Washington, DC, USA, 2020. [Google Scholar]
- Bellassen, V.; Luyssaert, S. Carbon sequestration: Managing forests in uncertain times. Nat. News 2014, 506, 153. [Google Scholar] [CrossRef] [Green Version]
- De Deyn, G.B.; Cornelissen, J.H.C.; Bardgett, R.D. Plant functional traits and soil carbon sequestration in contrasting biomes. Ecol. Lett. 2008, 11, 516–531. [Google Scholar] [CrossRef]
- Carlyle-Moses, D.E.; Livesley, S.; Baptista, M.D.; Thom, J.; Szota, C. Urban trees as green infrastructure for stormwater mitigation and use. For. Interact. 2020, 397–432. [Google Scholar]
- Rahman, M.A.; Stratopoulos, L.M.F.; Moser-Reischl, A.; Zölch, T.; Häberle, K.-H.; Rötzer, T.; Pretzsch, H.; Pauleit, S. Traits of trees for cooling urban heat islands: A meta-analysis. Build. Environ. 2020, 170, 106606. [Google Scholar] [CrossRef]
- Wang, Z.-H.; Zhao, X.; Yang, J.; Song, J. Cooling and energy saving potentials of shade trees and urban lawns in a desert city. Appl. Energy 2016, 161, 437–444. [Google Scholar] [CrossRef]
- De Deyn, G.B.; Cornelissen, J.H.C.; Bardgett, R.D.; Scharenbroch, B.C. Urban trees for carbon sequestration. In Carbon Sequestration in Urban Ecosystems; Wiley Online Library: Hoboken, NJ, USA, 2012; Volume 11, pp. 121–138. [Google Scholar]
- Aerts, R.; Bruffaerts, N.; Somers, B.; Demoury, C.; Plusquin, M.; Nawrot, T.S.; Hendrickx, M. Tree pollen allergy risks and changes across scenarios in urban green spaces in Brussels, Belgium. Landsc. Urban Plan. 2021, 207, 104001. [Google Scholar] [CrossRef]
- Lara, B.; Rojo, J.; Fernández-González, F.; González-García-Saavedra, A.; Serrano-Bravo, M.D.; Pérez-Badia, R. Impact of Plane Tree Abundance on Temporal and Spatial Variations in Pollen Concentration. Forests 2020, 11, 817. [Google Scholar] [CrossRef]
- United Nations UN Report: Nature’s Dangerous Decline ‘Unprecedented’; Species Extinction Rates ‘Accelerating’ – United Nations Sustainable Development. Available online: https://www.un.org/sustainabledevelopment/blog/2019/05/nature-decline-unprecedented-report/ (accessed on 19 May 2021).
- Şekercioğlu, Ç.H.; Mendenhall, C.D.; Oviedo-Brenes, F.; Horns, J.J.; Ehrlich, P.R.; Daily, G.C. Long-term declines in bird populations in tropical agricultural countryside. Proc. Natl. Acad. Sci. USA 2019, 116, 9903–9912. [Google Scholar] [CrossRef] [Green Version]
- Cooke, R.S.C.; Eigenbrod, F.; Bates, A.E. Projected losses of global mammal and bird ecological strategies. Nat. Commun. 2019, 10, 2279. [Google Scholar] [CrossRef] [Green Version]
- McCallum, M.L. Vertebrate biodiversity losses point to a sixth mass extinction. Biodivers. Conserv. 2015, 24, 2497–2519. [Google Scholar] [CrossRef]
- Bolam, F.C.; Mair, L.; Angelico, M.; Brooks, T.M.; Burgman, M.; Hermes, C.; Hoffmann, M.; Martin, R.W.; McGowan, P.J.K.; Rodrigues, A.S.L.; et al. How many bird and mammal extinctions has recent conservation action prevented? Conserv. Lett. 2021, 14. [Google Scholar] [CrossRef]
- Ritchie, H. Extinctions-Our World in Data. Available online: https://ourworldindata.org/extinctions (accessed on 19 May 2021).
- Braveman, P.; Gruskin, S. Defining equity in health. J. Epidemiol. Community Health 2003, 57, 254–258. [Google Scholar] [CrossRef]
- Schlosberg, D. Defining Environmental Justice; Oxford University Press: Oxford, UK, 2007; ISBN 9780199286294. [Google Scholar]
- Anguelovski, I.; Connolly, J.J.T.; Pearsall, H.; Shokry, G.; Checker, M.; Maantay, J.; Gould, K.; Lewis, T.; Maroko, A.; Roberts, J.T. Opinion: Why green “climate gentrification” threatens poor and vulnerable populations. Proc. Natl. Acad. Sci. USA 2019, 116, 26139–26143. [Google Scholar] [CrossRef] [Green Version]
- Gould, K.; Lewis, T. Green Gentrification: Urban Sustainability and the Struggle for Environmental Justice; Routledge: London, UK, 2016; ISBN 315687321. [Google Scholar]
- Anguelovski, I. From Toxic Sites to Parks as (Green) LULUs? New Challenges of Inequity, Privilege, Gentrification, and Exclusion for Urban Environmental Justice. J. Plan. Lit. 2016, 31, 23–36. [Google Scholar] [CrossRef]
- Anguelovski, I.; Irazábal-Zurita, C.; Connolly, J.J.T. Grabbed Urban Landscapes: Socio-spatial Tensions in Green Infrastructure Planning in Medellín. Int. J. Urban Reg. Res. 2019, 43, 133–156. [Google Scholar] [CrossRef]
- Barcelona Lab for Urban Environmental Justice and Sustainability Green Gentrification. Available online: http://www.bcnuej.org/green-gentrification/ (accessed on 12 May 2021).
- Price, D. 7 Policies That Could Prevent Gentrification. Available online: https://shelterforce.org/2014/05/23/7_policies_that_could_prevent_gentrification/ (accessed on 12 May 2021).
- O’Neill, J.; Tabish, H.; Welch, V.; Petticrew, M.; Pottie, K.; Clarke, M.; Evans, T.; Pardo Pardo, J.; Waters, E.; White, H.; et al. Applying an equity lens to interventions: Using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J. Clin. Epidemiol. 2014, 67, 56–64. [Google Scholar] [CrossRef]
- Cronin-de-Chavez, A.; Islam, S.; McEachan, R.R.C. Not a level playing field: A qualitative study exploring structural, community and individual determinants of greenspace use amongst low-income multi-ethnic families. Health Place 2019, 56, 118–126. [Google Scholar] [CrossRef]
- Kaczynski, A.T.; Koohsari, M.J.; Stanis, S.A.W.; Bergstrom, R.; Sugiyama, T. Association of street connectivity and road traffic speed with park usage and park-based physical activity. Am. J. Health Promot. 2014, 28, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Zuniga-Teran, A.A.; Stoker, P.; Gimblett, R.H.; Orr, B.J.; Marsh, S.E.; Guertin, D.P.; Chalfoun, N. V Exploring the influence of neighborhood walkability on the frequency of use of greenspace. Landsc. Urban Plan. 2019, 190, 103609. [Google Scholar] [CrossRef]
- Jeffery, C.R. Crime Prevention Through Environmental Design; Sage Publications: Beverly Hills, CA, USA, 1971. [Google Scholar]
- Ardoin, N.M.; Bowers, A.W.; Gaillard, E. Environmental education outcomes for conservation: A systematic review. Biol. Conserv. 2020, 241, 108224. [Google Scholar] [CrossRef]
- Kruize, H.; van der Vliet, N.; Staatsen, B.; Bell, R.; Chiabai, A.; Muiños, G.; Higgins, S.; Quiroga, S.; Martinez-Juarez, P.; Aberg Yngwe, M.; et al. Urban Green Space: Creating a Triple Win for Environmental Sustainability, Health, and Health Equity through Behavior Change. Int. J. Environ. Res. Public Health 2019, 16, 4403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CHAWLA, A.L.; Rivkin, M. Early childhood education for sustainability in the United States of America. In Research in early childhood education for sustainability; Routledge: London, UK, 2014; pp. 264–281. ISBN 131576749X. [Google Scholar]
- Chawla, L. Benefits of Nature Contact for Children. J. Plan. Lit. 2015, 30, 433–452. [Google Scholar] [CrossRef]
- Chawla, L. The Natural World as Prepared Environment. NAMTA J. 2014, 39, 41–59. [Google Scholar]
- Chawla, L. Childhood nature connection and constructive hope: A review of research on connecting with nature and coping with environmental loss. People Nat. 2020, 2, 619–642. [Google Scholar] [CrossRef]
- Chawla, L. Childhood experiences associated with care for the natural world: A theoretical framework for empirical results. Child. Youth Environ. 2007, 17, 144–170. [Google Scholar]
- Chawla, L. Growing up green: Becoming an agent of care for the natural world. J. Dev. Process. 2009, 4, 6–23. [Google Scholar]
- Kuo, M.; Browning, M.H.E.M.; Sachdeva, S.; Lee, K.; Westphal, L. Might school performance grow on trees? Examining the link between “greenness” and academic achievement in urban, high-poverty schools. Front. Psychol. 2018, 9, 1669. [Google Scholar] [CrossRef] [PubMed]
- Browning, M.H.E.M.; Rigolon, A. School green space and its impact on academic performance: A systematic literature review. Int. J. Environ. Res. Public Health 2019, 16, 429. [Google Scholar] [CrossRef] [Green Version]
- Kuo, M.; Barnes, M.; Jordan, C. Do experiences with nature promote learning? Converging evidence of a cause-and-effect relationship. Front. Psychol. 2019, 10, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tuen Veronica Leung, W.; Yee Tiffany Tam, T.; Pan, W.-C.; Wu, C.-D.; Candice Lung, S.-C.; Spengler, J.D. How is environmental greenness related to students’ academic performance in English and Mathematics? Landsc. Urban Plan. 2019, 181, 118–124. [Google Scholar] [CrossRef]
- Gerstein, D.E.; Bates, C.R.; Bohnert, A.M. Evaluating a Green Schoolyard Transformation: A Protocol Utilizing the RE-AIM Framework. Child. Youth Environ. 2021, 31, 187–198. [Google Scholar] [CrossRef]
- Chawla, L.; Keena, K.; Pevec, I.; Stanley, E. Green schoolyards as havens from stress and resources for resilience in childhood and adolescence. Health Place 2014, 28, 1–13. [Google Scholar] [CrossRef]
- Muvengwi, J.; Kwenda, A.; Mbiba, M.; Mpindu, T. The role of urban schools in biodiversity conservation across an urban landscape. Urban For. Urban Green. 2019, 43, 126370. [Google Scholar] [CrossRef]
- American Forests What is Urban Forestry? A Quick 101-American Forests. Available online: https://www.americanforests.org/blog/what-is-urban-forestry-a-quick-101/?gclid=CjwKCAjwnPOEBhA0EiwA609ReSiWydv3nSL4MaFA_QXeCMxr8lNY7EgkLBLTVq1ofc3yMIJjbnhSXRoCPq4QAvD_BwE (accessed on 13 May 2021).
- Edwards, P.E.T.; Sutton-Grier, A.E.; Coyle, G.E. Investing in nature: Restoring coastal habitat blue infrastructure and green job creation. Mar. Policy 2013, 38, 65–71. [Google Scholar] [CrossRef]
- Groundwork Milwaukee Green Jobs & Education. Available online: https://www.groundworkmke.org/green-jobs-and-education (accessed on 8 April 2021).
- Wudeward Urban Forest Products The Forest Outside Your Front Door. Available online: https://wudeward.com/resources/ (accessed on 21 May 2021).
- Urban Wood Network What is Urban Wood? Available online: https://urbanwoodnetwork.org/about/what-is-urban-wood (accessed on 21 May 2021).
- MacFarlane, D.W. Potential availability of urban wood biomass in Michigan: Implications for energy production, carbon sequestration and sustainable forest management in the U.S.A. Biomass Bioenergy 2009, 33, 628–634. [Google Scholar] [CrossRef]
- Nowak, D.J.; Greenfield, E.J.; Ash, R.M. Annual biomass loss and potential value of urban tree waste in the United States. Urban For. Urban Green. 2019, 46, 126469. [Google Scholar] [CrossRef]
- USDA Forest Service. Successful Approaches to Recycling Urban Wood Waste; Department of Agriculture, Forest Service: Madison, WI, USA, 2002.
- Stai, S.M.; Wiseman, P.E.; Fernholz, K. Urban Wood Utilization in Virginia, North Carolina, and Georgia: A Comparison of Industry Practices and Perceptions. Available online: https://www.dovetailinc.org/upload/tmp/1579556331.pdf (accessed on 27 February 2021).
- Lewis, E.; Chamel, O.; Mohsenin, M.; Ots, E.; White, E.T. Biophilic Design LookBook. Available online: https://f.hubspotusercontent40.net/hubfs/5577290/PDFs/Think_Wood_BiophilicLookBook_021921.pdf?__hstc=206820108.85f5caba05e2f96f43e1f1b4fb5e08fe.1620923658976.1620923658976.1620923658976.1&__hssc=206820108.1.1620923658976&__hsfp=1568047958&hsCtaTracking=b9 (accessed on 21 May 2021).
- Dovetail Partners Estimates of Carbon Dioxide Withheld from the Atmosphere by Urban Hardwood Products. Available online: https://dovetailinc.org/portfoliodetail.php?id=5e260f4243877 (accessed on 21 May 2021).
- US Forest Service. Urban and Community Forestry Program. Available online: https://www.fs.usda.gov/managing-land/urban-forests/ucf (accessed on 25 May 2021).
- Wisconsin Department of Natural Resources. Available online: https://widnr.widen.net/view/pdf/77tgnbh66w/2020-Statewide-Forestry-Action-Plan.pdf?t.download=true&u=acpgx5 (accessed on 25 May 2021).
- Wolf, K.L.; Kruger, L.E. Urban Forestry Research Needs: A Participatory Assessment Process. J. For. 2010, 108, 39–44. [Google Scholar] [CrossRef]
- Sharma, S.; Henriques, I. Stakeholder influences on sustainability practices in the Canadian forest products industry. Strateg. Manag. J. 2005, 26, 159–180. [Google Scholar] [CrossRef]
- The New York Times Free Trees? Many Detroit Residents Say No Thanks. Available online: https://www.nytimes.com/2019/01/07/science/detroit-trees-health.html (accessed on 13 May 2021).
- Schwarz, K.; Fragkias, M.; Boone, C.G.; Zhou, W.; McHale, M.; Grove, J.M.; O’Neil-Dunne, J.; McFadden, J.P.; Buckley, G.L.; Childers, D.; et al. Trees grow on money: Urban tree canopy cover and environmental justice. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [Green Version]
- Reflo-Sustainable Water Solutions Green Schools Consortium of Milwaukee. Available online:https://www.gscm.refloh2o.com/ (accessed on 19 May 2021).
- Urban Milwaukee Menomonee Valley Partners, Urban Ecology Center Complete Transformation of 24-Acre Brownfield. Available online:https://urbanmilwaukee.com/pressrelease/menomonee-valley-partners-urban-ecology-center-complete-transformation-of-24-acre-brownfield/ (accessed on 13 May 2021).
- Arbor Day Foundation Urban Trees and Private Property. Available online:https://www.arborday.org/trees/bulletins/documents/093-summary.pdf (accessed on 13 May 2021).
- Ko, Y.; Lee, J.H.; McPherson, E.G.; Roman, L.A. Factors affecting long-term mortality of residential shade trees: Evidence from Sacramento, California. Urban For. Urban Green. 2015, 14, 500–507. [Google Scholar] [CrossRef]
- Ko, Y.; Roman, L.A.; Mcpherson, E.G.; Lee, J. Does Tree Planting Pay Us Back? Lessons from Sacramento, CA. Arborist News. 2016, 50–54. Arborist News. Available online: https://www.fs.fed.us/nrs/pubs/jrnl/2016/nrs_2016_ko_001.pdf (accessed on 10 February 2021).
- Roman, L.A.; Walker, L.A.; Martineau, C.M.; Muffly, D.J.; MacQueen, S.A.; Harris, W. Stewardship matters: Case studies in establishment success of urban trees. Urban For. Urban Green. 2015, 14, 1174–1182. [Google Scholar] [CrossRef] [Green Version]
- Groundwork Milwaukee Community Garden Health Hub. Available online: https://www.groundworkmke.org/health-hubs (accessed on 8 April 2021).
- Estes, N. A Red Deal. Available online: https://jacobinmag.com/2019/08/red-deal-green-new-deal-ecosocialism-decolonization-indigenous-resistance-environment (accessed on 28 January 2021).
- Curtice, K.; Choo, E. Indigenous populations: Left behind in the COVID-19 response. Lancet 2020, 395, 1753. [Google Scholar] [CrossRef]
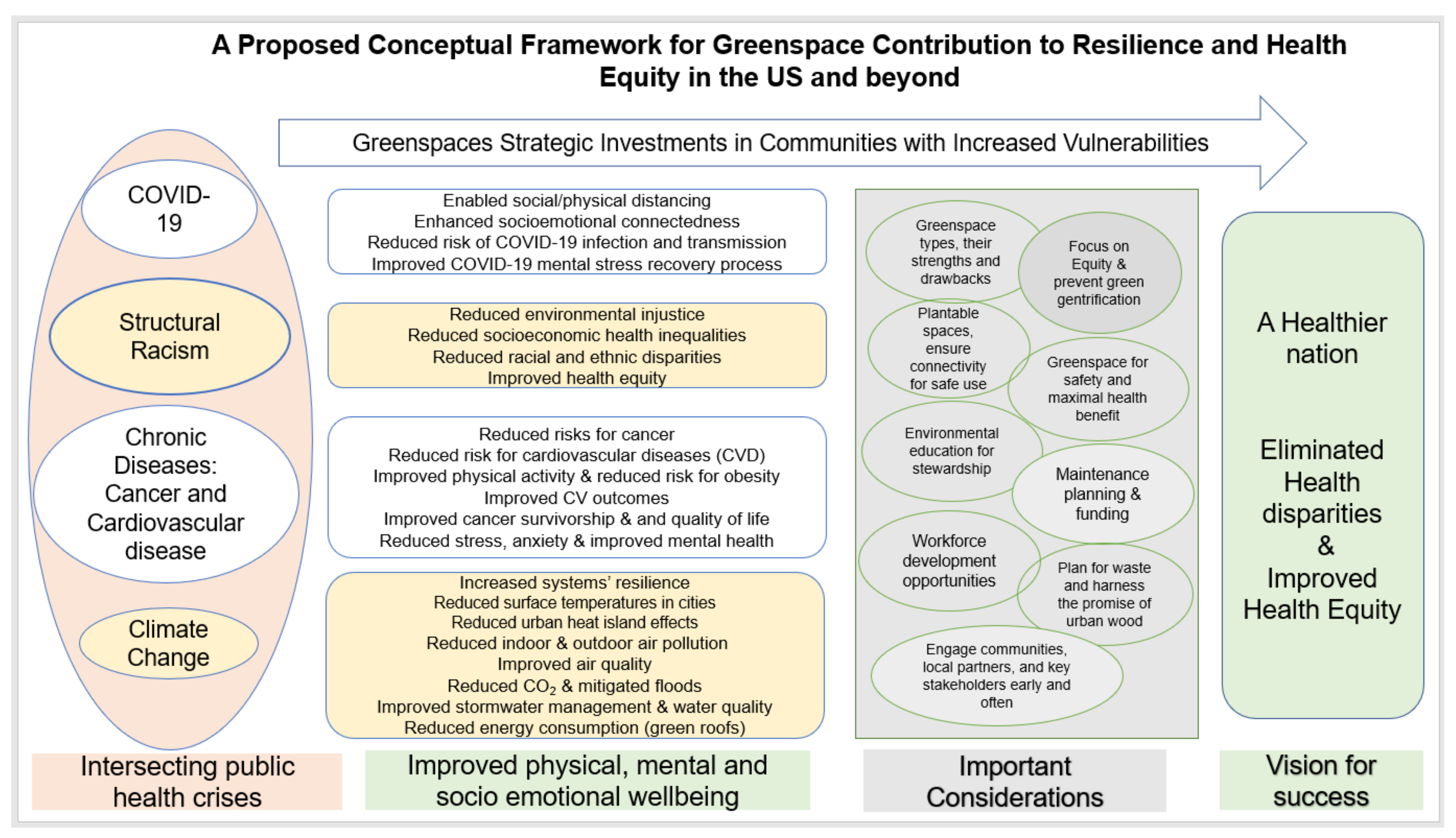
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bikomeye, J.C.; Namin, S.; Anyanwu, C.; Rublee, C.S.; Ferschinger, J.; Leinbach, K.; Lindquist, P.; Hoppe, A.; Hoffman, L.; Hegarty, J.; et al. Resilience and Equity in a Time of Crises: Investing in Public Urban Greenspace Is Now More Essential Than Ever in the US and Beyond. Int. J. Environ. Res. Public Health 2021, 18, 8420. https://doi.org/10.3390/ijerph18168420
Bikomeye JC, Namin S, Anyanwu C, Rublee CS, Ferschinger J, Leinbach K, Lindquist P, Hoppe A, Hoffman L, Hegarty J, et al. Resilience and Equity in a Time of Crises: Investing in Public Urban Greenspace Is Now More Essential Than Ever in the US and Beyond. International Journal of Environmental Research and Public Health. 2021; 18(16):8420. https://doi.org/10.3390/ijerph18168420
Chicago/Turabian StyleBikomeye, Jean C., Sima Namin, Chima Anyanwu, Caitlin S. Rublee, Jamie Ferschinger, Ken Leinbach, Patricia Lindquist, August Hoppe, Lawrence Hoffman, Justin Hegarty, and et al. 2021. "Resilience and Equity in a Time of Crises: Investing in Public Urban Greenspace Is Now More Essential Than Ever in the US and Beyond" International Journal of Environmental Research and Public Health 18, no. 16: 8420. https://doi.org/10.3390/ijerph18168420
APA StyleBikomeye, J. C., Namin, S., Anyanwu, C., Rublee, C. S., Ferschinger, J., Leinbach, K., Lindquist, P., Hoppe, A., Hoffman, L., Hegarty, J., Sperber, D., & Beyer, K. M. M. (2021). Resilience and Equity in a Time of Crises: Investing in Public Urban Greenspace Is Now More Essential Than Ever in the US and Beyond. International Journal of Environmental Research and Public Health, 18(16), 8420. https://doi.org/10.3390/ijerph18168420








